Abstract
Background and Purpose
In patients with acute ischemic stroke treated with thrombectomy, additional retriever passes may increase the likelihood of recanalization, but also the risk of intracranial hemorrhage. This multicenter retrospective register study aimed to evaluate the impact of retriever passes on treatment efficacy and safety outcomes in patients treated with mechanical thrombectomy.
Materials and Methods
Patients with ischemic stroke due to large artery occlusion in anterior circulation and treated with mechanical thrombectomy were enrolled. The primary efficacy outcome was a favorable functional outcome defined as modified Rankin Scale score of 0–2 at 90 days. Major safety outcome was symptomatic intracranial hemorrhage (SICH) and mortality. Multivariate logistic regression was used to analyze the impact of retriever passes on efficacy and safety outcomes.
Results
Of the 472 enrolled patients, the likelihood of favorable outcome declined in patients with more than three retriever passes (44.4% in patients with three passes, 26.3% with four passes, 14.8% with five or more passes). Multivariate logistic regression analysis identified three or less passes as an independent predictor for favorable functional outcomes (OR 2.44, 95% CI 1.10–5.45, P = 0.029). More than three passes was associated with an increased risk of SICH (OR 2.24, 95% CI 1.16–4.33, P = 0.016).
Conclusions
More than three retriever passes may increase the rate of recanalization, but not the likelihood of favorable functional outcomes in ischemic stroke patients treated with mechanical thrombectomy. Notably, multiple retriever passes may also increase the risk of intracranial hemorrhage.
Evidence-Based Medicine
Level of Evidence: Level 4, Case Series.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mechanical thrombectomy has emerged as a first-line treatment for acute ischemic stroke caused by large arterial occlusion. Favorable outcomes depend on timely and successful recanalization of the target vessels [1,2,3,4,5]. However, recanalization with stent retriever thrombectomy is not always successful after the initial pass even using the latest devices. Additional retriever passes may increase the likelihood of recanalization, in addition to the risks of intracranial hemorrhage and artery reocclusion [6, 7] and such extra attempts may also prolong the procedure times. The disadvantages of multiple retriever passes may attenuate or even negate the positive effects of recanalization. Therefore, determination of the maximum optimal number of retriever passes is important in order to optimize the treatment efficacy and safety of the thrombectomy procedure.
Previous studies observed that the recanalization rate increased slightly, but the risk of parenchymal hemorrhage increased simultaneously, with more than three passes of Merci or pREset stent retriever [8, 9]. Thereafter, the maximal number of retriever passes was prescriptively limited to three for any given occlusion. This criterion was followed in a majority of clinical trials [10, 11], but in a minority of trials, up to six passes was permitted [12]. As part of the instructions for the Solitaire retriever (Covidien, Irvine, CA) used to treat ischemic stroke, no more than three passes are recommended. On the other hand, in the instructions for the Trevo retriever (Stryker, Fremont, CA), a structurally similar device, up to six passes are recommended. Although some studies observed increased recanalization rate with more than three passes [9, 13], whether this additional recanalization could translate into favorable outcomes remains to be determined.
It is well known that intracranial atherosclerotic disease-related large artery occlusion is typically refractory to mechanical thrombectomy with the recommended number of retriever passes and usually requires multiple retriever passes or additional angioplasty [14]. The importance of when to terminate the thrombectomy procedure after multiple retriever passes is obviously, so an ideal chance/risk trade-off on the number of retriever passes might be expected for positive patient outcomes. This study aimed to evaluate the impact of multiple retriever passes on procedure efficacy and safety outcomes in a cohort of Chinese acute ischemic stroke patients treated with mechanical thrombectomy.
Methods
Study Design and Patients
Endovascular treatment for Acute Anterior Circulation Ischemic Stroke Registry (ACTUAL) is a multicenter register program to assess the efficacy and safety of endovascular treatment for acute ischemic stroke in real-world practice. All clinical data from patients with acute ischemic stroke due to large artery occlusion in anterior circulation receiving mechanical thrombectomy were retrospectively collected from 21 stroke centers in China. Each center performed at least 30 endovascular procedures annually. Ethics approval was obtained from ethics committee of each local center. Due to its retrospective nature, the informed consent to study was waived by the local ethical committees.
Patients were typically treated with thrombectomy if they: (1) were diagnosed with acute ischemic stroke; (2) aged 18 years or older; (3) had a causal occlusion in internal carotid artery, M1 or M2 segment of the middle cerebral artery; (4) had a premorbid modified Rankin Scale (mRS) score of < 2; (6) had a pretreatment Alberta Stroke Program Early Computed Tomography Score (ASPECTS) of ≥ 6; and (7) could be initiated with thrombectomy within 6 h of stroke onset. To precisely assess the impact of retriever passes, patients were excluded if the target vessel was recanalized via thrombus aspiration, balloon angioplasty or stenting implantation.
Baseline Assessment
Stroke etiology was classified according to the criteria outlined in Trial of ORG 10172 in Acute Stroke Treatment (TOAST) [15]. Baseline stroke severity was assessed with National Institutes of Health Stroke Scale (NIHSS) on admission. Pretreatment cerebral infarction cores were evaluated with ASPECTS [16]. The score of ASPECTS ranges from 0 to 10, with a score of greater than 7 indicating a small or absent infarction core. Collateral status was evaluated with the American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) grading system [17]. ASITN/SIR score range from 0 (no collateral perfusion) to 4 (complete collateral perfusion). All imaging results were retrospectively assessed by two physicians independently, if disagreement existed, the opinion of a third experienced physicians was invited.
Endovascular Procedures
Intravenous thrombolysis was recommended if recombinant tissue plasminogen activator (rt-PA) bolus could be initiated within 4.5 h of stroke onset as per current AHA/ASA guidelines suggested criteria for acute ischemic stroke [18]. All patients eligible for intravenous thrombolysis were treated with mechanical thrombectomy given they met the aforementioned criteria. Thrombectomy was usually performed with a Solitaire or a Trevo retriever. Distal occlusion balloons were not used routinely, because the device was unavailable in most involving centers. Successful recanalization was defined as a modified Thrombolysis in Cerebral Infarction (mTICI) score of 2b or 3 [17]. One retriever pass was defined as a stent-like device passed through the occlusion inside a microcatheter, deployed completely, and was pulled out successfully through the guiding catheter [19]. Any additional attempt of pass was left open to the operator. The prospective decision of termination of each single procedure was based on the experience of interventionists given that various clinical factors as well as procedure complications, including the tortuosity vascular access, impacted clot, and underlying stenosis in situ thrombosis, all of which are usually suspected to be resistant case. No mandatory minimum or maximum number of retriever passes was made in this real practice.
Outcome Measurements
Patients were followed up with a clinic visit or via a telephone interview at 90 days after the index stroke. Primary efficacy outcome was a favorable functional outcome defined as mRS of 0–2 at 90 days, and secondary clinical outcomes of successful recanalization defined as mTICI score of 2b or 3. Major safety outcomes were absence of symptomatic intracranial hemorrhage (SICH) within 72 h after thrombectomy and mortality at 90 days. A CT scan was performed within 3 days of endovascular treatment, or whenever an intracranial hemorrhage (ICH) was indicated. Intracranial hemorrhage was determined as symptomatic or asymptomatic ones according to Heidelberg Bleeding Classification criteria [20]. Symptomatic intracranial hemorrhage (SICH) was diagnosed if the newly observed ICH was associated with any of the following items: (1) neurological deterioration ≥ 4 total points on NIHSS at the time of diagnosis compared to immediately before worsening; (2) an increase of ≥ 2 points in any NIHSS subcategory; (3) deterioration led to intubation, hemicraniectomy, external ventricular drain placement, or any other major medical/surgical interventions; (4) absence of alternative explanation for deterioration. Asymptomatic ICH was diagnosed if the newly observed ICH was not accompanied by any implications for prognosis or change in management, and there is no substantive change in the patient’s neurological status.
Statistical Analysis
Kolmogorov–Smirnov test was performed to evaluate the normality of distribution. Continuous variables were presented as means and SDs, but medians and interquartile ranges were used in case of non-normal distributions. Categorical variables were presented as numbers and percentages. The Student t test or the Mann–Whitney U test was used to compare continuous variables according to their normality. The Chi-square or the Fisher exact test was used to compare categorical variables where applicable. Receiver operator characteristic curve (ROC) analysis at maximum Youden index was performed to identify the cut-off points for the optimum number of retriever passes. Multivariate logistic regression was used to analyze the impact of retriever passes on clinical outcomes after adjusting for confounders with at least marginal significance (P < 0.1) or clinically relevant factors. A two-tailed P value < 0.05 was deemed statistically significant. Statistical analyses were performed using SPSS 22.0 (IBM, Armonk, NY).
Result
Study Population
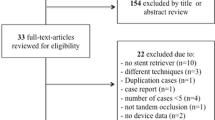
The ACTUAL retrospectively enrolled 698 consecutive acute ischemic stroke patients with endovascular treatment. Of the 632 patients who received stent retriever thrombectomy, 64 patients were treated with retrievable stent combined stent implantation, 48 patients with combined balloon, 42 patients with combined balloon and stent implantation, and 6 patients with combined aspiration. Ultimately, a cohort of 472 patients treated with the stent retriever alone was enrolled in this study. The selection flowchart is shown in online resource Figure 1.
Comparisons of Baseline Characteristics and Outcomes
Demographic and baseline characteristics are presented in Table 1. Mean age was 64.9 ± 12.2 years, and 55.3% of enrolled patients were male. Solitaire retriever was used in 468 (99.2%), and Trevo retriever in 4 (0.8%) patients. Successful recanalization was achieved in 407 (86.2%) patients and favorable functional outcome was obtained in 194 (41.1%) patients. Symptomatic intracranial hemorrhage was observed in 81 patients (17.2%) within 72 h after endovascular treatment and the overall mortality was 25.8% (122/472) at 90 days.
Of the 472 patients treated with stent retriever thrombectomy alone, 169 (35.8%) were attempted with one, 157 (33.3%) with two, 81 (17.2%) with three, and 65 (13.7%) with four or more passes. The median number of retriever passes was two (ranged 1–9, Online Resource Table 1). Univariate analysis revealed that the rate of successful recanalization increased with the number of retriever passes (77.8% in patients with three passes, 86.8% in patients with four passes, Fig. 1). The likelihood of favorable outcome declined with number of retriever passes in patients with three or more passes (44.4% in patients with three passes, 26.3% in patients with four passes, 14.8% in patients with five or more passes). Meanwhile, the risk of SICH (21% in patients with three passes, 26.3% in patients with four passes, 40.7% in patients with five or more passes) and mortality (27.2% in patients with three passes, 31.6% in patients with four passes, 44.4% in patients with five or more passes) increased with number of retriever passes. Furthermore, ROC analysis at maximum Youden index identified 2.5 passes as the cut-off for positive 90-day functional outcomes (maximum Youden index = 0.083). Regarding ISCH, 2.5 passes was also identified as the best discriminator (maximum Youden index = 0.106). Based on a real clinical practice, three passes was identified as the ideal chance/risk trade-off between the efficiency and safety.
When patients were dichotomized by procedure employing less than or equal to three passes or more than three passes (Table 1). Patients with three or less passes had a lower baseline NIHSS score (median 17, IQR 13–21 versus 19, IQR 15–23; P = 0.048) and better collateral circulation (52.8 vs. 28.1%; P < 0.001) than those with more than three passes. Those with more than three passes had a lower proportion of successful recanalization (78.5 vs. 87.5%; P = 0.05), longer procedure time (143 vs. 90 min; P < 0.001) and higher risk of symptomatic intracranial hemorrhage (32.3 vs. 14.7%; P < 0.001) than those with three or less passes. Patients with more than three passes had a lower proportion of favorable functional outcomes (21.5 vs. 44.2%; P = 0.001; Fig. 2), and higher mortality at 90 days (36.9 vs. 24.1%; P = 0.028).
Predictors of Efficacy and Safety Outcomes
After adjusting for major confounders, multivariate logistic regression identified successful recanalization as an independent predictor for favorable functional outcome (OR 4.38, 95% CI 1.79–10.72, P = 0.001; Table 2). Three or less retrievers passes was associated with favorable functional outcome (OR 2.44, 95% CI 1.10–5.45, P = 0.029). Furthermore, completing more than three passes was associated with an increased risk of SICH (OR 2.24, 95% CI 1.16–4.33, P = 0.016; Online Resource Table 2), but was not an independent predictor of mortality (OR 1.30, 95% CI 0.55–3.07, P = 0.547).
Subgroup Analysis
A total of 65 patients treated with more than three passes, up to 51 (78.5%) patients still achieved successful recanalization. However, no difference was found in the rate of favorable functional outcomes at 90 days between successful recanalization and unsuccessful recanalization (23.5 vs. 14.3%; P = 0.716, Online Resource Figure 2). With regarding safety outcomes, a statistic difference on SICH was not also found between successful recanalization and unsuccessful recanalization (31.4 vs. 35.7%; P = 0.757), whereas a higher mortality was identified in patients with unsuccessful recanalization (64.3 vs. 29.4%; P = 0.017). After adjusting for age, hypertension, admission glucose level, pretreatment systolic blood pressure, initial NIHSS and SICH, the multivariate analysis found that successful recanalization was not any more associated with mortality (OR 0.36, 95% CI 0.05–2.53, P = 0.306).
Discussion
In this multicenter registry study, the chance of successful recanalization increased with every extra retriever pass, but the probability of a favorable outcome decreased after three retriever passes. Conversely, the risk of SICH and mortality increased significantly. Furthermore, three or less passes was identified as an independent predictor of favorable functional outcomes, and more than three passes was associated with an increased risk of SICH.
The results of this study indicated that the additional recanalization achieved with more than three passes of retriever do not necessarily translate into a favorable outcome. The higher proportion of futile recanalization in patients with multiple retriever passes may be explained, in part, by the delay of recanalization. In this study, median procedure times to recanalization with three or less passes was 90 min, while it was 143 min in patients with more than three passes. In clinical trials [10, 12], delayed recanalization has been associated with unfavorable functional outcomes in patients treated with mechanical thrombectomy. Pooled analysis demonstrated that every 30-min delay in recanalization may increase the likelihood of functional dependence (mRS ≥ 3) by 11% [21]. Meanwhile, previous studies have demonstrated that multiple retriever passes more easily induce endothelial damage [6, 22], which can result in artery stenosis or reocclusion after recanalization, or embolize the distal artery and block the collateral flow to the potentially salvageable tissues [23, 24]. All these possibilities may decrease the likelihood of favorable outcomes in patients treated with multiple retrievers passes.
With regarding safety outcomes, a higher rate of SICH (32.3 vs. 14.7%) and mortality (36.9 vs. 24.1%) was observed in patients with multiple retriever passes compared to patients with three or less passes. Multiple retriever passes may cause endothelial damage and blood–brain barrier disruption, both of which were associated with increased risk of SICH [25, 26]. It has been demonstrated that SICH may significantly decrease the likelihood of favorable functional outcomes after mechanical thrombectomy [7]. Therefore, an increased risk of SICH may be also partly responsible for the futile recanalization in patients with multiple retrievers passes. Meanwhile, consistent with the North American Solitaire Acute (NASA) Stroke Registry, more than three passes and SICH were associated with a higher mortality despite achieving successful recanalization [27].
One of crucial issues addressed in this study was when should thrombectomy procedure be terminated after multiple retriever passes and other revascularization measures sought. In this study, we found that three passes provide the optimal balance point between efficacy and safety, as successful recanalization was not any more associated with a favorable functional outcome after three unsuccessful retrievals. However, no more than two retriever passes was identified as an appropriate number for favorable functional outcomes in other studies [28, 29]. This discrepancy may be explained by the fact that more patients (13.8%) were treated with more than three passes in this study, while only 6.3% of patients listed in the NASA Stroke Registry were treated with more than three passes in NASA Stroke Registry [30]. In addition, patients with acute ischemic stroke caused by atherosclerotic and occluded of the terminal internal carotid artery were more common in our cohort. These patients usually require more retriever passes for the recanalization of an occluded artery [14, 31].
Several limitations of this study should be noted when interpreting the results. The retrospective nature of the study may have generated systematic biases. For example, the involved centers may have followed different protocols of endovascular treatment. Secondly, reocclusion or distal embolization, which might affect clinical outcomes, was not assessed in this cohort. Finally, whether an additional pass should be attempted or not was usually determined by the interventionists based on their clinical experiences, which may have also generated bias.
In conclusion, more than three retriever passes may increase the rate of successful recanalization, but not the likelihood of favorable functional outcomes. Additionally, multiple retriever passes may be associated with an increased risk of intracranial hemorrhage.
Abbreviations
- SICH:
-
Symptomatic intracranial hemorrhage
- mTICI:
-
Modified thrombolysis in cerebral infarction
- mRS:
-
Modified Rankin Scale
- ACTUAL:
-
Endovascular Treatment for Acute Anterior Circulation Ischemic Stroke Registry
References
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20. https://doi.org/10.1056/nejmoa1411587.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009–18. https://doi.org/10.1056/nejmoa1414792.
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–306. https://doi.org/10.1056/nejmoa1503780.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–30. https://doi.org/10.1056/nejmoa1414905.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–95. https://doi.org/10.1056/nejmoa1415061.
Kang DH, Kim YW, Hwang YH, Park SP, Kim YS, Baik SK. Instant reocclusion following mechanical thrombectomy of in situ thromboocclusion and the role of low-dose intra-arterial tirofiban. Cerebrovasc Dis. 2014;37(5):350–5. https://doi.org/10.1159/000362435.
Hao Y, Yang D, Wang H, Zi W, Zhang M, Geng Y, et al. Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke. Stroke. 2017;48(5):1203–9. https://doi.org/10.1161/strokeaha.116.016368.
Loh Y, Jahan R, McArthur DL, Shi ZS, Gonzalez NR, Duckwiler GR, et al. Recanalization rates decrease with increasing thrombectomy attempts. AJNR Am J Neuroradiol. 2010;31(5):935–9. https://doi.org/10.3174/ajnr.a1958.
Kurre W, Aguilar-Perez M, Schmid E, Sperber W, Bazner H, Henkes H. Clinical experience with the pREset stent retriever for the treatment of acute ischemic stroke—a review of 271 consecutive cases. Neuroradiology. 2014;56(5):397–403. https://doi.org/10.1007/s00234-014-1346-y.
Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380(9849):1241–9. https://doi.org/10.1016/s0140-6736(12)61384-1.
Pereira VM, Gralla J, Davalos A, Bonafe A, Castano C, Chapot R, et al. Prospective, multicenter, single-arm study of mechanical thrombectomy using Solitaire Flow Restoration in acute ischemic stroke. Stroke. 2013;44(10):2802–7. https://doi.org/10.1161/strokeaha.113.001232.
Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012;380(9849):1231–40. https://doi.org/10.1016/s0140-6736(12)61299-9.
Angermaier A, Michel P, Khaw AV, Kirsch M, Kessler C, Langner S. Intravenous thrombolysis and passes of thrombectomy as predictors for endovascular revascularization in ischemic stroke. J Stroke Cerebrovasc Dis. 2016;25(10):2488–95. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.06.024.
Matias-Guiu JA, Serna-Candel C, Matias-Guiu J. Stroke etiology determines effectiveness of retrievable stents. J Neurointerv Surg. 2014;6(2):e11. https://doi.org/10.1136/neurintsurg-2012-010395.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000;355(9216):1670–4. https://doi.org/10.1016/s0140-6736(00)02237-6.
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44(9):2650–63. https://doi.org/10.1161/strokeaha.113.001972.
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals From the American Heart Association/American Stroke Association. Stroke. 2015;46(10):3020–35. https://doi.org/10.1161/str.0000000000000074.
Hann S, Chalouhi N, Starke R, Gandhe A, Koltz M, Theofanis T, et al. Comparison of neurologic and radiographic outcomes with Solitaire versus Merci/Penumbra systems for acute stroke intervention. Biomed Res Int. 2013;2013:715170. https://doi.org/10.1155/2013/715170.
von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg Bleeding Classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015;46(10):2981–6. https://doi.org/10.1161/strokeaha.115.010049.
Shi ZS, Liebeskind DS, Xiang B, Ge SG, Feng L, Albers GW, et al. Predictors of functional dependence despite successful revascularization in large-vessel occlusion strokes. Stroke. 2014;45(7):1977–84. https://doi.org/10.1161/strokeaha.114.005603.
Gory B, Bresson D, Kessler I, Perrin ML, Guillaudeau A, Durand K, et al. Histopathologic evaluation of arterial wall response to 5 neurovascular mechanical thrombectomy devices in a swine model. AJNR Am J Neuroradiol. 2013;34(11):2192–8. https://doi.org/10.3174/ajnr.a3531.
Kurre W, Vorlaender K, Aguilar-Perez M, Schmid E, Bazner H, Henkes H. Frequency and relevance of anterior cerebral artery embolism caused by mechanical thrombectomy of middle cerebral artery occlusion. AJNR Am J Neuroradiol. 2013;34(8):1606–11. https://doi.org/10.3174/ajnr.A3462.
Chalumeau V, Blanc R, Redjem H, Ciccio G, Smajda S, Desilles JP, et al. Anterior cerebral artery embolism during thrombectomy increases disability and mortality. J Neurointerv Surg. 2018. https://doi.org/10.1136/neurintsurg-2018-013793.
Khatri R, McKinney AM, Swenson B, Janardhan V. Blood-brain barrier, reperfusion injury, and hemorrhagic transformation in acute ischemic stroke. Neurology. 2012;79(13 Suppl 1):S52–7. https://doi.org/10.1212/WNL.0b013e3182697e70.
Renu A, Laredo C, Lopez-Rueda A, Llull L, Tudela R, San-Roman L, et al. Vessel wall enhancement and blood-cerebrospinal fluid barrier disruption after mechanical thrombectomy in acute ischemic stroke. Stroke. 2017;48(3):651–7. https://doi.org/10.1161/strokeaha.116.015648.
Linfante I, Walker GR, Castonguay AC, Dabus G, Starosciak AK, Yoo AJ, et al. Predictors of mortality in acute ischemic stroke intervention: analysis of the North American Solitaire Acute Stroke Registry. Stroke. 2015;46(8):2305–8. https://doi.org/10.1161/strokeaha.115.009530.
Linfante I, Starosciak AK, Walker GR, Dabus G, Castonguay AC, Gupta R, et al. Predictors of poor outcome despite recanalization: a multiple regression analysis of the NASA registry. J Neurointerv Surg. 2016;8(3):224–9. https://doi.org/10.1136/neurintsurg-2014-011525.
Seker F, Pfaff J, Wolf M, Ringleb PA, Nagel S, Schonenberger S, et al. Correlation of thrombectomy maneuver count with recanalization success and clinical outcome in patients with ischemic stroke. AJNR Am J Neuroradiol. 2017;38(7):1368–71. https://doi.org/10.3174/ajnr.A5212.
Zaidat OO, Castonguay AC, Gupta R, Sun CH, Martin C, Holloway WE, et al. North American Solitaire Stent Retriever Acute Stroke registry: post-marketing revascularization and clinical outcome results. J Neurointerv Surg. 2014;6(8):584–8. https://doi.org/10.1136/neurintsurg-2013-010895.
Eesa M, Almekhlafi MA, Mitha AP, Wong JH, Goyal M. Manual aspiration thrombectomy through balloon-tipped guide catheter for rapid clot burden reduction in endovascular therapy for ICA L/T occlusion. Neuroradiology. 2012;54(11):1261–5. https://doi.org/10.1007/s00234-012-1039-3.
Acknowledgements
We acknowledge Shuyan Lu, Ph.D., for her statistical assistance.
Funding
This study was partly funded by National Natural Science Foundation of China (Nos. 81571143, 81400993 and 81530038), Jiangsu Provincial Special Program of Medical Science (No. BL2013025) and Chinese Postdoctoral Science Fund (No. 2015M572815).
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bai, Y., Pu, J., Wang, H. et al. Impact of Retriever Passes on Efficacy and Safety Outcomes of Acute Ischemic Stroke Treated with Mechanical Thrombectomy. Cardiovasc Intervent Radiol 41, 1909–1916 (2018). https://doi.org/10.1007/s00270-018-2022-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2022-0