Abstract
To clarify the changes of cervical (cVEMP) and ocular (oVEMP) vestibular evoked myogenic potentials induced by air-conducted sound (ACS) and bone-conducted vibration (BCV) in patients with vestibular neuritis (VN), patients with VN (n = 30) and normal controls (n = 45) underwent recording of cVEMP and oVEMP in response to ACS (1,000 Hz, 5 ms, tone bursts) and BCV (500 Hz, short tone burst). Patients with VN showed a high proportion of oVEMP abnormalities in response to both ACS (80.0 %) and BCV at the forehead (Fz, 73.3 %) or the mastoid (76.7 %). In contrast, cVEMPs were mostly normal with both ACS and BCV in the patients. The dissociations in the abnormalities of cVEMP and oVEMP induced by ACS and BCV at the mastoids and at the forehead in patients with VN suggest that oVEMP reflects functions of the superior vestibular nerve and most likely the utricular function. The results of our study suggest that oVEMP induced by either ACS or BCV appears to depend on integrity of the superior vestibular nerve, possibly due to the utricular afferents travelling in it. In contrast, cVEMP elicited by either ACS or BCV may reflect function of the saccular afferents running in the inferior vestibular nerve.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Air-conducted sound (ACS) or bone-conducted vibration (BCV) elicits vestibular evoked myogenic potentials (VEMPs) that are now widely used to assess the otolith function [1]. Cervical VEMPs (cVEMPs) are recorded in the contracted sternocleidomastoid (SCM) muscles in response to either the ACS or BCV, and are known to reflect the functions of ipsilateral saccular and inferior vestibular nerve [2, 3]. In contrast, ocular VEMPs (oVEMPs) are recorded from the extraocular muscles, mostly the inferior oblique ones that are known to reflect crossed otolithic function originating from the contralateral utricle. In contrast to cVEMP that reflects descending uncrossed sacculocollic pathway in the lower brainstem [4], oVEMP may be mediated by ascending connection to the oculomotor nuclei and probably a manifestation of crossed otolith-ocular reflex pathways [5–9].
It has previously been believed that the vestibular responses evoked by sounds originate from the saccule and are mediated by the saccular afferents running in the inferior division of the vestibular nerve [1, 10, 11]. However, there has been increasing evidence supporting that ACS stimulates not only the saccular receptors, but also some utricular receptors [3, 10–14]. In the guinea pigs, the utricular afferents in the caudal superior vestibular nerve are activated by ACS as well as BCV [13, 15, 16].
Our recent study has also documented that patients with superior vestibular neuritis (VN) had an abnormal oVEMP and normal cVEMP in response to ACS, while those with inferior VN exhibited a normal oVEMP and abnormal cVEMP to ACS [6]. The dissociations in the abnormalities of cVEMP and oVEMP in patients with superior or inferior VN suggest that oVEMP in response to ACS may be mediated by the superior vestibular nerve and an activation of the utricular receptors.
Although there have been increasing evidences showing that both the utricular and saccular afferents are activated by ACS as well as BCV [12, 15, 17, 18], there have been debates regarding whether the saccular and utricular neurons can be selectively activated by ACS and BCV, i.e., the afferent specificity [19–21]. In this study, we attempted to determine the pathways mediating the oVEMP and cVEMP in response to ACS and BCV by characterizing the abnormalities in patients with VN.
Methods
Subjects
In this prospective study, we enrolled 30 patients with a mean age of 56 years (range 25–78 years, 15 men) with acute onset of severe prolonged vertigo whose symptoms include postural imbalance, spontaneous nystagmus, nausea or vomiting during a period ranging from March to December, 2012. All the patients were evaluated within ten days (range 2–6 days) of symptom onset in the acute stage of the disease. The patients underwent neuro-otologic evaluations and these include audiometric examination, caloric test, subjective visual vertical (SVV) test, and the cVEMP and oVEMP testing with ACS and BCV at the mastoid process and in the middle forehead (Fz) (Table 1).
Inclusion criteria for patients with VN in the current study were as follows: (1) Acute onset of vertigo, (2) Appearance of mixed horizontal and torsional nystagmus, (3) A positive head-impulse test for the horizontal semicircular canal (SCC), (4) A unilaterally absent or reduced caloric response, i.e., a caloric paresis score >25 %, (5) The absence of auditory and neurologic signs. In addition, exclusion criteria for the current study are as follows: (1) Concurrent auditory symptoms, (2) A previous history of hearing impairment.
We served 45 normal healthy people with a mean age of 51.8 years (range 22–78 years, consisting of 21 men and 24 women) who had no deficits of hearing or vestibular function. There were no differences in the age and sex ratio between the patient and control groups. All the procedures were performed in accordance with the Declaration of Helsinki and were approved by the Institutional Review Board (IRB) of Chonbuk National University Hospital.
Cervical and ocular VEMP recording
To record cVEMPs, we placed the subjects on a bed in a supine position, raised their head to approximately 30° from the horizontal, rotated it contralaterally and activated the sternocleidomastoid muscle (SCM). Then the surface EMG activity was measured from an active electrode placed over the belly of the ipsilateral SCM and from a reference electrode on the medial clavicle using self-adhesive Ag/AgCl electrodes. An earth electrode was placed over the sternum.
To record oVEMPs using surface EMG electrodes, we placed the subjects on a bed in a supine position with the head supported on a pillow. In each eye, the active recording electrode was placed on the infra-orbital ridge 1 cm below the center of each lower eyelid and the reference electrode was placed about 2 cm below that active electrode [7, 8, 20, 22]. The ground electrode was placed on the forehead. During oVEMP recording, the subjects had an upward gaze approximately 25° above straight ahead and maintained a small fixation point approximately 60 cm from the eyes. The signals were amplified by differential amplifiers (bandwidth 10–2,000 Hz), and the unrectified signals were averaged (n = 100).
Stimuli were generated by customized software (Cadwell Laboratories, Kennewick, WA). We used unilateral 1000 Hz, 5 ms ACS tone bursts as the stimulation delivered at an intensity of 100 dB nHL through calibrated headphones. The maximum tone burst amplitude was 50 μV and a total of 100 stimuli were delivered at a rate of 5 Hz. The potentials were sampled at 10 kHz for 60 ms, from 10 ms before to 50 ms following the stimulus onset. For BC stimulation, vibration was delivered to the middle forehead (Fz) and each mastoid of all the subjects by a hand-held minishaker with an attached perspex rod (Model 4810, Bruel and Kjaer P/L, Denmark). The BC vibration was used by the pulse stimulus with the peak amplitude of the stimulus was at 85 dB force level (FL). Tone stimuli were used at 500 Hz frequency with 2-1-2 Pip which has a 2 cycle rise, 1 cycle plateau and a 2 cycle fall. A total of 100 stimuli were presented at a rate of 5.1 Hz and recorded from 10 ms before to 60 ms after stimulus onset. Cervical VEMPs generated by the vibration of the mastoid process were recorded ipsilaterally. To evaluate the response that was recorded from the SCM ipsilateral to the stimulated mastoid, the initial biphasic positive and negative peaks were measured. Then, the EMG potentials were amplified, band-pass filtered at 10–3,000 Hz, and sampled at 5 kHz. Following this, the data from the stimulus onset to 50 ms was averaged. To ensure adequate levels of activation and to enable fine adjustment of the head position, we monitored the subjects to adjust the EMG levels for each side and to allow measurement of the background contraction levels and the calculation of the normalized amplitudes. We used EMG rectification to calculate amplitudes, where the amplitude was defined as the value of the difference between p13 and n23. To calculate the asymmetry ratio (AR) of the amplitude, the difference of the amplitudes between the sides were divided by the sum and then multiplied by 100.
Both p13 and n23 peak latencies were calculated. We did not record cVEMP induced by BC vibration in the forehead because we had difficulties in maintaining the adequate contraction of SCM muscles during the forehead vibration. For oVEMPs produced by bone vibration at the mastoids, the initial negative and positive peaks beneath the eye contralateral to the stimulated mastoid were obtained. For vibration stimulation in the forehead region (Fz), the earliest biphasic peaks were measured bilaterally. Negative potentials at the active electrodes were displayed as upward deflections. The amplitude of n10 was defined from the negative peak to the positive one. The symmetry of the n10 amplitude of each eye was quantified by the AR, as defined above according to the amplitude of the n10 response to stimulation.
For both cervical and ocular VEMPs, responses from the neck and eyes are described with reference to the lesion side, i.e., the ‘‘ipsilesional’’ or ‘‘contralesional’’ side in both groups.
Caloric irrigation and subjective visual vertical (SVV)
All the patients were tested with the bithermal caloric test and the subjective visual vertical (SVV) test. The detailed methods of SVV were described at the previous report [6, 9]. Vestibular paresis on caloric irrigation was defined as an asymmetry of more than 25 % [23], and a mean of more than ±2.5° of the ten measurements of the static SVV determined binocularly was considered a criterion for a pathological tilt of static SVV.
Statistical analysis
All the data about ipsilesioanl and contralesional responses to the side of the neuritis was re-coded, thus making it possible to manage the results at a time with no respect to the location of the neuritis. We compared such variables as latencies, amplitude and AR between the two groups using the Student t tests. In addition, we compared the clinical characteristics between the two groups using the Chi square and the ANOVA. Statistical analysis was done using SPSS version 14 (SPSS Inc., Chicago, IL). All data was expressed as mean ± SD (SD: standard deviation). A p value of 0.05 was considered statistically significant.
Results
cVEMP and oVEMP in response to ACS
In the healthy control group, the p13 and n23 latencies and p13-n23 amplitude of cVEMP in response to ACS (1,000 Hz, 5 ms short tone burst) showed symmetry between the sides with the AR of amplitude being 9.9 ± 0.9 %. Likewise, the n10 latency and amplitude of ACS-induced oVEMP recorded in the eye contralateral to the stimulation were symmetrical with an amplitude AR at 15.1 ± 12.1 %. Detailed data were described at the previous paper [6, 9]. We determined the abnormality when each value of the patients exceeded the mean ± 2 SD compare to the control group.
In response to ACS, the majority of patients showed normal cVEMP in the ipsi- (96.7 %) and contralesional SCM (83.4 %) (Table 2). In contrast, ACS induced abnormal oVEMP in 80.0 % of the patients when the involved ear was stimulated. When compared to the control group, the patients showed a significantly greater AR of amplitude (52.0 ± 39.5 vs. 15.1 ± 12.1 %, p < 0.001, t test, Table 3).
oVEMP in response to BCV at the forehead (Fz)
In healthy subjects, oVEMPs recorded from beneath the eyes in response to brief BCV at Fz consist of an initial negativity peaking at about 10 ms after stimulus onset (n10). The mean n1 latency of oVEMPs were symmetric between the right and the left side (mean ± SD, 11.6 ± 1.6 vs. 11.5 ± 2.4 ms) and the average value of the peak-to-peak amplitudes was also approximately equal for both eyes (mean ± SD, 5.4 ± 5.0 uV on the right and 5.5 ± 5.8 uV on the left) with the amplitude AR of 18.4 ± 11.9 % (Table 3).
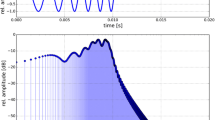
By contrast, in the patient group, BCV at the forehead-induced oVEMPs were mostly asymmetric. In the contralesional eye, a high proportion of patients (22/30, 73.3 %) showed abnormal results in contrast to mostly normal findings in the ipsilesional eye (27/30, 90 %) (Table 3; Fig. 1). Among the asymmetric oVEMP responses, the n10 component was absent (8/22, 36.4 %), markedly reduced (10/22, 45.5 %) or delayed (4/22, 18.2 %), beneath the eye opposite the affected ear (Table 3). The mean ARs for the patient group and control group were 41.9 ± 33 and 18.4 ± 11.9 %, respectively, which was significantly greater in the patient group (p < 0.001).
VEMPs (n10) recorded from a representative patient (Pt. 19, Table 1) with left superior vestibular neuritis (Lt. SVN) in response to stimulation with short tone bursts BCV. Negative potentials are shown as upward deflections. Cervical VEMP to bone vibration at the mastoid processes produced symmetrical responses at both SCM muscles (a). In contrast, oVEMP to vibration at the mastoid process (b) and at the middle forehead (c) showed asymmetric responses with decreased responses at the contralesional eye (the right eye) and robust responses at the ipsilesional eye (the left eye)
cVEMP and oVEMP in response to BCV at the mastoid process
In response to BCV (500-Hz short-tone burst) at the mastoid, healthy controls showed symmetric oVEMP responses on the eye opposite to stimulating mastoid process (Table 3). Mean peak latencies of initial negativity (n10) was symmetric on both eyes (10.9 ± 1.1 ms at the left eye and 10.8 ± 1.8 ms at the right eye), and the mean n10 AR was 23.5 ± 22.8 %. cVEMPs to mastoid BCV also showed symmetric response with mean initial positive peaks of 15.4 ± 0.9 ms at the right SCM and 15.4 ± 1.1 ms at the left SCM, and mean amplitude of 647.7 uV and 509.4 uV at each side with AR of 17.7 %.
In the patient group, BCV at the mastoid process produced inconsistent results of cervical and ocular VEMPs. A large proportion of patients (76.7 %) revealed abnormal oVEMPs on the contralesional eye. In contrast, on the ipsilesional eye, most patients showed normal response (Table 3; Fig. 1). The mean AR of the patients group was also significantly greater than control group (p < 0.01). The cVEMP to mastoid BCV, however, showed normal responses on both sides (Table 2). The asymmetry ratio was also not significant.
Discussion
Our results showed that there were distinct patterns of abnormalities in patients with VN to AC sound and BC vibration at the middle forehead and at each mastoid. Irrespective to the stimulation modalities of ACS or BCV, or their stimulating sites at the forehead or at the mastoid, most VN patients showed abnormal oVEMP and normal cVEMP (Fig. 1; Tables 2, 3).
Electrical stimulation of the nerve from the utricular macula activates the contralateral inferior oblique in cats [24, 25], and neurons in the superior vestibular nerve that originate from the utricular macula are activated by BCV in the guinea pig [26]. Previously, most patients with superior VN showed markedly reduced or absent n10 under the contralesional eye during Fz vibration, including our result [7, 8, 13, 25, 27]. Considering that all utricular afferents course in the superior vestibular nerve and the n10 was reduced in most of our patients, the n10 of the oVEMP to BCV at the forehead (Fz) is probably mediated by the superior vestibular nerve and probably due to activation of utricular receptors. Our data shows the proportion of abnormalities of oVEMP to forehead vibration was similar to that of oVEMP to mastoid vibration (73.3 vs. 76.7 %, Table 3). This suggests that, irrespective to the site of stimulation, bone-conducted vibration appears to stimulate similarly saccular or utricular macular, or both.
It has been known that saccular afferents project to inhibitory neurons in the ipsilateral vestibular nuclei, which in turn project ipsilaterally to spinal motoneurons and inhibit the ipsilateral SCM muscle [29, 30]. Saccular neurons project strongly to cervical SCM muscles whereas utriculo-cervical projections are not as strong [31, 32]. In contrast, utricular afferents have strong projections to the oculomotor system, whereas saccular projections to the oculomotor system are weak and polysynaptic [32, 33]. In healthy subjects, by BC vibration at the mastoid process recorded at the ipsilateral SCM, the response consisted of a short-latency biphasic positive/negative wave followed by a second negativity (Fig. 2a). Our results of VN demonstrated the dissociated results of cervical and ocular VEMPs to BC vibration at the mastoid process, in which oVEMPs showed mostly abnormal on the contralesional eye with contrast to bilaterally symmetric results of cVEMPs (Tables 2, 3; Figs. 1, 2b). This inconsistency in the cervical and ocular VEMPs induced by BCV at the mastoid in patients with VN selectively involving the superior vestibular nerve suggest that the origin of the vestibular nerve afferents of oVEMP differ from those of cVEMP to mastoid BCV. It was suggested that the vestibular end organ primarily excited by the BC vibration at the mastoid was the utricle [3, 28], given the predominant orientation in the horizontal plane [34, 35] and their sensitivity to shearing forces in the interaural direction. However, if BC vibration at the mastoid process only or predominantly stimulates utricle, VN patients with utricular dysfunction would show absence or reduced response on the ipsilesional SCM. Instead of afferent organ specificity to BC vibration at different stimulating sites, both utricle and saccular macula may be highly sensitive to low-frequency vibration irrespective to the site of stimulation. Therefore, unilateral utricular dysfunction due to VN would make little differences on the results of cVEMPs compare to healthy subjects which may reflect ipsilesional responses from saccular macular (Fig. 2b). On the basis of the differential pattern of oculomotor and cervical projection of each otolith, it may indicate that measuring oVEMPs predominantly reflects utricular function, and cVEMPs predominantly reflects saccular function irrespective to stimuli methods (Fig. 2) [12].
Schematic illustrations of ocular and cervical VEMP pathways in healthy subject (a) and in patients with the superior vestibular neuritis (SVN) (b) during short tone burst BCV at the mastoid process. Saccular neurons project strongly to cervical SCM muscles whereas utricular afferents have strong projections to the oculomotor system.Thirty-two healthy subjects (a) showed similar positive/negative shapes of cVEMP on the isilateral SCM and negative/positive wave of oVEMP on the contralateral eye. In patients with SVN with ipsilesional utricular dysfunction (b), vibration on the mastoid leads to generation of inhibitory positive wave on the ipsilesional SCM (cVEMP) while reduced oVEMP on the contralesional eye
In our patients with VN, the AR of cVEMP were about 27 % without a difference between ACS and BCV, which were not statistically different from those in normal controls (Table 2). Likewise, the ARs of oVEMP were similar around 50 % irrespective of the stimulus modalities, but significantly higher than those in normal controls (Table 3). Accordingly, the ARs of oVEMP did not differ among the stimulus modalities.
As shown in our data, the n10 potentials of oVEMP in the VN patients were presented but reduced or delayed potentials on the contralesional eye in a number of patients. It means that VN may affect the entire superior vestibular nerve or more frequently partially affect the superior division of the vestibular nerve. In patients with VN partially involving the superior vestibular nerve, the horizontal and anterior canals and utricular functions are partially impaired, as shown by caloric weakness (not complete paresis) and partially impaired oVEMP. Some patients had symmetrical n10 responses to Fz and mastoid BCV stimulation as well as ACS stimulation. These may be due to that otolithic afferents in the superior nerve were not affected, instead the patient may have had an isolated horizontal canal dysfunction. That being the case, it is necessary to be cautious about interpretation of the results of oVEMP in patients with VN, since there are probably various grades of superior vestibular neuritis so that in some VN patients the utricular nerve may be wholly or partially spared.
In conclusion, this study revealed that dissociated results of cervical and ocular VEMPs in patients with VN, in which cVEMPs were often unaffected, while oVEMPs were often abnormal irrespective to the stimuli modalities, and to the sites of stimuli. Therefore, oVEMP induced by ACS and BCV at the Fz as well as at the mastoid process seems to depend on the integrity of the superior vestibular nerve, possibly due to utricular afferents travelling in it. In contrast, cVEMP by ACS and BCV at the mastoid process reflects the function of the saccular afferents and the inferior vestibular nerve.
References
Welgampola MS (2008) Evoked potential testing in neuro-otology. Curr Opin Neurol 21:29–35
Colebatch JG, Halmagyi GM, Skuse NF (1994) Myogenic potentials generated by a click-evoked vestibulocollic reflex. J Neurol Neurosurg Psychiatry 57:190–197
Curthoys IS (2010) A critical review of the neurophysiological evidence underlying clinical vestibular testing using sound, vibration and galvanic stimuli. Clin Neurophysiol 121:132–144
Kim S, Lee HS, Kim JS (2010) Medial vestibulospinal tract lesions impair sacculo-collic reflexes. J Neurol 257:825–832
Curthoys IS (1987) Eye movements produced by utricular and saccular stimulation. Aviat Space Environ Med 58:192–197
Shin BS, Oh SY, Kim JS et al (2012) Cervical and ocular vestibular-evoked myogenic potentials in acute vestibular neuritis. Clin Neurophysiol 123:369–375
Iwasaki S, McGarvie LA, Halmagyi GM et al (2007) Head taps evoke a crossed vestibulo-ocular reflex. Neurology 68:1227–1229
Iwasaki S, Smulders YE, Burgess AM et al (2008) Ocular vestibular evoked myogenic potentials to bone conducted vibration of the midline forehead at Fz in healthy subjects. Clin Neurophysiol 119:2135–2147
Oh SY, Kim JS, Lee JM et al (2013) Ocular vestibular evoked myogenic potentials induced by air-conducted sound in patients with acute brainstem lesions. Clin Neurophysiol 124:770–778
Murofushi T, Curthoys IS (1997) Physiological and anatomical study of click-sensitive primary vestibular afferents in the guinea pig. Acta Otolaryngol 117:66–72
Murofushi T, Curthoys IS, Gilchrist DP (1996) Response of guinea pig vestibular nucleus neurons to clicks. Exp Brain Res 111:149–152
Murofushi T, Curthoys IS, Topple AN et al (1995) Responses of guinea pig primary vestibular neurons to clicks. Exp Brain Res 103:174–178
Iwasaki S, Chihara Y, Smulders YE et al (2009) The role of the superior vestibular nerve in generating ocular vestibular-evoked myogenic potentials to bone conducted vibration at Fz. Clin Neurophysiol 120:588–593
Curthoys IS, Iwasaki S, Chihara Y et al (2010) The ocular vestibular-evoked myogenic potential to air-conducted sound; probable superior vestibular nerve origin. Clin Neurophysiol 122:611–616
de Burlet HM (1929) Zur vergleichenden Anatomie der Labyrinth innervations. J Comp Neurol 47:155–169
Curthoys IS, Vulovic V (2011) Vestibular primary afferent responses to sound and vibration in the guinea pig. Exp Brain Res 210:347–352
Curthoys IS (2008) The scientific basis of new clinical tests of otoliths function. In: XXV Barany Society Meeting, Kyoto
Curthoys IS, Vulovic V, Sokolic L et al (2012) Irregular primary otolith afferents from the guinea pig utricular and saccular maculae respond to both bone conducted vibration and to air conducted sound. Brain Res Bull 89:16–21
Rosengren SM, Welgampola MS, Colebatch JG (2010) Vestibular evoked myogenic potentials: past, present and future. Clin Neurophysiol 121:636–651
Todd NP, Rosengren SM, Aw ST et al (2007) Ocular vestibular evoked Myogenic potentials (OVEMPs) produced by air- and bone-conducted sound. Clin Neurophysiol 118:381–390
Welgampola MS, Carey JP (2010) Waiting for the evidence: VEMP testing and the ability to differentiate utricular versus saccular function. Otolaryngol Head Neck Surg 143:281–283
Rosengren SM, McAngus Todd NP, Colebatch JG (2005) Vestibular-evoked extraocular potentials produced by stimulation with bone-conducted sound. Clin Neurophysiol 116:1938–1948
Honrubia V (1994) Quantitative vestibular function tests and the clinical examination. Vestibular Rehabilitation. FA Davis Co, Philadelphia, pp 116–119
Suzuki JI, Tokumasu K, Goto K (1969) Eye movements from single utricular nerve stimulation in the cat. Acta Otolaryngol 68:350–362
Manzari L, Tedesco A, Burgess AM, Curthoys IS (2010) Ocular vestibular-evoked myogenic potentials to bone-conducted vibration in superior vestibular neuritis show utricular function. Otolaryngol Head Neck Surg 143:274–280
Curthoys IS, Kim J, McPhedran SK et al (2006) Bone conducted vibration selectively activates irregular primary otolithic vestibular neurons in the guinea pig. Exp Brain Res 175:256–267
Iwasaki S, Smulders YE, Burgess AM et al (2008) Ocular vestibular evoked myogenic potentials in response to bone conducted vibration of the midline forehead at Fz—a new indicator of unilateral otolithic loss. Audiol Neurotol 13:396–404
Govender S, Rosengren SM, Colebatch JG (2012) Vestibular neuritis has selective effects on air- and bone-conducted cervical and ocular vestibular evoked myogenic potentials. Clin Neurophysiol 122:1246–1255
Uchino Y, Sasaki M, Sato H et al (2005) Otolith and canal integration on single vestibular neurons in cats. Exp Brain Res 164:271–285
Kushiro K, Zakir M, Ogawa Y et al (1999) Saccular and utricular inputs to sternocleidomastoid motoneurons of decerebrate cats. Exp Brain Res 126:410–416
Fukushima K, Peterson BW, Wilson VJ (1979) Vestibulospinal, reticulospinal and interstitiospinal pathways in the cat. Prog Brain Res 50:121–136
Uchino Y, Kushiro K (2011) Differences between otolith- and semicircular canal-activated neural circuitry in the vestibular system. Neurosci Res 71:315–327
Rosengren SM, Todd NP, Colebatch JG (2009) Vestibular evoked myogenic potentials evoked by brief interaural head acceleration: properties and possible Origin. J Appl Physiol 107:841–852
Lindeman HH (1973) Anatomy of the otolith organs. Adv Otorhinolaryngol 20:405–433
Tribukait A, Rosenhall U (2001) Directional sensitivity of the human macula utriculi based on morphological characteristics. Audiol Neurotol 6:98–107
Acknowledgments
Dr. S.-Y. Oh is supported by Fund of Biomedical Research Institute, Chonbuk National University Hospital and by research funds of Chonbuk National University in 2012. Dr. J.S. Kim, T.-H. Yang, B.-S. Shin, S.-K. Jeong report no disclosures.
Conflicts of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oh, SY., Kim, JS., Yang, TH. et al. Cervical and ocular vestibular-evoked myogenic potentials in vestibular neuritis: comparison between air- and bone-conducted stimulation. J Neurol 260, 2102–2109 (2013). https://doi.org/10.1007/s00415-013-6953-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-013-6953-8