Abstract
Background
Sudden infant death syndrome (SIDS) causes early infant death with an incidence between 0.5 and 2.5 cases among 1000 live births. Besides central sleep apnea and thermal dysregulation, infections have been repeatedly suggested to be implicated in SIDS etiology.
Methods
To test the risk contribution of common genetic variants related to infection, we genotyped 40 single-nucleotide polymorphisms (SNPs) from 15 candidate genes for association with SIDS in a total of 579 cases and 1124 controls from Germany and the UK in a two-stage case control design.
Results
The discovery-stage series (267 SIDS cases and 303 controls) revealed nominally significant associations for variants in interleukin 6 (IL6) (rs1880243), interleukin 10 (IL10) (rs1800871, rs1800872), and mannose-binding lectin 2 (MBL2) (rs930506), and for several other variants in subgroups. Meta-analyses were then performed in adding genotype information from a genome-wide association study of another 312 European SIDS cases and 821 controls. Overall associations were observed for two independent variants in MBL2: rs930506 in a co-dominant model (odds ratio (OR) = 0.82, p = 0.04) and rs1838065 in a dominant model (OR = 1.27, p = 0.03).
Conclusion
Our study did not replicate published associations of IL10 variants with SIDS. However, the evidence for two independent MBL2 variants in the combined analysis of two large series seems consistent with the hypothesis that infection may play a role in SIDS pathogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden infant death syndrome (SIDS) is the leading cause of death in infants aged between 1 month and 1 year in industrialized countries [1] with an incidence between 0.5 and 2.5 cases among 1000 live births [2]. SIDS is both unforeseeable and unexpected by history, and thereinafter, undertaken investigations usually fail to demonstrate an adequate cause of death [3, 4]. In 1969, Bergman pointed out that SIDS does not depend on a single cause that leads to the death of an infant, but rather on the interaction of several convening risk factors [3]. Therefore, it seems unlikely that SIDS represents one single disease; it rather stands for a collective term describing a heterogeneous clinical condition [5].
Most of the risk factors are established and include environmental triggers on the one hand, such as sleeping in prone position, sleeping environment, overheating, season of the year, and nicotine exposure [6–10]. On the other hand, there are biological factors, which are less well understood and may include genes involved in cardiac function, transmitter function in the brainstem, regulation of respiratory function, and the immune system [11–15].
One research field of interest with regard to SIDS is the medullary serotonergic (5-HT) network in the brainstem, where serotonin is an important mediator of interactions between the nervous and immune system [16–18]. In this context, Vege et al. pointed out that the brain might be the target organ for a lethal mechanism initiated by an immune reaction characterized by increased IL6 levels in cerebrospinal fluid (CSF) of SIDS infants and infants that died from infectious diseases [17, 18]. Rognum et al. hypothesized that IL6 binds to IL6 receptors on 5-HT neurons and that this might result in a downstream effect [16]. From postmortem examination reports, over 40 % of infants affected by SIDS seem to show signs of slight infection during the 2 weeks preceding death [19, 20]. Especially upper respiratory tract infections are a common finding of SIDS autopsies [21]. Other inflammatory processes often seem to be located in the digestive tract, nervous system and blood [1], and there is evidence that a rapid, uncontrolled release of inflammatory mediators in response to an infection or their toxins could be a causative factor of SIDS [22]. The above-mentioned findings suggest that at least a subset of the infants that later die of SIDS are more vulnerable to simple infections and that an activated immune system may be involved in SIDS pathogenesis [5]. Based on the indication of immune response involvement in at least some SIDS cases [23, 24], we hypothesized that polymorphisms located in genes encoding some of the key modulators of the immune system might lead to an increased tendency to infections and thus to a more vulnerable infant with an increased liability to die of SIDS. Although in previous studies some selected genes related to inflammation were already tested for association with SIDS, e.g., IL-10 [25–27] or IL-6 [16], a comprehensive study on a broad scope of loci is missing. Therefore, we investigated 579 SIDS cases and 1124 controls for 40 polymorphisms in 15 candidate genes involved in immunomodulatory mechanisms in two-stage case/control design.
Patients and methods
Patients
The SIDS group investigated at Hannover Medical School includes 267 Caucasian infants from Germany (163 males and 104 females; median age at death, 99 days; age range, 1–365 days). Information on sleeping position, date of birth, and death were obtained from the postmortem examination reports. The control group includes samples from 303 healthy Caucasian children and adults from Hannover and Göttingen (167 males and 136 females) obtained from consenting volunteers or routine paternity testing. The cohort comprised 145 infants, aged between 8 and 12 months (and thus past the peak prevalence of SIDS), 63 girls and 82 boys. Due to anonymization of the samples, an exact mean age could not be given.
The replication sample consisted of 365 SIDS cases (age range 8–365 days) with both autopsy information and biosamples available. Of those, 317 originated from the multi-center German study on sudden infant death (GeSID) [28]; the other 48 cases were recruited and autopsied in the UK at the Sheffield Children’s Hospital (SCHC) [29]. Both GeSID and SCHC used a standardized autopsy protocol, and only infants suffering from sudden unexplained death where no causes of death could be determined postmortem were classified as SIDS. For the replication sample, no information concerning sex and ethnicity was available due to anonymization. A total of 823 healthy controls (425 males and 398 females) from the Kooperative Gesundheitsforschung in der Region Augsburg (KORA) F4 study [30] were used. All centers providing case data obtained the approval of their local medical ethics committees. All participants in KORA have given written informed consent and the Bayerische Landesärztekammer approved the studies.
The cases included in the Hannover and replication samples can be counted among the subclassification “Category II SIDS” [31].
Genetic analyses
Our selection procedure and two-stage case/control design is illustrated in Online Resource 1. Discovery (first-stage genotyping) was performed in the Hannover cohort. Genomic DNA from blood, saliva, or thymus tissue samples had been extracted using the QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. Forty-six SNPs in 16 genes associated previously with variable immunological responses in different diseases such as sepsis, septic shocks, or toxic shock-like reactions were finally genotyped after a selection based on literature search using PubMed keywords “sepis, infection, cytokine polymorphisms, interleukin, singe nucleotide polymorphism, SNP, gene polymorphism” (Online Resource 2). For genotyping, allele-specific SNPtype assays were run on 192.24 Genotyping Dynamic Arrays using the Biomark EP1 platform (Fluidigm Corp., South San Francisco, CA, USA). FAM and HEX-labeled primers, detecting either one allele of the respective SNP, were designed by Fluidigm. Genotyping experiments were performed as described [32]. For internal quality control, 61 samples (10.7 %) were run in duplicates. FAM and HEX signals were detected after each PCR cycle, and the resulting data were analyzed using the Fluidigm SNP Genotyping Analysis software version 4.
Replication (second-stage genotyping) was performed using GeSID [28] and SCHC [29] as cases and KORA F4 [30] as controls. All cases of GeSID and SCHC were genotyped on Illumina HumanHap660W-Quad BeadChips (657,366 markers) following standard protocols. For the GWAS, genotypes were called using Illumina’s Bead Studio software. Controls from KORA F4 were genotyped on the Illumina HumanHap550-Quad+ BeadChip (539,741 markers), and genotypes were called also using Bead Studio. Due to the different genotyping platforms used for cases and controls, we performed step-wise merging of the genotype data. GeSID and SCHC data, both obtained with the 660 W-Quad, could be directly merged; exclusion of monomorph markers and discordant missing markers resulted in 561,490 remaining markers. Merging with KORA genotypes and the same filtering steps yielded a set of 505,759 markers available in all three cohorts. A total of 312 cases (278 from GeSID, 34 from SCHC) and 821 controls met quality control criteria (individual call rate ≥95 %, genotype call rate ≥98 %, MAF≥5 %, PHWE ≥1e-5). Prephasing with ShapeIt2 followed by imputation using IMPUTE2 (http://mathgen.stats.ox.ac.uk/impute/impute_v2.html) against reference data from 1000genomes (http://www.1000genomes.org/) phase 1 version 3 genotypes resulted in the final marker set of 4,634,138 polymorphisms with info-score ≥0.8. Of the 40 SNPs from discovery stage, 11 were genotyped and 29 imputed in the replication sample.
Data analyses
In the Hannover cohort, genotypes were drawn from the cluster plots after manual review, and Hardy–Weinberg equilibrium was tested using a χ2 test. SNPs with poor clustering (n = 6) were omitted from further data analysis. Statistical analysis for the remaining 40 SNPs was performed under three different models with Sequence Variation Suite 7.0 (Golden Helix Inc.). A basic allelic test was employed to compare allele frequency distribution between groups; furthermore, a Cochrane–Armitage trend test for genotype distribution under an additive risk model was applied. In addition, homozygous major and minor allele genotype distributions were separately compared between SIDS cases and controls under dominant and recessive models, respectively.
For stratified analyses, samples were grouped into four different subcategories according to parameters that are known to increase the risk of SIDS as previously demonstrated [33, 34]. These include (i) gender (two strata: males only (SIDS, n = 159; controls, n = 167) and females only (SIDS, n = 94; controls, n = 74)), (ii) age at death (2–4 months (n = 84) vs all controls), (iii) sleeping in prone position (n = 56, vs all controls), and (iv) a season category as a proxy for outside temperature at the time of death (four strata: spring (n = 61), summer (n = 56), autumn (n = 66), and winter (n = 65); each vs all controls).
Logistic regression analyses were performed to fit models including the covariates gender, age group (six categories), season (four categories), and sleep position, and odds ratios and z-values were obtained by STATA12. Selected covariates were also included in a case-only analysis using logistic regression.
Haplotype analysis was performed using Haploview 4.0 to detect and investigate SNP haplotypes that stood out in this study. This analysis was limited to genes that harbored more than one candidate variant, specifically IL6, IL10, IL10RA, and MBL2. Linkage disequilibrium plots and pairwise LD were also obtained from the Single Nucleotide Polymorphism Annotator (SNiPA, http://snipa.helmholtz-muenchen.de/snipa/) [35].
Meta-analyses were performed in adding genotype information from a replication sample that included all candidate loci studied here for 312 SIDS cases and 821 healthy controls. Eleven variants had been genotyped directly, and 29 variants had been imputed. Further meta-analyses for IL6 and IL10 included published results from a literature search using the keywords “interleukin 6 and SIDS,” “IL6 and SIDS,” “interleukin 10 and SIDS,” and “IL10 and SIDS” in PubMed (http://www.ncbi.nlm.nih.gov/pubmed, approached on Aug 9, 2014).
Results
In the discovery sample, the Hannover SIDS study, a total of 570 individuals (267 SIDS and 303 controls) were successfully genotyped for 40 candidate variants and were subjected to data analysis. Call rates were above 95 % for all 40 SNPs. Concordance rates were 100 % for 32 SNPs, 97.9 % for four SNPs, and 95.8 % for four SNPs. All 40 variants were tested for their association with SIDS under recessive, dominant, and co-dominant models (Online Resource 3). Table 1 summarizes the results for those variants at p < 0.05 under at least one model (Table 1). Online Resource 4 includes the unfavorable genotypes for the significant SNPs in this study. Main analyses suggested that, prior to correction for multiple testing, the two SNPs rs1800871 (IL10*c.-854C/T, also known as -819C/T) and rs1800872 (IL10*-c.627A/C, also known as -592A/C) were associated with SIDS, with the strongest evidence obtained under an additive model (p = 0.002). Furthermore, rs1880243 in IL6 and rs930506 in MBL2 were associated with SIDS under a recessive model (p = 0.014 for rs1880243 and 0.006 for rs930506, respectively).
In stratified analyses, 16 SNPs were nominally associated at a significance level of α = 0.05 in any of the subgroups (Table 1). Eight SNPs, including rs1800871 and rs1800872 in IL10, showed associations in more than one subcategory, while eight other SNPs were significant for single subgroups. In the prominent subcategory “winter,” two independent SNPs rs4358188 and rs5743507 in BPI (bactericidal/permeability-increasing protein) showed nominally significant associations with SIDS (Table 1).
To corroborate the findings, we also performed case–control and case-only studies using logistic regression analyses with gender as covariate, and age, season, or sleeping position as stratifying variables in cases (Online Resource 5). The case–control studies with gender as a covariate confirmed nominally significant associations for all three IL10 variants. Stratified case-only analyses revealed nominally significant associations in subgroups for variants in IL1B, IL6, IL10RA, and ACE (Online Resource 5). However, none of these findings remained statistically significant after FDR correction for multiple testing.
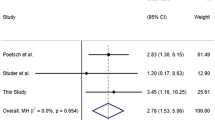
We sought to validate the genotyping results further in a meta-analysis with other data from a second case–control series. From the replication dataset, we excerpted genotype data for all 40 candidate variants (11 genotyped, 29 imputed) and included both studies into Mantel–Haenszel meta-analyses under three different models (dominant, recessive, additive). While the previous associations with IL6 and IL10 variants did not replicate in the second case–control set, borderline evidence of association (p = 0.05) was obtained for rs11216666 in IL10RA under a co-dominant model (odds ratio (OR) 1.20, 95 % confidence interval (95%CI) 1.00; 1.45), and for rs1891320 (phospholipase A2, group IIA) and rs1554973 (Toll-like receptor 4) under the recessive model (Online Resource 6). Interestingly, the strongest associations in the meta-analysis were obtained for two independent variants in the mannose-binding lectin 2 gene, MBL2, with rs930506 in a co-dominant model (OR 0.82, 95%CI 0.67; 0.99, p = 0.04) (Fig. 1) and rs1838065 in a dominant model (OR 1.27, 95%CI 1.03; 1.57, p = 0.03) (Fig. 2). The first result corroborated the association of rs930506 with SIDS in our initial series, and the second result supported an association of rs1838065 with SIDS in the replication sample. There was some evidence for heterogeneity between the studies for rs1838065 (I 2 = 80.8 %, p het = 0.02) but not for rs930506 (I 2 = 0.0 %, p het = 0.47). In regard that two out of four genotyped MBL2 variants showed evidence for association, we performed a haplotype analysis including all four variants (Table 2). The most significant MBL2 haplotype in the replication sample, GGCT, remained associated with SIDS in a fixed-effects meta-analysis of both case–control studies (OR 1.19, 95%CI 1.02; 1.38, p = 0.03) (Fig. 3).
Meta-analysis rs930506 (co-dominant). Mantel–Haenszel meta-analyses with data from Hannover and replication sample under a co-dominant model (OR 0.815, 95%CI 0.670; 0.991, p = 0.041). n cases = 579, n controls = 1124. OR, odds ratio; 95%CI, 95 % confidence interval; MHH, Hannover series at Hannover Medical School
Meta-analysis rs1838065 (dominant). Mantel–Haenszel meta-analyses with data from Hannover and replication sample under a dominant model (OR 1.269, 95%CI 1.028; 1.567, p = 0.027). There was some evidence for heterogeneity between the studies for rs1838065 (p het = 0.022). n cases = 579, n controls = 1124. OR, odds ratio; 95%CI, 95 % confidence interval; MHH, Hannover series at Hannover Medical School
Meta-analysis for MBL2 risk haplotype. Fixed-effects meta-analysis of both case–control studies for the most significant MBL2 haplotype in the replication sample, GGCT, which remained significant (OR 1.19, 95%CI 1.02; 1.38, p = 0.03). n cases = 579, n controls = 1124. Risk haplotype, GGCT. OR, odds ratio; 95%CI, 95 % confidence interval; MHH, Hannover series at Hannover Medical School
Discussion
Because SIDS etiology is known to be linked to infections in at least some cases and immune response has been shown to be genetically influenced, it was tempting to speculate that some of the variants are also associated with SIDS. Therefore, we have investigated 40 candidate gene variants in key regulators of the immune system for association to SIDS in the two largest SIDS case–control series available from Germany. All selected gene variants had been associated previously with variable immunological responses in different diseases such as sepsis, septic shocks, or toxic shock-like reactions. We used a two-stage design, followed by a combined analysis of 579 cases and 1124 controls. At a power of 80 %, this study should have been able to detect main effects larger than OR 1.38 for a minor allele frequency (MAF) of 0.1, OR 1.28 for MAF 0.2, or OR 1.25 for MAF 0.3, respectively.
Although the initial study from Hannover showed evidence for an overall association of IL6 and IL10 variants with SIDS, these findings did not replicate in the second series of similar size, suggesting that they may have been spurious findings. A meta-analysis of all published studies with the two large series reported here did not confirm any association of single IL6 variant rs1800795 or IL10 variants rs1800871, rs1800872, and rs1800896, or the respective haplotypes, with SIDS (data not shown). It is still possible that these variants play a role in subgroups, which have not been addressable in all studies.
In the mannose-binding lectin 2, MBL2, rs930506 was associated with SIDS in the Hannover series, and rs1838065 was associated with SIDS in the replication study. Both variants are not highly correlated with each other (r 2 = 0.14). In the combined analyses of both studies, rs930506 remained significant in a co-dominant model (p = 0.04) and rs1838065 in a dominant model (p = 0.03). Although these results do not persist after correction for multiple testing, nonetheless the respective SNPs may indicate a biological relevance for the etiology of SIDS and are therefore worthy of discussion.
As a part of the acute phase protein family, MBL2 is responsible for the activation of the complement system via the lectin pathway. It is synthesized in the liver and circulates to bind to carbohydrates on microbial surfaces such as mannose, mannosamine, and hexosamine, to necrotic and apoptotic cells. MBL2 has a crucial role in preventing and terminating an infection. Certain polymorphisms in MBL2 can impair MBL function and have been proposed to increase susceptibility to infectious diseases [36]. We are not aware of previous genetic studies of MBL2 polymorphism with SIDS. Kilpatrick et al. [37] have reported that mean MBL2 values were higher in their SIDS group than in controls, supporting a role for infection and/or polymorphism in SIDS. However, their study was small (46 cases and 26 controls), and since it investigated serum samples, not genetic variants, it cannot be directly compared with ours. It may also be notable that, according to our study, the risk conferred by MBL2 variant rs930506 was significant in males. As mentioned before and according to Moon et al. [1], gender seems to be an important risk factor. Boys seem to be more vulnerable and more likely to die of SIDS than girls. According to postmortem examination reports, 60 % of the infants that died because of SIDS are males [1].
Stratified analyses in the Hannover series revealed suggestive associations for additional variants in subgroups. In the prominent subcategory “winter,” the SNPs rs4358188 (bactericidal/permeability-increasing protein, BPI) and rs5743507 (BPI) showed significant associations with SIDS. Both variants are only weakly correlated (r 2 = 0.16). It has been observed that 75 % of SIDS deaths occur during the cold season. In addition, the winter season seems to be associated with an increased number of respiratory infections and over 40 % of infants that later die of SIDS seem to show signs of slight infections during the 2 weeks preceding death [19, 20]. BPI plays a central role in host defense against Gram-negative bacteria and their endotoxins due to its function in antimicrobial and endotoxin-neutralizing reactions [38, 39].
In summary, this large two-stage case–control study did not indicate a single variant in the chosen immunological candidate genes that exerts a strong main effect on the predisposition toward SIDS or withstands the correction for multiple testing. Suggestive evidence was obtained for an association of independent genetic variants in MBL2. If our findings can be confirmed in validation studies, such results may provide new directions for targeted research in SIDS etiology and contribute to a better understanding of molecular risk factors for SIDS and ultimately lead to an improved prediction and prevention of fatal outcomes in the future.
References
Moon RY, Horne RSC, Hauck FR (2007) Sudden infant death syndrome. Lancet 370:1578–1587. doi:10.1016/S0140-6736(07)61662-6
Publikation - Gesundheit - Ergebnisse der Todesursachenstatistik für Deutschland - Ausführliche vierstellige ICD10-Klassifikation - 2013 - Statistisches Bundesamt (Destatis)
Beckwith JB (1970) Discussion of terminology and definition of sudden infant death syndrome. Univ. Washingt. Press
Willinger M, James LS, Catz C (1991) Defining the sudden infant death syndrome (SIDS): deliberations of an expert panel convened by the National Institute of Child Health and Human Development. Pediatr Pathol 11:677–684
Courts C, Madea B (2010) Genetics of the sudden infant death syndrome. Forensic Sci Int 203:25–33. doi:10.1016/j.forsciint.2010.07.008
Stanley FJ, Byard RW (1991) The association between the prone sleeping position and sudden infant death syndrome (SIDS): an editorial overview. J Paediatr Child Health 27:325–328
Kleemann WJ, Schlaud M, Poets CF et al (1996) Hyperthermia in sudden infant death. Int J Leg Med 109:139–142
Blair PS, Fleming PJ, Bensley D et al (1996) Smoking and the sudden infant death syndrome: results from 1993-5 case-control study for confidential inquiry into stillbirths and deaths in infancy. Confidential Enquiry into Stillbirths and Deaths Regional Coordinators and Researchers. BMJ 313:195–198
Hauck FR, Herman SM, Donovan M et al (2003) Sleep environment and the risk of sudden infant death syndrome in an urban population: the Chicago infant mortality study. Pediatrics 111:1207–1214. doi:10.1542/peds.111.5.S1.1207
Douglas AS, Allan TM, Helms PJ (1996) Seasonality and the sudden infant death syndrome during 1987-9 and 1991-3 in Australia and Britain. BMJ 312:1381–1383
Wang DW, Desai RR, Crotti L et al (2007) Cardiac sodium channel dysfunction in sudden infant death syndrome. Circulation 115:368–376. doi:10.1161/CIRCULATIONAHA.106.646513
Opdal SH, Opstad A, Vege Å̊, Rognum TO (2003) IL-10 gene polymorphisms are associated with infectious cause of sudden infant death. Hum Immunol 64:1183–1189. doi:10.1016/j.humimm.2003.08.359
Kinney HC (2009) Brainstem mechanisms underlying the sudden infant death syndrome: evidence from human pathologic studies. Dev Psychobiol 51:223–233. doi:10.1002/dev.20367
Rand CM, Patwari PP, Carroll MS, Weese-Mayer DE (2013) Congenital central hypoventilation syndrome and sudden infant death syndrome: disorders of autonomic regulation. Semin Pediatr Neurol 20:44–55. doi:10.1016/j.spen.2013.01.005
Klintschar M, Reichenpfader B, Saternus K-S (2008) A functional polymorphism in the tyrosine hydroxylase gene indicates a role of noradrenalinergic signaling in sudden infant death syndrome. J Pediatr 153:190–193. doi:10.1016/j.jpeds.2008.02.032
Rognum IJ, Haynes RL, Vege A et al (2009) Interleukin-6 and the serotonergic system of the medulla oblongata in the sudden infant death syndrome. Acta Neuropathol 118:519–530. doi:10.1007/s00401-009-0535-y
Vege A, Rognum TO, Scott H et al (1995) SIDS cases have increased levels of interleukin-6 in cerebrospinal fluid. Acta Paediatr 84:193–196
Vege A, Rognum TO, Anestad G (1999) IL-6 cerebrospinal fluid levels are related to laryngeal IgA and epithelial HLA-DR response in sudden infant death syndrome. Pediatr Res 45:803–809. doi:10.1203/00006450-199906000-00004
Hoffman HJ, Damus K, Hillman L, Krongrad E (1988) Risk factors for SIDS. results of the national institute of child health and human development SIDS cooperative epidemiological study. Ann N Y Acad Sci 533:13–30
Wilson CE (1999) Sudden infant death syndrome and Canadian Aboriginals: bacteria and infections. FEMS Immunol Med Microbiol 25:221–226
Heininger U, Kleemann WJ, Cherry JD (2004) A controlled study of the relationship between Bordetella pertussis infections and sudden unexpected deaths among German infants. Pediatrics 114:e9–e15. doi:10.1542/peds.114.1.e9
Blackwell CC, Weir DM, Busuttil A (1995) Infectious agents, the inflammatory responses of infants and sudden infant death syndrome (SIDS). Mol Med Today 1:72–78
Blackwell CC, Moscovis SM, Gordon AE et al (2004) Ethnicity, infection and sudden infant death syndrome. FEMS Immunol Med Microbiol 42:53–65. doi:10.1016/j.femsim.2004.06.007
Blackwell CC, Moscovis SM, Gordon AE et al (2005) Cytokine responses and sudden infant death syndrome: genetic, developmental, and environmental risk factors. J Leukoc Biol 78:1242–1254. doi:10.1189/jlb.0505253
Opdal SH, Rognum TO (2011) Gene variants predisposing to SIDS: current knowledge. Forensic Sci Med Pathol 7:26–36. doi:10.1007/s12024-010-9182-9
Summers AM, Summers CW, Drucker DB et al (2000) Association of IL-10 genotype with sudden infant death syndrome. Hum Immunol 61:1270–1273. doi:10.1016/S0198-8859(00)00183-X
Korachi M, Pravica V, Barson AJ et al (2004) Interleukin 10 genotype as a risk factor for sudden infant death syndrome: determination of IL-10 genotype from wax-embedded postmortem samples. FEMS Immunol Med Microbiol 42:125–129. doi:10.1016/j.femsim.2004.06.008
Findeisen M, Vennemann M, Brinkmann B et al (2004) German study on sudden infant death (GeSID): design, epidemiological and pathological profile. Int J Leg Med 118:163–169. doi:10.1007/s00414-004-0433-8
Prtak L, Al-Adnani M, Fenton P et al (2010) Contribution of bacteriology and virology in sudden unexpected death in infancy. Arch Dis Child 95:371–376. doi:10.1136/adc.2009.162792
Holle R, Happich M, Lowel H et al (2005) KORA--a research platform for population based health research. Gesundheitswesen 67(Suppl 1):S19–S25. doi:10.1055/s-2005-858235
Krous HF, Beckwith JB, Byard RW et al (2004) Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and diagnostic approach. Pediatrics 114:234–238. doi:10.1542/peds.114.1.234
Läer K, Dörk T, Vennemann M et al (2015) Polymorphisms in genes of respiratory control and sudden infant death syndrome. Int J Legal Med 129:977–984. doi:10.1007/s00414-015-1232-0
Läer K, Vennemann M, Rothämel T, Klintschar M (2014) Mitochondrial deoxyribonucleic acid may play a role in a subset of sudden infant death syndrome cases. Acta Paediatr 103:775–779
Läer K, Vennemann M, Rothämel T, Klintschar M (2013) Association between polymorphisms in the P2RY1 and SSTR2 genes and sudden infant death syndrome. Int J Legal Med 127:1087–1091. doi:10.1007/s00414-013-0887-7
Arnold M, Raffler J, Pfeufer A et al (2015) SNiPA: an interactive, genetic variant-centered annotation browser. Bioinformatics 31:1334–1336. doi:10.1093/bioinformatics/btu779
Bouwman LH, Roep BO, Roos A (2006) Mannose-binding lectin: clinical implications for infection, transplantation, and autoimmunity. Hum Immunol 67:247–256. doi:10.1016/j.humimm.2006.02.030
Kilpatrick DC, James VS, Blackwell CC et al (1998) Mannan binding lectin and the sudden infant death syndrome. Forensic Sci Int 97:135–138
Marra MN, Wilde CG, Griffith JE et al (1990) Bactericidal/permeability-increasing protein has endotoxin-neutralizing activity. J Immunol 144:662–666
Schultz H, Weiss JP (2007) The bactericidal/permeability-increasing protein (BPI) in infection and inflammatory disease. Clin Chim Acta 384:12–23. doi:10.1016/j.cca.2007.07.005
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The local ethics committee at Hannover Medical School has approved this study.
Statement of financial support
Intramural funding from Hannover Medical School and Financial assistance from the Foundation for the study of Infant Deaths (FSID), 11 Belgrave Road, London SW1V 1RB UK is kindly acknowledged.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Online Resource 1
Study design. From 65 intended SNPs, 46 were successfully designed as a SNPtype assay. Six of them dropped out of the study because of poor clustering. Accordingly, 40 SNPs were part of the discovery and replication stage. A list of all 65 SNPs with rs codes is provided in the Study design. QC, Quality control (PDF 148 kb)
Online Resource 2
(PDF 104 kb)
Online Resource 3
(PDF 72 kb)
Online Resource 4
(PDF 73 kb)
Online Resource 5
(PDF 79 kb)
Online Resource 6
(PDF 103 kb)
Rights and permissions
About this article
Cite this article
Fard, D., Läer, K., Rothämel, T. et al. Candidate gene variants of the immune system and sudden infant death syndrome. Int J Legal Med 130, 1025–1033 (2016). https://doi.org/10.1007/s00414-016-1347-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-016-1347-y