Abstract
Sudden infant death syndrome (SIDS) is a multifactorial syndrome and assumingly, among other mechanisms, a deficit in respiratory control leads to a failure of arousal and autoresuscitation when the child is challenged by a stressful homeostatic event, e.g., hypoxia. We hypothesize that genetic polymorphisms involved in respiratory control mediated in the medulla oblongata contribute to SIDS. Therefore, a total of 366 SIDS cases and 421 controls were genotyped for 48 SNPs in 41 candidate genes. Genotyping was performed using Fluidigm nanofluidic technology. Results were obtained for 356 SIDS and 406 controls and 38 SNPs. After correction for multiple testing, one SNP retained a nominally significant association with seasonal SIDS: rs1801030 in the phenol sulfotransferase 1A1 gene (subgroup: death occurring during summer). A borderline association could be also observed for rs563649 in the opioid receptor μ1 gene in a recessive model (subgroup: death occurring during autumn). As a conclusion, although these data suggest two SNPs to be associated with different subgroups of SIDS cases, none of them can fully explain the SIDS condition, consistent with its multifactorial etiology. Given the great complexity of respiratory control and our initial findings reported here, we believe it is worthwhile to further investigate genes involved in the respiratory system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden infant death syndrome (SIDS) is the leading cause of death in infants aged between 1 month and 1 year with a mean incidence rate of approximately five per 10,000 live births in developed countries [1]. A genetic basis for SIDS has been considered for long and genes investigated so far are involved either in early embryologic development, cardiac function, transmitter function in the brainstem, or regulation of the immune system and respiratory function [2–7]. The so-called brainstem hypothesis states that an important subset of SIDS deaths occurs as the result of a failure of protective responses (e.g., arousal reaction) to homeostatic stressors, such as hypotension or prolonged apnea, which primarily occur during sleep [8]. Short physiological periods of apnea are quite common in sleeping newborns; long-lasting apneas, however, are a sign of either a disturbed energy provision of the brainstem, or the result of a pathological or immature respiratory network [9].
The respiratory network located in the medulla oblongata is responsible for rhythmogenesis [10]. Various neuromodulators control the activity of the rhythm-generating network and therefore, serotonin, substance P, noradrenalin, and others play a crucial role by intervening in the many synaptic interactions between respiratory neurons [11].
Within the respiratory network, acetylcholine acts on nicotinic (α4β2) or muscarinic (M2 and M3) receptors. While M3 receptors are excitatory and positively coupled to a Gq/11 protein, M2 receptors are inhibitory and suppress adenylyl cyclase C [12]. Substance P has primarily excitatory effects and binds to three main receptor types: NK1, NK2, and NK3 receptors. NK1 receptors are located within the preBötC region, and they are coupled to excitatory Gq/11 protein, and they modulate Na+, Ca2+, and K+ channels [13]. Further, excitatory transmitters are cholecystokinin, acting on CCK1 receptors within one or more medullary or pontine respiratory groups, thyrotropin-releasing hormone, which induces bursting properties in neurons of the Ncl. tractus solitarius, and histamine, acting primarily on H1 receptors [14–16]. Primarily, inhibitory modulators are opioids and somatostatin [17]. While the mechanisms of action of somatostatin are not fully understood, activation of opioid receptors κ and μ depresses the frequency of respiratory activity [18, 19]. Dopamine, serotonin, and noradrenaline are examples of transmitters that exert both inhibitory and excitatory effects by acting on different receptors. Although the biphasic modulation of the respiratory rhythm seems to be best explained by the activation of 5-HT2A (excitatory), 5-HT2C (excitatory), and 5-HT1A (inhibitory), the natural conditions activating these receptors remain to be elucidated [20]. However, the release of different modulators is obviously highly regulated and coordinated by the respiratory system, and neuromodulators with apparently similar effects may have complex modulatory consequences when simultaneously released [11].
We hypothesize that polymorphisms located in genes coding for some of the key modulators of respiratory control might present a genetic background in the etiology of SIDS that might lead to a decreased ability in handling stressful respiratory events. Thus, we opted to type 366 SIDS cases and 421 control cases for 48 polymorphisms in 41 candidate genes associated with respiratory control (see Table 1).
Materials and methods
Patients and methods
The SIDS group comprised 366 Caucasian infants (229 males and 137 females, mean age at death 130 days, age range 5–365 days) from Germany who died unexpectedly in their first year of life, and whose deaths remained without a definite cause despite thorough post mortem examination. The samples were drawn from case collections in Hannover and Göttingen. Information on sleeping position, date of birth, and death were obtained from the respective autopsy report. The control group comprised samples from 421 healthy German Caucasian children and adults (228 males and 193 females) obtained from consenting volunteers and routine paternity testing. The cohort comprised 134, aged between 8 and 12 months (and thus past the peak prevalence of SIDS), 56 girls and 78 boys. Due to anonymization of the samples, an exact mean age could not be given, but most children were in the lower half of this range. When comparing the typing results for these healthy children and the 287 adults in the control cohort, no significant differences were noted. This study has been approved by the local ethics committee at Hannover Medical School.
Genomic DNA was extracted from either blood, saliva, or tissue samples using the QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions as described (@). For genotyping, allele-specific SNPtype assays were run on 192.24 Dynamic Arrays using the Biomark EP1 platform (Fluidigm Corp., South San Francisco, CA, USA) [21]. Primers (FAM and HEX-labeled, detecting either one allele of the respective SNP) used in this study were designed by Fluidigm (see supplementary table 1). Specific target amplification (STA) of 190 samples and two non-template controls (NTCs) per array was performed using 2× Multiplex PCR Master Mix (Qiagen, Hilden, Germany), 10× SNPtype STA Primer Pool, PCR-certified water and genomic DNA. Thermocycling conditions on a 7500 Real-Time PCR System (Life Technologies, Darmstadt, Germany) were as follows: 15 s at 95 °C followed by 14 cycles of 15 s at 95 °C, and 4 min at 60 °C. STA products were diluted 50-fold with 1× TE buffer. Before loading the biochip, both 10× assay mix and sample mix were prepared: The 10× assay mix comprised of 2 μl 2× Assay Loading Reagent (Fluidigm), 1.2 μl PCR-certified water, and 1 μl SNPtype assay mix (Fluidigm), whereas the sample mix contained 2.25 μl 2× Fast Probe Master Mix (Biotium, Hayward, CA, USA), 0.225 μl SNPtype 20× Sample Loading Reagent (Fluidigm), 0.075 μl SNPtype Reagent (Fluidigm), 0.027 μl ROX (Invitrogen, Carlsbad, CA, USA), 0.048 μl PCR-certified water, and 2 μl STA product (1:50). Each array was loaded with 190 samples, two NTCs and 24 SNPtype assays: 3 μl of each assay and sample mix was pipetted into separate inlets on the frame of the Dynamic Array chip following the manufacturer’s instructions. Samples and assays were mixed using the IFC Controller RX (Fluidigm). The Dynamic Array was then subjected to thermocycling on the Fluidigm Biomark EP1 platform (Fluidigm), following the default PCR protocol. FAM and HEX signals were detected after each PCR cycle, and to obtain genotype calls, resulting data were analyzed using the Fluidigm SNP Genotyping Analysis software version 3. Eighty samples were run in duplicates for internal quality control.
Data analysis
Cluster plots were manually inspected, and SNPtype assays with poor clustering or call rates below 90 % were eliminated from the study (one assay). Further, Hardy-Weinberg equilibrium was tested using χ 2 tests, and SNPs with significant deviations from HWE were omitted (six assays). Finally, assays that turned out to be monomorphic in our study population were excluded from further data analysis (three assays). Twenty-five samples had to be excluded from the study, because of either unmet inclusion criteria of the SIDS group or controls, or genotyping failures (after second genotyping). Statistical analysis was then performed with Sequence Variation Suite 7.0 (Golden Helix Inc.) on unambiguous results for 38 SNPs. Genetic association between single loci and SIDS was calculated using χ 2 test for allele frequency distribution as a basic allelic test and using a Cochrane-Armitage trend test for genotype distribution under an additive risk model. Finally, homozygous major allele genotypes or homozygous minor allele genotypes were compared between cases and controls under a dominant or recessive model, respectively. The accumulation of type I error due to multiple testing was addressed using false discovery rate (FDR) correction. In addition to the main analysis, samples were stratified into 4 different subcategories according to parameters known to increase the risk of SIDS, including gender (four test models: females only (SIDS n = 124, controls n = 187); female SIDS cases versus all controls; males only (SIDS n = 215, controls n = 219); and male SIDS cases versus all controls), age at death (four test models: 0–4 months (n = 195); 4–8 months (n = 87); 8–12 months (n = 48); and 2–4 months (n = 112); each versus all controls), sleeping in the prone position (n = 92 versus all controls), and a season category as a proxy for outside temperature at the time of death (six test models: spring (n = 87), summer (n = 75), autumn (n = 72), winter (n = 97), warm season (spring + summer; n = 162), and cold season (autumn + winter; n = 169, all were tested versus all controls).
Results
A total of 762 samples (356 SIDS and 406 controls) were successfully genotyped for 38 loci and were subjected to data analysis. We achieved a call rate above 96 % from the 762 samples genotyped for 38 SNPs. Concordance rates were 100 % for 30 SNPs and 98.7 % for eight SNPs.
In the stratified analysis, none of the SNPs showed a significant main effect (see supplementary table 1), but 21 SNPs fell below a significance level of α = 0.05 in any one of the four subgroups (Table 2). After correction for multiple testing, one SNP remained with a significantly different genotype distribution between SIDS and controls: the rare G allele of SNP rs1801030, encoding the missense variant p.M223V in the phenol sulfotransferase 1A1 gene, which was found in three cases of the SIDS “summer” subgroup (both, additive model and dominant model: χ 2/Armitage FDR = 0.004), but neither in any other SIDS subgroups nor in the control group. The SNP rs563649, located in the 5′-untranslated region (5′-UTR) of the opioid receptor μ1 gene, showed borderline significance regarding rare homozygotes (T/T) in the SIDS “autumn” subgroup compared to controls (recessive model, χ 2 FDR = 0.049, OR = 16.4 (95% CI = 1.68–160)). Two further SNPs gave significant results at α = 0.05 in more than three SIDS subgroups before correction for multiple testing: SNP rs7735184 (subgroups “males only”, “males vs. all controls”, “0–4 months”, and “prone sleep position”) and SNP rs7832552 (subgroups “2–4 months”, “0–4 months”, “winter”, and “autumn + winter”). These findings did not remain statistically significant after FDR correction, but may still indicate a biological relevance for the etiology of SIDS.
Discussion
A deficit in brainstem-mediated respiratory and autonomic control, including reduced chemoreceptor sensitivity, failure to initiate inspiration, respiratory rhythm abnormalities, and gasping deficit, seems to be the main contributor to a failure of arousal, and therefore autoresuscitation, when the child is challenged by a stressful homeostatic event, e.g., hypoxia and/or hypercapnia [22].
Although there is good evidence that the most important neurotransmitter playing a role in SIDS is serotonin, we still believe it is worthwhile to also investigate other than serotonin-related genes. Our candidate approach in the present study was based on reviews covering neurotransmitters in brainstem respiratory neurons [11, 23], and we opted to genotype 787 samples for 48 polymorphisms in genes that encode receptors, transporters, and enzymes involved in synthesis or degradation of transmitters associated with respiratory control (see Table 1).
We found that the TT genotype of rs563649 in the opioid receptor μ1 gene OPRM1 showed a borderline association with children who died of SIDS in autumn. Autumn is a sensitive “transition period” during which a respiratory infection is more likely to occur which precedes a multitude of SIDS cases. SNP rs563649 is located within a structurally conserved internal ribosomal entry site (IRES) in the 5′-UTR of an alternatively spliced OPRM1 isoform (MOR-1K) [24, 25]. IRESs need to have a precise secondary structure for proper functioning, and it was shown that the rare T allele of rs563649 causes a less optimal base pairing leading to a truncated 6 transmembrane (6TM) OPRM1 isoform rather than the canonical 7TM OPRM1. The 6TM isoform is suggested to display excitatory rather than inhibitory effects, explaining the findings of less analgesia following morphine administration in subjects with one or two T alleles [24]. This is an interesting finding because we had expected to find a more potent opioid receptor (suppressing respiratory drive more effectively) rather than a low-efficiency receptor variant (displaying rather excitatory effects) in SIDS cases.
The other SNP showing a significant result was rs1801030, located in SULT1A1, the gene coding for phenol sulfotransferase 1A1. SULT1A1 catalyzes the sulfate conjugation of small phenols, such as neurotransmitters and steroid hormones, and rs1801030 defines the SULT1A1*3 allozyme with a p.M223V change (c.A667G) [26]. The *3 variant has a similar or lower intrinsic enzyme activity compared to both the *1 and *2 variant, depending on the substrate [27]. The enzyme activity with regard to serotonin, dopamine, or (nor) adrenaline has not been investigated yet, though one can assume a normal-activity allozyme that has no effect on the catabolism on the before-mentioned neurotransmitters [28]. It was recently suggested that this polymorphism might be involved in sudden cardiac death after food intake and this might also apply to SIDS, in which often a full stomach is found upon autopsy [29]. Nevertheless, it is notable, that all heterozygotes detected (n = 4) occurred exclusively in the SIDS group with three of these cases having died in summer. This finding might indicate an involvement of rs1801030 in the etiology of SIDS but, as a note of caution, this result is based on a very small number of carriers. Data from the 1000 Genomes Project (http://browser.1000genomes.org/index.html) document a carrier frequency of 4 % in Europeans which would exceed our frequency in SIDS. Clearly, larger sample sizes will be required to define the effect of the p.M223V variant, if any, in the etiology of this condition. It remains unclear, however, why this association is valid only during summer. One explanation, among others, might be that the spectrum of mechanisms causative for SIDS might differ between seasons: In the cold season respiratory virus infections are common and might lead, according to the triple risk hypothesis, to SIDS. During summer, such infections are uncommon, and thus other mechanisms more related to SULT1A1 might prevail.
Additionally, two SNPs showed significant results in more than one SIDS subgroup before correction for multiple testing: Firstly, rs7832552, located within the thyrotropin-releasing hormone receptor gene TRHR [30], in the subgroups of SIDS: “0–4 months”, “2–4 months”, “autumn and winter”, and “winter”, suggesting a possible association with death at an early stage in late season. Secondly, rs7735184, located in HTR4, the gene encoding 5-hydroxytryptamine (serotonin) receptor 4 [11] for which our uncorrected results show that homozygous T allele carriers appeared significantly more frequent in the SIDS subgroups “males only”, “males vs. all controls”, and “prone sleep position” which might suggest that the T allele displays a less efficient variant of the serotonin 4 receptor resulting in a reduced reaction to stresses of the pulmonary system such as impaired breathing due to a prone sleep position.
Although two polymorphisms, rs563649 and rs1801030, showed significant results in our stratified analysis, the interpretation is limited in view of the highly complex regulation of respiratory control that ranges from the level of chemoreception to the level of central networks (especially the VRG) and to motor neurons in the spinal cord. An additional difficulty is the fact that the same transmitter can result in various effects on respiratory activity by acting on different receptors or by being released with different cotransmitters. A further interesting question is, whether and to what extent different neuromodulators can compensate for each other in case of impairment of one transmitter (system). Future genetic association studies may help to unravel additional pieces of this network of interacting modules.
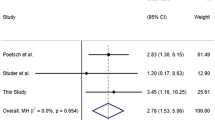
This study is among the largest case control studies on SIDS, both in terms of sample size and numbers of polymorphisms. Most comparable studies have a cohort size of well under 200 [e.g., 31–33], and recently, it was proposed that such a study should ideally comprise at least 200 case samples [34]. This criterion would be almost doubly fulfilled by our study on 366 SIDS cases and 421 controls. Nevertheless, it remains that our control sample consists of adults and infants. However, as both groups did not differ statistically, we are optimistic that the inferences drawn from this study are not biased by this fact.
In this large stratified case-control study, we provide evidence for a significant association of a subset of SIDS cases with two polymorphisms in selected candidate genes related to respiratory control: opioid receptor μ1 (OPRM1, subgroup: autumn) and sulfotransferase 1A1 (SULT1A1, subgroup: summer). In view of our findings presented here, it is unlikely that one of the investigated polymorphisms exerts a strong main effect on the predisposition towards SIDS. In a polygenic context, however, several gene variants in one infant may result in a significant impairment of respiratory control which may be lethal in combination with other exogenous risk factors.
References
Moon RY, Horne RSC, Hauck FR (2007) Sudden infant death syndrome. Lancet 370:1578–1587
Weese-Mayer DE, Berry-Kravis EM, Zhou L et al (2004) Sudden infant death syndrome: case-control frequency differences at genes pertinent to early autonomic nervous system embryologic development. Pediatr Res 56:391–395
Wang DW, Desai RR, Crotti L et al (2007) Cardiac sodium channel dysfunction in sudden infant death syndrome. Circulation 115:368–376
Klintschar M, Reichenpfader B, Saternus KS (2008) A functional polymorphism in the tyrosine hydroxylase gene indicates a role of noradrenalinergic signaling in sudden infant death syndrome. J Pediatr 153(2):190–193
Läer K, Vennemann M, Rothämel T, Klintschar M (2013) Association between polymorphisms in the P2RY1 and SSTR2 genes and sudden infant death syndrome. Int J Legal Med 127(6):1087–1091
Opdal SH, Opstad A, Vege A, Rognum TO (2003) IL-10 gene polymorphisms are associated with infectious cause of sudden infant death. Hum Immunol 64:1183–1189
Rand CM, Patwari PP, Carroll MS, Weese-Mayer DE (2013) Congenital central hypoventilation syndrome and sudden infant death syndrome: disorders of autonomic regulation. Semin Pediatr Neurol 20(1):44–55
Kinney HC (2009) Brainstem mechanisms underlying the sudden infant death syndrome: evidence from human pathologic studies. Dev Psychobiol 51(3):223–233
Gaultier C (1999) Sleep apnea in infants. Sleep Med Rev 3(4):303–312
Alheid GF, McCrimmon DR (2008) The chemical neuroanatomy of breathing. Respir Physiol Neurobiol 164(1–2):3–11
Doi A, Ramirez J (2008) Neuromodulation and the orchestration of the respiratory rhythm. Respir Physiol Neurobiol 164(1–2):96–104
Shao XM, Feldman JL (2005) Cholinergic neurotransmission in the pre-Bötzinger complex modulates excitability of inspiratory neurons and regulates respiratory rhythm. Neuroscience 130(4):1069–1081
Quartara L, Maggi CA (1997) The tachykinin NK1 receptor. Part I: ligands and mechanisms of cellular activation. Neuropeptides 31(6):537–563
Ellenberger HH, Smith FM (1999) Sulfated cholecystokinin octapeptide in the rat: pontomedullary distribution and modulation of the respiratory pattern. Can J Physiol Pharmacol 77(7):490–504
Dekin MS, Richerson GB, Getting PA (1985) Thyrotropin-releasing hormone induces rhythmic bursting in neurons of the nucleus tractus solitarius. Science 229(4708):67–69
Dutschmann M, Bischoff AM, Büsselberg D, Richter DW (2003) Histaminergic modulation of the intact respiratory network of adult mice. Pflugers Arch 445(5):570–576
Llona I, Eugenín J (2005) Central actions of somatostatin in the generation and control of breathing. Biol Res 38(4):347–352
Haji A, Takeda R (2001) Effects of a kappa-receptor agonist U-50488 on bulbar respiratory neurons and its antagonistic action against the mu receptor-induced respiratory depression in decerebrate cats. Jpn J Pharmacol 87(4):333–337
Manzke T, Guenther U, Ponimaskin EG et al (2003) 5-HT4(a) receptors avert opioid-induced breathing depression without loss of analgesia. Science 301(5630):226–229
Onimaru H, Shamoto A, Homma I (1998) Modulation of respiratory rhythm by 5-HT in the brainstem-spinal cord preparation from newborn rat. Pflugers Arch 435(4):485–494
Wang J, Lin M, Crenshaw A et al (2009) High-throughput single nucleotide polymorphism genotyping using nanofluidic dynamic arrays. BMC Genomics 10:561
Paterson DS, Hilaire G, Weese-Mayer DE (2009) Medullary serotonin defects and respiratory dysfunction in sudden infant death syndrome. Respir Physiol Neurobiol 168(1–2):133–143
Stornetta RL (2008) Identification of neurotransmitters and co-localization of transmitters in brainstem respiratory neurons. Respir Physiol Neurobiol 164(1–2):18–27
Shabalina SA, Zaykin DV, Gris P et al (2009) Expansion of the human mu-opioid receptor gene architecture: novel functional variants. Hum Mol Genet 18(6):1037–1051
Diatchenko L (2011) Elucidation of mu-opioid gene structure: how genetics can help predict responses to opioids. Eur J Pain Suppl 5(2):433–438
Nagar S, Walther S, Blanchard RL (2006) Sulfotransferase (SULT) 1A1 polymorphic variants *1, *2, and *3 are associated with altered enzymatic activity, cellular phenotype, and protein degradation. Mol Pharmacol 69(6):2084–2092
Rebbeck TR, Troxel AB, Shatalova EG et al (2007) Lack of effect modification between estrogen metabolism genotypes and combined hormone replacement therapy in postmenopausal breast cancer risk. Cancer Epidemiol Biomarkers Prev 16(6):1318–1320
Ung D, Nagar S (2007) Variable sulfation of dietary polyphenols by recombinant human sulfotransferase (SULT) 1A1 genetic variants and SULT1E1. Drug Metab Dispos 35(5):740–746
Eagle K (2012) Hypothesis: holiday sudden cardiac death: food and alcohol inhibition of SULT1A enzymes as a precipitant. J Appl Toxicol 32(10):751–755
Liu XG, Tan LJ, Lei SF et al (2009) Genome-wide association and replication studies identified TRHR as an important gene for lean body mass. Am J Hum Genet 84(3):418–423
Liebrechts-Akkerman G, Liu F, Lao O, Ooms AH, van Duijn K, Vermeulen M, Jaddoe VW, Hofman A, Engelberts AC, Kayser M (2014) PHOX2B polyalanine repeat length is associated with sudden infant death syndrome and unclassified sudden infant death in the Dutch population. Int J Legal Med 128:621–629
Studer J, Bartsch C, Haas C (2014) Sodium/proton exchanger 3 (NHE3) and sudden infant death syndrome (SIDS). Int J Legal Med 128:939–943
Klintschar M, Heimbold C (2012) No association of SIDS with two polymorphisms in genes relevant for the noradrenergic system: COMT and DBH. Acta Paediatr 101:1079–1082
Poetsch M, Todt R, Vennemann MM, Bajanowski T (2015) It’s not that, either - neither polymorphisms in PHOX2B nor in MIF are involved in Sudden Infant Death Syndrome (SIDS). Int J Legal Med
Acknowledgments
The authors would like to thank all persons who provided samples, especially Prof. K.-S. Saternus, Göttingen, as well as Doris Engmann, Claudia Schütz, and Peter Schürmann for excellent technical support. Moreover, they would like to thank K. Eagle, Katy, TX, USA, for the suggestion to include SULT1A1 into the analysis.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
Primer sequences developed for typing the SNP loci. ASP1 allele-specific primer 1, ASP2 allele-specific primer 2, LSP locus-specific primer, STA specific target (pre)amplification primer. The reaction involves a specific target preamplification using primers LSP and STA followed by a nested PCR using LSP, ASP1, and ASP2. (XLSX 12 kb)
ESM Table 2
Full results for the statistical analysis of 764 samples (358 SIDS and 406 controls) for 38 single nucleotide polymorphisms (SNPs) in genes involved in respiratory control. (XLSX 27 kb)
Rights and permissions
About this article
Cite this article
Läer, K., Dörk, T., Vennemann, M. et al. Polymorphisms in genes of respiratory control and sudden infant death syndrome. Int J Legal Med 129, 977–984 (2015). https://doi.org/10.1007/s00414-015-1232-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-015-1232-0