Abstract
In the present study, radiation doses and cancer risks resulting from abdominopelvic radiotherapy planning computed tomography (RP-CT) and abdominopelvic diagnostic CT (DG-CT) examinations are compared. Two groups of patients who underwent abdominopelvic CT scans with RP-CT (n = 50) and DG-CT (n = 50) voluntarily participated in this study. The two groups of patients had approximately similar demographic features including mass, height, body mass index, sex, and age. Radiation dose parameters included CTDIvol, dose–length product, scan length, effective tube current, and pitch factor, all taken from the CT scanner console. The ImPACT software was used to calculate the patient-specific radiation doses. The risks of cancer incidence and mortality were estimated based on the BEIR VII report of the US National Research Council. In the RP-CT group, the mean ± standard deviation of cancer incidence risk for all cancers, leukemia, and all solid cancers was 621.58 ± 214.76, 101.59 ± 27.15, and 516.60 ± 189.01 cancers per 100,000 individuals, respectively, for male patients. For female patients, the corresponding risks were 742.71 ± 292.35, 74.26 ± 20.26, and 667.03 ± 275.67 cancers per 100,000 individuals, respectively. In contrast, for DG-CT cancer incidence risks were 470.22 ± 170.07, 78.23 ± 18.22, and 390.25 ± 152.82 cancers per 100,000 individuals for male patients, while they were 638.65 ± 232.93, 62.14 ± 13.74, and 575.73 ± 221.21 cancers per 100,000 individuals for female patients. Cancer incidence and mortality risks were greater for RP-CT than for DG-CT scans. It is concluded that the various protocols of abdominopelvic CT scans, especially the RP-CT scans, should be optimized with respect to the radiation doses associated with these scans.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Based on results from biological and epidemiological studies, it is commonly accepted that cancer risk is increased by ionizing radiation exposure (National Research Council 2006). Approximately 48% of the average ionizing radiation dose to the USA general population originates from diagnostic medical procedures. Computed tomography (CT) scans constitute the greatest source of diagnostic medical radiation exposures to the USA general population (24% of total radiation exposure) (NCRP 2009; UNSCEAR 2017, 2018; Schauer and Linton 2009). It was estimated that the number of CT scan examinations increased from 62 million per year in 2006 to 85 million in 2011 in the United States (Brenner and Hall 2007; Miglioretti et al. 2013; IMV Medical Information Division 2012). Studies have indicated that the cancer risk is increased in patients who were exposed to ionizing radiation for medical reasons (Miglioretti et al. 2013; Wu et al. 2015).
Abdominopelvic CT scans are among the most common diagnostic examinations in adults. Because they include sensitive organs and involve long scan lengths, radiation doses are of particular concern. The average effective dose to patients from an abdominopelvic CT scan is about 10 mSv, which is typically several times greater than annual exposures from natural background (Zondervan et al. 2011). Furthermore, the use of treatment planning CT scans before radiation therapy has significantly increased (Sanderud et al. 2015). Given that approximately 50% of all patients with cancer receive radiation therapy in their treatment course (Mahmoudi et al. 2016), CT scans play a substantial role in staging and treatment planning in both radiation therapy and follow-up of patients with cancer (Yu et al. 2009).
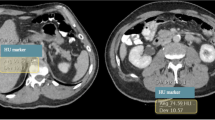
CT scans in radiotherapy treatment planning are applied for two reasons: to allow an accurate identification of the location of tumor and surrounding organs at risk, and to provide a map of the tissue electron density which is used in a treatment planning system (TPS) for dose calculation (Davis et al. 2017). For accurate dose calculations, a correct relationship between CT numbers or Hounsfield units (HUs) and electron densities is necessary (Mahmoudi et al. 2016). There are many parameters included in a CT scan protocol; some, but not all, of these parameters influence HU values (Ebert et al. 2008; Skrzynski et al. 2010). Variation of HU values in CT images can result in inaccuracies in the radiation therapy process. Typically, HU tolerances of ± 20 HU for soft tissue and ± 50 HU for lungs and bone are acceptable, because they are associated with dose uncertainties of less than 1% in TPS (Davis et al. 2017). Unfortunately, there are only few published studies on the optimization of CT scan protocols in radiation therapy. Such protocols should be adjusted to optimize image quality and radiation exposures in TPS (Davis et al. 2017).
CT imaging provides good visualization of the target volume and neighboring critical normal tissue, and allows for three-dimensional (3D) dose calculations; thus, the dose distribution over the entire irradiated volume can be calculated. 3D images of target volumes and critical organs are essential for the complex planning required in novel radiation therapy modalities such as intensity-modulated radiation therapy (IMRT) (Dawson and Menard 2010). Therefore, in CT examinations for radiotherapy planning, high-quality images are required. However, such high-quality CT scans may expose patients to higher and, perhaps, unnecessary radiation doses as compared to diagnostic CT scans.
Currently, the potential risk of radiation-induced cancer resulting from diagnostic imaging procedures, with a particular emphasis on CT scans, is receiving increasing attention (Rühm and Harrison 2020; Alawad and Abujamea 2021; Mahmoodi and Chaparian 2020; Karimizarchi and Chaparian 2017; Chaparian and Zarchi 2018). Recently, the National Research Council of the US National Academy of Sciences has published a report entitled “Biological Effects of Ionizing Radiation (BEIR) VII Phase 2”. In that report, risks of low-dose radiation exposure are estimated (National Research Council 2006). These risks are based on the data obtained from epidemiological studies on Hiroshima and Nagasaki atomic bomb survivors, patients who received medical radiation exposures, workers at nuclear power plants, and populations residing in areas where nuclear accidents had happened, such as the Chernobyl region. By the use of this information, cancer risks associated with low-dose radiation exposure can be predicted (see for example Wu et al. 2015).
Abdominopelvic CT scans are one of the most common examinations in medical diagnostics. Exposure to the involved ionizing radiation can increase the risk of cancer induction in patients undergoing such examinations, because of the fact that radiosensitive organs may also be exposed during the procedure, and because of the involved extended scan lengths. Consequently, the possible cancer risk due to CT scans should not be ignored (Sanderud et al. 2015), although there is no clear proof that low-dose radiation exposure can induce cancer (Fazel et al. 2009).
The present study was conducted to compute radiation absorbed doses and effective doses, and estimate and compare cancer incidence and cancer mortality risks of patients with abdominopelvic radiotherapy involving treatment planning CT scans and abdominopelvic diagnostic CT scans.
Methods
Investigated individuals
The present cross-sectional study was designed to estimate and compare cancer incidence and mortality risks in patients with abdominopelvic radiotherapy planning CT scans (RP-CT) and abdominopelvic diagnostic CT scans (DG-CT). Two groups of patients from the Shams Hospital (Urmia, Iran) with RP-CT (n = 50) and DG-CT (n = 50) voluntarily participated in the study. The number of patients enrolled for each group was selected based on availability. Written informed consent was obtained from all the participants. The inclusion criteria of the participants of the study were non-emergency, non-pregnant, non-three-phase scanning mode, and being older than 32 years. During the study, no patient was excluded. The two groups of patients were approximately matched for age, weight, and height. The DG-CT group consisted of 23 women and 27 men, while the RP-CT group included 19 women and 31 men.
Demographics and radiation dose parameters of the 100 patients were collected from September 2016 to July 2017. Patients’ demographic information included age, weight, sex, height, and body mass index (BMI). Dosimetric parameters as obtained from the CT console included volume CT dose index (CTDIvol), dose–length product (DLP), peak kilovoltage (kVp), tube current (mAs), collimation value, and pitch setting.
CT scan protocol
All the participants underwent an abdominopelvic CT scan (DG-CT and RP-CT) utilizing a 64-slice CT scanner (Philips Brilliance CT 64-slice; Philips Healthcare, Amsterdam, The Netherlands). The scan parameters were 120 kVp, 184 mAs, mean ± standard deviation (SD) of the scan length of 564.34 ± 42.36 mm, a rotation time of 0.5 s, a pitch of 0.859:1, a 64 × 0.625 mm collimation size, and a 2.5 mm slice thickness, for the RP-CT scans, while the corresponding scan parameters were 120 kVp, 181 mAs, 404.84 ± 29.93 mm, 0.5 s, 0.798:1, 64 × 0.625 mm, and 2 mm, for the DG-CT scans.
Radiation dose
Organ doses were calculated by Monte Carlo simulation (ImPACT CT dosimetry software package, version 1.0.4; developed by the scanner evaluation center of United Kingdom National Health Service), using a standardized hermaphrodite adult-stylized phantom to model photon transport from CT (Jones and Shrimpton 1993; Shrimpton et al. 2006; Jansen and Shrimpton 2011) and National Radiological Protection Board (NRPB) Monte Carlo datasets. ImPACT CT dosimetry software involves some uncertainties in calculating effective and organ doses in body CT images (Salimi et al. 2018). However, their effects on the results of this study are negligible due to the use of nearly similar demographic characteristics for both patient groups (RP-CT and DG-CT). To perform dose calculation for each patient, radiation dose parameters such as CTDIvol, DLP, pitch value, kVp, and mAs as recorded by the CT scanner console were used.
Based on the BEIR VII report, sensitive organs included in the cancer risk estimations were stomach, liver, colon, bladder, lung, prostate (for men), and uterus, ovarian, and breast (for women) (Huda et al. 2011). Radiation dose calculations and cancer risk estimations were performed assuming only a single CT scan per patient. Dose calculations were made in the following order:
Organ dose in the standard patient (70 kg) was calculated using Eq. 1
where the N-factor is a normalized coefficient, and CTDIvol is the CTDI volume obtained from the scanner console at the end of the examination.
For each organ, the N-factor was obtained from the ImPACT software (Eq. 2)
where (Organ dose)ImPACT is the organ dose calculated by the ImPACT software, and (CTDIvol)ImPACT is the CTDIvol acquired from ImPACT.
Organ doses in a patient with a certain weight, (Organ dose)W, were calculated as (Eq. 3)
where the W-factor denotes a weighting correction factor.
Equation 4 can be used to correct the differences among each patient and the ImPACT phantom (Huda et al. 2011). The weighting correction factor for a patient with standard size (70 kg) would be 1.0. For constant radiation exposure, an increase in the size of the patients results in a reduction in the W-factor, and vice versa
in which R(W) represents the W-factor which is a patient weight correction factor, and W is the patient mass (kg).
The effective radiation dose for each patient was obtained from Eq. 5
where DLP (mGy.cm) was obtained from the scanner console.
The C-factor is a correction factor obtained by dividing the effective dose by the DLP (Eq. 6), both of which were obtained from ImPACT calculator. The unit of the C-factor was mSv/mGy.cm unit
where EImPACT represents the effective dose calculated by the ImPACT software, and DLPImPACT is the DLP obtained from ImPACT.
Estimation of cancer risk
The risk of cancer induction has been described in the Biologic Effects of Ionizing Radiation (BEIR) VII report (National Research Council 2006) and is expressed by the lifetime attributable risk (LAR) (Eq. 7)
where D is the absorbed dose (in the BEIR VII report set equal to 100 mGy), 'e' denotes the patients' age at the time of exposure, 'a' is the attained age, which is calculated as e + L to 100 (L being the risk-free latent period that equals 5 years) accounting for the remaining lifetime, S(a) indicates the probability of survival until age ‘a’, and S(e) is the probability of survival until age ‘e’.
Calculation of cancer risk can be performed for particular cancers and also for all cancers combined (Smith-Bindman et al. 2009; Hoang et al. 2015). In the present study, the cancer types considered in the calculation of cancer risk were as follows: all cancers, leukemia, and all solid cancers. The risks of cancer incidence and cancer mortality were also calculated based on the method proposed by the BEIR VII committee (National Research Council 2006). The age- and sex-specific cancer incidence and mortality risks for a specific cancer were estimated using the linear interpolation of the two closest listed ages (Tables 12D-1 and 12D-2 of the BEIR VII document) (Einstein et al. 2007; Smith-Bindman et al. 2009).
Statistical analysis
All the statistical analyses were performed using the SPSS statistical software package (SPSS Inc., Chicago, IL, USA, version 16.0). Linear polynomial regression models were used to estimate cancer incidence and mortality risks. To fit the data, standardization methods were used, which included constant variance and linearity of the dependent variable to the independent variable. In addition, student’s independent t test was utilized to compare means of the continuous variables between the two groups. Differences were interpreted as statistically significant if the p value was < 0.05.
Results
Table 1 shows age, mass, height, and BMI for the two groups of patients.
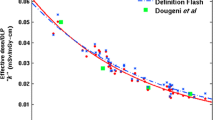
CTDIvol, DLP, and scan length values for RP-CT were 12.56 ± 2.81 mGy, 841.50 ± 229.02 mGy.cm, and 564.34 ± 42.36 mm, respectively. For DG-CT, the corresponding values were 12.65 ± 3.12 mGy, 646.27 ± 17.92 mGy.cm, and 404.84 ± 29.93 mm, respectively. The mean values of DLP and CTDIvol versus patient BMI showed that DLP and CTDIvol increased with increasing BMI in both groups (Fig. 1).
Scatter plots of volume-computed tomography dose index (CTDIvol) versus body mass index (BMI) (a), and dose–length product (DLP) versus BMI (b), in abdominopelvic radiotherapy treatment planning computed tomography (RP-CT) and diagnostic CT (DG-CT) scans; dotted and solid lines indicate linear fits through the data
The effective radiation dose for RP-CT was 13.91 ± 2.48 and 12.08 ± 3.51 mSv for males and females, respectively, as compared to 10.73 ± 1.53 and 10.79 ± 2.42 mSv for DG-CT. The doses absorbed by different organs in both groups are given in Table 2.
For RP-CT, the testes received the maximum absorbed dose (20.17 mGy) in male patients, whereas in female patients, the organ that received the highest dose was the adrenal gland (24.17 mGy). The lung had the lowest absorbed dose (10.60 mGy) in male patients, whereas in female patients, the breast received the minimum absorbed dose (9.25 mGy). For DG-CT, the highest absorbed dose was for the kidneys for both sexes, i.e., 18.79 mGy in males and 19.04 mGy in females. The testes had the minimum absorbed dose (1.37 mGy) in male patients, while in female patients, the breast had the lowest absorbed dose (0.77 mGy) (Table 2).
The risks of cancer incidence and mortality for different cancers are summarized in Tables 3 and 4 (Fig. 2). In the RP-CT group, the mean ± SD of the cancer incidence risk of all cancers, leukemia, and all solid cancers was 621.58 ± 214.76, 101.59 ± 27.15, and 516.60 ± 189.01 cancers per 100,000 individuals, respectively, for male patients. In contrast, for female patients, the corresponding risks were 742.71 ± 292.35, 74.26 ± 20.26, and 667.03 ± 275.67 cancers per 100,000 individuals, respectively.
The highest risk of cancer incidence was found for all cancers combined, for both sexes (940.45 cancers in males and 1280.12 cancers in females per 100,000 individuals. Leukemia had the lowest risk of cancer incidence, with 58.33 cancers in males and 43.39 cancers in females per 100,000 individuals (Fig. 3). In the DG-CT group, the male patients had a mean ± SD incidence risk for all cancers, leukemia, and all solid cancers risk of 470.22 ± 170.07, 78.23 ± 18.22, and 390.25 ± 152.82 cancers per 100,000 individuals, respectively. In the female patients, the corresponding numbers were 638.65 ± 232.93, 62.14 ± 13.74, and 575.73 ± 221.21 cancers per 100,000 individuals. The maximum risk of cancer incidence was related to all cancer risk with a value of 764.80 cancers per 100,000 individuals in males, and 1,107.37 cancers per 100,000 individuals in females. The lowest risk of cancer incidence was related to leukemia with 40.91 cancers per 100,000 individuals in male patients and 37.46 cancers per 100,000 individuals in female patients (Fig. 3).
For RP-CT, the risk of cancer-related mortality for all cancers, leukemia, and all solid cancers were 400.06 ± 121.60, 89.64 ± 23.09, and 311.45 ± 101.06 deaths per 100,000 individuals for males, respectively. These risks were 514.07 ± 173.83, 69.86 ± 17.67, and 443.51 ± 157.40, respectively, for females. The maximum risk of cancer mortality was seen in all cancer risk of both sexes: 594.83 deaths in males and 793.17 deaths in females per 100,000 individuals. The leukemia cancer risk in both sexes had the lowest risk of cancer mortality, 50.08, and 37.09 deaths per 100,000 individuals, respectively, in males and females (Fig. 4). For DG-CT, the male and female patients had mean ± SD of cancer mortality risk of all cancers, leukemia, and all solid cancers of 305.82 ± 89.60, 69.72 ± 15.06, and 235.74 ± 76.92 deaths per 100,000 individuals and 436.37 ± 128.77, 58.23 ± 10.84, and 377.77 ± 118.82 deaths per 100,000 individuals, respectively. In males, all cancer risk had the highest risk of cancer mortality, with 468.78 deaths per 100,000 individuals. In females, the highest risk of cancer mortality was related to all cancers (686.13 deaths per 100,000 individuals). In contrast, the lowest risk of cancer mortality was observed in leukemia (35.98 deaths per 100,000 individuals) and (38.02 deaths per 100,000 individuals) in males and females, respectively (Fig. 4). Figures 3 and 4 show the risks of cancer incidence and mortality of both groups versus age. The results demonstrate that the cancer risks in both groups decreased with increasing age of the patients (Figs. 3 and 4). The results also indicated a direct relationship between effective dose and risk of cancer incidence and cancer mortality (Figs. 5 and 6).
Discussion
The ImPACT Dosimetry software was used to calculate organ and effective doses in both males and females, to estimate the corresponding cancer risk associated with abdominopelvic radiation doses in RP-CT and DG-CT examinations.
The relationship between age, sex, and dosimetric parameters of the scanner was also elucidated. In both investigated patient groups, there was a direct correlation between CTDIvol and BMI, which might be due to the high production of scatter radiation in patients with a high BMI (Fig. 1). Mehnati et al. (2017), Bagherzadeh et al. (2018), and Isreal et al. (2010) obtained similar results for the relationship between CTDIVol and BMI. In contrast, in another study by Huda et al. (2011), CTDIvol did not depend on patient size (BMI). Furthermore, the present study found a direct relationship between DLP and BMI (Fig. 1), which is in line with the results of studies by Sanderud et al. (2015) and Bagherzadeh et al. (2018).
The mean CTDIVol in the two groups of patients who underwent abdominopelvic CT scans for RP-CT and DG-CT were not significantly different. However, Sanderud et al. (2015) reported that there was a considerable difference between the CTDIVol of patients who underwent thorax RP-CT scans and thorax DG-CT scans, which could be because they used a different number of slices per rotation for the two groups of patients.
The DLP in the RP-CT scans was almost 1.5 times higher than that in the DG-CT scans. This result can be attributed to a large scan length in the RP-CT scans as compared to DG-CT scans: for the RP-CT group, the scan length was 1.4 times greater than that in the DG-CT group.
Fujii et al. (2009) evaluated organ and effective doses to patients who underwent routine adult and pediatric CT examinations using different types of 64-slice CT scanners. They reported CTDIvol, DLP, and scan length of 17.6 mGy, 848 mGy.cm, and 482 mm, respectively. For adult abdominopelvic examinations, these results are similar to those reported in the present study. In addition, the ranges of the parameters mentioned above were 10.3–22.9 mGy, 503–1,138 mGy.cm, and 488–497 mm, for other types of 64-slice CT scanners (Fujii et al. 2009). The various techniques utilized for mAs modulation and variations among phantom and patients' sizes may have caused the observed discrepancy in CTDIvol values.
In the RP-CT scans, the effective doses were higher than those in the DG-CT scans. This can be attributed to the large scan length in the RP-CT scans caused by organs such as lungs, breast (in females), and testes (in males) that received greater doses compared to the DG-CT scans. Indeed, the scan length is defined by the necessity to include particular anatomical regions in the radiotherapy planning.
The effective dose values of the current study were in the range of values (10.3–20.7 mSv) reported by Fujii et al. (2007, 2009) and Nishizawa et al. (2008). However, in the present study, effective doses were greater than the values of 1.47–8.15 mSv in 6- and 16-slice scanners reported by Mehnati et al. (2017), and of 6.0–7.8 mSv in a 16-slice scanner reported by Van der Molen et al. (2007).
For RP-CT patients, the risk of cancer incidence in both sexes was higher than that for DG-CT patients. This difference can be due to the long scan length in the RP-CT scans that expose the lungs, testes (in males), breast, and ovaries (in females) to greater radiation doses. Furthermore, the risk of cancer mortality in the RP-CT scans was higher than that in the DG-CT scans, probably due to the same reasons.
Results of t tests also showed significant differences between the cancer incidence and cancer mortality of the two groups (RP-CT and DG-CT) in males (p < 0.05). However, no significant differences were observed in females, except for leukemia (Tables 3 and 4).
The risk of cancer induction depends on sex, age at exposure, type of radiation, and total absorbed dose to the body (National Research Council 2006). Typically, younger patients are more sensitive to the effects of radiation exposure than older patients (Choi et al. 2014; Isreal et al. 2010). Consequently, the risk of cancer for young patients is higher and decreased with increasing age at exposure (Figs. 3 and 4), as reported by Mahmoodi and Chaparian (2020), Karimizarchi and Chaparian (2017), Chaparian and Zarchi (2018), Li et al. (2011), and Huda et al. (2011). The risk of cancer also increased with increasing effective dose (Figs. 5 and 6), and these results are similar to those reported by Faletra et al. (2010). Abdominopelvic CT scans showed a remarkable risk of cancer induction, which is close the cancer risk due to cardiac CT angiography (Bagherzadeh et al. 2018). This may again be due to the long scan length and the fact that many radiosensitive organs are located in the abdominopelvic region.
There are some limitations of this study. First, the studies that were conducted for the same purposes used either an anthropomorphic phantom or an anthropomorphic mathematical phantom to estimate effective dose, because effective dose cannot be measured. Phantom models are limited, because the factual organ absorbed dose is dependent on the patient's size, weight, and fat repartition (Chang and Hou 2011). Second, Tables 12D-1 and 12D-2 of the BEIR VII report were used in the present study for estimating the cancer risk associated with abdominopelvic CT scans. However, the BEIR VII prediction models are based on an analysis of cancer risk transfer between the Japanese and US populations (Wu et al. 2015). Third, in the present study, cancer risk could have been somewhat underestimated compared to the actual cancer risk of the investigated patients, because there are certain organs such as spleen, kidney, small intestine, etc., that might receive a significant radiation dose, but are not considered in the estimation of risk. Fourth, the differences in the demographic parameters of the two groups of patients may have affected the results of the present study. Finally, it should be emphasized that in radiation therapy, the main dose contribution does not arise from any CT scans, but from the subsequent radiotherapy procedures, which will greatly surpass the doses from the CT scans and, hence, dominate the cancer risk.
Conclusion
The main purpose of this study was to explore any differences in radiation doses and the related cancer risks between two CT protocols. However, the impact of the detailed CT parameters used for DG-CT and RP-CT protocols on image quality was not investigated in the current study. The results obtained here showed no significant difference in the CTDIvol of the two groups of patients. The DLP of the RP-CT group was higher than that of the DG-CT group, which is due to the large scan length in the RP-CT scans. Both risks of cancer incidence and cancer mortality were greater in the RP-CT scans as compared to the DG-CT scans. Therefore, any protocols of abdominopelvic CT scans, especially RP-CT scans, should be optimized to minimize absorbed doses to the exposed organs, of course without compromising image quality. Furthermore, protection devices can be used to prevent unnecessary radiation exposure of some radiosensitive organs.
Data availability
The dataset used and analyzed for the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Alawad S, Abujamea A (2021) Awareness of radiation hazards in patients attending radiology departments. Radiat Environ Biophys 60:453–458
Bagherzadeh S, Jabbari N, Khalkhali HR (2018) Estimation of lifetime attributable risks (LARs) of cancer associated with abdominopelvic radiotherapy treatment planning computed tomography (CT) simulations. Int J Radiat Biol 94:454–461
Brenner DJ, Hall EJ (2007) Computed tomography–an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Chang ML, Hou JK (2011) Cancer risk related to gastrointestinal diagnostic radiation exposure. Curr Gastroenterol Rep 13:449–457
Chaparian A, Zarchi HK (2018) Assessment of radiation-induced cancer risk to patients undergoing computed tomography angiography scans. Int J Radiat Res 16(1):107–115
Choi SJ, Kim EY, Kim HS, Choi HY, Cho J, Yang HJ, Chung YE (2014) Cumulative effective dose associated with computed tomography examinations in adolescent trauma patients. Pediatr Emerg Care 30:479–482
Davis AT, Palmer AL, Nisbet A (2017) Can CT scan protocols used for radiotherapy treatment planning be adjusted to optimize image quality and patient dose? A systematic review. Br J Radiol 90(1076):20160406
Dawson LA, Menard C (2010) Imaging in radiation oncology: a perspective. Oncologist 15(4):338–349
Ebert MA, Lambert J, Greer PB (2008) CT-ED conversion on a GE Lightspeed-RT scanner: the influence of scanner settings. Australas Phys Eng Sci Med 31:154–159
Einstein AJ, Henzlova MJ, Rajagopalan S (2007) Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 298:317–323
Faletra FF, D’Angeli I, Klersy C, Averaimo M, Klimusina J, Pasotti E, Pedrazzini GB, Curti M, Carraro C, Diliberto R, Moccetti T, Auricchio A (2010) Estimates of lifetime attributable risk of cancer after a single radiation exposure from 64-slice computed tomographic coronary angiography. Heart 96:927–932
Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ, Nallamothu BK (2009) Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 361(9):849–857
Fujii K, Aoyama T, Koyama S, Kawaura C (2007) Comparative evaluation of organ and effective doses for paediatric patients with those for adults in chest and abdominal CT examinations. Br J Radiol 80:657–667
Fujii K, Aoyama T, Yamauchi-Kawaura C, Koyama S, Yamauchi M, Ko S, Akahane K, Nishizawa K (2009) Radiation dose evaluation in 64-slice CT examinations with adult and paediatric anthropomorphic phantoms. Br J Radiol 82:1010–1018
Hoang JK, Reiman RE, Nguyen GB, Januzis N, Chin BB, Lowry C, Yoshizumi TT (2015) Lifetime attributable risk of cancer from radiation exposure during parathyroid imaging: comparison of 4D CT and parathyroid scintigraphy. AJR Am J Roentgenol 204:W579–W585
Huda W, Schoepf J, Abro JA, Mah E, Costello P (2011) Radiation-related cancer risks in a clinical patient population undergoing cardiac CT. AJR Am J Roentgenol 196:W159–W165
IMV Medical Information Division (2012) IMV 2012 CT market outlook report. Des Plaines, IL: IMV Medical Information Division
Isreal GM, Cicchiello L, Brink J, Huda W (2010) Patients size and radiation exposure in thoracic, pelvic, and abdominal CT examinations performed with automatic exposure control. AJR Am J Roentgenol 195:1342–1346
Jansen JT, Shrimpton PC (2011) Calculation of normalised organ and effective doses to adult reference computational phantoms from contemporary computed tomography scanners. Prog Nuc Sci Technol 2:165–171
Jones DG, Shrimpton PC (1993) Normalised organ doses for X-ray computed tomography calculated using Monte Carlo techniques. NRPB-SR250. Chilton (UK): National Radiological Protection Board
Karimizarchi H, Chaparian A (2017) Estimating risk of exposure induced cancer death in patients undergoing computed tomography pulmonary angiography. Radioprotection 52(2):81–86
Li X, Samei E, Segars WP, Sturgeon GM, Colsher JG, Toncheva G, Yoshizumi TT, Frush DP (2011) Patient-specific radiation dose and cancer risk estimation in CT: Part II. Application to patients. Med Phys 38:408–419
Mahmoodi M, Chaparian A (2020) Organ doses, effective dose, and cancer risk from coronary CT angiography examinations. AJR Am J Roentgenol 214(5):1131–1136
Mahmoudi R, Jabbari N, Aghdasi M, Khalkhali HR (2016) Energy dependence of measured CT numbers on substituted materials used for CT number calibration of radiotherapy treatment planning systems. PLoS ONE 11(7):e01588282016
Mehnati P, Amirnia A, Jabbari N (2017) Estimating cancer induction risk from abdominopelvic scanning with 6- and 16-slice computed tomography. Int J Radiat Biol 12:1–10
Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, Feigelson HS, Roblin D, Flynn MJ, Vanneman N, Smith-Bindman R (2013) The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 167(8):700–707
National Research Council (2006) Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. The National Academies Press, Washington, DC. https://www.nap.edu/catalog/11340 /healt h-risks -from-expos ure-to-low-level s-of-ioniz ing-radiation
NCRP (2009) Ionizing radiation exposure of the population of the United States. NCRP Report No. 160. National Council on Radiation Protection and Measurements, Bethesda, Maryland
Nishizawa K, Mori S, Ohno M, Yanagawa N, Yoshida T, Akahane K, Iwai K, Wada SI (2008) Patient dose estimation for multi-detector row CT examinations. Radiat Prot Dosim 128:98–105
Rühm W, Harrison RM (2020) High CT doses return to the agenda. Radiat Environ Biophys 59:3–7
Salimi Y, Deevband MR, Ghafarian P (2018) Uncertainties in effective dose estimation for CT transmission scan in total body PET-CT imaging with Auto mA3D tube current modulation. Int J Radiat 16:465–472
Sanderud A, England A, Hogg P, Fossa K, Svensson SF, Johansen S (2015) Radiation dose differences between thoracic radiotherapy planning CT and thoracic diagnostic CT scans. Radiography 22:107–111
Schauer DA, Linton OW (2009) National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. Radiology 253:293–296
Shrimpton PC, Hillier MC, Lewis MA, Dunn M (2006) National survey of doses from CT in the UK: 2003. Br J Radiol 79:968–980
Skrzynski W, Zielinska-Dabrowska S, Wachowicz M, Slusarczyk-Kacprzyk W, Kukolowicz P, Bulski W (2010) Computed tomography as a source of electron density information for radiation treatment planning. Strahlenther Onkol 186:327–333
Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de Gonzalez A, Miglioretti DL (2009) Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 169:2078–2086
UNSCEAR 2016 (2017) Report to the General Assembly, with Scientific Annexes. Sources, effects and risks of ionizing radiation. United Nations, New York
UNSCEAR 2017 (2018) Report to the General Assembly, with Scientific Annexes. Sources, effects and risks of ionizing radiation. United Nations, New York
Van der Molen AJ, Veldkamp WJ, Geleijns J (2007) 16-slice CT: achievable effective doses of common protocols in comparison with recent CT dose surveys. Br J Radiol 80:248–255
Wu TH, Lin WC, Chen WK, Chang YC, Hwang JJ (2015) Predicting cancer risks from dental computed tomography. J Dent Res 94(1):27–35
Yu L, Liu X, Leng S, Kofler JM, Ramirez-Giraldo JC, Qu M, Christner J, Fletcher JG, McCollough CH (2009) Radiation dose reduction in computed tomography: techniques and future perspective. Imaging Med 1(1):65–84
Zondervan RL, Hahn PF, Sadow CA, Liu B, Lee SI (2011) Frequent body CT scanning of young adults: indications, outcomes, and risk for radiation-induced cancer. J Am Coll Radiol 8:501–507
Acknowledgements
We especially thank the Vice Chancellor for Research (VCR) of Urmia University of Medical Sciences, who approved and supported this project. We also thank the Shams Hospital for data collection and management.
Funding
The current work was supported by grant IR.UMSU.REC. 1397.235. The funding bodies played no role in the design of the study, in collection, analysis, and interpretation of the data, and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
NJ, SB, and HRK were responsible for the conceptualization and acquisition of the data. NJ, SB, and HRK were responsible for the methodology. NJ and SB were responsible for the writing, review, and/or revision of the manuscript. NJ, SB, and HRK were responsible for the administrative, technical, or material support. NJ was responsible for the study supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The ethics committee of Urmia University of Medical Sciences approved all procedures of this experiment (ethical approval no: IR.UMSU.REC.1394-01-62-2186).
Informed consent
Written informed consent was obtained from the study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bagherzadeh, S., Jabbari, N. & Khalkhali, H.R. Radiation dose and cancer risks from radiation exposure during abdominopelvic computed tomography (CT) scans: comparison of diagnostic and radiotherapy treatment planning CT scans. Radiat Environ Biophys 60, 579–589 (2021). https://doi.org/10.1007/s00411-021-00942-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-021-00942-6