Abstract
Evaluating the knowledge of patients attending radiology departments regarding ionizing radiation used in medical imaging and its associated hazards can provide knowledge of the patient’s awareness level of the associated risk of the radiation used in medical imaging. The aims of this study were to evaluate the awareness of patients regarding medical radiation types used in medical diagnostic imaging and its influence on their decision to proceed with that procedure. Over an 8-months period, a total of 418 patients, 48% Men and 52% Women, presenting for diagnostic imaging in the department of radiology, completed a 15-point questionnaire. The questionnaire included demographic and radiation awareness sections. Less than 32% of the participants had a potential risk of radiation explained by the doctor before the procedure. 59% of the participants expressed that the potential risk of radiation makes them anxious; less than about 25% of the participants showed that the potential risk of radiation affects their decision to have the procedure. Overall, the data collected from this survey indicate that there is a lack of information about radiation risk provided to the patients prior to the diagnostic procedure. Efforts should be made to ensure that patients receiving multiple medical imaging tests are aware of the radiation they are receiving.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ionizing radiation is well recognized as a causative agent of acute and chronic health problems (e.g., cancers and genetic mutations) that can lead to mortality and morbidity (Brenner and Hall 2007; Christodouleas et al. 2011; Giles et al. 1956; Howe and McLaughlin 1996; Linet et al. 2009, 2012; Smith-Bindman 2010; Smith-Bindman et al. 2009; UNSCEAR 2000. The United Nations Scientific Committee on the Effects of Atomic Radiation 2000). The increase utilization of ionizing radiation in medical imaging and health care practice has increased over the past decades, which is regarded as a potential health hazard (Berdahl et al. 2013; Chung et al. 2019; Coleman et al. 2005; Smith-Bindman et al. 2008).
Individuals can be exposed to radiation from various resources, including naturally occurring, medical imaging, and other human-made non-medical equipment. The perception and awareness of ionizing radiation effects varies between the general population and radiation experts due to their knowledge and competence (Kanda et al. 2012; Mainous and Hagen 1993; Ria et al. 2017; Schauer and Linton 2009; Slovic 1996).
Many patients might not be aware of the risks associated with radiation diagnostic examination; others trust their treating physician and simply follow their orders without attempting to understand the risks associated with the requested procedures. Some referring physicians feel hesitant giving the patient sufficient information about the potential risk of exposure to radiation, and this might be due to the fear that the patient may refuse a procedure that is critical for diagnosis and treatment (Banerjee et al. 2019; Hollada et al. 2015; Mattsson and Nilsson 2015; Schuster et al. 2018). Sometimes the referring physicians do not have sufficient information or time to discuss complex technical details about the procedures and levels of radiation exposure that result from their use (Ricketts et al. 2013; Schuster et al. 2018). Increasing patient information is an important aspect of patients’ autonomy. Earnest suggested that having a written organ specific consent would give patients the information that a reasonable person would want to know prior to having a screening chest CT examination (Earnest et al. 2003). Underestimation of radiation hazards might put the patients at high risk of frequent ionizing radiation exposures. This can increase the radiation hazard, especially with the availability of a new generation of medical equipment that lead to higher radiation doses, such as computed tomography (Almaghrabi 2016; Avramova-Cholakova et al. 2015; Doss 2014; Montes et al. 2013; Salerno et al. 2018; Salvatori et al. 2019). A lack of systematic radiation monitoring and documentation of radiation exposure history in the patient file increases the risk of exceeding the safe limits of radiation exposure for individuals. The European Directive 2013/59/EURATOM requires patient radiation dose information to be included in the medical report of radiological procedures (European_Soc_Radiology 2015). On the other hand, we increasingly see patients becoming more involved in their own medical care. Prior to attending the hospital, they seek information to be better prepared for their hospital examination. They increasingly use online search engines to read about the risks and effects of their imaging procedure (Kenny et al. 2019).
To provide effective communication to the patient, it is necessary to first assess the patient's level of knowledge regarding medical exposure. To evaluate the level of radiation awareness, qualitative assessment among patients would help in better understanding the current situation and the best ways to improve radiation awareness.
The goal of this work is to survey patients' current knowledge level of both medical exposure to ionizing radiation and professional disciplines and communication means used by patients to garner information.
Methods
A cross-sectional survey-based design was used. A consecutive series of 418 eligible patients attending the radiology department for investigation at King Khalid University Hospital, Riyadh, Saudi Arabia, from January 2017 to August 2017 were included in this study. 500 questionnaires were distributed and 418 were the final responses. Approval from the institutional review board was obtained before the commencement of the study, Ref. No. 17/0037/IRB. Candidates attending their radiologic examination, including routine X-ray imaging, CT, fluoroscopy, MRI, US, or nuclear medicine and agreed in participating, were provided an informational sheet that explained the intentions of the study before undergoing the procedure.
The questionnaire was designed by the authors and was available in both Arabic and English languages and consisted of fifteen multiple-choice questions, included demographic information (gender, age range, radiology history and education level). Respondents were asked if they were provided with radiation information upon examination from the health workers’ team and whether that has an influence on their decision on proceeding with the radiology procedure. The questionnaire included a question on the participants’ knowledge about radiation used in medical imaging and the source of this knowledge, the respondents were asked to choose whether it was from TV and Radio, Magazines and Newspapers, school, internet, family and friends or from the radiology technician. The questionnaire also included a question about which radiology modality posed the greatest health risk, the respondents were asked to choose between CT, X-ray or they have the same risk. The remaining questions covered the radiation awareness knowledge of ionizing radiation, which represents the basic aspects of underlining radiation safety awareness, such as radiation-induced cancer, and cause of infertility and fetal malformations.
The statistical analysis was carried out using SPSS version 20.0 (IBM Corp., Armonk, NY, USA). The quantitative variables were expressed as mean plus-minus standard deviation while the qualitative variables were recorded as proportions or percentages. Different groups were made according to age, sex and educational level and the different responses were compared between the groups. A chi-square test was used to test for significant differences in proportions between the different groups. Moreover, we did linear by linear association analysis to see the trend of different variables or the questions response’s according to sex, education level and to different age groups. p values less than 0.05 were considered significant.
Results
There were 418 respondents to the survey (217 women, 201 men). The majority of respondents (52%) were aged between 21 and 40 years (Table 1).
Most (68.1%) of the respondents replied that the doctor did not explain the potential risk of radiation, and 57.2% of the respondents answered that they have read/heard about the radiation risk of medical imaging. They derived their information from various sources: TV/radio, school, an article in the newspaper, the Internet, or people around with no significant variation between the sources. Only 50.5% of respondents thought that CT is more dangerous than an x-ray. More than half (59.1%) of the respondents replied that the potential risk of radiation makes them anxious (women showed a higher percentage: 65.0%). Most of the respondents answered that the potential risk of radiation did not affect their decision about doing the procedure (76%) (Table 2).
42% of our respondents did not believe that frequent exposure to radiation can cause cancer (Table 2). Only 41.6% of our respondents thought that frequent radiation can cause infertility (Table 2). 90.2% of respondents agreed that radiation exposure can cause fetal malformation.
Awareness of radiation hazards and its possible relationship with cancer was noticed to be higher in the middle-aged group (60%). This decreases among the older age group (40%). Infertility and its probability in case of frequent radiation were not well recognized among all age groups. All age groups show good awareness regarding pregnancy risks associated with radiation. We found that age had a significant impact on the general knowledge about the risk related to medical imaging (p value = 0.001). Young aged patients have read/heard more about the risk related to medical imaging than old aged patients (Table 3).
With respect to education level we found knowledge about the possible risk related to medical imaging increased with the level of education (p value = 0.004) (Table 4). Also, education had a significant impact on the awareness of the relation between frequent exposure to radiation and the possible risk of developing cancer (p value = 0.001). Education level was not significantly related to the patient been anxious to the potential risk of radiation nor affects the patient decision about doing the procedure (Table 4).
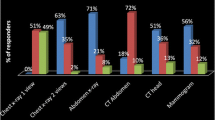
In respect to sex, we found that women were more anxious about the potential risk of radiation than men (p value = 0.031). Women also thought that radiation exposure in pregnancy can increase the risk of fetal malformations more than men (p value = 0.024). Men significantly more often than women thought that frequent exposure to radiation can increase the risk of infertility (p value = 0.001). Sex had no impact on affecting patient decision about doing the procedure with respect to the potential risk of radiation (Fig. 1).
Comparison of sex-based patient’s awareness of ionizing radiation. See Table 2 for the content of the questions. p values are based on Chi-square test
Discussion
The involvement of radiation imaging in the health care system has been evolving rapidly over recent years. Although it has a great impact on clinical practice and management of patients, it is associated with a risk of adverse health effects.
Awareness and appreciation of the risks associated with undergoing these modalities are an important element of modern societies. We aimed through this study to assess awareness of radiation hazards among our study population.
Only 58% of studied participants thought that frequent exposure to radiation can increase the risk of developing cancer. Only 50.5% of respondents thought that CT is more dangerous than an X-ray. These findings demonstrate a need for patients to be appropriately informed of the benefits and risks associated with the radiation used in medical imaging.
Our study variables were mainly age, sex, and educational level. Although our sample size was small, it properly reflects our population with respect to age and sex. It also includes different education levels and can give us a comprehensive assessment of awareness among patients visiting the radiology departments.
In comparison with other studies, we found similar results on that educational level does not play a major role in regard to radiation hazard awareness (Alshammari et al. 2019). At some aspects of radiation hazard, the percentage of awareness was higher in the low education level group.
Awareness of possible radiation-induced infertility was obviously affected by sex. Unfortunately, women were less aware of radiation hazards and their possible negative effects on their fertility. With regard to adverse effects of radiation, this result suggests that patients’ awareness about teratogenic risk associated with ionizing radiation was very high, most of the respondents (90.2%) do think that radiation exposure in pregnancy can increase the risk of fetal malformation, this was higher than the findings in Aldossari study 49.3% (Aldossari et al. 2019).
Based on our survey regarding knowledge and awareness, we concluded that people in young and old adult age groups, in contrast to the middle-aged groups, had a relatively low level of knowledge and awareness of radiation hazards. There needs to be more focus on health education to improve awareness among these age groups.
Most of the participants stated that the potential risk of radiation was not explained to them by their doctors (68.4%), demonstrating the lack of proper communication between the radiologist and the patient. An important element of modern medical procedures is shared decision making, which implies involving patients in the decision regarding the need of medical imaging.
The knowledge and awareness of the radiation doses and risks can help the clinicians better discussing the risks and benefits of radiology procedures with their patients. It also guides them when making decisions regarding the need and the frequency of scans (Al-Rammah 2016).
Limitations
This study was conducted in the department of radiology in the university hospital and provides information relevant to a single radiology department in Saudi Arabia. It is possible that patients from different practices including private and large public hospitals, as well as patients in other geographical locations, in particular small cites or remote areas, would have responded to the survey differently. Thus, the study findings have limited external validity. In addition, in this study the health risk of radiation used in medical imaging was generalized and was not related to a specific kind of imaging modality. Therefore, the participants may have responded to some of the questions differently if they were asked about a specific kind of radiology procedures.
Conclusions
The findings of this study suggest that in general there is a lack of knowledge among patients leading to an underestimation of risks associated with ionizing radiation exposure. Clearly, there is a need for improved communication between health professionals and patients. Radiation hazard is a critical issue in the health care system that needs to be addressed by clinicians and radiation protection officers. The patient should be more involved in the decision to proceed with radiology procedures and should be more aware of the level of radiation that they will be exposed to as well as the previous radiation exposures that he/she received. The radiation exposure and the associated risks should be discussed with the patient at different points and levels. Radiologists, radiographers/technologists and referring physicians have different roles. Referring physicians will discuss the clinical need for the imaging procedure but the discussion about radiation exposure is more likely to occur at the point of imaging. It is very important that health professionals are well prepared to communicate and discuss in simple language that can be easily understood the risks associated with radiological imaging.
Recommendations
Radiology departments need to provide adequate information to patients to ensure that patients are informed of the benefits and risks associated with the exposure derived from imaging procedures. Healthcare practitioners should be able to inform patients about the benefits and potential risks of ionizing radiation for medical purposes based upon evidence-based practice and guidelines (Ribeiro et al. 2020).
More health education is required for the general population. This will help to emphasize the situation of awareness toward the radiation hazard and improve health care in general.
References
Aldossari H, Ahmed N, AlShammari A (2019) Evaluation of awareness on radiation protection and knowledge about ionizing radiation among patients awaiting radiological examinations: a cross-sectional survey. Austin J Radiol 6(3):1100–1104
Almaghrabi A (2016) Study of knowledge and awareness of radiation exposure risk in Makkah, Saudi Arabia. Int J Adv Res 4(7):1852–1856
Al-Rammah TY (2016) CT radiation dose awareness among paediatricians. Ital J Pediatr 42:77. https://doi.org/10.1186/s13052-016-0290-3
Alshammari K, Alramadan L, Ali J, Farraj M, Alanazi K, Almurbati A (2019) Knowledge and perception of patients towards the hazards and dose of diagnostic radiation in Bahrain. Int J Med Dev Ctries 3(12):1128–1134
Avramova-Cholakova S, Dimcheva M, Petrova E, Garcheva M, Dimitrova M, Palashev Y et al (2015) Patient doses from hybrid SPECT-CT procedures. Radiat Prot Dosim 165(1–4):424–429. https://doi.org/10.1093/rpd/ncv130
Banerjee I, McNulty JP, Catania D, Maccagni D, Masterson L, Portelli JL et al (2019) An investigation of procedural radiation dose level awareness and personal training experience in communicating ionizing radiation examinations benefits and risks to patients in two european cardiac centers. Health Phys 117(1):76–83. https://doi.org/10.1097/HP.0000000000001049
Berdahl CT, Vermeulen MJ, Larson DB, Schull MJ (2013) Emergency department computed tomography utilization in the United States and Canada. Ann Emerg Med 62(5):486–494. https://doi.org/10.1016/j.annemergmed.2013.02.018
Brenner DJ, Hall EJ (2007) Computed tomography—an increasing source of radiation exposure. N Engl J Med 357(22):2277–2284. https://doi.org/10.1056/NEJMra072149
Christodouleas JP, Forrest RD, Ainsley CG, Tochner Z, Hahn SM, Glatstein E (2011) Short-term and long-term health risks of nuclear-power-plant accidents. N Engl J Med 364(24):2334–2341. https://doi.org/10.1056/NEJMra1103676
Chung JH, Duszak R, Hemingway J, Hughes DR, Rosenkrantz AB (2019) Increasing utilization of chest imaging in US Emergency Departments From 1994 to 2015. J Am Coll Radiol 16(5):674–682. https://doi.org/10.1016/j.jacr.2018.11.011
Coleman RE, Delbeke D, Guiberteau MJ, Conti PS, Royal HD, Weinreb JC et al (2005) Concurrent PET/CT with an integrated imaging system: intersociety dialogue from the joint working group of the American College of Radiology, the Society of Nuclear Medicine, and the Society of Computed Body Tomography and Magnetic Resonance. J Nucl Med 46(7):1225–1239
Doss M (2014) Addition of diagnostic CT scan does not increase the cancer risk in patients undergoing SPECT studies: comment on Brix et al.: radiation risk and protection of patients in clinical SPECT/CT. Eur J Nucl Med Mol Imaging 41(Suppl 1):S146–S147. https://doi.org/10.1007/s00259-014-2711-0
Earnest F, Swensen SJ, Zink FE (2003) Respecting patient autonomy: screening at CT and informed consent. Radiology 226(3):633–634. https://doi.org/10.1148/radiol.2263020626
European_Soc_Radiology (2015) Summary of the European Directive 2013/59/Euratom: essentials for health professionals in radiology. (1869–4101). Retrieved from <Go to ISI>://WOS:000215424900002
Giles D, Hewitt D, Stewart A, Webb J (1956) Malignant disease in childhood and diagnostic irradiation in utero. Lancet 271(6940):447. https://doi.org/10.1016/s0140-6736(56)91923-7
Hollada J, Speier W, Oshiro T, Marzan-McGill R, Ruehm SG, Bassett LW et al (2015) Patient’s perceptions of radiation exposure associated with mammography. Am J Roentgenol 205(1):215–221. https://doi.org/10.2214/Ajr.14.13650
Howe GR, McLaughlin J (1996) Breast cancer mortality between 1950 and 1987 after exposure to fractionated moderate-dose-rate ionizing radiation in the Canadian Fluoroscopy Cohort Study and a comparison with breast cancer mortality in the Atomic Bomb Survivors Study. Radiat Res 145(6):694–707. https://doi.org/10.2307/3579360
Kanda R, Tsuji S, Yonehara H (2012) Perceived risk of nuclear power and other risks during the last 25 years in Japan. Health Phys 102(4):384–390. https://doi.org/10.1097/HP.0b013e31823abef2
Kenny E, Byrne B, Lewis M, King DM (2019) Perception of medical radiation risk in Ireland: Results of a public survey. Phys Med 68:96–103. https://doi.org/10.1016/j.ejmp.2019.10.033
Linet MS, Kim KP, Rajaraman P (2009) Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatr Radiol 39(Suppl 1):S4-26. https://doi.org/10.1007/s00247-008-1026-3
Linet MS, Slovis TL, Miller DL, Kleinerman R, Lee C, Rajaraman P et al (2012) Cancer risks associated with external radiation from diagnostic imaging procedures (vol 62, pg 75, 2012). Cancer J Clin 62(4):277–277. https://doi.org/10.3322/caac.21145
Mainous AG 3rd, Hagen MD (1993) Public perceptions of radon risk. Fam Pract Res J 13(1):63–69
Mattsson S, Nilsson M (2015) On the estimation of radiation-induced cancer risks from very low doses of radiation and how to communicate these risks. Radiat Prot Dosim 165(1–4):17–21. https://doi.org/10.1093/rpd/ncv037
Montes C, Tamayo P, Hernandez J, Gomez-Caminero F, Garcia S, Martin C et al (2013) Estimation of the total effective dose from low-dose CT scans and radiopharmaceutical administrations delivered to patients undergoing SPECT/CT explorations. Ann Nucl Med 27(7):610–617. https://doi.org/10.1007/s12149-013-0724-6
Ria F, Bergantin A, Vai A, Bonfanti P, Martinotti AS, Redaelli I et al (2017) Awareness of medical radiation exposure among patients: a patient survey as a first step for effective communication of ionizing radiation risks. Phys Med 43:57–62. https://doi.org/10.1016/j.ejmp.2017.10.014
Ribeiro A, Husson O, Drey N, Murray I, May K, Thurston J et al (2020) Ionising radiation exposure from medical imaging-a review of Patient’s (un) awareness. Radiography (lond) 26(2):e25–e30. https://doi.org/10.1016/j.radi.2019.10.002
Ricketts ML, Baerlocher MO, Asch MR, Myers A (2013) Perception of radiation exposure and risk among patients, medical students, and referring physicians at a tertiary care community hospital. Can Assoc Radiol J 64(3):208–212. https://doi.org/10.1016/j.carj.2012.05.002
Salerno S, Nardi C, Tudisca C, Matranga D, Vernuccio F, Di Piazza A et al (2018) Complete written/oral information about dose exposure in CT: is it really useful to guarantee the patients’ awareness about radiation risks? Radiol Med 123(10):788–798. https://doi.org/10.1007/s11547-018-0909-0
Salvatori M, Rizzo A, Rovera G, Indovina L, Schillaci O (2019) Radiation dose in nuclear medicine: the hybrid imaging. Radiol Med 124(8):768–776. https://doi.org/10.1007/s11547-019-00989-y
Schauer DA, Linton OW (2009) NCRP report No. 160, ionizing radiation exposure of the population of the United States, medical exposure—are we doing less with more, and is there a role for health physicists? Health Phys 97(1):1–5. https://doi.org/10.1097/01.HP.0000356672.44380.b7
Schuster AL, Forman HP, Strassle PD, Meyer LT, Connelly SV, Lee CI (2018) Awareness of radiation risks from CT scans among patients and providers and obstacles for informed decision-making. Emerg Radiol 25(1):41–49. https://doi.org/10.1007/s10140-017-1557-8
Slovic P (1996) Perception of risk from radiation. Radiat Prot Dosim 68(3–4):165–180
Smith-Bindman R (2010) Is Computed tomography Safe? N Engl J Med 363(1):1–4. https://doi.org/10.1056/NEJMp1002530
Smith-Bindman R, Miglioretti DL, Larson EB (2008) Rising use of diagnostic medical imaging in a large integrated health system. Health Aff 27(6):1491–1502. https://doi.org/10.1377/hlthaff.27.6.1491
Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R et al (2009) Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 169(22):2078–2086. https://doi.org/10.1001/archinternmed.2009.427
UNSCEAR (2000) The United Nations Scientific committee on the effects of atomic radiation. Health Phys 79(3):314
Acknowledgements
The authors would like to thank the Deanship of Scientific Research for funding and supporting this research through the initiative of DSR scholarship support. Thanks to our medical student colleagues, Khalid Alkhamis and Majed Altulayan, for their help. Finally, we would like to express our special thanks of gratitude to Professor Syed Shahid Habib for his support and advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alawad, S., Abujamea, A. Awareness of radiation hazards in patients attending radiology departments. Radiat Environ Biophys 60, 453–458 (2021). https://doi.org/10.1007/s00411-021-00919-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-021-00919-5