Abstract
Background
Regulatory T lymphocytes (Tregs) are known to have host-immune dampening effects in many tumors and to be associated with increased tumor recurrence. Pharmacologic therapies have been developed to target these cells and hence strengthen the host’s immune system. The FoxP3 gene is a marker of Tregs and can be visualized with immunohistochemistry (IHC). We investigated the presence and pattern of Tregs in non-small-cell lung tumors to determine possible therapeutic targets in lung cancer.
Methods
We selected archival samples of primary lung carcinoma and benign inflamed lung from 32 surgical resections. We created a tissue array containing duplicate cores from the N1 and N2 nodal stations from 16 of the cases along with paired benign lung and tumor. We used whole-slide analysis for the other 16 cases. We used FoxP3 IHC to visualize Tregs in all lymphoid tissue present and to assess the quantity and pattern within the tissues.
Results
All lymphoid tissue contains Tregs, but adenocarcinoma had significantly higher levels than both inflammatory lung controls and squamous carcinomas (p ≤ 0.008). Benign N1 lymph nodes (from patients with lung cancer) showed higher numbers of Tregs for adenocarcinoma versus squamous carcinoma.
Conclusions
These findings reveal that Tregs are present in all lung tissues examined, but with significant enrichment in adenocarcinoma. This may lead to a more permissive microenvironment for adenocarcinoma and may explain aggressive patterns of tumor spread for this histology. Lung cancer patients with adenocarcinoma histology may benefit most from Treg-targeted therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Rudolf Virchow believed pathology stemmed from alterations of normal physiology and insufficiency of the immune regulatory apparatus [1]. Dysregulated self-immunity involves a recently recognized regulatory T lymphocyte subset (Treg) shown to play a role in self-recognition and autoimmunity. CD4 + CD25 + Tregs are a subset of CD4 T cells that suppress immune responses and previously referred to as suppressor T cells. Tregs account for 5–15 % of CD4+ cells in humans [2].
Tregs were originally discovered in mice engineered to lack interleukin-2 (IL-2), and they appear to be crucial for the maintenance of tolerance [3]. Intracellularly, FoxP3 is the master gene regulator for inducing Treg phenotype. It encodes FoxP3 protein (previously called scurfin), a transcriptional repressor [4, 5]. Nuclear Foxp3 is currently the only specific immunohistochemical marker for regulatory T cells. In the host, Tregs lessen immune responses, both innate and adaptive.
Tregs have been implicated to play a role in multiple sclerosis, rheumatoid arthritis, and HIV. There is a syndrome of human deficiency of FoxP3 that causes polyendocrinopathy, enteropathy, immune dysregulation, and X-linked inheritance (IPEX) syndrome [4]. Tregs have also been shown to suppress host immune responses to a variety of cancers, including lung, ovarian, colon, esophageal, pancreatic, breast, and melanoma [6–11]. Patients with non-small-cell lung cancer who have a higher proportion of tumor-associated Treg cells relative to non-Treg lymphocytes have a significantly higher risk of recurrence [12, 13]. CD25 is the IL-2 receptor alpha. It is present on activated T cells, not just in Tregs. Cytotoxic T-lymphocyte-associated antigen (CTLA-4) plays a critical role in the regulation of T-cell activation. The programmed death-1 coinhibitory receptor (PD-1) is also expressed by these activated T cells. Targeting Treg cell function in patients with non-small-cell lung cancer using fully human monoclonal antibodies against CTLA-4 (anti-CTLA-4) and PD-1(anti-PD-1) appears to result in significant antitumor activity [14, 15].
We investigated the presence and pattern of Treg lymphocyte infiltration in human non-small-cell lung cancers with respect to histologic subtype. We also tested the draining lymph nodes from N1 (ipsilateral peribronchial, hilar, and intrapulmonary nodes) and N2 (ipsilateral mediastinal and subcarinal nodes) [16] stations from patients with primary lung tumors for the presence and quantity of Tregs.
Methods
Following DHMC IRB approval, 32 cases of formalin-fixed paraffin-embedded lung tissue were selected from the pathology department archives. For half of the cases [5 squamous cell carcinoma (SCC), 7 invasive adenocarcinoma (ADC), 1 adenocarcinoma in situ, 2 inflammatory cases (1 bronchiectasis and 1 interstitial fibrosis), and 1 metastatic thyroid carcinoma to the lung], whole-tissue slides were cut from the paraffin block and incubated with 1:50 dilution of purified anti-Foxp3 antibody (Biolegend, San Diego CA). We used a modification of a method previously described [12] for quantifying Treg cells relative to total tumor-infiltrating lymphocytes in the tumor section. We used whole slides in these cases because we wanted to examine the pattern of tumor-infiltrating lymphocytes and also quantitate the Tregs within and around the whole tumor. The amount of lymphoid tissue in each tumor section was quantitated as the number of lymphoid aggregates within ten contiguous fields of tumor at 20× magnification. This sum was represented as “A.” The quantitation of Tregs in each slide was based on the number of FoxP3-positive lymphocytes within each lymphoid high-power field, 40× magnification, averaged over ten fields, and represented as “B.” These values were multiplied to give a Treg expression index (A × B). The slides of a case of ADC, SCC, and a representative benign case are shown in Figs. 1, 2, and 3, respectively.
a Invasive adenocarcinoma showing multiple lymphoid aggregates interspersed with tumor (H&E, 2× scanning magnification). b The same tumor as in panel A, at 20× magnification, showing three lymphoid aggregates and the edge of a fourth. c FoxP3 IHC of the same case showing lymphocytes with positive nuclear stain (40× magnification)
a Invasive squamous cell carcinoma with tumor necrosis and lymphoid aggregates, mainly at the edge of the tumor toward the top of the photo (H&E, 2× scanning magnification). b The same tumor as in panel A, at 20× magnification, showing two lymphoid aggregates. c FoxP3 IHC of the same case showing a few lymphocytes with positive nuclear stain (40× magnification)
a A benign section of lung, removed for symptomatic bronchiectasis, showing fibrosis and inflammation (H&E, 2× scanning magnification). b The same tumor as in panel A, at 20× magnification, showing a single lymphoid aggregate. c FoxP3 IHC showing very few positive cells within the lymphoid tissue. The macrophages show a high degree of cytoplasmic background. A few specks of anthracotic pigment are seen in the lower-left field (20× magnification)
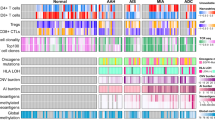
The other half of the cases [12 primary lung carcinomas, each with N1 and N2 draining lymph nodes available (5 squamous cell carcinomas and 7 adenocarcinomas)] were selected for a tissue array. Control tissues consisted of 2 inflammatory lung cases (1 organizing pneumonia and 1 interstitial fibrosis) and 2 mediastinal lymph nodes with sarcoid. Clinically, all of these cases were staged as pN0, except for one case of ADC which was N1, according to the final pathology reports, in accord with AJCC guidelines [16]. No known metastases were present. The array had two 12-mm cores from each of the following: primary tumor, N1 node, N2 node, and control tissue. The array was incubated for 20 min with 1:100 dilution of purified anti-Foxp3 antigen (Biolegend, San Diego, CA). The number of positive cells in each array dot was counted and the average counts were calculated for all cases and for ADC and SCC separately. Statistics were calculated using GraphPad Software, Inc. (La Jolla, CA)
Results
We found differences in the quantity of Tregs in the individual tumor histologies. ADC showed a higher Treg index than SCC (Table 1). The benign inflammatory lung cases were intermediate between ADC and SCC.
In our tissue array, the average number of Treg cells for N1 and N2 draining nodes differed with histology (Table 2). The greatest difference was seen in the N1 nodes. The average N1 Treg count for ADC was 126, and for SCC it was 3.5 (p ≤ 0.008, unpaired t test). The N2 nodes were similar for all cases. Our case of ADC with a positive N1 node showed a high level of Tregs (138), but the highest count was in a case of ADC with benign (N0) nodes (350 Tregs).
We found that whole-slide sections of tumor were needed to evaluate the presence and location of Tregs within lung cancers. No definite pattern was identified in regard to the location of lymph tissue at the tumor interface with normal lung versus within the tumor proper. Tregs were found in both locations. The lung tumors that were represented in the tissue array dots only showed few Tregs, likely as a result of the small sampling. The benign nodes within the array (surgically removed for the evaluation and eventual diagnosis of sarcoid) showed greater numbers of Tregs than SCC but lower than ADC. We did not test any lymph nodes completely unassociated with any pulmonary disease.
Conclusions
A robust immune system can be a great aide to the patient with cancer. Our bodies are under constant immune surveillance. Understanding our immune response could have great therapeutic potential for a disease such as lung cancer, which continues to lead cancer death worldwide. Host lymphocyte response can be a positive prognostic factor in certain tumor types [17]. Within the lung, natural killer cells in greater numbers appear to have antitumor properties [18]. Treg lymphocytes, however, cause a tumor-permissive environment to occur [19]. Metastatic lymph nodes in lung cancer have been shown to have a decrease in NK cells and an increase in Tregs [20]. This study confirms that Treg quantity varies with histology, in both the primary tumor and in the draining lymph nodes. However, we demonstrated that even in benign (N0) lymph nodes, the N1 station nodes were enriched for Tregs in the case of ADC but not SCC. It is possible that the lymphocyte composition within the regional nodes could change as the disease progresses.
In the cases of primary lung tumor, all lymphoid aggregates showed some Foxp3-positive cells, suggesting that Tregs are present in all reactive lymphoid tissue. Our benign tissue also showed lymphoid aggregates, and within these aggregates Tregs were present. Their proportions approximated levels seen in SCC and were far less than in ADC cases. Tumors that induced a greater amount of lymphoid stroma tended to have the greatest Foxp3 index. Within the ADC family of tumors, there were more Tregs present than in SCC. We found no difference in the location of the Treg cells in our whole-slide sections of primary tumor (center of tumor vs. edge of tumor).
It is possible therefore that histology is related to the lymphocyte immune response. Tumors with ADC phenotype have greater numbers of Tregs and, therefore, possibly a weaker immune response compared with tumors with SCC phenotype. The quantitative differences in Tregs suggest that ADC is associated with a more permissive environment for nodal spread versus SCC. This has been found in a similar study [20]. Schneider et al. [20] also found enhancement of Tregs in lymph nodes containing metastatic deposits. Our single case of metastatic thyroid carcinoma to the lung tissue showed the greatest number of Tregs, which supports the tumor-permissive theory. Although we included only one case of tumor metastatic to the lung from a nonlung primary (thyroid), comparatively it had very high numbers of Tregs and may warrant further study of metastatic tumors to the lung.
In the radiology literature, CT scan usage for preoperative mediastinal node staging has shown that nodes with long-axis diameter <1 cm are usually negative for metastasis, and the sensitivity for identifying nodal metastases by CT is higher with SCC than for ADC (81 vs. 50 %, respectively) [21]. This presumably is the result of the “ability” of the ADC to metastasize to the node without increasing the size of the node. Tumor can slip, unprotested, into the node without invoking nodal follicular hyperplasia reactions. This phenomenon may also be partly explained by our findings of significantly increased Treg cells within the N1 nodes of ADC compared to SCC.
In summary, we found that all lung tissues with lymphocyte infiltrates, benign or malignant, contain some Treg cells, but they are greater in ADC than in SCC. In addition, N1 station nodes (benign N0 stage) from patients with ADC lung primary showed enrichment with Tregs compared to SCC.
References
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357:539–545
Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M (1995) Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol 155(3):1151–1164
Sutmuller RP, Van Duivenvoorde LM, Van Elsas A et al (2001) Synergism of cytotoxic T lymphocyte-associated antigen 4 blockade and depletion of CD25 regulatory T cells in antitumor therapy reveals alternative pathways for suppression of autoreactive cytotoxic T lymphocyte responses. J Exp Med 194(6):823–832
Fontenot JD, Gavin MA, Rudensky AY (2003) Foxp3 programs the development and function of CD4 CD25 regulatory T cells. Nat Immunol 4(4):330–336
Hori S, Nomura T, Sakaguchi S (2003) Control of regulatory T cell development by the transcription factor Foxp3. Science 299(5609):1057–1061
Wolf D, Wolf AM, Rumpold H et al (2005) The expression of the regulatory T cell-specific forkhead box transcription factor Foxp3 is associated with poor prognosis in ovarian cancer. Clin Cancer Res 11(23):8326–8331
Liyanage UK, Moore TT, Joo HG et al (2002) Prevalence of regulatory T cells is increased in peripheral blood and tumor microenvironment of patients with pancreas or breast adenocarcinoma. J Immunol 169(5):2756–2761
Sasada T, Kimura M, Yoshida Y, Kanai M, Takabayashi A (2003) CD4CD25 regulatory T cells in patients with gastrointestinal malignancies: possible involvement of regulatory T cells in disease progression. Cancer 98(5):1089–1099
Ichihara F, Kono K, Takahashi A, Kawaida H, Sugai H, Fujii H (2003) Increased populations of regulatory T cells in peripheral blood and tumor-infiltrating lymphocytes in patients with gastric and esophageal cancers. Clin Cancer Res 9(12):4404–4408
Halpern AC, Schuchter LM (1997) Prognostic models in melanoma. Semin Oncol 24(1 Suppl 4):S2–S7
Gajewski TF, Meng Y, Blank C et al (2006) Immune resistance orchestrated by the tumor microenvironment. Immunol Rev 213(1):131–145
Petersen RP, Campa MJ, Sperlazza J et al (2006) Tumor infiltrating Foxp3 regulatory T-cells are associated with recurrence in pathologic stage I NSCLC patients. Cancer 107(12):2866–2872
Shimizu K, Nakata M, Hirami Y, Yukawa T, Maeda A, Tanemoto K (2010) Tumor-infiltrating Foxp3+ regulatory t cells are correlated with cyclooxygenase-2 expression and are associated with recurrence in resected non-small cell lung cancer. J Thorac Oncol 5(5):585–590
Lynch TJ, Bondarenko I, Luft A et al (2011) Ipilimumab in combination with paclitaxel and carboplatin as first-line treatment in stage IIIB/IV non-small-cell lung cancer: results from a randomized, double-blind, multicenter phase II study. J Clin Oncol 30(17):2046–2054
Brahmer JR, Horn L, Antonia S et al (2012) Clinical activity and safety of anti-PD1 (BMS-936558, MDX-1106) in patients with advanced non-small-cell lung cancer. J Clin Oncol 30(2 suppl):abstr 7509
Sobin LH, Gospodarowicz MK, Wittekind C (2009) TNM classification of malignant tumors (International Union against Cancer), 7th edn. Wiley-Blackwell, New York, pp 136–146
Huh JW, Lee JH, Kim HR (2012) Prognostic significance of tumor-infiltrating lymphocytes for patients with colorectal cancer. Arch Surg 147(4):366–372
Esendagli G, Bruderek K, Goldmann T et al (2008) Malignant and nonmalignant lung tissue areas are differentially populated by natural killer cells and regulatory T cells in non-small cell lung cancer. Lung Cancer 59(1):32–40
Woo EY, Yeh H, Chu CS et al (2002) Cutting edge: regulatory T cells from lung cancer patients directly inhibit autologous T cell proliferation. J Immunol 168(9):4272–4276
Schneider T, Kimpfler S, Warth A et al (2011) Foxp3+ regulatory T cells and natural killer cells distinctly infiltrate primary tumors and draining lymph nodes in pulmonary adenocarcinoma. J Thorac Oncol 6(3):432–438
Staples CA, Muller NL, Miller RR, Evans KG, Nelems B (1988) Mediastinal nodes in bronchogenic carcinoma: comparison between CT and mediastinoscopy. Radiology 167(2):367–372
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Black, C.C., Turk, M.J., Dragnev, K. et al. Adenocarcinoma Contains More Immune Tolerance Regulatory T-cell Lymphocytes (Versus Squamous Carcinoma) in Non-small-Cell Lung Cancer. Lung 191, 265–270 (2013). https://doi.org/10.1007/s00408-013-9455-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-013-9455-7