Abstract
Purpose
The purpose of this article is to provide an up-to-date summary of sarcopenia and its clinical implications for patients with head and neck cancer (HNC).
Methods
We conducted a literature review of recent studies investigating the prevalence of sarcopenia in HNC patients, its detection using MRI or CT scans, and its association with clinical outcomes such as disease-free and overall survival time, radiotherapy-related side effects, cisplatin toxicity, and surgical complications.
Results
Sarcopenia, characterized by low skeletal muscle mass (SMM), is a prevalent condition in HNC patients and can be effectively detected using routine MRI or CT scans. Low SMM in HNC patients is associated with increased risks of shorter disease-free and overall survival times, as well as radiotherapy-related side effects such as mucositis, dysphagia, and xerostomia. In addition, cisplatin toxicity is more severe in HNC patients with low SMM, leading to higher dose-limiting toxicity and treatment interruptions. Low SMM may also predict higher risks of surgical complications in head and neck surgery. Identifying sarcopenic patients can aid physicians in better riskstratifying HNC patients for therapeutic or nutritional interventions to improve clinical outcomes.
Conclusions
Sarcopenia is a significant concern for HNC patients and can impact their clinical outcomes. Routine MRI or CT scans can effectively detect low SMM in HNC patients. Identifying sarcopenic patients can aid physicians in better risk-stratifying HNC patients for therapeutic or nutritional interventions to improve clinical outcomes. Further research is needed to explore the potential of interventions to mitigate the negative effects of sarcopenia in HNC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancers (HNC) are among the most common types of cancers globally, with 890,000 new cases and 450,000 deaths each year [1]. These tumors can arise from various areas in the head and neck, such as the pharynx, larynx, oral cavity, and sinonasal cavity. Patients with HNC are typically diagnosed at a locally advanced stage, requiring multidisciplinary treatment with a combination of modalities [2]. Malnutrition is prevalent in 30–50% of HNC patients at the time of diagnosis due to symptoms such as dysphagia, odynophagia, and restrictions on oral nutrition associated with tumor location [3, 4]. Personal habits like excessive alcohol consumption, tobacco use, and long-term inadequate nutritional intake are common risk factors for malnutrition in patients with HNC before treatment [5]. Additionally, metabolic changes associated with cancer, such as early stages of cancer cachexia, can affect nutritional status [5].
Antineoplastic therapies have improved locoregional control and survival in recent years [6, 7]. However, the acute and long-term adverse effects of these treatments may worsen malnutrition due to xerostomia, mucositis-related odynophagia, or anorexia [8]. In addition, there are iatrogenic causes of malnutrition, such as pain or leakage associated with the implanted percutaneous endoscopic gastrostomy tube, unhealthy teeth extraction before radiotherapy, opioid-induced gastrointestinal alterations, and lack of awareness of malnutrition [9]. Skeletal muscle depletion is a typical sign of cancer-related malnutrition, and it may play a role in the progression of sarcopenia [10]. Taken together, malnutrition and skeletal muscle mass (SMM) depletion are significant concerns for patients with HNC because of many reasons aforementioned specific to this population, and are observed much more frequently than other cancer types [11, 12].
As head and neck cancer is a complex and challenging disease to treat, with a high risk of recurrence and metastasis, there is a need for prognostic markers. Recent research has focused on identifying novel prognostic markers for HNC, including molecular biomarkers, pan-immune-inflammation value (PIV), programmed death-ligand 1 (PD-L1) expression in human tissue, genetic markers, and imaging-based markers [13,14,15]. These markers can provide valuable information on tumor biology, treatment response, and patient outcomes and hold great promise for guiding personalized treatment strategies. One such promising nutrition-related biomarker is low skeletal muscle mass, which refers to sarcopenia and has gained interest in recent decades. This article aims to provide an up-to-date summary of sarcopenia and its clinical implications for patients with HNC.
Materials and procedures
We conducted a literature search on the associations between sarcopenia and head and neck cancer patients using the databases PubMed, Google, Web of Science, and EMBASE. We used search terms such as “skeletal muscle mass”, “skeletal muscle index”, “muscle depletion”, “sarcopenia”, “head and neck cancer”, “HNC”, “postoperative complications”, “survival rate”, “prognosis”, “survival” and “toxicity”. We removed duplicate findings and screened the remaining studies for relevance by two authors (Erul E and Guven D). Abstracts, full-text articles that were unavailable, and non-English publications were excluded. We selected randomized controlled trials, meta-analyses, clinical studies, and systematic reviews that were relevant to the topics above.
Sarcopenia measurement
In 2019, the European Working Group on Sarcopenia in Elderly Patients updated the definition of sarcopenia as a muscle disease (muscle failure) with low muscle strength as its primary determinant [16]. Sarcopenia should be considered if reduced muscle strength is observed, and the diagnosis is confirmed by low muscle quality or mass and low muscle strength. Severe sarcopenia is diagnosed when patients have reduced muscle strength, low muscle mass/quality, and poor physical performance [16]. However, muscle function is rarely tested in clinical settings, and the oncology literature has often describes sarcopenia as simply a reduction in muscle mass. Computed tomography (CT) and magnetic resonance imaging (MRI) are already available for staging and follow-up, and SMM could be routinely determined retrospectively and used as an objective risk stratification tool in the clinical context. The association of low muscle mass with cancer-specific adverse outcomes, including treatment toxicity and mortality, has been documented in medical and surgical oncology settings across numerous cancer sites and treatment approaches [17, 18]. As a result, the terms low SMM and sarcopenia are frequently used interchangeably in oncologic research.
There are various methods for evaluation of skeletal muscle mass [16] such as dual-energy X-ray absorptiometry [19, 20], anthropometry [21], bioelectrical impedance analysis [22, 23], MRI/CT [24], and ultrasound [25]. However, dual-energy X-ray absorptiometry, anthropometry, and bioelectrical impedance analysis are not routinely utilized in daily practice and may differ significantly across observers. In the cancer literature, CT and MRI are routinely available as more objective methods for SMM evaluation. The phrase radiologically defined sarcopenia now refers to a more common method of characterizing SMM using MRI/CT scans [26].
Shen et al. demonstrated that measuring cross-sectional muscle area (CSMA) in a single section in the third lumbar (L3) vertebra on the abdomen CT scans is correlated with total body muscle volume [27]. The skeletal muscle index (SMI) can be calculated using the following formula: CSMA at determined CT/MRI level divided by squared height (m2) [28]. However, abdomen CT scans are not routinely performed in patients with HNC, and they expose the patient to additional radiation and cost. Swartz et al. developed a new formula for SMM evaluation at the third cervical vertebra (C3) level of cervical CT. They found a strong correlation between C3 SMI on the head and neck CT and L3 SMI on the abdomen CT (r = 0.785, p < 0.001). The formula that predicts CSMA at the L3 level from C3-level CSMA using weight, age, and gender demonstrated a strong correlation (r = 0.891) between predicted and actual CSMA at the L3 level [12]. Thus, a cervical CT scan can accurately evaluate SMM without the need for additional imaging or burden on the patient (Figs. 1, 2).
Bril et al. also found a strong correlation (Spearman’s rs = 0.75; p = 0.01) between CSMA at L3 and C3, confirming earlier studies in the literature [29]. Several prediction formulas were also demonstrated in the studies showing that cervical and abdominal SMM highly correlate [30,31,32]. To assess the interobserver agreement of this new method, six observers independently measured CSMA at the C3 level on cervical CT in a study. The study demonstrated high interobserver agreement in vertebra selection, single slice selection, and SMM measurement at the C3 level. Intraclass correlation coefficients were excellent for all CSMA measures (0.763–0.969; all p < 0.001) [33]. In another study, high intraobserver and interobserver agreement were found for CSMA, sternocleidomastoid, and paravertebral muscle measurement [34]. Additionally, Olson et al. recently generated normalized gender-specific C3 SMI cut-offs and validated their predictive efficacy in an additional population of HNC patients with cervical CTs. The study showed that C3 SMI cut-offs were predictive in males but not in females in patients with HNC [35].
Recently in a study involving patients with HNC and a healthy population, Yoon et al. investigated the predictive validity of CSMA at C3 for CSMA at L3. They found a high correlation (r = 0.864) between L3 SMM and C3 SMM in healthy participants, as well as in non-sarcopenic individuals with a strong correlation (r = 0.876) [36]. However, the correlation was only fair (r = 0.381) in sarcopenic individuals, which contradicts previous findings. The authors suggested that changes in skeletal mass loss pattern at C3 and L3 might be responsible for this correlation difference. They also cautioned that using cervical CT to assess SMM in sarcopenic individuals with HNC may not be a good predictor of lumbar SMM [36]. Following this study in the Asian cohort, Brit et al. conducted another cohort study involving North-West European HNC patients. They found a strong to excellent correlation between SMM at L3 and C3 in patients with normal and low SMM [37]. However, a recent study by Vangelov et al. reported little agreement between the abdominal and cervical skeletal muscle mass measures. They suggested that estimates of SMM based on C3 cannot substitute accurate data on L3 SMM due to low agreement, relative bias, and incorrect sarcopenia categorization [38].
There are also some caveats that should be mentioned. C3SMI may not be accurately defined in patients with recurrent or locally advanced HNC (LA-HNC), particularly if there is extranodal extension, cervical lymphadenopathy, or muscle wasting due to neck dissection. One possible solution to this problem is to double the measurable sternocleidomastoid side, unless both sternocleidomastoids are invaded by lymphadenopathies [12, 34].
CT scans are not routinely performed for all patients with HNC, and a significant proportion of these patients may only undergo MRI. In a study of 50 patients with oropharyngeal cancer, the correlation between SMM measurement using CT and MRI was analyzed. The study concluded that when evaluating SMM using CSMA at the C3 level, MRI and CT demonstrated a substantial correlation (0.97; 95% CI: 0.94–0.98, p < 0.01) [39]. These findings were supported by Zwart et al., who found a high correlation between cervical MRI and CT. Therefore, MRIs may be utilized as a reliable alternative imaging method when cervical CT is unavailable for SMM measurement [40].
Muscle radiodensity and quality are additional parameters for sarcopenia linked to significant health outcomes. Prado et al. found a correlation between sarcopenia and low muscle radiation attenuation on CT scans in patients with cancer [28]. Pathological variations in muscle attenuation can be caused by excessive intermuscular fat accumulation or poor muscle “quality” [41]. Mapping of psoas/paraspinal muscles for radiation attenuation has demonstrated the phenomenon of myosteatosis [42]. This approach emphasizes that reduced attenuation areas can be found within the radiodensity ranges of adipose tissue, and skeletal muscle can have normal and lower attenuation, indicating worse quality muscle with attenuation zones [41]. Myosteatosis occurs as a preceding shift in muscle structure before a reduction in strength and performance and requires further investigation [43].
Sarcopenia as a prognostic marker
Several studies have demonstrated that low SMM in HNC patients is a risk factor for a decreased survival rate. The majority of these studies have recently been evaluated in the systematic meta-analyses [26, 44,45,46,47]. In a meta-analysis involving 1059 patients with HNC, the pre-treatment incidence of sarcopenia varied from 6.6% to 64.6%, while post-treatment sarcopenia prevalence ranged from 12.4% to 65.8%. Both pre-treatment low SMI (HR 2.07; 95% CI, 1.47–2.92) and post-treatment low SMI (HR 2.93; 95% CI, 2.00–4.29) were associated with a shorter overall survival [46]. Wong et al. also identified a poorer overall survival for HNC patients with low SMM (HR 1.98; 95% CI: 1.64–2.39) in another meta-analysis [26]. In addition, a subgroup analysis of three studies showed that estimated L3 SMM from C3SMM measurement was still a significant predictive factor for identifying overall survival [26]. Hua et al. analyzed data from 11 studies involving almost 2500 patients with HNC and demonstrated consistent findings. Based on both univariate and multivariate analyses, the sarcopenia group had substantially lower relapse-free survival (HR = 1.74, 95% CI: 1.43–2.12, p < 0.00001; HR = 1.68, 95% CI: 1.27–2.23, p = 0.003) [45]. There was no difference in the impact of sarcopenia on the Asian and non-Asian subgroups in the study. Sarcopenia also predicted disease-free survival in patients with HNC in a meta-analysis by Surov and Wienke that included 7704 individuals who received various curative treatment methods (HR 1.64, 95% CI (1.33–2.03), p < 0.00001) [44]. In another meta-analysis of 3233 patients with HNC, sarcopenia predicted poor prognosis in both the radiotherapy (HR 2.50, 95% CI 1.95–3.21) and surgery groups (HR 1.63, 95% CI 1.40–1.90) [47]. Negative impacts of sarcopenia were more noticeable in the surgery group than in the RT group [47]. Based on studies and meta-analyses, low SMM was linked to poor overall survival and disease-free survival regardless of treatment modalities [47], tumor localization [48, 49], region of study population [45], and measurement level [26]. There were also studies combining low SMM and systemic inflammation biomarkers that found higher prognostic effects for survival [50, 51]. Another study on head and neck cancers evaluated combined muscle strength, muscle function, and SMM. When each of them was assessed separately, SMM was not found to be a significant prognostic on overall survival, but in combination, overall survival was statistically lower in sarcopenic patients [52]. In a study with advanced oral cavity cancers, SMI was evaluated at pre-radiotherapy, third month, and ninth-month CT after treatment. The overall survival (HR: 1.88, 95% confidence interval: 1.58–2.23; p < 0.001) of patients with progressive muscle loss throughout the process was significantly lower [53].
Recently, the impact of reduced muscle attenuation in cancer patients on clinical outcomes has gained interest. Martin et al. found that muscle attenuation is an independent predictor of survival in cancer patients, including patients with HNC (HR 1.25, 95% CI 1.07–1.46, p < 0.001) [10]. In another study, Findlay et al. showed that skeletal muscle loss, sarcopenia, or myosteatosis was associated with unplanned hospitalization costs and shorter overall survival in patients with HNC [54]. Baseline myosteatosis may be an independent risk factor for shorter overall survival and might have a greater impact on decreasing overall survival than baseline sarcopenia [54]. Similarly, Yoshimura et al. also revealed that patients with oral squamous carcinoma with high intramuscular adipose content in psoas muscle had reduced overall survival (p < 0.01) [55]. They also found that muscle quality and quantity correlate between C3 and L3 levels and that low muscle quality in the cervical region also decreased overall survival [48].
The relationship between body composition and body mass index (BMI) and prognosis in head and neck cancers is complex, with conflicting studies on this subject in the literature [56]. While it has been established that patients with low BMI and cachectic cancer have a worse prognosis, a study by Prado et al. revealed that obesity, on the other hand, does not preclude the occurrence of cancer cachexia and sarcopenia [28]. The study demonstrated the presence of a sarcopenic obesity group, which is reshaping oncologic research. Increased pre-treatment BMI was found to be associated with better cancer survival in patients with HNC in some studies [57, 58]. Sarcopenia was also similarly linked to a worse overall survival rate regardless of the BMI group, indicating that sarcopenic obesity might be a worse prognostic factor in patients with HNC than BMI [49, 56]. In a recent study of 216 oropharyngeal patients, sarcopenic obesity remained a significant negative prognostic factor for overall survival (HR 4.42; 95% CI 1.52–12.90, p = 0.01) and disease-free survival (HR 3.90; 95% CI 1.03–14.75, p = 0.04) independent of other well-known prognostic factors like HPV status [49].
Patients with head and neck cancer often experience changes in fat distribution in addition to sarcopenia, which can lead to increased morbidity and mortality. Recent studies have suggested that analyzing fat compartments in the head and neck area may also serve as a complementary marker for sarcopenia in patients with HNC. A study by Lee et al. investigated the associations between subcutaneous adipose tissue and visceral adipose features with survival outcomes in patients with HNC [59]. They found that patients with high visceral adipose volume both had superior survival rates compared to patients who were underweight or normal weight and those with a low visceral adipose volume (p < 0.05). These findings suggest that analyzing fat compartments in the head and neck area may also be a useful tool for identifying HNC patients like sarcopenia and may help guide interventions to improve their outcomes. Cancer cachexia, sarcopenia, and sarcopenic obesity can occur at any body weight and BMI, and imaging methods as an opportunistic tool may be useful for identifying occult muscle wasting.
Studies suggest that the combination of skeletal muscle loss and increased adipose tissue may lead to the production and release of proinflammatory cytokines such as interleukin (IL)-1 and IL-6, as well as adipokines like leptin and tumor necrosis factor-alpha [60]. Sarcopenic patients may have decreased levels of myokine, adiponectin, and IL-15, which can inhibit the immune system, specifically natural killer cells [61]. Despite skeletal muscle functioning as an endocrine organ that secretes myokine peptides with antineoplastic activity, and which regulate metabolism, inflammation, immunological function, and adipose tissue oxidation, the mechanism of survival effects on cancer patients is yet to be fully understood [62, 63]. Sarcopenia may also serve as an indicator of overall physical fitness, which can impact surgical complications that may delay or hinder adjuvant therapy, and chemo-radiotherapy complications that may result in treatment cessation. Therefore, sarcopenia should be considered a “vital sign” beyond muscle dysfunction [64].
Sarcopenia as a predictor of toxicity and postoperative complications
In recent decades, there has been increased attention given to body composition and its relationship to treatment-related toxicities. Numerous studies have investigated the role of low SMM in chemotherapy dose-limiting toxicities (CDLT) among patients with HNC. CDLT is defined as any toxicity that results in a 50% reduction in cisplatin dosage, a four-day treatment delay, and cisplatin termination following the first or second treatment cycle or switch to carboplatin. Wendrich et al. conducted a study that showed CDLT occurred more frequently in HNC patients with low SMM compared to those with normal SMM (44.3% vs 13.7%, Fisher’s exact test: p < 0.001, Relative Risk = 3.2). Patients with low SMM had over threefold increased risk for CDLT, and those who experienced CDLT had significantly decreased overall survival compared to those without CDLT (36.6 vs 54.2 months) [65]. Bril and Chargi et al. reported consistent findings that low SMM increased CDLT in HNC patients receiving high-dose cisplatin [66, 67]. Another study with 213 patients with HNC found that low SMM was significantly associated with premature discontinuation of chemotherapy due to toxicity (p = 0.021, OR 0.96 [0.92–0.99]) [68]. Huang et al. demonstrated that chemotherapy dose reduction and modification were more frequent in sarcopenic nasopharyngeal carcinoma patients [69]. A recent study with 92 HNC patients receiving induction chemotherapy (docetaxel, cisplatin, and 5-fluorouracil) found that patients with low SMI experienced more frequent chemotherapy-related toxicity compared to those with higher SMI [70]. These findings suggest that sarcopenia is a predictor of toxicity in patients with HNC, and may have implications for treatment planning and dosing adjustments.
Cisplatin dosage is crucial for effectiveness of chemotherapy, and reduced cumulative cisplatin doses can lead to poorer oncologic outcomes [71]. Clinicians are primarily concerned with suboptimal therapy, including dosage reduction and delays, and therefore, the largest tolerable cisplatin dose is warranted for curative purposes. Several theories have been proposed for cisplatin-related CDLT in sarcopenic patients. Due to the hydrophilic nature of cisplatin, it can bind to fat-free body mass, of which SMM is the largest component. A study by Chargi et al. showed that muscle loss alters the pharmacokinetics of cisplatin, and HNC patients with low SMM have higher-bound cisplatin levels [72]. Low pre-treatment SMM might also be utilized to support a treatment de-escalation strategy, such as weekly low-dose cisplatin, to improve treatment adherence and cumulative cisplatin dosage provided [66].
In a recent study of 61 refractory or metastatic HNC patients who received immunotherapy, no significant relationship was found between low SMM and immunotherapy-related adverse events [73]. Similarly, a study by Huiskamp et al. investigating dose-limiting toxicity in LA-HNC patients receiving cetuximab and radiotherapy found that low SMM had no prognostic role for cetuximab-related dose-limiting toxicity [74].
Radiotherapy to the head and neck region can cause severe adverse effects, such as dysphagia, mucositis, and, eventually, xerostomia. Prolonged radiation (> 8 weeks) due to radiotherapy-related side effects can negatively impact survival outcomes in patients with oral squamous cell carcinoma who receive surgery and adjuvant radiotherapy [75]. Patients with low SMI are particularly at risk of these side effects. In one study, patients with low SMI were more likely to require more than one week of treatment gap due to poor oral intake, infection or mucositis [76]. In another study, over 20% of sarcopenic patients with HNC had a prolonged radiotherapy treatment interruption due to radiotherapy-related esophagitis, mucositis, or dermatitis [77]. However, a recent prospective study found no association between sarcopenia and dysphagia, mucositis, or dermatitis toxicity in either the chemo-radiotherapy or radiotherapy groups of patients with HNC [78]. Nevertheless, grade ≥ 3 mucositis was found to be linked to low SMM in a study with 60 oral cavity cancers who received chemo-radiotherapy after surgery [79]. In another prospective study of 977 patients with HNC; low SMM was associated with physician-rated grade ≥ 3 dysphagia [80]. Interestingly, there is a complex relationship between sarcopenia and dysphagia. Dysphagia as a toxicity may have been seen more frequently in the sarcopenic group due to a vicious cycle between sarcopenia and dysphagia. Dysphagia and malnutrition may result in sarcopenia. Sarcopenia, if swallowing-related muscles are affected, may cause dysphagia and deteriorate malnutrition [80]. Furthermore, Lee et al. found that SMI loss progressively from pre-treatment to the third month after treatment was linked to acute grade ≥ 3 mucositis and grade ≥ 2 dysphagia [53]. Additionally, low SMM in patients with HNC treated with chemo-radiotherapy was found to be a risk factor for aspiration pneumonia [81] and extended feeding tube dependency [82] in studies.
In terms of radiation-induced late toxicity, a study found that sarcopenia was associated significantly with physician-rated xerostomia and physician-rated dysphagia (OR = 2.02 (95% CI = 1.17–3.51), p = 0.012) [83]. These findings suggest that low SMM before treatment can be a predictor of radiotherapy-related acute and late toxicity in patients with HNC.
Several studies have investigated the impact of radiation therapy on muscle function in patients with head and neck cancer [84, 85]. Radiotherapy is designed to destroy cancer cells by delivering high-energy radiation to the cancerous tissue, but it can also damage healthy tissue in the surrounding area, including the muscles [86]. The muscles in the head and neck region are particularly vulnerable to radiation damage because they are small and located close to the target area. Radiation therapy can cause significant muscle atrophy and weakness in patients with HNC [84, 86]. A study by van der Molen et al. found that radiation therapy led to a significant decline in muscle strength and endurance in patients with HNC [87]. Patients may experience muscle weakness, stiffness, and fatigue, which can significantly affect their quality of life [88]. The severity of muscle damage depends on several factors, such as the total radiation dose, the fractionation schedule, and the type of radiation used [89]. Radiation oncologists use various techniques to minimize the risk of muscle damage during treatment. For instance, intensity-modulated radiation therapy [90] and proton therapy [91] can deliver radiation more precisely, thereby minimizing exposure to healthy tissue, including the muscles. In addition, some patients may be candidates for brachytherapy [92], which involves placing radioactive seeds directly into the tumor or surrounding tissue, further reducing exposure to healthy tissue.
Sarcopenia has been identified as an independent unfavorable prognostic factor for various postoperative complications in patients undergoing surgery for head and neck cancer. These complications include wound complications [93, 94], pharyngocutaneous fistula [93,94,95,96], prolonged hospital stay [94, 97], flap-specific complications [94, 98], readmission [99], blood transfusion requirement [100], and surgical site infection [101].
In a study by Achim et al., the impact of preoperative low SMM on pharyngocutaneous fistula development, wound complications, and postoperative complications was assessed in patients with HNC undergoing total laryngectomy [93]. The study found that 24% of sarcopenic patients developed pharyngocutaneous fistula, while it was not observed in the non-sarcopenic group. Additionally, 50% of sarcopenic patients experienced wound complications, compared to only 13% of non-sarcopenic patients. Sarcopenia was identified as an independent adverse prognostic factor for the development of all post-total laryngectomy pharyngocutaneous fistula and wound complications [93].
In another study, Ansari et al. found that low SMM was a negative predictor of free fibula flap problems in patients with HNC who underwent free fibula flap reconstruction, regardless of age, comorbidity, ischemia duration, or smoking [98]. Additionally, a study of 122 patients with oral cancer reported that low SMM was a significant independent predictor of surgical site infection (p = 0.015, OR = 1.41 for 5 cm2/m2 drop) [101]. Orzell et al. defined sarcopenia as low SMM with low muscle strength and assessed the impact on major surgical complications in HNC patients, finding that sarcopenia was associated with longer hospital stay [97]. Jones et al. found that patients with low SMM were more likely to require transfusions during surgery. They suggested that transfusion-related complications might also be more frequent in this population, and this should be taken into account when blood products are scarce prior to surgery [100].
Sarcopenic patients may have reduced physiological capacity to recover after surgery and lower tolerance to surgical stress due to alterations in protein metabolism [93]. The preoperative evaluation of SMM could aid in identifying high-risk patients for severe complications and serve as a prediction tool in clinical practice. A robust evaluation of sarcopenia may provide an opportunity for nutrition optimization before surgery, which could lower the likelihood of complications following surgery.
Exercise and nutritional intervention to improve muscle quantity and quality in head and neck
Cancer survivors
Our review also focuses on the regular evaluation and treatment of sarcopenia in patients with HNC. A multidisciplinary approach, including rehabilitation therapists, psychiatrists, otolaryngologists, medical oncologists, and radiation oncologists is essential in the treatment of patients with HNC. Given significant physical, psychological, and social effects of HNC cancers on patients, an interdisciplinary approach aids in optimally planning and managing their treatment [102]. Managing and preventing sequelae such as dry mouth, swallowing and speech difficulty, and depression after surgery and systemic therapy, requires regular follow-up and evaluation by professionals familiar with the disease [103]. Patients are at risk of depression from head and neck cancer, therefore screening for depression is recommended [103]. Dental healthcare should be performed before treatment to reduce the risk of side effects after radiotherapy. Patients should be referred to a dietitian at diagnosis, during and after treatment since adequate nutritional support can help prevent severe weight loss in patients with head and neck cancers [104].
While therapeutic and nutritional interventions in head and neck cancer can pose challenges, there are established approaches that can be applied from other cancer types, such as pancreatic cancer [105]. One example of an interdisciplinary approach that has been examined in pancreatic cancer is the use of nutritional and exercise interventions to prevent or manage sarcopenia [105, 106]. These interventions may involve working with a team of healthcare professionals, including dietitians, exercise physiologists, and physical therapists, to develop individualized exercise and dietary plans to help patients maintain or improve their muscle mass and strength.
Overall, the current findings regarding the detrimental effects of sarcopenia are clinically significant because sarcopenia is a potentially modifiable condition, and early detection of vulnerable patients may allow for therapeutic intervention to reduce treatment-related adverse events. Lifestyle changes, particularly dietary patterns and treatment procedures have all been suggested [107]. The most common interventions for sarcopenia include protein supplements, calorie intake, and regular resistance training (both resistance and aerobic) aimed at enhancing muscle mass and strength [108, 109]. In a recent study, although it did not reach statistical significance, patients with laryngeal and oropharyngeal cancer who complied with frequent dietetic counseling and contact after receiving definitive radiotherapy tended to have better clinical progression-free survival and overall survival [5]. Additionally, sarcopenia is linked to the development of cancer-related exhaustion in patients with HNC, and increasing muscle mass through resistance training may help to reduce exhaustion and enhance well-being [110]. In a study, Lønbro et al. showed that there were significant correlations between lean body mass, maximum muscular strength, and functional performance. Patients with HNC had worse values of these variables than healthy people after radiation, although these impairments were corrected after 3 months of resistance training [111]. Preventive swallowing exercises have been studied in individuals with HNC receiving chemo-radiotherapy to enhance swallowing function before or during therapy. Post-treatment swallowing function improved as a result of these therapies [112]. However, in a prospective study with 243 patients with HNC receiving radiotherapy or chemo-radiotherapy, adverse outcomes of sarcopenia on survival still existed despite adequate nutrition management with dietician consultation [78]. A randomized study with a small sample size in patients with HNC found that a three-month lifestyle and exercise program during radiotherapy had no significant impact on the primary endpoint of body composition [113]. This inconsistency may be due to the small sample size of the study as a limitation. Recently, in a study of patients with oropharyngeal carcinoma, a large proportion of patients still had functional impairments in swallowing, mouth opening, and speech function (25%, 20%, and 58%, respectively) after radiotherapy, despite the implementation of a focused rehabilitation program for prevention [114].
Management of malnutrition and sarcopenia could be challenging since the time period between HNC diagnosis and radiotherapy is typically short, as noted in previous research [78]. As a result, it remains unclear to what extent a patient’s physical condition and nutritional health could be improved before and during therapy to mitigate the detrimental consequences of sarcopenia. Future research is needed to investigate these processes more thoroughly in the future.
Discussion and future perspectives
Numerous studies with convincing evidence have shown that sarcopenia in HNC is associated with poor prognosis, poor surgical outcomes, and an increased risk of complications and chemo-radiotherapy toxicity. However, there is still room for improvement in muscle measurement, statistical analyses and validated sex- and region-specific standard cut-point values for the diagnosis. SMI cut-point values for diagnosing sarcopenic individuals should be addressed since there is no consensus in the literature [34] (Table 1). In studies, patients with HNC are stratified as low SMI and normal SMI using statistical techniques such as dichotomization according to various SMI cut of values [31, 46]. Patients with low SMI under the cut-point values are assumed to have the same risk of toxicity and risk of death and vice versa. However, this approach obscures true dose–response relationships, and analytic limitations need to be improved in future studies [115, 116]. According to the definition of Prada et al. [28], L3SMI cut-off values (55 cm2/m2 for men, 38.5 cm2/m2 for women) indicate that both SMI values of 50 and 20 are sarcopenic and have the same risk. Similarly, a woman with a SMI of 39 is not sarcopenic, while a woman with a SMI of 38 is sarcopenic. Despite the benefits of imaging methods, the incidence of aberrant muscle features in patients with HNC and the assessment of sarcopenia varies greatly between studies. Many studies in the literature have identified sarcopenia using skeletal mass indices with heterogenous cut-offs [117, 118] from various body areas, such as the infrahyoid [119], temporal [120], masticatory muscle [121], and lumbar paravertebral muscle [122]. In this scenario, no sentinel muscle for sarcopenia assessment has been approved, making the literature data difficult to interpret [123]. Additional studies are required to address these issues and establish age, sex, and race-specific reference values for CSMA at the level of C3 or L3 for diagnosis of sarcopenia.
In the field of sarcopenia, an area that could be explored in future research is myosteatosis. Since muscle structure and composition vary with micro and macroscopic aspects, investigating myosteatosis could provide insights into muscle quality. Developing diagnostic criteria for low muscle attenuation and a systematic technique for quantifying myosteatosis would be beneficial to this emerging field of study. More research is needed to use muscle quality as the primary parameter for defining sarcopenia and specifying therapy for myosteatosis [16]. Secondly, creating biorepositories and automated software utilizing artificial intelligence, such as machine learning and deep learning, are promising area [124, 125]. These technologies would provide a more accurate, automatic measurement of total muscle volume according to MRI or CT imaging, making SMM measurement easier to implement in clinical practice [124]. The time it takes to evaluate sarcopenia in a clinical context is a limiting factor, and these instruments could yield precise body composition data in seconds without manual effort [125, 126]. There is also substantial variability in anatomy at a single section, such as C3 or L3, suggesting that single-section analysis is of limited use. Using high technology for body composition analysis on individuals with 3D analysis is a more accurate technique [126, 127].
Conclusion
Patients with HNC are at a high risk of malnutrition and sarcopenia. Simple and reliable methods to detect SMM exist, such as routine MRI or CT scans of the head and neck cancers. However, using abdominal CT imaging to detect sarcopenia is not practical as it is rarely used in routine practice for patients with HNC. Low SMM in patients with HNC is significantly associated with shorter disease-free and overall survival time. Additionally, cisplatin and radiation toxicity are more severe in patients with HNC with low SMM, resulting in higher dose-limiting toxicity and treatment interruptions. In head and neck surgery, a low SMM could predict surgical complications. Identifying sarcopenic patients could help physicians with better risk stratification for therapeutic or nutritional interventions to improve clinical outcomes in patients with HNC. Therefore, international collaborations are needed to develop a methodological agreement and reporting standards in sarcopenia research to validate these findings and provide their application in a clinical setting.
References
Global Cancer Observatory (2021) International agency for research on cancer. World Health Organization. https://gco.iarc.fr/. Accessed June 06, 2021
Chow LQM (2020) Head and neck cancer. N Engl J Med 382:60–72. https://doi.org/10.1056/NEJMra1715715
Alshadwi A, Nadershah M, Carlson ER et al (2013) Nutritional considerations for head and neck cancer patients: a review of the literature. J Oral Maxillofac Surg 71:1853–1860. https://doi.org/10.1016/j.joms.2013.04.028
Dewansingh P, Bras L, ter Beek L et al (2023) Malnutrition risk and frailty in head and neck cancer patients: coexistent but distinct conditions. Eur Arch Otorhinolaryngol 280:1893–1902. https://doi.org/10.1007/s00405-022-07728-6
Kabarriti R, Bontempo A, Romano M et al (2018) The impact of dietary regimen compliance on outcomes for HNSCC patients treated with radiation therapy. Support Care Cancer 26:3307–3313. https://doi.org/10.1007/s00520-018-4198-x
Bauml J, Seiwert TY, Pfister DG et al (2017) Pembrolizumab for platinum-and cetuximab-refractory head and neck cancer: results from a single-arm, phase II study. J Clin Oncol 35:1542
Mesía R, Garcia-Saenz JA, Lozano A et al (2017) Could the addition of cetuximab to conventional radiation therapy improve organ preservation in those patients with locally advanced larynx cancer who respond to induction chemotherapy? An organ preservation Spanish Head and Neck Cancer Cooperative Group Phase 2 study. Int J Radiat Oncol Biol Phys 97:473–480
Mason H, DeRubeis MB, Burke N et al (2016) Symptom management during and after treatment with concurrent chemoradiotherapy for oropharyngeal cancer: a review of the literature and areas for future research. World J Clin Oncol 7:220
Gorenc M, Kozjek NR, Strojan P (2015) Malnutrition and cachexia in patients with head and neck cancer treated with (chemo)radiotherapy. Rep Pract Oncol Radiother 20:249–258. https://doi.org/10.1016/j.rpor.2015.03.001
Martin L, Gioulbasanis I, Senesse P et al (2020) Cancer-associated malnutrition and CT-defined sarcopenia and myosteatosis are endemic in overweight and obese patients. J Parenter Enter Nutr 44:227–238. https://doi.org/10.1002/jpen.1597
Pressoir M, Desné S, Berchery D et al (2010) Prevalence, risk factors and clinical implications of malnutrition in French Comprehensive Cancer Centres. Br J Cancer 102:966–971. https://doi.org/10.1038/sj.bjc.6605578
Swartz JE, Pothen AJ, Wegner I et al (2016) Feasibility of using head and neck CT imaging to assess skeletal muscle mass in head and neck cancer patients. Oral Oncol 62:28–33. https://doi.org/10.1016/j.oraloncology.2016.09.006
Guven DC, Erul E, Yilmaz F et al (2022) The association between pan-immune-inflammation value and survival in head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-022-07804-x
Zwart AT, Cavalheiro VJ, Lamers MJ et al (2023) The validation of low-dose CT scans from the [18F]-FDG PET-CT scan to assess skeletal muscle mass in comparison with diagnostic neck CT scans. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-023-06117-3
Yadav AK, Singh N, Yadav SK et al (2023) Expression of miR-145 and miR-18b in peripheral blood samples of head and neck cancer patients. Indian J Clin Biochem. https://doi.org/10.1007/s12291-023-01119-2
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Shachar SS, Williams GR, Muss HB et al (2016) Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer 57(58–67):20160213. https://doi.org/10.1016/j.ejca.2015.12.030
Kazemi-Bajestani SM, Mazurak VC, Baracos V (2016) Computed tomography-defined muscle and fat wasting are associated with cancer clinical outcomes. Semin Cell Dev Biol 54(2–10):20150903. https://doi.org/10.1016/j.semcdb.2015.09.001
Buckinx F, Landi F, Cesari M et al (2018) Pitfalls in the measurement of muscle mass: a need for a reference standard. J Cachexia Sarcopenia Muscle 9(269–278):20180119. https://doi.org/10.1002/jcsm.12268
Hull H, He Q, Thornton J et al (2009) iDXA, Prodigy, and DPXL dual-energy X-ray absorptiometry whole-body scans: a cross-calibration study. J Clin Densitom 12(95–102):20081122. https://doi.org/10.1016/j.jocd.2008.09.004
Landi F, Onder G, Russo A et al (2014) Calf circumference, frailty and physical performance among older adults living in the community. Clin Nutr 33(539–544):20130731. https://doi.org/10.1016/j.clnu.2013.07.013
Rossi AP, Fantin F, Micciolo R et al (2014) Identifying sarcopenia in acute care setting patients. J Am Med Dir Assoc 15:303.e307-312. https://doi.org/10.1016/j.jamda.2013.11.018
Lapornik N, AvramovičBrumen B, Plavc G et al (2023) Influence of fat-free mass index on the survival of patients with head and neck cancer. Eur Arch Otorhinolaryngol 280:1909–1917. https://doi.org/10.1007/s00405-022-07732-w
Beaudart C, McCloskey E, Bruyère O et al (2016) Sarcopenia in daily practice: assessment and management. BMC Geriatr 16(170):20161005. https://doi.org/10.1186/s12877-016-0349-4
Ticinesi A, Narici MV, Lauretani F et al (2018) Assessing sarcopenia with vastus lateralis muscle ultrasound: an operative protocol. Aging Clin Exp Res 30(1437–1443):20180426. https://doi.org/10.1007/s40520-018-0958-1
Wong A, Zhu D, Kraus D et al (2021) Radiologically defined sarcopenia affects survival in head and neck cancer: a meta-analysis. Laryngoscope 131:333–341. https://doi.org/10.1002/lary.28616
Shen W, Punyanitya M, Wang Z et al (2004) Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol 97:2333–2338. https://doi.org/10.1152/japplphysiol.00744.2004
Prado CMM, Lieffers JR, McCargar LJ et al (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9:629–635. https://doi.org/10.1016/S1470-2045(08)70153-0
Bril SI, Chargi N, Wendrich AW et al (2021) Validation of skeletal muscle mass assessment at the level of the third cervical vertebra in patients with head and neck cancer. Oral Oncol 123:105617. https://doi.org/10.1016/j.oraloncology.2021.105617
Jung AR, Roh J-L, Kim JS et al (2019) Efficacy of head and neck computed tomography for skeletal muscle mass estimation in patients with head and neck cancer. Oral Oncol 95:95–99. https://doi.org/10.1016/j.oraloncology.2019.06.009
Lu X, Tian Y, Huang J et al (2021) Evaluating the prognosis of oral squamous cell carcinoma patients via L3 skeletal muscle index. Oral Dis. https://doi.org/10.1111/odi.14074
Vangelov B, Bauer J, Moses D et al (2023) A prediction model for skeletal muscle evaluation and computed tomography-defined sarcopenia diagnosis in a predominantly overweight cohort of patients with head and neck cancer. Eur Arch Otorhinolaryngol 280:321–328. https://doi.org/10.1007/s00405-022-07545-x
Bril SI, Wendrich AW, Swartz JE et al (2019) Interobserver agreement of skeletal muscle mass measurement on head and neck CT imaging at the level of the third cervical vertebra. Eur Arch Otorhinolaryngol 276:1175–1182. https://doi.org/10.1007/s00405-019-05307-w
Zwart AT, van der Hoorn A, van Ooijen PMA et al (2019) CT-measured skeletal muscle mass used to assess frailty in patients with head and neck cancer. J Cachexia Sarcopenia Muscle 10:1060–1069. https://doi.org/10.1002/jcsm.12443
Olson B, Edwards J, Degnin C et al (2022) Establishment and validation of pre-therapy cervical vertebrae muscle quantification as a prognostic marker of sarcopenia in patients with head and neck cancer. Front Oncol. https://doi.org/10.3389/fonc.2022.812159
Yoon J-K, Jang JY, An Y-S et al (2021) Skeletal muscle mass at C3 may not be a strong predictor for skeletal muscle mass at L3 in sarcopenic patients with head and neck cancer. PLoS ONE 16:e0254844. https://doi.org/10.1371/journal.pone.0254844
Bril SI, van Beers MA, Chargi N et al (2021) Skeletal muscle mass at C3 is a strong predictor for skeletal muscle mass at L3 in sarcopenic and non-sarcopenic patients with head and neck cancer. Oral Oncol 122:105558. https://doi.org/10.1016/j.oraloncology.2021.105558
Vangelov B, Bauer J, Moses D et al (2022) The effectiveness of skeletal muscle evaluation at the third cervical vertebral level for computed tomography-defined sarcopenia assessment in patients with head and neck cancer. Head Neck 44:1047–1056. https://doi.org/10.1002/hed.27000
Chargi N, Ansari E, Huiskamp LFJ et al (2019) Agreement between skeletal muscle mass measurements using computed tomography imaging and magnetic resonance imaging in head and neck cancer patients. Oral Oncology 99:104341. https://doi.org/10.1016/j.oraloncology.2019.06.022
Zwart AT, Becker J-N, Lamers MJ et al (2021) Skeletal muscle mass and sarcopenia can be determined with 1.5-T and 3-T neck MRI scans, in the event that no neck CT scan is performed. Eur Radiol 31:4053–4062. https://doi.org/10.1007/s00330-020-07440-1
Prado CM, Cushen SJ, Orsso CE et al (2016) Sarcopenia and cachexia in the era of obesity: clinical and nutritional impact. Proc Nutr Soc 75:188–198. https://doi.org/10.1017/S0029665115004279
Aubrey J, Esfandiari N, Baracos VE et al (2014) Measurement of skeletal muscle radiation attenuation and basis of its biological variation. Acta Physiol (Oxf) 210:489–497. https://doi.org/10.1111/apha.12224
Zamboni M, Gattazzo S, Rossi AP (2019) Myosteatosis: a relevant, yet poorly explored element of sarcopenia. Eur Geriatr Med 10:5–6. https://doi.org/10.1007/s41999-018-0134-3
Surov A, Wienke A (2021) Low skeletal muscle mass predicts relevant clinical outcomes in head and neck squamous cell carcinoma. A meta analysis. Ther Adv Med Oncol 13:17588359211008844. https://doi.org/10.1177/17588359211008844
Hua X, Liu S, Liao J-F et al (2020) When the loss costs too much: a systematic review and meta-analysis of sarcopenia in head and neck cancer. Front Oncol 9:1561–1561. https://doi.org/10.3389/fonc.2019.01561
Findlay M, White K, Stapleton N et al (2021) Is sarcopenia a predictor of prognosis for patients undergoing radiotherapy for head and neck cancer? A meta-analysis. Clin Nutr 40:1711–1718. https://doi.org/10.1016/j.clnu.2020.09.017
Takenaka Y, Takemoto N, Oya R et al (2021) Prognostic impact of sarcopenia in patients with head and neck cancer treated with surgery or radiation: a meta-analysis. PLoS One 16:e0259288. https://doi.org/10.1371/journal.pone.0259288
Yoshimura T, Suzuki H, Takayama H et al (2021) Prognostic role of preoperative sarcopenia evaluation of cervical muscles with long-term outcomes of patients with oral squamous cell carcinoma. Cancers 13:4725. https://doi.org/10.3390/cancers13184725
Chargi N, Bril SI, Swartz JE et al (2020) Skeletal muscle mass is an imaging biomarker for decreased survival in patients with oropharyngeal squamous cell carcinoma. Oral Oncol 101:104519. https://doi.org/10.1016/j.oraloncology.2019.104519
Yamahara K, Mizukoshi A, Lee K et al (2021) Sarcopenia with inflammation as a predictor of survival in patients with head and neck cancer. Auris Nasus Larynx 48:1013–1022. https://doi.org/10.1016/j.anl.2021.03.021
Lee J, Liu S-H, Dai K-Y et al (2021) Sarcopenia and systemic inflammation synergistically impact survival in oral cavity cancer. Laryngoscope 131:E1530–E1538. https://doi.org/10.1002/lary.29221
Chargi N, Bril SI, Emmelot-Vonk MH et al (2019) Sarcopenia is a prognostic factor for overall survival in elderly patients with head-and-neck cancer. Eur Arch Otorhinolaryngol 276:1475–1486. https://doi.org/10.1007/s00405-019-05361-4
Lee J, Liu SH, Chen JC et al (2021) Progressive muscle loss is an independent predictor for survival in locally advanced oral cavity cancer: a longitudinal study. Radiother Oncol 158:83–89. https://doi.org/10.1016/j.radonc.2021.02.014
Findlay M, Brown C, De Abreu LR et al (2020) Sarcopenia and myosteatosis in patients undergoing curative radiotherapy for head and neck cancer: Impact on survival, treatment completion, hospital admission and cost. J Hum Nutr Diet 33:811–821. https://doi.org/10.1111/jhn.12788
Yoshimura T, Suzuki H, Takayama H et al (2020) Impact of preoperative low prognostic nutritional index and high intramuscular adipose tissue content on outcomes of patients with oral squamous cell carcinoma. Cancers 12:3167. https://doi.org/10.3390/cancers12113167
Fattouh M, Chang GY, Ow TJ et al (2019) Association between pretreatment obesity, sarcopenia, and survival in patients with head and neck cancer. Head Neck 41:707–714. https://doi.org/10.1002/hed.25420
Hicks DF, Bakst R, Doucette J et al (2018) Impact of obesity on outcomes for patients with head and neck cancer. Oral Oncol 83:11–17. https://doi.org/10.1016/j.oraloncology.2018.05.027
Albergotti WG, Davis KS, Abberbock S et al (2016) Association of pretreatment body mass index and survival in human papillomavirus positive oropharyngeal squamous cell carcinoma. Oral Oncol 60:55–60. https://doi.org/10.1016/j.oraloncology.2016.07.003
Lee JW, Ban MJ, Park JH et al (2019) Visceral adipose tissue volume and CT-attenuation as prognostic factors in patients with head and neck cancer. Head Neck 41:1605–1614. https://doi.org/10.1002/hed.25605
Tilg H, Moschen AR (2006) Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol 6:772–783. https://doi.org/10.1038/nri1937
Lutz CT, Quinn LS (2012) Sarcopenia, obesity, and natural killer cell immune senescence in aging: altered cytokine levels as a common mechanism. Aging (Albany NY) 4:535–546. https://doi.org/10.18632/aging.100482
Anandavadivelan P, Lagergren P (2016) Cachexia in patients with oesophageal cancer. Nat Rev Clin Oncol 13:185–198. https://doi.org/10.1038/nrclinonc.2015.200
Pratesi A, Tarantini F, Di Bari M (2013) Skeletal muscle: an endocrine organ. Clin Cases Miner Bone Metab 10:11–14. https://doi.org/10.11138/ccmbm/2013.10.1.011
Bone AE, Hepgul N, Kon S et al (2017) Sarcopenia and frailty in chronic respiratory disease. Chron Respir Dis 14:85–99. https://doi.org/10.1177/1479972316679664
Wendrich AW, Swartz JE, Bril SI et al (2017) Low skeletal muscle mass is a predictive factor for chemotherapy dose-limiting toxicity in patients with locally advanced head and neck cancer. Oral Oncol 71:26–33. https://doi.org/10.1016/j.oraloncology.2017.05.012
Bril SI, Al-Mamgani A, Chargi N et al (2022) The association of pretreatment low skeletal muscle mass with chemotherapy dose-limiting toxicity in patients with head and neck cancer undergoing primary chemoradiotherapy with high-dose cisplatin. Head Neck 44:189–200. https://doi.org/10.1002/hed.26919
Chargi N, Bashiri F, Wendrich AW et al (2022) Image-based analysis of skeletal muscle mass predicts cisplatin dose-limiting toxicity in patients with locally advanced head and neck cancer. Eur Arch Otorhinolaryngol 279:3685–3694. https://doi.org/10.1007/s00405-021-07229-y
Sealy MJ, Dechaphunkul T, van der Schans CP et al (2020) Low muscle mass is associated with early termination of chemotherapy related to toxicity in patients with head and neck cancer. Clin Nutr 39:501–509. https://doi.org/10.1016/j.clnu.2019.02.029
Huang X, Lv LN, Zhao Y et al (2021) Is skeletal muscle loss associated with chemoradiotherapy toxicity in nasopharyngeal carcinoma patients? A prospective study. Clin Nutr 40:285–302. https://doi.org/10.1016/j.clnu.2020.05.020
Lere-Chevaleyre A, Bernadach M, Lambert C et al (2022) Toxicity of induction chemotherapy in head and neck cancer: the central role of skeletal muscle mass. Head Neck 44:681–690. https://doi.org/10.1002/hed.26954
Mehanna H, Robinson M, Hartley A et al (2019) Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. Lancet 393:51–60
Chargi N, Molenaar-Kuijsten L, Huiskamp LFJ et al (2022) The association of cisplatin pharmacokinetics and skeletal muscle mass in patients with head and neck cancer: the prospective PLATISMA study. Eur J Cancer 160:92–99. https://doi.org/10.1016/j.ejca.2021.10.010
Arribas L, Plana M, Taberna M et al (2021) Predictive value of skeletal muscle mass in recurrent/metastatic head and neck squamous cell carcinoma patients treated with immune checkpoint inhibitors. Front Oncol. https://doi.org/10.3389/fonc.2021.699668
Huiskamp LFJ, Chargi N, Devriese LA et al (2020) The predictive and prognostic value of low skeletal muscle mass for dose-limiting toxicity and survival in head and neck cancer patients receiving concomitant cetuximab and radiotherapy. Eur Arch Otorhinolaryngol 277:2847–2858. https://doi.org/10.1007/s00405-020-05972-2
Cheng Y-J, Tsai M-H, Chiang C-J et al (2018) Adjuvant radiotherapy after curative surgery for oral cavity squamous cell carcinoma and treatment effect of timing and duration on outcome—a Taiwan Cancer Registry national database analysis. Cancer Med 7:3073–3083. https://doi.org/10.1002/cam4.1611
Nagpal P, Pruthi DS, Pandey M et al (2021) Impact of sarcopenia in locally advanced head and neck cancer treated with chemoradiation: an Indian tertiary care hospital experience. Oral Oncol 121:105483. https://doi.org/10.1016/j.oraloncology.2021.105483
Ganju RG, Morse R, Hoover A et al (2019) The impact of sarcopenia on tolerance of radiation and outcome in patients with head and neck cancer receiving chemoradiation. Radiother Oncol 137:117–124. https://doi.org/10.1016/j.radonc.2019.04.023
Thureau S, Lebret L, Lequesne J et al (2021) Prospective evaluation of sarcopenia in head and neck cancer patients treated with radiotherapy or radiochemotherapy. Cancers (Basel). https://doi.org/10.3390/cancers13040753
Yamaguchi T, Makiguchi T, Nakamura H et al (2021) Impact of muscle volume loss on acute oral mucositis in patients undergoing concurrent chemoradiotherapy after oral cancer resection. Int J Oral Maxillofac Surg 50:1195–1202. https://doi.org/10.1016/j.ijom.2020.12.005
Karavolia E, van Rijn-Dekker MI, Van den Bosch L et al (2022) Impact of sarcopenia on acute radiation-induced toxicity in head and neck cancer patients. Radiother Oncol. https://doi.org/10.1016/j.radonc.2022.03.009
Endo K, Ueno T, Hirai N et al (2021) Low skeletal muscle mass is a risk factor for aspiration pneumonia during chemoradiotherapy. Laryngoscope 131:E1524–E1529. https://doi.org/10.1002/lary.29165
Karsten RT, Al-Mamgani A, Bril SI et al (2019) Sarcopenia, a strong determinant for prolonged feeding tube dependency after chemoradiotherapy for head and neck cancer. Head Neck 41:4000–4008. https://doi.org/10.1002/hed.25938
van Rijn-Dekker MI, van den Bosch L, van den Hoek JGM et al (2020) Impact of sarcopenia on survival and late toxicity in head and neck cancer patients treated with radiotherapy. Radiother Oncol 147:103–110. https://doi.org/10.1016/j.radonc.2020.03.014
Kumarasiri A, Liu C, Kamal M et al (2017) Changes in pharyngeal constrictor volumes during head and neck radiation therapy: implications for dose delivery. J Cancer Res Ther 13:218–223
Mogadas S, Busch C-J, Pflug C et al (2020) Influence of radiation dose to pharyngeal constrictor muscles on late dysphagia and quality of life in patients with locally advanced oropharyngeal carcinoma. Strahlenther Onkol 196:522–529
Chiu Y-H, Tseng W-H, Ko J-Y et al (2022) Radiation-induced swallowing dysfunction in patients with head and neck cancer: a literature review. J Formos Med Assoc 121:3–13. https://doi.org/10.1016/j.jfma.2021.06.020
van der Molen L, Heemsbergen WD, de Jong R et al (2013) Dysphagia and trismus after concomitant chemo-intensity-modulated radiation therapy (chemo-IMRT) in advanced head and neck cancer; dose–effect relationships for swallowing and mastication structures. Radiother Oncol 106:364–369. https://doi.org/10.1016/j.radonc.2013.03.005
Brook I (2020) Late side effects of radiation treatment for head and neck cancer. Radiat Oncol J 38:84–92. https://doi.org/10.3857/roj.2020.00213
Kim JH, Jenrow KA, Brown SL (2014) Mechanisms of radiation-induced normal tissue toxicity and implications for future clinical trials. Radiat Oncol J 32:103–115. https://doi.org/10.3857/roj.2014.32.3.103
Hong TS, Ritter MA, Tomé WA et al (2005) Intensity-modulated radiation therapy: emerging cancer treatment technology. Br J Cancer 92:1819–1824. https://doi.org/10.1038/sj.bjc.6602577
Liu H, Chang JY (2011) Proton therapy in clinical practice. Chin J Cancer 30:315–326. https://doi.org/10.5732/cjc.010.10529
Bhalavat R, Budrukkar A, Laskar SG et al (2020) Brachytherapy in head and neck malignancies: Indian Brachytherapy Society (IBS) recommendations and guidelines. J Contemp Brachyther 12:501–511. https://doi.org/10.5114/jcb.2020.100385
Achim V, Bash J, Mowery A et al (2017) Prognostic indication of sarcopenia for wound complication after total laryngectomy. JAMA Otolaryngol Head Neck Surg 143:1159–1165. https://doi.org/10.1001/jamaoto.2017.0547
Alwani MM, Jones AJ, Novinger LJ et al (2020) Impact of sarcopenia on outcomes of autologous head and neck free tissue reconstruction. J Reconstr Microsurg 36:369–378. https://doi.org/10.1055/s-0040-1701696
Bril SI, Pezier TF, Tijink BM et al (2019) Preoperative low skeletal muscle mass as a risk factor for pharyngocutaneous fistula and decreased overall survival in patients undergoing total laryngectomy. Head Neck 41:1745–1755. https://doi.org/10.1002/hed.25638
Casasayas M, García-Lorenzo J, Gómez-Ansón B et al (2022) Low skeletal muscle mass assessed directly from the 3rd cervical vertebra can predict pharyngocutaneous fistula risk after total laryngectomy in the male population. Eur Arch Otorhinolaryngol 279:853–863. https://doi.org/10.1007/s00405-021-07127-3
Orzell S, Verhaaren BFJ, Grewal R et al (2022) Evaluation of sarcopenia in older patients undergoing head and neck cancer surgery. Laryngoscope 132:356–363. https://doi.org/10.1002/lary.29782
Ansari E, Chargi N, van Gemert JTM et al (2020) Low skeletal muscle mass is a strong predictive factor for surgical complications and a prognostic factor in oral cancer patients undergoing mandibular reconstruction with a free fibula flap. Oral Oncol 101:104530. https://doi.org/10.1016/j.oraloncology.2019.104530
Jung AR, Roh JL, Kim JS et al (2021) The impact of skeletal muscle depletion on older adult patients with head and neck cancer undergoing primary surgery. J Geriatr Oncol 12:128–133. https://doi.org/10.1016/j.jgo.2020.06.009
Jones AJ, Campiti VJ, Alwani M et al (2021) Sarcopenia is associated with blood transfusions in head and neck cancer free flap surgery. Laryngoscope Investig Otolaryngol 6:200–210. https://doi.org/10.1002/lio2.530
Makiguchi T, Yamaguchi T, Nakamura H et al (2019) Impact of skeletal muscle mass volume on surgical site infection in free flap reconstruction for oral cancer. Microsurgery 39:598–604. https://doi.org/10.1002/micr.30494
Chaukar DA, Walvekar RR, Das AK et al (2009) Quality of life in head and neck cancer survivors: a cross-sectional survey. Am J Otolaryngol 30:176–180. https://doi.org/10.1016/j.amjoto.2008.05.001
Pfister DG, Spencer S, Adelstein D et al (2020) Head and neck cancers, version 2.2020, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 18:873–898. https://doi.org/10.6004/jnccn.2020.0031
Bozzetti F, Gurizzan C, Lal S et al (2022) A European survey on the practice of nutritional interventions in head–neck cancer patients undergoing curative treatment with radio(chemo)therapy. Eur Arch Otorhinolaryngol 279:1499–1508. https://doi.org/10.1007/s00405-021-06920-4
Parker NH, Gorzelitz J, Ngo-Huang A et al (2021) The role of home-based exercise in maintaining skeletal muscle during preoperative pancreatic cancer treatment. Integr Cancer Ther 20:1534735420986615. https://doi.org/10.1177/1534735420986615
Carli F, Gillis C, Scheede-Bergdahl C (2017) Promoting a culture of prehabilitation for the surgical cancer patient. Acta Oncol 56:128–133
Arends J, Baracos V, Bertz H et al (2017) ESPEN expert group recommendations for action against cancer-related malnutrition. Clin Nutr 36:1187–1196. https://doi.org/10.1016/j.clnu.2017.06.017
Freiberger E, Sieber C, Pfeifer K (2011) Physical activity, exercise, and sarcopenia—future challenges. Wien Med Wochenschr 161:416–425. https://doi.org/10.1007/s10354-011-0001-z
Morley JE, Argiles JM, Evans WJ et al (2010) Nutritional recommendations for the management of sarcopenia. J Am Med Dir Assoc 11:391–396. https://doi.org/10.1016/j.jamda.2010.04.014
Grote M, Maihöfer C, Weigl M et al (2018) Progressive resistance training in cachectic head and neck cancer patients undergoing radiotherapy: a randomized controlled pilot feasibility trial. Radiat Oncol 13:215. https://doi.org/10.1186/s13014-018-1157-0
Lønbro S, Dalgas U, Primdahl H et al (2013) Lean body mass and muscle function in head and neck cancer patients and healthy individuals—results from the DAHANCA 25 study. Acta Oncol 52:1543–1551. https://doi.org/10.3109/0284186X.2013.822553
Kotz T, Federman AD, Kao J et al (2012) Prophylactic swallowing exercises in patients with head and neck cancer undergoing chemoradiation: a randomized trial. Archiv Otolaryngol Head Neck Surg 138:376–382
Capozzi LC, McNeely ML, Lau HY et al (2016) Patient-reported outcomes, body composition, and nutrition status in patients with head and neck cancer: results from an exploratory randomized controlled exercise trial. Cancer 122:1185–1200. https://doi.org/10.1002/cncr.29863
Karsten RT, Chargi N, van der Molen L et al (2022) Dysphagia, trismus and speech impairment following radiation-based treatment for advanced stage oropharyngeal carcinoma: a one-year prospective evaluation. Eur Arch Otorhinolaryngol 279:1003–1027. https://doi.org/10.1007/s00405-021-06870-x
Royston P, Altman DG, Sauerbrei W (2006) Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med 25:127–141. https://doi.org/10.1002/sim.2331
Prado CM, Purcell SA, Laviano A (2020) Nutrition interventions to treat low muscle mass in cancer. J Cachexia Sarcopenia Muscle 11:366–380. https://doi.org/10.1002/jcsm.12525
van der Werf A, Langius JAE, de van der Schueren MAE et al (2018) Percentiles for skeletal muscle index, area and radiation attenuation based on computed tomography imaging in a healthy Caucasian population. Eur J Clin Nutr 72: 288–296. https://doi.org/10.1038/s41430-017-0034-5
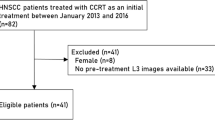
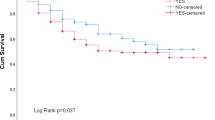
Erul E, Guven DC, Ozbay Y, Altunbulak AY, Kahvecioglu A, Ercan F, Yesil MF, Ucdal MT, Cengiz M, Yazici G, Kuscu O, Suslu N, Gullu I, Onur MR, Aksoy S (2023) Evaluation of sarcopenia as a prognostic biomarker in locally advanced head and neck squamous cell carcinoma. Biomark Med 17(2):87–99. https://doi.org/10.2217/bmm-2022-0748
Yunaiyama D, Okubo M, Arizono E et al (2021) Sarcopenia at the infrahyoid level as a prognostic factor in patients with advanced-stage non-virus-related head and neck carcinoma. Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-021-07147-z
Lee B, Bae YJ, Jeong WJ et al (2021) Temporalis muscle thickness as an indicator of sarcopenia predicts progression-free survival in head and neck squamous cell carcinoma. Sci Rep 11(19717):20211005. https://doi.org/10.1038/s41598-021-99201-3
Chang SW, Tsai YH, Hsu CM et al (2021) Masticatory muscle index for indicating skeletal muscle mass in patients with head and neck cancer. PLoS ONE 16:e0251455. https://doi.org/10.1371/journal.pone.0251455
Stone L, Olson B, Mowery A et al (2019) Association between sarcopenia and mortality in patients undergoing surgical excision of head and neck cancer. JAMA Otolaryngol Head Neck Surg 145:647–654. https://doi.org/10.1001/jamaoto.2019.1185
Baracos VE (2017) Psoas as a sentinel muscle for sarcopenia: a flawed premise. J Cachexia Sarcopenia Muscle 8:527–528. https://doi.org/10.1002/jcsm.12221
Koitka S, Kroll L, Malamutmann E et al (2021) Fully automated body composition analysis in routine CT imaging using 3D semantic segmentation convolutional neural networks. Eur Radiol 31:1795–1804. https://doi.org/10.1007/s00330-020-07147-3
Blanc-Durand P, Campedel L, Mule S et al (2020) Prognostic value of anthropometric measures extracted from whole-body CT using deep learning in patients with non-small-cell lung cancer. Eur Radiol 30:3528–3537. https://doi.org/10.1007/s00330-019-06630-w
Weston AD, Korfiatis P, Kline TL et al (2019) Automated abdominal segmentation of CT scans for body composition analysis using deep learning. Radiology 290:669–679. https://doi.org/10.1148/radiol.2018181432
Dabiri S, Popuri K, Ma C et al (2020) Deep learning method for localization and segmentation of abdominal CT. Comput Med Imaging Graph 85(101776):20200814. https://doi.org/10.1016/j.compmedimag.2020.101776
Acknowledgements
The authors would like to thank Nurbanu Kocdemir Erul, an otolaryngologist at Ankara city hospital, for her support with drawings.
Author contributions
Conceptualization, E.E., S.A., and D.C.G.; methodology, E.E. and D.C.G, M.R.O; supervision, S.A.,D.C.G., I.G., M.R.O writing—original draft, E.E., D.C.G and S.A.; writing—review & editing, E.E.,D.C.G., S.A., G.Y., and M.R.O The published version of the work has been reviewed and approved by all authors.
Funding
The authors received no financial support for this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Erul, E., Guven, D.C., Onur, M.R. et al. Role of sarcopenia on survival and treatment-related toxicity in head and neck cancer: a narrative review of current evidence and future perspectives. Eur Arch Otorhinolaryngol 280, 3541–3556 (2023). https://doi.org/10.1007/s00405-023-08014-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08014-9