Abstract
Purpose
While metastases directed therapy for oligometastatic disease is recommended in different cancer entities, the treatment of solitary metastases in head and neck squamous cell carcinoma (HNSCC) patients is not clearly defined.
Methods
A retrospective analysis was performed on data from 143 HNSCC patients treated between 2001 and 2016 in a tertiary university hospital. Clinical factors and outcome were measured using the median survival of patients receiving metastases specific therapy in comparison with matched control patients.
Results
In 37 patients, distant metastases were treated specifically with either surgery and/or stereotactic ablative radiotherapy and had with 23.97 months a more than three times higher median survival than 10 untreated matched controls with potentially treatable distant metastases (7.07 months).
Conclusions
Our retrospective analysis demonstrates a significant survival benefit for HNSCC patients who received a specific therapy regarding distant metastasis irrespective of localization as compared to a matched control cohort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck squamous cell carcinoma (HNSCC) is the sixth most common cancer in the world [1]. Despite ongoing advances in surgery, radio- and chemotherapy, 5-year survival rates still remain under 50% [2]. One of the limiting factors is remote mestastasis. The incidence of distant metastases at the initial clinical presentation is, at 10%, lower than in other cancer entities [3]. However, 20–30% of the patients with advanced condition develop distant metastasis during the course of their disease [4].
Currently, the presence of single or multiple metastasis is given the status ‘M1’. According to NCCN guidelines, the treatment of distant metastases is dependent on a performance score, and can determine if a systemic therapy or best supportive care is in the patients’ best interest [5]. In selected patients, surgical or radiation therapy of distant metastases can be considered [5]. It remains, however, unclear how to identify the patients benefiting from specific therapy like surgery or radiation of distant metastases.
The spectrum theory, which was introduced for breast cancer in 1994, stated that the disease stage at the first clinical presentation could fall into a spectrum ranging from indolent disease, to widely spread metastatic disease [6]. One year later, the term oligometastases was coined for the presence of one to few metastases [7]. Data show that oligometastatic cancers may represent a distinct clinical entity [8] and that patients may benefit from a metastatic specific therapy. Therapeutic options include surgery, stereotactic radiation, or cryotherapy [6]. In colon carcinoma, for example, meta analyses of retrospective studies show that patients with liver oligometastases benefit from metastasectomy with a 5 year survival rate of about 30% [9]. Despite the lack of sufficient prospective, randomized trials of treated and untreated patients in colon carcinoma, metastasectomy of one to few metastases of the liver is recommended in guidelines [10]. The evidence for metastasectomy of lung metastases in colon carcinoma, however, is still controversial, and prospective studies are needed [11]. A systematic review reported level 2a evidence of the effectiveness of pulmonary metastasectomy for metachronous metastases in HNSCC [12]. Reports on liver metastasectomy for HNSCC are scarce [13]. The aim of this study was, therefore, to retrospectively assess if HNSCC patients may benefit from metastases specific therapy. In addition, radiotherapy was compared to surgical metastasectomy, which in some cases was performed in combination with radiotherapy.
Materials and methods
Patients’ data
A total of 195 patients were diagnosed with distant metastatic HNSCC disease between January 2001 and January 2016 at the Department of Otolaryngology, Head and Neck Surgery, Technical University of Munich. Clinical data were retrieved from electronic medical records and filed medical records. These patients were routinely followed up on in the tumor consultation hour of the department of otolaryngology. Patients who fulfilled the following criteria were included: (1) pathologically confirmed squamous cell carcinoma and (2) metastatic disease at clinical presentation or development of metastasis in the observation period. Of the 195 patients, 52 had to be excluded because of missing clinical data or because radiologically suspected metastases at clinical presentation showed no progression in the observation period. Data from the remaining 143 patients were analyzed. The primary tumor was treated with surgery, chemotherapy, radiotherapy, or a combination of these according to German guidelines for head and neck cancer. 21 of the 143 Patients had their metastases surgically removed and histology confirmed the diagnosis of a metastasis as opposed to a secondary tumor. The remaining 122 patients were diagnosed as metastatic disease using CT imaging alone. Patients’ characteristics are listed in Table 1. Patients who were treated for distant metastases were compared to a matched control group of ten patients with a Karnofsky performance status scale higher than 60% with potentially treatable metastases by radiotherapy on retrospective analysis by two radiation therapists.
Data analysis
Overall survival (OS) was defined as the duration from the date of diagnosis of the primary tumor to either the date of death from any cause or censoring at last follow-up (August, 15th, 2016). The median survival (MS) of the cohort was defined as the time that 50% of the patients survived as of the date of metastasis. Patients who were treated for metastatic disease were compared in median survival to a matched control group as described in the last section.
Statistical analysis
All computations were performed with SPSS 23 (IBM, Armonk, USA). MS was analyzed using the Kaplan–Meier method, and statistical significance was assessed with the log-rank-test. Univariate and multivariate analyses were performed using the Cox proportional hazards model. Covariates included patient factors (Karnofsky performance score, sex, and age), tumor features (T classification, N classification, and M classification) and therapy of single and oligometastases. A 2-tailed p value < 0.05 was considered as statistically significant.
Results
Hepatic and osseous metastases are negative prognostic markers
In the analysis of 143 patients, we found a 2-year OS of 21.7% and 5-year OS of 3.5%. MS was 7.56 months with respect to diagnosis of the metastases. 32.6% of the patients had metastases at the time of initial tumor diagnosis, and 67.4% developed metastases in the observational period (Table 1). A total of 30 patients had a Karnofsky performance index lower than 70 with a significant lower median survival (Fig. 1a). The univariate analysis showed a hazard ratio of 0.5 for patients with a Karnofsky Index higher than 70. Patients with synchronous M1 situation had a significantly higher median survival (Fig. 1b). Initial tumor in oral cavity, liver, bone, and mediastinal metastases were significantly negative prognostic factors (Fig. 1c–f). Primary metastases in these locations were associated with a significant higher risk of death as illustrated by the increased hazard ratio. Alcohol consumption was associated with higher median overall survival (p = 0.01). Local tumor manifestation at diagnosis of M1 situation was not associated with significant higher survival (p = 0.34).
Selected Kaplan–Meier curves of survival of significant patient characteristics are shown. Karnofsky performance index lower than 70, metachronous M1 situation, primary in oral cavity, no history of alcohol consumption, occurrence of mediastinal, liver, and bone metastases were negative prognostic factors within our data
Significant longer survival in patients with specific therapy of metastases
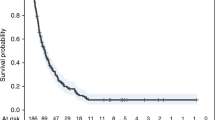
Patient survival was analyzed with attention given on distant metastases and the treatment thereof. The median survival of patients with single organ metastases (67.8%) was significantly higher compared with patients with metastases in several organs (p < 0.01; Table 2; Fig. 2a). The hazard ratio for patients with a single organ metastasis was significantly lower (0.38). Patients who had a singular metastasis (38/143) had a significantly prolonged median survival (p < 0.01; Fig. 2b), as did patients with oligometastases (p < 0.01, Fig. 2c). Furthermore, 37 patients received local therapy of their distant metastases (either surgery, radio therapy, or combination) and had a significant longer median survival with 23.97 months versus 7.07 months in patients with untreated but potentially treatable distant metastases (Fig. 2d). Hazard ratio for these patients in the univariate analysis was 0.25, and thus significantly lowered. In the group of the 37 patients who received local metastatic therapy and the 10 patients with potentially treatable metastatic sites, 16 patients had their primary locally controlled (Table 4) while 31 patients had no controlled local tumor. Median survival was 19.07 and 13.41 months, the difference was not statistically significant (p = 0.77).
By investigation of the patient’s survival as a function of the metastasis and its treatment, we found, that metastases in only one organ, singular metastasis, oligo-metastases and the specific therapy of the metastases are positive predictors. There was no significant difference between specific treatment of distant metastasis with surgery or radiotherapy
To confirm the results, a Cox regression model was performed. In this multivariate analysis, patients with a metastasis who received metastases specific treatment had, with 0.06, a significantly lower hazard ratio than untreated patients. Patients with a primary in the oral cavity had a significantly higher hazard ratio (p = 0.03). Performance status, age, alcohol consumption, presence of liver, bone or mediastinal metastasis and M1 at diagnosis of primary were not statistically significant in this model (Table 3).
Radiotherapy and surgery as an equivalent treatment option
Next, we examined the different specific therapies of distant metastases. Clinical characteristics of patients are depicted in Table 4. We found that of the 37 patients receiving local therapy, 21 had surgery in part combined with radiotherapy, while 16 underwent radiotherapy. Patients receiving radiotherapy had a higher median survival (25.71 versus 20.29 months, Fig. 2e) which was not statistically significant (p = 0.73). One patient receiving pulmonary metastatic resection died postoperatively.
Discussion
Currently, HNSCC patients with a single metastasis, oligometastases or a multi-organ spread disease are categorized as M1 and usually treated with palliative chemotherapy or best supportive care. Some patients also receive specific therapy such as surgery or radiotherapy of distant metastases. Unfortunately, clear guidelines are lacking on which distant metastases should be treated with radiotherapy, surgery, or systemic chemotherapy. The current NCCN guideline only states that specific therapy of metastases is an option in patients with an M1 situation at initial presentation with limited metastases and a performance scale of 0–1 [5]. Furthermore, it is stated that in patients with recurrent or persistent disease with distant metastases, palliative radiotherapy can be considered [5]. In this study, we, therefore, retrospectively analyzed 143 HNSCC patients with M1 situations for prognostic factors and assessed which patients benefit from a specific surgical or radiation therapy of distant metastases.
One limitation of our study is that the diagnosis of distant metastasis was only histologically proven in the patients that had their metastases surgically removed (21 of 143 patients). The remaining patients had their metastatic disease diagnosed by imaging. Metastatic disease was seen on imaging and discussed in our interdisciplinary tumor board. For lung tumors, a secondary tumor instead of metastatic disease can, therefore, not be ruled out in certain cases. Further limitation is given by the number of patients included in this study and the retrospective nature of the analysis.
Poor clinical performance, for example, measured by the Karnofsky score, has been reported as a negative prognostic factor in most tumor entities including head and neck cancer [14]. In addition, in our cohort, patients with a Karnofsky performance status scale over 60 had a three times higher median survival. Baatenenburg de Jong et al. report T and N status as a significant prognostic factor in overall survival in their study of 1396 head and neck cancer patients [15]. Although there was a trend in our analysis (Table 1), higher T and N classification were not significant for median survival in our study. This is most likely due to the relatively small number of patients included. The presence of liver metastases has been discussed to be associated with worse prognosis in different tumor entities such as nasopharyngeal cancer [16, 17]. In our analysis, patients with liver metastases also had a significant lower median survival. Bone metastases have been demonstrated to be a negative prognostic factor in tumors of different origins [18]. In accordance, we show, that patients with bone metastases had a 6 months’ shorter median overall survival when compared to the rest of the cohort. Furthermore, patients with mediastinal lymph nodes had also a significant shorter median survival.
In addition, in our cohort, patients with metastases in multiple organs had a significant worse outcome. Median survival in patients with only one metastatic site was with 11.31 months more than three times longer than in patients, where metastases had spread to multiple organs (3.45 months). In the univariate analysis, hazard ratio for patients with singular metastatic organ was 0.38, and thus, risk to die was 62% lower in the observation period compared to patients with metastases in multiple organs. Similar results can be found in the literature. For example, Han and colleagues report the number of metastatic sites as a prognostic factor in renal cell carcinoma. Patients with multiple organ metastases had a median survival of 11 months, while patients with only bone or lung metastases had both a median survival of 31 months [19].
Our data show a benefit of specifically treating patients with metastasis. Patients with metastases when either treated by radiation therapy and/or surgical resection had a significant more than three times higher median survival (23.97 months) than patients with potentially specifically treatable distant metastases that did not receive local therapy of their metastases (7.07 months). This is in accordance with findings in the literature. Nakajima et al. demonstrate a disease free survival of 24 months in a cohort of 58 patients with head and neck cancer who had their lung metastases surgically removed [20]. Yotsukura show a median 37 months disease free survival after lung metastasectomy in a total of 34 patients including 19 patients with squamous cell carcinoma, 10 patients with adenoid cystic carcinoma and five with other diseases [21]. According to the hazard ratio, risk of death in the observation period was significantly reduced by 75% in the patients group with specifically treated metastases. In the control group (ten patients) only patients with a Karnofsky index higher than 60 were included. Specifically treated patients had a higher rate of local tumor control and metachronous distant metastases which could also explain part of the higher median survival in this group. However, a better control group could only be created in a prospective randomized trial which is ethically not feasible. In the multivariate cox regression, the specific therapy of distant metastases and primary in oral cavity were only significant factors. Specific therapy of the metastases was associated with a 94% reduced risk (hazard ratio 0.06). Primary in oral cavity was associated with a high hazard ratio (25.7). This should be interpreted with caution and could be overstated because of the limited sample size. Karnofsky scale was not significant in this model. This could be due to the small subgroup of only 47 patients.
We did not measure a statistically significant difference in median survival between surgery or with radiation therapy treated patients. Among the limited data in the literature Hiroshi and colleagues show that SBRT is comparable to surgery in stage I non-small cell lung carcinoma [22]. Unfortunately, in our cohort one of 21 surgically treated patients died after resection of lung metastases. In view of the periprocedural morbidity and mortality, radiotherapy might be more appropriate in the palliative setting.
Despite lack of sufficient prospective studies, metastasectomy or stereotactic ablative radiotherapy of one to a few liver metastases is recommended in selected patients with a good liver function according to international guidelines for colon carcinoma [10, 23]. These recommendations are based on the analysis of the outcome of metastasectomized patients exceeding those outcomes normally associated with metastatic colorectal cancer [24]. While randomized prospective studies are probably ethically infeasible [25], there are also only a few studies retrospectively comparing outcomes of locally treated and untreated metastases in other cancer entities. For example, Toshiki et al. retrospectively compared 22 patients receiving resection of liver metastases together with surgery of their primary gastric cancer versus 25 patients only receiving surgery of their primary and found a significant longer survival of the first group [26].
Conclusion
In conclusion, while treatment of one or a few distant metastases is recommended in other cancer entities like colon carcinoma in selected patients, treatment of metastases in HNSCC is not clearly defined. Although validity is limited by retrospective analysis, our study demonstrates a significant survival benefit for HNSCC patients who received specific treatment of their metastasis regardless of the origin. These data should be confirmed in a large multicenter prospective analysis to increase the data quality. However, based on the results randomization seems ethically infeasible.
References
Parkin DM et al (2005) Global cancer statistics, 2002. CA Cancer J Clin 55(2):74–108
Bernier J et al (2004) Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med 350(19):1945–1952
Argiris A et al (2008) Head and neck cancer. Lancet 371(9625):1695–1709
Vermorken JB, Specenier P (2010) Optimal treatment for recurrent/metastatic head and neck cancer. Ann Oncol 21(Suppl 7):vii252-61
National Comprehensive Cancer Network (2016) NCCN clinical practice guidelines in oncology head and neck cancers (Version 1.2016). https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed 23 Sept 2016
Reyes DK, Pienta KJ (2015) The biology and treatment of oligometastatic cancer. Oncotarget 6(11):8491–8524
Hellman S, Weichselbaum RR (1995) Oligometastases. J Clin Oncol 13(1):8–10
Weichselbaum RR, Hellman S (2011) Oligometastases revisited. Nat Rev Clin Oncol 8(6):378–382
Simmonds P et al (2006) Surgical resection of hepatic metastases from colorectal cancer: a systematic review of published studies. Br J Cancer 94(7):982–999
Mahmoud N, Bullard K, Dunn (2010) Metastasectomy for stage IV colorectal cancer. Dis Colon Rectum 53(7):1080–1092
Fiorentino F et al (2010) Pulmonary metastasectomy in colorectal cancer: a systematic review and quantitative synthesis. J R Soc Med 103(2):60–66
Young ER et al (2015) Resection of subsequent pulmonary metastases from treated head and neck squamous cell carcinoma: systematic review and meta-analysis. Clin Otolaryngol 40(3):208–218
Florescu C, Thariat J (2014) Local ablative treatments of oligometastases from head and neck carcinomas. Crit Rev Oncol Hematol 91(1):47–63
Mehanna H et al (2010) Head and neck cancer—Part 2: treatment and prognostic factors. BMJ 341(c4690):721–725
Baatenburg de Jong RJ et al (2001) Prediction of survival in patients with head and neck cancer. Head Neck 23(9):718–724
Khanfir A et al (2007) Prognostic factors in metastatic nasopharyngeal carcinoma. Cancer/Radiothérapie 11(8):461–464
Tian YH et al (2016) Oligometastases in AJCC stage IVc nasopharyngeal carcinoma: a subset with better overall survival. Head Neck 38(8):1152–1157
Yucel B et al (2015) The negative prognostic impact of bone metastasis with a tumor mass. Clinics (Sao Paulo) 70(8):535–540
Han K-R et al (2003) Number of metastatic sites rather than location dictates overall survival of patients with node-negative metastatic renal cell carcinoma. Urology 61(2):314–319
Nakajima Y et al (2017) Surgical treatment for pulmonary metastasis of head and neck cancer: study of 58 cases. Ann Thorac Cardiovasc Surg 23(4):169–174
Yotsukura M et al (2015) Survival predictors after resection of lung metastases of head or neck cancers. Thorac Cancer 6(5):579–583
Onishi H et al (2011) Stereotactic body radiotherapy (SBRT) for operable stage I non-small-cell lung cancer: can SBRT be comparable to surgery? Int J Radiat Oncol Biol Phys 81(5):1352–1358
Comito T et al (2015) Liver metastases and SBRT: a new paradigm? Rep Pract Oncol Radiother 20(6):464–471
Pfannschmidt J, Dienemann H, Hoffmann H (2007) Surgical resection of pulmonary metastases from colorectal cancer: a systematic review of published series. Ann Thorac Surg 84(1):324–338
Khatri VP, Petrelli NJ, Belghiti J (2005) Extending the frontiers of surgical therapy for hepatic colorectal metastases: is there a limit? J Clin Oncol 23(33):8490–8499
Shinohara T et al (2015) Survival benefit of surgical treatment for liver metastases from gastric cancer. J Gastrointest Surg 19(6):1043–1051
Acknowledgements
The authors gratefully acknowledge Armin Ott from the Institute for Medical Statistics and Epidemiology at Technical University of Munich for his advice on the statistical analysis.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest.
Ethics approval
Only routine clinical data were retrospectively collected from patients’ charts and pseudonymously analyzed, and therefore, no formal ethical approval was obtained. We declare that all authors have contributed to read and approved the final manuscript for submission.
Additional information
Dominik Schulz and Markus Wirth contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Schulz, D., Wirth, M., Piontek, G. et al. Improved overall survival in head and neck cancer patients after specific therapy of distant metastases. Eur Arch Otorhinolaryngol 275, 1239–1247 (2018). https://doi.org/10.1007/s00405-018-4920-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-4920-9