Abstract
Early-stage head and neck carcinomas can usually be controlled with the appropriate treatment. In these patients, the long-term prognosis mainly depends on second metachronous malignancies, frequently in the aerodigestive tract. Our study aims to identify risk factors for the appearance of second tumours in this group of patients with early head and neck cancer. Of 949 patients included in the study, 189 (20%) developed a metachronous second primary malignancy, most frequently in the aerodigestive tract. Independent risk factors associated with second tumours were heavy alcohol use and the location of the index tumour in the oropharynx. Compared to non-drinkers, heavy drinkers (>80 g/day) presented a 1.8-times higher risk of a second tumour (CI 95%: 1.01–3.50). Patients with oropharyngeal tumours had a 2.15-higher risk than patients with oral cavity tumours (CI 95%: 1.03–4.47). Recursive partitioning analysis was used to characterise two risk groups for second tumours. The low-risk group included patients over 75 years and patients with low levels of carcinogen use. It comprised 171 patients (18%) with a 5.3% frequency of second tumours. The high-risk group accounted for 80% of the patients ( n =778), and the rate of second neoplasms was 16.3%. Classification of the patients according to the mentioned variables allows us to focus follow-up and prevention efforts on high-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In most patients with early-stage (stages I and II) squamous cell carcinomas of the head and neck (SCCHN), tumour control is achieved with the appropriate treatment. Long-term survival depends mainly on the appearance of metachronous second primary tumours (MSPT) in the aerodigestive tract, that is, second primary malignancies discovered more than 6 months after the index tumour has been detected.
Several studies have been published on this subject. Some evaluate second tumours and the overall prognosis in early stage laryngeal carcinomas treated with surgery [7] or radiotherapy [3, 4], while others study index tumours in other locations—mainly oral cavity tumours—treated with radiotherapy [15].
The aim of this study was firstly to analyse the incidence, distribution and prognosis of MSPT in patients with an early stage (I and II) head and neck index tumour and secondly to define the risk factors for the development of second tumours in this group of patients.
Materials and methods
Data used in this study were obtained retrospectively from a database that prospectively collects information on the patient’s clinical status, including carcinogen use, tumour characteristics, treatment and follow-up of all the patients with a malignant head-and-neck tumour diagnosed in our hospital since 1985.
A total of 1,049 patients with stage I-II squamous cell carcinomas of the oral cavity, oropharynx, hypopharynx and larynx were diagnosed in our department in the period between 1985–2000. Forty-four patients presenting with synchronic tumours and 56 patients lost to follow-up in the first 3 years were excluded. This study was thus made up of 949 patients with stage I-II carcinomas and a minimum follow-up of 3 years.
The routine follow-up programme in our hospital consists of recent medical history and locoregional examinations at bimonthly intervals during the 1st year, every 3 months in the 2nd year, every 4 months between the 3rd and 5th years, and every 6 months thereafter. All patients undergo annual chest radiography. The control visits are carried out alternately by the departments involved in the treatment of the patients: otorhinolaryngology, radiotherapy and medical oncology. Warren and Gates criteria for defining a second tumour were followed [14].
We evaluated the incidence of MSPT, as well as the location and histology of the second neoplasm, the relation between the appearance of a MSPT and several epidemiological variables and patient survival in relation to the appearance of a second neoplasm.
The chi-square method and the Fisher exact test were used to compare frequencies, and the actuarial Kaplan-Meier method to calculate the risk of appearance of a second neoplasm and survival rates. A Cox proportional hazard regression model studied the relation between epidemiological factors and the risk of appearance of a second neoplasm. A recursive partitioning analysis was employed to define MSPT risk groups.
Results
During the follow-up period, a MSPT was diagnosed in 189 patients (20%). Table 1 shows the distribution of the second tumours in relation to the location of the index tumour. About 72% of MSPT were carcinomas of the aerodigestive tract (35% pulmonary, 6% oesophageal and in 31% a secondary head and neck carcinoma).
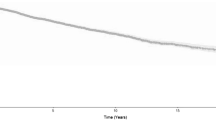
Figure 1 shows the MSPT-free actuarial survival curve for total second malignancies and also that for second tumours of the aerodigestive tract alone. Following diagnosis of the index tumour, early stage SCCHN had a 3% actuarial risk per annum of MSPT in any location, and a 2.4% per annum in the aerodigestive tract. Interestingly, the shape of the survival curves shows that this risk was continuous throughout the follow-up period.
Table 2 shows the distribution of MSPT in the aerodigestive tract in the function of variables such as age at diagnosis of the index tumour, sex, primary tumour location, stage, alcohol or tobacco use when the index tumour was diagnosed and the modality of treatment. Statistically significant differences were found in the univariate analysis regarding age at the diagnosis of primary malignancy (older patients presented a lower frequency of second tumours), tumour location (oro-hypopharynx primary tumours showed a higher incidence of MSPT) and alcohol and tobacco use (the higher the level of use, the higher the frequency of MSPT).
The Cox proportional hazard regression model was used to study the possibility of an interaction among the variables of the study (Table 3). Alcohol use and location of the index tumour in the oropharynx were independent variables regarding MSPT in the aerodigestive tract. Compared to patients with no history of alcohol use, those who consumed over 80 g per day showed a 1.8-times higher risk of MSPT (CI 95%: 1.01–3.50). Using index carcinomas in the oral cavity as a reference category, patients with index carcinomas in the oropharynx had a 2.15-higher risk of the appearance of a second neoplasm (CI 95%: 1.03–4.47).
Of the 949 patients included in the study, 92 (9.7%) died because of failure in controlling the index tumour and 66 (7.0%) because of the development of a MSPT in the aerodigestive tract. For stage I tumours, mortality due to the primary index tumour (6.4%) was similar to that of MSPT in the aerodigestive tract (6.6%). For stage II tumours, mortality due to index tumours (14.1%) was twice as high as that of MSPT in the aerodigestive tract (7.4%).
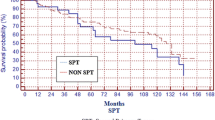
Figure 2 shows the adjusted actuarial survival after MSPT diagnosis. Survival outcome was best in second tumours of the head and neck, with a 5-year survival of 61%. Second tumours of the lung or oesophagus showed a considerably worse prognosis, with a 5-year survival of 19 and 0%, respectively. Secondary malignancies in locations other than the aerodigestive tract presented a 5-year actuarial survival of 53%.
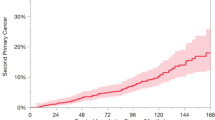
A repercussive partitioning analysis technique helped to define two groups of patients according to the risk of a second neoplasm in the aerodigestive tract (Fig. 3). Variables included in the model were the index tumour localization, age at diagnosis of the index tumour, previous use of alcohol and tobacco and treatment modality. In our population the model defined two risk groups. The low-risk group, which included elderly patients and patients with a lower level of tobacco and alcohol use, comprised 171 patients (18%) who presented a 5.3% frequency of second tumour in the aerodigestive tract during the follow-up period. The remaining patients ( n =778) were classified in the high-risk group and showed a MSPT rate of 16.3%. The hazard ratio curve for the development of a SMPT in the aerodigestive tract depending on the risk group is shown in Fig. 4.
Classification tree obtained with a recursive partitioning analysis technique obtained from the variables with the highest discrimination analysis: Group 1: patients with low-risk of metachronous aerodigestive tract second tumour; group 2: patients with high-risk of metachronous aerodigestive tract second tumour. Number of patients included in each terminal branch/percentatge of patients with a second tumour. Alcohol: alcohol use previous to index tumour diagnosis; tobacco: tobacco use previous to index tumour diagnosis; RT radiotherapy
Discussion
Patients with a SCCHN have an increased risk of second malignancy, usually a squamous cell carcinoma of the aerodigestive tract. Longitudinal studies show that the risk of second tumours remains constant throughout the follow-up period [5, 8]. Second tumours in the aerodigestive tract are related to the “condemned-mucosa syndrome” [10]. According to this theory, the carcinogenic effects of tobacco and alcohol leading to index head and neck cancer also act on the entire mucosa of the aerodigestive tract, originating the appearance of further carcinomas.
The impact of second tumours on long-term results is particularly important in early stages of SCCHN. When index tumour healing probability is high, development of a second tumour will affect final survival more than the index tumour itself [3, 4, 11].
The role of the extension of the index tumour in the appearance of second neoplasms is still subject to debate. In a multivariate analysis, Jones et al. [5] found an increased incidence of second tumours in patients with index tumours in early stages, while other authors could not demonstrate this relationship [8, 12].
Some publications have specifically analysed the problem of second neoplasms in SCCHN in the early stages. Fujita et al. [3] studied second neoplasias in 158 patients with T1 glottis cancer treated with radiotherapy. About 22% of the patients developed a second tumour, located in the aerodigestive tract in 67%. Compared with the normal population the risk of developing a second malignant tumour in the aerodigestive tract was 8.5 (CI 95%: 5.2–11.8). Overall, 8.2% patients died from laryngeal cancer, while 15% died from the second neoplasia.
Similarly, 28% of the 240 patients with T1-T2 laryngeal cancers treated with radiotherapy by Holland et al. [4] developed a second malignancy, located in the aerodigestive tract in 71% of the cases. As many as 85% of second malignancies appeared metachronously, maintaining a constant incidence throughout the follow-up period.
Yamamoto et al. [15] analysed the relationship between the location of the index tumour and the development of second neoplasias in patients with early stage SCCHN treated with radiotherapy. In their series, 33% of 1,609 SCCHN patients developed a second tumour, the aerodigestive tract being the most frequent location (71%). Second tumours in the aerodigestive tract were more frequent when index tumours were located in the oropharynx (34%), hypopharynx (21%) or floor of the mouth (21%) rather than the tongue (12%) or larynx (7%).
Similar findings have been published for patients treated surgically. Lacourreye et al. [7] found MSPT in 24% of patients with glottic tumours treated with partial surgery. Once again, most (67%) were located in the upper aerodigestive tract. The 2% annual incidence of second neoplasms remained unchanged throughout the follow-up period.
Khuri et al. [6] communicated their preliminary results of a clinical assay to evaluate the efficacy of 13-cis-retinoid acid in the prevention of second malignancies in early stage SCCHN treated with surgery or radiotherapy. The 1,127 patients included in the study presented an annual 5.1% incidence of second tumours constantly throughout the follow-up period. They found 66% of second neoplasms in the aerodigestive tract. Statistically significant differences in the incidence of MSPT were found in relation to the location and staging of the primary tumour. The annual incidence for pharyngeal tumours was 5.1% and that for laryngeal tumours 2.7% ( P =0.001). Tobacco-related malignancies showed a higher incidence in stage II tumours (4.8%) than in stage I tumours (2.7%) ( P =0.001%).
Among risk factors related to the development of second neoplasias, both past tobacco use [7, 8] and the persistence in tobacco or alcohol use after diagnosis of the index [2] tumour prevail. According to our data, variables related to the development of MSPT in the aerodigestive tract were age at the time of diagnosis of the index tumour, index tumour location and use of alcohol and tobacco prior to the finding of the index tumour. Second tumours were more frequent after pharyngeal carcinomas in younger patients with high levels of carcinogen use. In a multivariate analysis, only two variables maintained their prognostic capacity regarding the appearance of second tumours. These were location of the index tumour in the oropharynx and past severe (>80 g/day) alcohol use.
Consistently with our results, all authors found that prognosis of patients with a second tumour in the aerodigestive tract depended mainly on its location [3, 4, 7]. Thus, survival of patients with pulmonary or oesophageal second neoplasms was considerably lower than that of patients with head and neck secondary tumours.
One of the main goals in the follow-up of head and neck tumours is the early detection of second neoplasias [13]. Obtaining a classification based on the risk to develop second tumours would be particularly useful, for it would allow optimisation of resources used in the follow-up of these patients. Recursive partitioning analysis is a mathematical technique that evaluates variable association depending on a final specific result. It is used to classify a population of patients into groups with similar results. A classification tree is obtained from the variables with the highest discrimination capacity. Terminal branches of the tree represent groups of patients with similar prognosis for the evaluated event, in this case, the development of MSPT in the aerodigestive tract.
According to our results, younger patients with greater past use of toxic substances showed a higher risk of MSPT in the aerodigestive tract, especially when the index tumour was located in the oropharynx or the hypopharynx.
As shown previously, the high-risk group for second malignancies comprises more than 80% of the patients with an index tumour in the head and neck. This represents one of the limitations of our study. We could not include in our study variables that have a significant role in the development of metachronous tumours such as toxic use after treatment [2] or individual predisposing factors [1, 9]. Including these variables in the analysis will probably help to narrow the spectrum of high-risk patients in future studies.
References
Bongers V, Snow GB, de Vries N, Cattan AR, Hall AG, van der Waal I, Braakhuis BJM (1995) Second primary head and neck squamous cell carcinoma predicted by the glutathione S-transferase expression in healthy tissue in the direct vicinity of the first tumor. Lab Invest 73:503–509
Do KA, Johnson MM, Doherty DA, Lee JJ, Wu XF, Dong Q, Hong WK, Khuri FR, Fu KK, Spitz MR (2003) Second primary tumors in patients with upper aerodigestive tract cancers: joint effects of smoking and alcohol (United States). Cancer Causes Control 14:131–138
Fujita M, Rudoltz MS, Canady DJ, Patel P, Machtay M, Pittard MQ, Mohiuddin M, Regine WF (1998) Second malignant neoplasia in patients with T1 glottic cancer treated with radiation. Laryngoscope 108:1853–1855
Holland JM, Arsanjani A, Liem BJ, Hoffelt SC, Cohen JI, Stevens KR (2002) Second malignancies in early stage laryngeal carcinoma patients treated with radiotherapy. J Laryngol Otol 116:190–193
Jones AS, Morar P, Phillips DE, Field JK, Husband D, Helliwell TR (1995) Second primary tumors in patients with head and neck squamous cell carcinoma. Cancer 75:1343–1353
Khuri FR, Kim ES, Lee JJ, Winn RJ, Benner SE, Lippman SM, Fu KK, Cooper JS, Vokes EE, Chamberlain RM, Williams B, Pajak TF, Goepfert H, Hong WK (2001) The impact of smoking status, disease stage, and index tumor site on second primary tumor incidence and tumor recurrence in the Head and Neck Retinoid Chemoprevention Trial. Cancer Epidemiol Biomarkers Prev 10:823–829
Laccourreye O, Hans S, Garcia D, Veivers D, Brasnu D, Laccourreye L (2002) Metachronous second primary cancers after successful partial laryngectomy for invasive squamous cell carcinoma of the true vocal cord. Ann Otol Rhinol Laryngol 111:204–209
León X, Quer M, Diez S, Orús C, López-Pousa A, Burgués J (1999) Second neoplasm in patients with head and neck cancer. Head Neck 21:204–10
Schantz SP, Spitz MR, Hsu TC (1990) Mutagen sensitivity in patients with head and neck cancers: a biologic marker for risk of multiple primary malignancies. J Nat Cancer Inst 82:1773–1775
Slaughter DP, Southwick HW, Smejkal W (1953) Field cancerization in oral stratified squamous epithelium. Cancer 6:963–968
Spector JG, Sessions DG, Chao KSC, Haughey BH, Hanson JM, Simpson JR, Perez CA (1999) Stage I (T1N0M0) squamous cell carcinoma of the laryngeal glottis: therapeutic results and voice preservation. Head Neck 21:707–717
Spector JG, Sessions DG, Haughey BH, Chao KSC, Simpson J, El Mofty S, Perez CA (2001) Delayed regional metastases, distant metastases, and second primary malignancies in squamous cell carcinomas of the larynx and hypopharynx. Laryngoscope 111:1079–87
de Visscher AVM, Manni JJ (1994) Routine long-term follow-up in patients treated with curative intent for squamous cell carcinoma o the larynx, pharynx, and oral cavity. Arch Otolaryngol Head Neck Surg 120:934–939
Warren S, Gates O (1932) Multiple malignant tumors: a survey of literature and statistical study. Am J Cancer 16:1358–414
Yamamoto E, Shibuya H, Yoshimura R, Miura M (2002) Site specific dependency of second primary cancer in early stage head and neck squamous cell carcinoma. Cancer 94:2007–2014
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
León, X., del Prado Venegas, M., Orús, C. et al. Metachronous second primary tumours in the aerodigestive tract in patients with early stage head and neck squamous cell carcinomas. Eur Arch Otorhinolaryngol 262, 905–909 (2005). https://doi.org/10.1007/s00405-005-0922-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-005-0922-5