Abstract
Purpose
To determine perioperative morbidity associated with the transvaginal mesh and analyse patient reported outcome measures following transvaginal mesh surgery via a prospective cohort study.
Methods
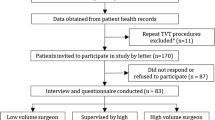
A retrospective review and a prospective cohort study of vaginal symptoms via a validated questionnaire (Ethically approved). 159 consecutive women who underwent transvaginal polypropylene mesh repair for pelvic organ prolapse from January 2009 to January 2012 by a single experienced urogynaecologist were identified using theatre records and formed the study population. The type and frequency of intraoperative and postoperative complications, mesh exposure rates and need for further surgery were recorded. 59/159 patients consented to complete both preoperative and postoperative assessment of vaginal symptoms using the validated International Consultation on Incontinence Modular Questionnaire-Vaginal symptoms (ICIQ-VS). 51/59 patients completed both questionnaires.
Results
The average age of the study population was 63 years (range 39–87 years). The mean BMI was 28.5 (range 20–40). 86 % (n = 138/159) had a previous hysterectomy. 98 % (n = 156/159) of patients did not have any intraoperative complications. 0.62 % (n = 1/159) had a bladder injury. Mesh exposure was noted in 4 % of the entire group (n = 6/135) at follow-up with overall reoperation rate of 9 % (n = 13/135). Statistically significant improvement in most arms of the ICIQ-VS questionnaire was noted in the cohort of 51 patients at follow-up.
Conclusion
Our data revealed a very low intraoperative complication rate with a mesh exposure rate of 4 %. The prospective study showed a statistically significant improvement in vaginal symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The transvaginal route for repair of severe or recurrent pelvic organ and vaginal vault prolapse using mesh has been plagued with controversy in the last few years leading to the removal of several mesh kits from the surgical scene.
Pelvic organ prolapse (POP) remains an important health issue for women with up to one in five women having one or more operations to correct prolapse over their lifetime [1]. 70 % of patients presenting with pelvic organ prolapse have two or all three vaginal compartments involved [1]. The transvaginal route is the primary surgical option for patients with pelvic organ prolapse including those with significantly raised body mass index (BMI), previous difficult abdominal surgery, stoma formation or failed surgery for prolapse carried out by the abdominal route.
The transvaginal approach has significant advantages over the abdominal approach including shorter operating time, earlier return to daily activities and decreased cost [2]. Abdominal surgery is not without significant complications including greater perioperative morbidity with a higher economic burden. Rare but devastating complications such as pyogenic spondylodiscitis and bowel obstruction have been reported following abdominal sacrocolpopexy [3].
Synthetic materials restore and strengthen pelvic floor anatomy, improve success rates and reduce recurrence, but they bring an increased risk of complications in comparison to traditional/native tissue repair [4]. Reported mesh exposure rates are still a significant problem with transvaginal mesh surgery with surgical excision required in approximately 10 % of cases [5]. A recent Cochrane review on surgical management of pelvic organ prolapse revealed a 11 % mesh erosion rate [2].
Several studies indicate that greater surgical experience is correlated with fewer mesh complications [6]. Inappropriate surgical indications, poor surgical techniques or the type of synthetic material can contribute to the complications [4].
We report a prospective study assessing vaginal symptoms following transvaginal polypropylene mesh repair and a retrospective study examining perioperative and postoperative complications. This report may help to give a more realistic view of the true value of transvaginal mesh without the confounding problem of inexperience or inadequate training.
Aims
To report experienced single surgeon data on intraoperative complications, short term postoperative complications, mesh exposure rates and necessity for additional surgery after transvaginal mesh repair of pelvic organ prolapse over a 3 year period and to report effectiveness of use of vaginal mesh for vaginal symptoms over a 4 year period using a prospective patient reported outcome measures study. Setting: Tertiary centre for urogynaecology.
Materials and methods
The retrospective project was supported by the Hospital Trust Research and Development team who confirmed it to be a service evaluation project. Hence, no ethical approval was needed for the retrospective project.
The prospective cohort study of vaginal symptoms was ethically approved (06/q1206/150). Voluntary patient consent was obtained in the gynaecology clinic preoperatively and postal questionnaires were sent to the patient postoperatively. No funding was required.
159 consecutive women who underwent transvaginal polypropylene mesh repair from January 2009 to January 2012 were identified using theatre database and formed the study population for the data on perioperative outcomes. All cases included in the study were carried out by a fully trained surgeon with a high volume of experience in mesh surgery.
Data regarding age, BMI, menopausal status, previous gynaecological surgery, duration of intravenous antibiotics, requirement for blood transfusion, postoperative pyrexia, postoperative urinary tract infection or wound infection, bladder care protocol, voiding dysfunction and need for intermittent self catheterisation (ISC) or Foleys indwelling catheterisation, buttock pain, pelvic pain, vaginal pain, mesh exposure at first follow-up visit and need for additional surgery to correct complications due to the mesh were obtained from patient records. All patients were given a follow-up appointment at 12 weeks after surgery and all underwent a vaginal examination to assess for mesh exposure.
Procedural details and intraoperative complications were noted from the operative notes recorded by the surgeon at the time of the procedure.
For purposes of this study, patients with symptoms of a urinary tract infection with a positive urine culture were diagnosed as having a postoperative urinary tract infection. Patients presenting to the general practitioner or hospital with symptoms of offensive vaginal discharge needing antibiotics with or without a positive culture on high vaginal swab were diagnosed as having a wound infection. A temperature of 38 °C and above constituted the definition of pyrexia in the postoperative period. Postoperative data were obtained from the nursing charts and follow-up records.
Mesh exposure was defined as mesh visible or palpable within the vagina at postoperative speculum examination. Site and size of mesh exposure was documented in the patient’s notes by the attending clinician.
The type and frequency of perioperative complications were documented using a standardised proforma. Our standard postoperative protocol included 48 h of intravenous Co-amoxiclav 1.2 g tds. Teicoplanin 400 mg 12 hourly and Metronidazole 500 mg 8 hourly was given IV in case of Penicillin allergy.
All patients had a postoperative vaginal pack and urethral catheter for 48 h. Patients were allowed home on Day 3 following a satisfactory bladder protocol (2 post void bladder residuals of <100 ml on bladder scan).
All complications were classified using the Joint International Urogynaecology Association and International Continence Society System [7].
Surgical technique involved correct identification of planes and meticulous tissue dissection. Local anaesthetic (0.25 % Chirocaine 20 ml with 1 in 200,000 Adrenaline diluted with 80–120 ml of normal saline) was used in all patients to allow precise and haemostatic separation of tissue planes and assist in postoperative pain relief.
For the anterior mesh, a full thickness midline incision was made on the anterior vaginal wall after local anaesthetic infiltration. Mobilisation of the vaginal epithelium from the underlying prevesical tissue was facilitated using hydrodissection. Careful blunt dissection was undertaken to access the ischial spines bilaterally to allow identification of the whole length of the arcus tendineus fascia and introduction of the anterior mesh. Care was taken to ensure that the mesh arm was not twisted during placement. Mesh overlay was fixed to the vault with 2/0 Polydioxanone sutures.
For the posterior mesh, a full thickness midline incision was made on the posterior vaginal wall using the same hydrodissection technique to allow reflection of the vagina from the underlying pre rectal tissue.
Dissection was undertaken to allow access to the ischial spines and sacrospinous ligaments bilaterally. Mesh was overlaid onto the rectovaginal fascia and attached to the perineal body.
59 patients of the above series consented to a prospective symptom assessment both preoperatively and up to a 4 year period following transvaginal mesh insertion. Postal questionnaires were sent to patients up to 4 years postoperatively.
The validated International Consultation on Incontinence Modular Questionnaire–Vaginal Symptoms (ICIQ–VS) was used to analyse and quantify vaginal symptoms including subjective success, quality of life outcomes and patient satisfaction for up to 4 years. Comparison between baseline and follow-up data was analysed using Student’s t test.
Results
159 consecutive women underwent a transvaginal mesh (TVM) repair by a senior experienced urogynaecologist.
60 % (n = 96/159) patients underwent a Posterior TVM.
10 % (n = 16/159) patients had an Anterior TVM and 29 % (n = 47/159) patients had a Total TVM with or without concomitant surgery. 20 % (n = 33/159) patients of the study group had a concomitant mid urethral sling (MUS) procedure. All patients undergoing concomitant MUS had preoperative urodynamic investigations confirming stress urinary incontinence.
Average age of the study population was 63 years (range 39–87 years).
Mean BMI was 28.5 (range 20–40). 86 % (n = 138/159) had a previous hysterectomy.
93 % (n = 149/159) were postmenopausal. 98 % (n = 156/159) patients did not have any intraoperative complications. 0.62 % (n = 1/159) had a bladder injury. 1 % (n = 2/159) patients had a blood loss of greater than 500 ml. Intraoperative bleeding necessitated a blood transfusion in 0.62 % (n = 1/159) of patients. 8 % (n = 14/159) had pyrexia (1 episode -24 h) postoperatively. 98 % (n = 157/159) patients had 48 h of intravenous antibiotics postoperatively.
One patient with bladder injury had an indwelling Foley’s catheter for 10 days.
15 % (n = 24/159) were lost to follow-up.
At follow-up, 29 % (n = 40/135) reported bladder symptoms. 47 % (n = 19/40) reported symptoms of urgency. 25 % (n = 10/40) developed de novo stress urinary incontinence. 2 % (n = 1/40) complained of slow flow whilst voiding. 12 % (n = 5/40) had sensation of incomplete emptying with high residuals. 2 % (n = 1/40) needed intermittent self catheterisation. 2 % (n = 1/40) reported occasional trickling of urine. 5 % (n = 2/40) reported recurrent urinary tract infections and 2 % (n = 1/40) reported 1 episode of urinary tract infection.
3 % (n = 4/135) in the study group reported dyspareunia at follow-up.
Mesh exposure in the follow-up group was noted to be 4 % (n = 6/135).
6 % (n = 2/33) patients who had a concomitant midurethral sling procedure needed release/revision of the tape due to poor voiding post operatively.
Patient characteristics are recorded in Tables 1 and 2. The majority were postmenopausal.
60.37 % (n = 96/159) patients had a Posterior TVM.
75 % (n = 72/96) of the posterior TVM group had a concomitant surgical procedure. 52 % (n = 39/74) had Posterior TVM + Anterior repair, 12 % (n = 9/74) had a Posterior TVM + MUS, 17 % (n = 13/74) had Posterior TVM + Anterior repair + MUS, 9 % (n = 7/74) had Posterior TVM + Vaginal hysterectomy + Anterior repair, 1 % (n = 1/74) had Posterior TVM + Vaginal adhesion release, 1 % (n = 1/74) had Posterior TVM + Removal of exposed anterior mesh fibres, 1 % (n = 1/74) had Posterior TVM and Peri urethral bulking agent, 1 % (n = 1/74) had Posterior TVM + MUS + Anterior repair + Excision of mesh from Transobturator tape.
10 % (n = 16/159) patients underwent an anterior TVM.
37 % (n = 6/16) of the Anterior TVM group had an additional surgical procedure.
66 % (n = 4/6) had an Anterior TVM and MUS, 16 % (n = 1/6) had an Anterior TVM with a posterior repair and 16 % (n = 1/6) had an Anterior TVM, posterior repair and MUS.
29 % (n = 47/159) patients had total TVM.
14 % (n = 7/47) of the Total TVM group had a concomitant surgical procedure.
41 % (n = 5/12) had a Total TVM and MUS. 16 % (n = 2/12) had a Total TVM with vaginal hysterectomy (Table 3).
Following surgery, urethral catheter was removed as per protocol at 48 h in all patients. 10 % (n = 16/159) patients needed recatheterisation for a week due to incomplete emptying of the bladder and high residuals. 25 % (n = 4/16) of these patients had a MUS procedure along with their mesh repair. 2 of these 4 patients had an unsuccessful trial without catheter and needed release of the tape.
Of the remaining 12 of the 16 patients, 50 % (n = 2/12) had an unsuccessful trial without catheter and required a suprapubic catheter (Table 4).
Our reoperation rate to correct postoperative complications associated with transvaginal mesh surgery was 9 % (n = 13/135). Mesh exposure was noted in 4.4 % cases at follow-up (n = 6/135) (Table 5).
14 % (n = 19/135) reported symptoms of urgency at follow-up. Of these, 5 % (n = 1/19) were from the Anterior TVM group, 5 % (n = 1/19) from the Anterior TVM and MUS group, 36 % (n = 7/19) from the Posterior TVM group, 36 % (n = 7/19) from the Posterior TVM with MUS group, 10 % (n = 2/19) from the Total TVM group and 5 % (n = 1/19) from the Total TVM with MUS group. 15 % (n = 3/19) underwent Intradetrusor Botox for overactive bladder.
59 patients of the 159 patients consented to preoperative and postoperative ICIQ–VS questionnaires.
51 patients completed both the preoperative and the postoperative ICIQ–VS questionnaire. The median duration of follow-up was 28 months (range 1–48 months). The mean age was 62 years (range 40–79 years). 88 % (n = 45/51) were postmenopausal. 50 % (n = 26/51) were sexually active.
11 % (n = 6/51) underwent Anterior TVM, 64 % (n = 33/51) underwent a Posterior TVM and 23 % (n = 12/51) had a Total TVM with or without a concomitant procedure.
Patient reported outcome measures for transvaginal mesh.
Dragging pain
82 % (n = 42/51) had complaints of dragging pain in the vagina preoperatively. Postoperatively, this had reduced to 41 % (n = 21/51). Average scores were 1.83 preoperatively and 1.05 postoperatively showing a statistically significant improvement in symptoms (p < 0.05).
Vaginal soreness
72 % (n = 37/51) had complaints of soreness in the vagina preoperatively. This was reduced to 49 % (n = 25/51). Average scores were 1.19 preoperatively and 0.74 postoperatively. This was statistically significant (p < 0.05).
Reduced vaginal sensation
55 % (n = 28/51) had complaints about reduced sensation in the vagina preoperatively. This reduced to 45 % (n = 23/51) postoperatively. Average scores were 1 preoperatively and 0.7 postoperatively. This difference was statistically significant (p < 0.05).
Vaginal laxity
73 % (n = 37/51) had complaints about the vaginal laxity preoperatively. This reduced to 31 % (n = 16/51) postoperatively. Average scores were 1.49 preoperatively and 0.5 postoperatively. This was a statistically significant improvement (p < 0.05).
Awareness of lump in the vagina
80 % (n = 41/51) complained of an awareness of a lump in the vagina. This reduced to 27 % (n = 14/51). Average scores were 2.49 preoperatively and 0.6 postoperatively (p < 0.05).
Visible lump in the vagina
60 % (n = 31/51) complained of being able to see a lump in the vagina. This reduced to 16 % (n = 8/51). Average scores were 1.64 preoperatively and 0.3 postoperatively (p < 0.05).
Vaginal dryness
71 % (n = 36/51) complained about dryness of the vagina preoperatively. This reduced to 62 % (n = 32/51). Average scores were 1.5 preoperatively and 1.1 postoperatively (p < 0.05).
Need to splint or digitate into the vagina to help defaecation
19 % (n = 10/51) patients needed to digitate into or splint the vagina to open the bowel preoperatively. This reduced to 15 % (n = 8/51) postoperatively. Average scores were 0.94 preoperatively and 0.2 postoperatively. This was a statistically significant improvement (p = 0.0004).
Awareness of the vagina being tight
17 % (n = 9/51) felt their vagina was too tight preoperatively. This stayed the same with 17 % (n = 9/51) feeling their vagina was too tight postoperatively. Average preoperative score was 0.27 and was 0.35 postoperatively. This was not statistically significant (p = 0.49).
Average quality of life scores
The average quality of life (QOL) scores were 6.7 preoperatively and 2.5 postoperatively. This was a statistically significant improvement (p < 0.05). The average vaginal symptom score was 22.25 preoperatively and 9.74 postoperatively. This was statistically significant (p < 0.05).
Average sexual matters score was 33 preoperatively and 30 postoperatively (p = 0.75).
Discussion
Successful surgical outcome is based on various factors such as correct identification of the pathology, correct patient selection, appropriate surgeon in terms of high volume experience and training and correct surgical technique. Knowledge of anatomy, identification of anatomical landmarks and surgical planes along with use of techniques such as hydrodissection to facilitate the operative process helps improve surgical outcomes.
We believe that surgical skill, experience and correct technique of mesh placement are vital for reducing complications during transvaginal mesh surgery.
An accurate dissection of tissues during surgery may be vital not only to reduce tissue damage and minimise disruption to the micro blood supply, but also to help reduce risks of haematoma formation. Haematomas are known to encourage infection and may decrease early mesh adherence and fibroblast ingrowth. Surgical expertise is vital for accurate placement of the mesh between the vagina and the bladder or the rectum. Placing the mesh within the vaginal wall itself may lead to interference with vaginal wall integrity and ultimately to mesh exposure.
Suburethral mesh remains the gold standard for the treatment of stress urinary incontinence, yet use of vaginal mesh for repair of prolapse has fallen into disrepute. The large area of mesh for transvaginal reinforcement necessitates a precise and accurate surgical technique to minimise intraoperative complications. Once training and surgical experience has been gained, complication rates for technically challenging procedures can be minimised. Complications associated with transvaginal mesh repair impair the patients’ quality of life and exposes the operating surgeon to litigation. Patient selection along with appropriate surgical expertise contributes towards lower intraoperative complication rates. Our study shows that in a large consecutive series of patients involving a single trained experienced surgeon, there were no major complications, minimal postoperative morbidity and statistically significant improvement in patient symptoms.
A previous retrospective study of 524 patients reported a global reoperation rate of 11 % [8]. Our global reoperation rate to correct postoperative complications related to the mesh procedure was 9 % (n = 13/135).
One multicenter study of 248 women undergoing transvaginal mesh repair reported visceral injury in 4.4 % of patients (n = 11/248). Minor complications occurred in 14.5 % of patients (n = 36/248) [9].
Our intraoperative complication rate was 2 %. A 0.5 cm bladder defect was noted in 0.62 % (n = 1/159) and was repaired intraoperatively with no long term consequences. There were no other visceral injuries and only 0.62 % (n = 1/159) needed a blood transfusion. In a multicenter RCT, rates of bladder perforation were found to be 3.5 % in the mesh-repair group and new stress urinary incontinence after surgery was 12.3 % [10].
Mesh retraction has been associated with de novo detrusor overactivity symptoms and vaginal pain [11]. In our group, 7 % (n = 10/135) had symptoms of de novo stress urinary incontinence. 14 % (n = 19/135) patients in our group had symptoms of urgency. Of these, only 10 % (n = 2/19) had a mesh exposure at follow-up.
3 % (n = 5/135) patients in our group had vaginal pain at follow-up. Of these, 2 patients needed division of vaginal adhesions, 1 patient required removal of the mesh and 1 patient needed release of mesh strap.
Several studies indicate that greater surgical experience is correlated with fewer mesh complications [5, 12]. Surgeons experienced in the operative technique of transvaginal mesh surgery have less mesh exposure compared to less experienced surgeons (2.9 vs 15.6 %, p = 0.02) [6].
A retrospective multicenter study of 289 women found a vaginal erosion rate of 10 % was noted [13]. A systematic review of 110 studies reported similar erosion rates of 10.3 %. Dyspareunia rates in this meta-analysis were described as being 9 % [14]. Statistical analysis of the learning curve of bilateral anterior sacrospinous ligament suspension associated with anterior mesh repair in a single centre showed that the risk of major complications was reduced by approximately 30 % every ten procedures (HR = 0.71, 95 % CI 0.53–0.95). The rate of mesh exposure was found to be 3.6 % [15].
In a review on functional outcomes after transvaginal mesh surgery, 7–33 % reported symptomatic recurrence of pelvic organ prolapse, 12–17 % reported de novo stress urinary incontinence which persisted in up to 68 % after trocar guided mesh surgery and 2–15 % reported de novo dyspareunia [16].
High anatomic cure rates following mesh repair with a 5 % mesh exposure rate was noted in a single centre observational study [17]. Mesh exposure rates in our study population were noted to be 4 % (n = 6/135) and 2 % (n = 4/135) reported dyspareunia in our group.
Sacrospinous vault fixation is an alternative option for post hysterectomy vault prolapse repair. However, a high incidence of recurrent cystocele ranging from 8 to 30 % has been noted [18].
A cross-sectional study of patients undergoing anterior pelvic floor repair with mesh reported high QOL scores 2 years post surgery [19]. QOL scores were noted to be significantly improved after mesh repair in a prospective multicenter study [20]. Our prospective study also showed a significant improvement in QOL scores postoperatively.
Hysterectomy concurrently performed with transvaginal mesh seems to increase mesh erosion rates [21]. 5 % (n = 9/159) had a concomitant hysterectomy along with the mesh procedure in our audited population. No mesh exposure was identified in this group.
Smoking has been associated with a threefold increased risk of developing erosions and age contributed to a 1.6-fold increased risk [22]. A 10.1-fold increase in the risk of developing erosions was present if BMI was greater than 30 [23].
26 % (n = 19/73) were recorded as being smokers and one of these patients was diagnosed with a mesh exposure.
We speculate that careful patient selection, adequate training, precise standardised technique and high surgical volume contributed to the low rate of intraoperative complications and the results reflect those that can be expected from an experienced urogynaecologist fully trained in transvaginal mesh technique. This report may help to give a more realistic view of the true value of transvaginal mesh without the confounding problem of inexperience or inadequate training.
Conclusion
98 % of our patients undergoing transvaginal mesh did not have any intraoperative complications. Mesh exposure was noted in 4 % (n = 6/135). 2 % (n = 4/159) reported dyspareunia. 29 % (n = 40/135) experienced postoperative bladder symptoms. 9 % (n = 13/135) patients needed further surgery to address postoperative complications due to the mesh.
A statistically significant improvement was noted in most arms of the vaginal symptoms questionnaire at long term-follow up suggesting that the transvaginal mesh has an important role to play in the management of pelvic organ prolapse and improvement in quality of life.
The transvaginal mesh is an important alternative choice for women with recurrent prolapse after failed conventional repair techniques or those with failed sacrocolpopexy or sacrospinous fixation. Emphasis must be placed on appropriate patient selection, standardising surgical technique and accredited training. Throwing the baby out with the bath water would mean the loss of a valuable technique that can effectively and safely treat severe and recurrent prolapse.
Limitations
Small cohort of patients for the prospective study. To our knowledge, however, it is the largest cohort of patients operated by a single surgeon and has the longest term follow-up data.
References
Olsen AL et al (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506
Maher C et al (2013) Surgical management of pelvic organ prolapse in women. Cochrane Datab Syst Rev 4:CD004014
Propst K et al (2014) Pyogenic spondylodiscitis associated with sacral colpopexy and rectopexy: report of two cases and evaluation of the literature. Int Urogynecol J 25(1):21–31
Ashok K, Petri E (2012) Failures and complications in pelvic floor surgery. World J Urol 30(4):487–494
van Geelen JM, Dwyer PL (2013) Where to for pelvic organ prolapse treatment after the FDA pronouncements? A systematic review of the recent literature. Int Urogynecol J 24(5):707–718
Achtari C et al (2005) Risk factors for mesh erosion after transvaginal surgery using polypropylene (Atrium) or composite polypropylene/polyglactin 910 (Vypro II) mesh. Int Urogynecol J Pelvic Floor Dysfunct 16(5):389–394
Haylen BT et al (2011) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) & grafts in female pelvic floor surgery. Int Urogynecol J 22(1):3–15
de Landsheere L et al (2012) Surgical intervention after transvaginal Prolift mesh repair: retrospective single-center study including 524 patients with 3 years’ median follow-up. Am J Obstet Gynecol 206(1):83e1–83e7
Altman D, Falconer C (2007) Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol 109(2 Pt 1):303–308
Altman D et al (2011) Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med 364(19):1826–1836
Rogowski A et al (2013) Mesh retraction correlates with vaginal pain and overactive bladder symptoms after anterior vaginal mesh repair. Int Urogynecol J 24(12):2087-2092
Vaiyapuri GR et al (2011) Use of the Gynecare Prolift system in surgery for pelvic organ prolapse: 1-year outcome. Int Urogynecol J 22(7):869–877
Abdel-Fattah M, Ramsay I (2008) Retrospective multicentre study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG Int J Obstet Gynaecol 115(1):22–30
Abed H et al (2011) Incidence and management of graft erosion, wound granulation, and dyspareunia following vaginal prolapse repair with graft materials: a systematic review. Int Urogynecol J 22(7):789–798
de Tayrac R et al (2012) Analysis of the learning curve of bilateral anterior sacrospinous ligament suspension associated with anterior mesh repair. Eur J Obstet Gynecol Reprod Biol 165(2):361–365
Baessler K (2012) Do we need meshes in pelvic floor reconstruction? World J Urol 30(4):479–486
Khan ZA, Thomas L, Emery SJ (2014) Outcomes and complications of trans-vaginal mesh repair using the Prolift kit for pelvic organ prolapse at 4 years median follow-up in a tertiary referral centre. Arch Gynecol Obstet 290(6):1151–1157
Cvach K, Dwyer P (2012) Surgical management of pelvic organ prolapse: abdominal and vaginal approaches. World J Urol 30(4):471–477
Hefni M et al (2013) Long-term quality of life and patient satisfaction following anterior vaginal mesh repair for cystocele. Arch Gynecol Obstet 287(3):441–446
Yesil A, Watermann D, Farthmann J (2014) Mesh implantation for pelvic organ prolapse improves quality of life. Arch Gynecol Obstet 289(4):817–821
Baessler K, Maher CF (2006) Mesh augmentation during pelvic-floor reconstructive surgery: risks and benefits. Curr Opin Obstet Gynecol 18(5):560–566
Araco F et al (2008) Risk evaluation of smoking and age on the occurrence of postoperative erosions after transvaginal mesh repair for pelvic organ prolapses. Int Urogynecol J Pelvic Floor Dysfunct 19(4):473–479
Araco F et al (2009) The influence of BMI, smoking, and age on vaginal erosions after synthetic mesh repair of pelvic organ prolapses. A multicenter study. Acta Obstet Gynecol Scand 88(7):772–780
Acknowledgments
Mrs Pat McFadden, Medical secretary whose help was invaluable in collection of patient records.
Conflict of interest
We declare we have no conflict of interest. I have had full control of all primary data and I agree to allow the journal to review data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balchandra, P., Marsh, F. & Landon, C. Perioperative outcomes and prospective patient reported outcome measures for transvaginal mesh surgery. Arch Gynecol Obstet 292, 875–882 (2015). https://doi.org/10.1007/s00404-015-3724-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3724-z