Abstract
This study evaluated the influence of age and smoking on the occurrence of vaginal erosions after transvaginal mesh repair of pelvic organ prolapses. We recruited all patients that underwent mesh correction of prolapses and excluded those with stress urinary incontinence, ongoing clinical infections, with a complete antibiotic course in the last 6 months, and with systemic diseases affecting tissue oxygenation. We enrolled 325 patients. Postoperative erosions were present in 6%. Age conferred a 1.6-fold increase in the risk to develop erosions while smoking a threefold increase. Patients with deep erosions had the highest values of pack years, and 6.85 pack years conferred a risk similar to advanced age. Age and smoking are important factors also after pelvic organ prolapse surgery. Our data could be used to stratify patients according to their estimated risk and to dedicate them to specific cares for prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Synthetic prostheses, widely accepted in general surgery, have been successfully introduced in gynecology for the treatment of stress urinary incontinences (SUIs) and of pelvic floor prolapses (POPs) [1]. Although advantages of small incisions and minimal surgical traumas immediately rendered these techniques attractive, specific complications, such as mesh vaginal erosions, seriously endangered the functional outcome [2]. Several factors contribute to the occurrence of postoperative erosions including the operative technique, implant size, and the specific properties of the sling material (pore size, stiffness, elasticity, and basic tissue compatibility). Even if their incidence is not related to the way used to place the tape (suprapubic or transobturator), placement of the sling in a plane too close to the urethra, the presence of inadequate vaginal tissue coverage, poor vaginal tissue vascularity, or bacterial infections (secondary to a draining hematoma or seeding of the mesh) may lead to early sling erosion/extrusion. Furthermore, poor tissue irrigation, local ischemia, poor mesh incorporation, and early resumption of sexual activities can also influence their occurrence [2–4].
Age and smoking are two important factors that usually impair wound healing. Laboratory and patient studies dating back almost a century describe an age-related decline in the rate of repair [5], and more recent works defined age-related alterations in the proliferative aspects of repair involving all aspects of wound healing, such as keratinocyte proliferation, inflammatory cells, matrix deposition, and neoangiogenesis [6–12]. On the contrary, the effects of cigarette smoking on wound healing were studied for the first time by Mosely and Finseth in 1977 [13], establishing that recovery from injuries is usually compromised in smokers patients [14]. Since then, many studies have shown that cigarette smoking leads to an increased incidence of postoperative wound infections, flap necroses (i.e., after face liftings, abdominoplasties) [15–16], wound dehiscences, and a general increase in overall complication rates [17–18]. All of them confirm a role of cigarettes in the cutaneous processes of healing, increasing the risk of infections especially in operations that require a perfect vascularization for healing (i.e., abdominoplasty) or that permanently introduce foreign bodies in the organism (breast augmentations) [18–20].
It is our working hypothesis that, as in other types of surgery, aging and smoking can alter the tissue oxygenation and influence the occurrence of vaginal erosions after prosthesis-based repair of POP. For this reason, we conducted this prospective trial to determine whether a significant relationship existed.
Materials and methods
The study received approval of the Institutional Ethics Committee. After a careful explanation about purposes and risks, patients were asked to participate to the study and had an informed consent signed. We prospectively recruited patients aged 45–75 years that underwent mesh correction of POP. All operations were conducted in an inpatient setting at the University “Tor Vergata” in Rome. We excluded patients affected by SUI (for the requirement of the additional sling), with ongoing clinical infections, that received a complete antibiotic course in the last 6 months before operation and with systemic diseases that adversely affect wound healing by impairing tissue oxygenation (cardiovascular diseases, hypertension, diabetes mellitus). Patients with SUI were diagnosed preoperatively with a urodynamic evaluation. When all conditions were satisfied and the inclusion/exclusion criteria of the study were met, patients were investigated about their smoke habits (specifically, the number of cigarettes smoked/day and the overall years of smoking), adopting a simplified version of the World Health Organization’s MONICA Manual Smoking Questionnaire [21]. In all patients, the smoking status was also confirmed by direct questioning of first-degree relatives.
Preoperative care
According to standard prophylaxis measures of deep venous thrombosis (DVT), low-molecular-weight heparin was administered (Clexane 4,000 UI) 1 h before the operation along with elastic stockings/mechanical calf compression until complete mobilization was obtained. Infection prophylaxis was administered with one dose of intravenous (i.v.) cefuroxime 750 mg (erythromycin—1 g i.v.—if specific allergies were referred) 10–30 min before the operation.
Surgical techniques
Prostheses were introduced via the anterior or posterior approach [22–24]. For anterior repair, the anterior vaginal wall was infiltrated with a local anesthetic (0.5% lignocaine), and a midline incision was made 2 cm below the external urethral meatus. The bladder was reached by blunt dissection from the vagina and paravescical spaces individuated. Two tiny skin incisions were made on the genitor-femoralis fold, near the hymen, and two other incisions more caudally and laterally. A tunneller, with the prosthesis included (GyneMesh-Soft PS, 10 × 15 cm, Gynecare Ethicon), was introduced in the obturator foramen and passed through the obturator membrane and obturator internal muscle until it reached the vagina. At this point, the prosthesis was anchored and the arms distended. Finally, the anterior vaginal incision was closed with 3/0 absorbable suture. For posterior repair, the posterior vaginal wall was infiltrated with 0.5% lignocaine. A midline vertical posterior vaginal incision was made, the rectus was reached by blunt dissection from the vagina, and pararectal spaces were individuated. Two small skin incisions for each side were made on the glutei, 3 cm posterior and lateral to the anal verge. A tunneller was introduced, with the prosthesis, and passed through the ischiatic fossa and exited on the para-rectal space. The posterior colpotomy was closed with 3/0 absorbable suture.
Postoperative care
Antibiotics were administered 12 and 48 h after the operation, and DVT prophylaxis continued until complete mobilization. Tramadol was usually given on patient’s request as analgesic. Patients without complications were discharged home 3 days after the operation. Outpatient follow-up visits were planned at the 7th, 14th, and 30th postoperative day and after 6 months. Postoperative vaginal erosions were defined on the basis of clinical signs (vaginal mucosa split, mesh exposure, pain, swelling, purulent drainage) and classified as superficial or deep [2, 25]. Superficial erosions were defined as those inferior to 2 cm in diameter or that involving just the vaginal mucosa with no evident signs of infection. They were managed by resuturing the vaginal mucosa in local anesthesia and, when mesh was exposed, resecting a small piece of it. When signs of local infection were present or the antibiogram was positive for pathogens, an oral antibiotic course was started. Deep erosions were defined as those greater than 2 cm in diameter, involving tissues deep below the mucosa and with evident signs of infection. In these cases, patients were readmitted to the hospital, and the mesh was removed in general anesthesia. After 8 weeks from the removal, it was reinserted.
The aim of this study was to assess if age and cigarette smoking influenced the incidence of vaginal erosions after synthetic mesh correction of POP. We recorded the age, weight, height, body mass index, number of previous vaginal deliveries, previous hysterectomies, associated pathologies, smoking status, number of cigarettes smoked/day, overall years of smoke, operative time, type of repair (anterior, posterior, both), number of catheterization days, postoperative necessity of recatheterization, complications (vaginal or bladder perforations, hematomas, obstructions, dyspareunia, superficial and deep vaginal erosions), recurrences, and reoperations. To evaluate the influence of chronic smoking and its amount on the occurrence of vaginal erosions, we calculated the number of pack years according to the National Cancer Institute definition (=number of packs smoked per day × number of years as a smoker).
A previous pilot evaluation of patients recovered in our institution found that 45–75 years was the most frequent class of age, and the recorded incidence of vaginal erosions was 3% (similar to that described in literature) [1]. An age cutoff was determined with receiver operating characteristic (ROC) curves to find the greatest areas of sensitivity and specificity: It corresponded to an area of 0.6 (sensitivity = 0.56; specificity = 0.75). To end the study in 5 years, without excessive costs and with a resulting test power of 90% (significance level = 0.05), 40 patients were needed for each group (younger vs older age and smokers vs no smokers), comprehensive of five patients in excess to balance an estimated dropout of 25% during the study and/or follow-up. The enrolment was conducted with a controlled strategy that allowed the obtaining of initially two groups according to the previously determined cutoff (younger patients [45–59 years] vs older patients [60–75 years]), subsequently classified into smokers vs nonsmokers. All patients presented in the hospital with a random access, to undergo routine preoperative investigations and for a final revision of surgical indications, and on that occasion were recruited.
Statistical analysis
All data analysis and calculation of sample size were performed using the Statistical Package for the Social Sciences Windows version 13.0 (SPSS, Chicago, IL). Descriptive statistics for quantitative continuous variables were the mean and standard deviation after confirmation of normal distribution, otherwise median and range. Normality assumptions have been demonstrated with histograms, Kolmogorov–Smirnov, and Shapiro–Wilk testings. Descriptive statistics for qualitative categorical variables was performed with frequencies.
Comparison for groups homogeneity was performed with the Student’s t test for continuous parametric variables, the Mann–Whitney test for continuous nonparametric, and the chi-squared test or Fisher’s exact test for categorical variables (Fisher’s if counts were inferior to 5). The odds ratio of age and smoking on the occurrence vaginal erosions was calculated. All p values were considered significant if inferior to 0.05.
Results
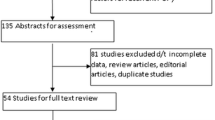
We followed the Consolidated Standards for Reporting of Trials criteria for the development and description of this trial [26]. The study began in January 2002 and ended in December 2006 with the recruitment of the last patient. We evaluated 397 patients and enrolled 343 of them. Twenty-five patients were excluded because of age (8 for age < 45 years, 17 for age > 75 years); 19 patients were excluded because they were affected by cardiac ischemic disease (n = 6), hypertension (n = 9), or diabetes mellitus (n = 4); four patients were excluded because they were affected by SUI and six patients because had received an antibiotic course in the previous 6 months to the operation. Eighteen patients were lost to follow-up, and 325 remained for the analysis.
Demographics and clinical characteristics are summarized in Table 1 and associated pathologies in Table 2. All tests used for normality confirmation proved a normal distribution for all variables exception that made for the number of pack years, operating times, and days of catheterization. We recorded 19 vaginal erosions (6%), 13 superficial and 6 deep. They occurred after a mean of 11 ± 3 days, superficial after 6 ± 2 days and deep infections after 29 ± 4 days. The most common organism isolated was the Staphylococcus epidermidis. No cases of bladder perforations, hematomas, deep vein thrombosis, or pulmonary embolism were observed. Patients were discharged home after a median of 4.3 days (range 3–6). The mean follow up was 22 months (range 13–48).
The z test and the chi-squared test confirmed that all groups (smokers vs nonsmokers and younger vs older patients) were homogeneous for variables analyzed (Table 1). According to the age of patients, we had 6 (4%) patients with erosions in the younger group and 13 (9%) in the older group (chi-squared; p < 0.05). Superficial erosions occurred in five (3%) patients of the younger group and eight (5%) of the older group (Fisher’s exact test; not significant [NS]). Deep erosions occurred in one patient (1%) of the younger group and in five (3%) of the older group (Fisher’s exact test; NS). The analysis of erosions occurrence showed significant differences for age between patients that developed them vs those erosion-free (62 ± 7 vs 59 ± 7 years; t test: p < 0.05).
Thirteen vaginal erosions occurred in smokers (9.5%) and six in nonsmokers (3.2%; chi-squared test; p < 0.05). Nine superficial erosions occurred in smokers (6.6%) and four in nonsmokers (2.1%; chi-squared test; NS). Four deep erosions occurred in smokers (2.9%) and two in nonsmokers (1.1%; Fisher’s exact test; NS). The analysis of erosions occurrence in smokers showed no significant differences between patients that developed them vs those erosion-free for the number of pack years (13 [5–31] vs 13 [3–31]; Mann–Whitney test: NS). Those that developed deep infections had the highest values when compared to overall smokers, and the difference was significant (number of pack years 25 [19–31] vs 13 [3–31]; Mann–Whitney test: p < 0.05). Such difference remained significant also when smokers with deep erosions were compared with those with superficial erosions (number of pack years 25 [19–31] vs 8 [5–31]; Mann–Whitney test: p < 0.05).
In all patients, the analysis of age (cutoff value of 60 years) and smoke (smokers vs nonsmokers) determined four different subgroups for the occurrence of vaginal erosions and OR (Fig. 1). Smokers had an incidence of 10% (13 of 137) and nonsmokers of 3% (6 of 188), corresponding to an OR of 3. Older patients had an incidence of 9% (13 of 151) and younger patients of 4% (6 of 174), with an OR of 2.5. In smokers, the incidence in older patients was 11% (10 of 93) and in younger of 7% (3 of 44), with an OR of 1.6. In nonsmokers, the incidence in older patients was 5% (3 of 58) and in younger 2% (3 of 130), with an OR of 2.3. In older patients, the incidence in smokers was 11% (10 of 93) and in nonsmokers 5% (3 of 58), with an OR of 2. In younger patients, the incidence in smokers was 7% (3 of 44) and in non smokers 2% (3 of 130), with an OR of 3.
Scatter plot showing the age (younger and older patients) vs pack years for the occurrence of vaginal erosions. Vertical continue line: cutoff between smokers and nonsmokers. Vertical dot line: cutoff between lighter and heavier smokers (6.85 pack years). Horizontal line: cutoff between older and younger patients (60 years)
A cutoff value of 6.85 pack years conferred a risk of postoperative erosions similar to that added by the age greater than 60 years (Fig. 1). Such cutoff was determined with ROC curves (area of 0.663; sensitivity = 0.53; specificity = 0.70). In heavier smokers (>6.85 pack years), the incidence in older patients was 11% (8 of 70) and in younger 6% (2 of 33), with an OR of 2. In lighter smokers and nonsmokers, the incidence in older patients was 6% (5 of 81) and in younger 3% (4 of 141), with an OR of 2.
Discussion
Vaginal erosions are important complications reported in up to 22% of cases after POP mesh repair. The exact causes are unclear, and probably several factors contribute to the wide range of erosion/extrusion rates, including operative technique, implant size, the specific properties of the sling material, poor tissue irrigation, local ischemia, poor mesh incorporation, and subclinical infection [3]. However, to date, no author specifically investigated the influence of age and/or smoking on the occurrence of such complications.
Laboratory and patient studies dating back almost a century describe an age-related decline in the rate of repair [5]. The majority of more recent studies define alterations in the proliferative aspects of repair involving keratinocyte proliferation [6] and changes in the function of inflammatory cells (macrophage and T cell) with alterations in chemokine content and phagocytic functions [7–8]. Furthermore, a reduced extracellular matrix synthesis is present in the aged skin [8] that derives from decreased tissue inhibitor of matrix metalloproteinase levels and a reduced deposition of matrix components [9–10]. Finally, angiogenesis is impaired [11] because of a reduced sprouting of aged microvessels [12].
Smoking usually increases the risk of postoperative complications in almost all types of surgery [27]. Different studies on plastic surgery patients correlated its influence on wound repair and tissue regeneration ability [19, 28–32]. In fact, principal components of tobacco (nicotine, nitric oxide, and carbon monoxide) influence wound healings in peripheral tissues [33–35]; the dermis, that has the highest sympathetic innervation, is particularly sensitive to the vasoconstrictive effects of smoking [36–37], and the increased level of carboxyhemoglobin and of platelet adhesiveness lead to microtrombi formation and a reduced ability to deliver oxygen [38–39]. Finally, increased serum levels of fibrinogen and of hemoglobin, a decreased fibrinolytic activity, and the direct endothelial injury [40–41] all contribute to the reduced local circulation.
The analysis of our patients showed that postoperative erosions were present in 6% of patients (n = 19), similar to that reported in literature [1], and that most of them (n = 13; 68%) were superficial. Most erosions (13 of 19; 68%) occurred in older patients (mean age in this group = 65 years; mean age of younger patients = 53 years), and age conferred a 1.6-fold increase in the chance of developing vaginal erosions. For these reasons, age could be an important factor that influences erosion occurrence, as usually happens in other types of surgery, possibly affecting tissue oxygenation and the organism’s ability to repair wounds. Furthermore, most erosions (13 of 19; 68%) occurred in smokers, and cigarette smoking conferred a threefold increase in the chance of developing vaginal erosions. In this case, the analysis showed that not only the smoking status but also the amount of smoking seemed to have an influence on the occurrence of erosions. In fact, smoker patients that developed deep erosions had the highest values of pack years when compared to those that experienced superficial infections and overall smokers. In this case, few simple questions during the process of history taking and the simple calculation of pack years could help the caregivers to roughly evaluate the patient’s risk to develop erosions. Finally, 6.85 pack years was the amount of smoked cigarettes that conferred a risk of erosions similar to that added by 12 years (the age difference between groups). Such data confirm that, as in other types of surgery, smoke influences the tissue ability to repair wounds and increase the incidence of postoperative complications derived from an impaired microcirculation and oxygenation.
Our study is a large and highly selected study that enrolled patients over 5 years. However, as it began in 2002, we did not perform a dosage of specific metabolites in the urine (i.e., Cotinine) or an extensive and specific preoperative pulmonary evaluation to objectively evaluate the amount of cigarettes smoked by patients. Fortunately, no patient reported to have quitted smoking or smoked only sporadically, and all those analyzed had a regular habit. However, to have a more objective estimate, in all smokers, the amount of cigarettes smoked per day and the number of years was confirmed by direct questioning to first-degree relatives. Furthermore, although the study was designed to evaluate the occurrence of all postoperative vaginal erosions, those that would seem to really matter are the ones requiring mesh removal. In this case, our study is underpowered, and future larger ones are necessary to confirm our data also in this subgroup of patients.
Conclusions
In our series, the incidence of vaginal erosions in patients undergoing POP repair with prostheses is 6%. Age greater than 60 years had a risk of 1.6, while smoking of 3.0. Results of this study would suggest that patients prone to develop erosions could be easily identified preoperatively by the class of age and the smoking status. Our data, if confirmed by future studies, could be used to stratify patients according to their estimated risk and dedicate them specific cares for prevention.
References
Huebner M, Hsu Y, Fenner DE (2006) The use of graft materials in vaginal pelvic floor surgery. Int J Gynaecol Obstet 92(3):279–88
Deval B, Haab F (2006) Management of the complications of the synthetic slings. Curr Opin Urol 16(4):240–243
Cervigni M, Natale F (2001) The use of synthetics in the treatment of pelvic organ prolapse. Curr Opin Urol 11(4):429–435
Belot F, Collinet P, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2005) Risk factors for prosthesis exposure in treatment of genital prolapse via the vaginal approach. Gynecol Obstet Fertil 33(12):970–974
DeNouy PL (1916) Cicatrization of wounds. J Exp Med 24:461–470
Gilchrest BA (1983) In vitro assessment of keratinocyte aging. J Invest Dermatol 81:184s–189s
Swift ME, Burns AL, Gray KL, DiPietro LA (2001) Age-related alterations in the inflammatory response to dermal injury. J Invest Dermatol 117(5):1027–1035
Ashcroft GS, Horan MA, Ferguson MW (1997) Aging is associated with reduced deposition of specific extracellular matrix components, an upregulation of angiogenesis, and an altered inflammatory response in a murine incisional wound healing model. J Invest Dermatol 108:430–437
Ashcroft GS, Herrick SE, Tarnuzzer RW, Horan MA, Schultz GS, Ferguson MW (1997) Human ageing impairs injury-induced in vivo expression of tissue inhibitor of matrix metalloproteinases (TIMP) -1 and -2 proteins and mRNA. J Pathol 183:169–176
Ashcroft GS, Horan MA, Herrick SE, Tarnuzzer RW, Schultz GS, Ferguson MW (1997) Age-related differences in the temporal and spatial regulation of matrix metalloproteinases (MMP) in normal skin and acute cutaneous wounds of healthy humans. Cell Tissue Res 290:581–591
Reed MJ, Corsa A, Pendergrass W, Penn P, Sage EH, Abrass IB (1998) Neovascularization in aged mice: delayed angiogenesis is coincident with decreased levels of transforming growth factor beta1 and type I collagen. Am J Pathol 152:113–123
Arthur WT, Vernon RB, Sage EH, Reed MJ (1998) Growth factors reverse the impaired sprouting of microvessels from aged mice. Microvasc Res 55:260–270
Mosely LH, Finseth F (1977) Cigarette smoking: impairment of digital blood flow and wound healing in the hand. Hand 9(2):97–101
Mosely LH, Finseth F, Goody M (1978) Nicotine and its effect on wound healing. Plast Reconstr Surg 61(4):570–575
Rees TD, Liverett DM, Guy CL (1984) The effect of cigarette smoking on skin-flap survival in the face lift patient. Plast Reconstr Surg 73(6):911–915
Krueger JK, Rohrich RJ (2001) Clearing the smoke: the scientific rationale for tobacco abstention with plastic surgery. Plast Reconstr Surg 108(4):1063–73
Chan LK, Withey S, Butler PE (2006) Smoking and wound healing problems in reduction mammaplasty: is the introduction of urine nicotine testing justified? Ann Plast Surg 56(2):111–115
Manassa EH, Hertl CH, Olbrisch RR (2003) Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plast Reconstr Surg 111(6):2082–2087
Rogliani M, Labardi L, Silvi E, Maggiulli F, Grimaldi M, Cervelli V (2006) Smokers: risks and complications in abdominal dermolipectomy. Aesthetic Plast Surg 30(4):422–424
Pittet B, Montandon D, Pittet D (2005) Infection in breast implants. Lancet Infect Dis 5(2):94–106
WHO MONICA Project (1992) WHO MONICA Manual: Smoking questionnaire. Available at: URL:http://www.ktl.fi/publications/monica/manual/part3/iii-1.htm
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift trade mark technique)—a case series multicentric study. Int Urogynecol J Pelvic Floor Dysfunct 18(7):743–752
Belot F, Collinet P, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2005) Prosthetic reinforcement by the vaginal approach after surgical repair of pelvic prolapse. J Gynecol Obstet Biol Reprod 34(8):763–767
Debodinance P, Berrocal J, Clave H, Cosson M, Garbin O, Jacquetin B et al (2004) Changing attitudes on the surgical treatment of urogenital prolapse: birth of the tension-free vaginal mesh. J Gynecol Obstet Biol Reprod 33(7):577–588
Deffieux X, Huel C, de Tayrac R, Bottero J, Porcher R, Gervaise A et al (2006) Vaginal mesh extrusion after transvaginal repair of cystocele using a prosthetic mesh: treatment and functional outcomes. J Gynecol Obstet Biol Reprod 35(7):678–684
Moher D, Schulz KF, Altman DG (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 357:1191–1194
Theadom A, Cropley M (2006) Effects of preoperative smoking cessation on the incidence and risk of intraoperative and postoperative complications in adult smokers: a systematic review. Tob Control 15(5):352–358
Rees TD, Liverett DM, Guy CL (1984) The effect of cigarette smoking on skin-flap survival in the face lift patient. Plast Reconstr Surg 73(6):911–915
Krueger JK, Rohrich RJ (2001) Clearing the smoke: the scientific rationale for tobacco abstention with plastic surgery. Plast Reconstr Surg 108(4):1063–1073
Chan LK, Withey S, Butler PE (2006) Smoking and wound healing problems in reduction mammaplasty: is the introduction of urine nicotine testing justified? Ann Plast Surg 56(2):111–115
Kryger ZB, Fine NA, Mustoe TA (2004) The outcome of abdominoplasty performed under conscious sedation: six-year experience in 153 consecutive cases. Plast Reconstr Surg 113(6):1807–1817
Spiegelman JI, Levine RH (2006) Abdominoplasty: a comparison of outpatient and inpatient procedures shows that it is a safe and effective procedure for outpatients in an office-based surgery clinic. Plast Reconstr Surg 118(2):517–522
Kaufman T, Eichenlaub EH, Levin M, Hurwitz DJ, Klain M (1984) Tobacco smoking: Impairment of experimental flap survival. Ann Plast Surg 13(6):468–472
Lawrence WT, Murphy RC, Robson MC et al (1984) The detrimental effect of cigarette smoking on flap survival: an experimental study in the rat. Br J Plast Surg 37(2):216–219
Van Adrichem LN, Hoegen R, Hovius SE, Kort WJ, van Strik R, Vuzevski VD et al (1996) The effect of cigarette smoking on the survival of free vascularized and pedicled epigastric flaps in the rat. Plast Reconstr Surg 97(1):86–96
Chang LD, Buncke G, Slezak S, Buncke HJ (1996) Cigarette smoking, plastic surgery, and microsurgery. J Reconstr Microsurg 12(7):467–474
Black CE, Huang N, Neligan PC, Levine RH, Lipa JE, Lintlop S et al (2001) Effect of nicotine on vasoconstrictor and vasodilator responses in human skin vasculature. Am J Physiol Regul Integr Comp Physiol 281(4):R1097–104
Astrup P, Kjeldsen K (1974) Carbon monoxide, smoking, and atherosclerosis. Med Clin North Am 58(2):323–350
Birnstingl MA, Brinson K, Chakrabarti BK (1971) The effect of short-term exposure to carbon monoxide on platelet stickiness. Br J Surg 58(11):837–839
Dintenfass L (1975) Elevation of blood viscosity, aggregation of red cells, haematocrit values and fibrinogen levels with cigarette smokers. Med J Aust 1(20):617–620
Meade TW, Chakrabarti R, Haines AP, North WR, Stirling Y (1979) Characteristics affecting fibrinolytic activity and plasma fibrinogen concentrations. Br Med J 1(6157):153–156
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors did not receive any sources of financial support for the study, including provision of supplies or services from a commercial organization.
Rights and permissions
About this article
Cite this article
Araco, F., Gravante, G., Sorge, R. et al. Risk evaluation of smoking and age on the occurrence of postoperative erosions after transvaginal mesh repair for pelvic organ prolapses. Int Urogynecol J 19, 473–479 (2008). https://doi.org/10.1007/s00192-007-0476-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-007-0476-8