Abstract
Purpose
The aim of our retrospective study was to assess and to compare the surgical complications of hysterectomy regarding the choice of procedure [abdominal (AH), vaginal (VH), and total laparoscopic hysterectomy (TLH)].
Methods
A total of 6,480 patient charts undergone hysterectomy were retrospectively analyzed. Data including transfusion, bladder, ureteral and bowel injury, cuff dehiscence, pulmoner embolus, febrile morbidity, hematoma, reoperation, pelvic wall problems were gathered. The Chi-square test and Student’s t test were used in the statistical analysis.
Results
The most common perioperative complication was blood transfusion which occurred in 114 patients (2.6%). VH patients required significantly less blood transfusion than AH (2.1, 2.6%, respectively). AH had significantly more bladder injury than VH (0.7, 0.4%, respectively). AH had significantly more ureteral injury than VH (0.2, 0.1%, respectively). AH had the same bowel injury as VH (0.1%). AH and VH necessitated significantly more reoperation than TLH (0.4, 0.2, 0.0%, respectively).
Conclusion
To our study, VH ensures less complication rates than AH. In experienced centers, VH can be a reliable alternative to AH. Controlled prospective studies with large patient volumes are required to compare TLH and VH according to complication rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hysterectomy is the most frequent major gynecological operation worldwide. There is still no consensus on the optimum method of hysterectomy [1]. There are lots of randomized studies comparing outcomes of various types of hysterectomies [2–4]. Abdominal hysterectomy (AH), vaginal hysterectomy (VH) or total laparoscopic hysterectomy (TLH) can be chosen contingent on the indication for surgery, uterine size, surgeon’s experience, and patient characteristics and the preference. Abdominal approach is still the choice of procedure at the majority of hysterectomies.
Abdominal and vaginal hysterectomies have been performed for centuries [5]. However, TLH was introduced by Reich [6]. TLH is a reliable and less invasive alternative to especially AH and has better postoperative recovery, reduced need of analgesics and shorter hospital stay [7–11]. VH is associated with shorter operating time and lower costs when compared with TLH [12].
The aim of our retrospective study was to compare the operative data and postoperative outcomes of VH, AH, and TLH at a single center in a given period of time.
Methods
We analyzed the surgical reports and files of all patients’ undergone hysterectomies for benign reasons between January 2001 and December 2009 at the gynecology clinic of Zekai Tahir Burak Women Health Education and Research Hospital, Ankara, Turkey. Patients with malignancy, additional operation beside hysterectomy, autoimmune disease, and coagulation disorders were excluded from the study. The study group consisted of 6,480 cases. The operations were performed by seven consultant gynecologists and their senior residents and fellows. Informed consent for all operations was warranted.
Of the 6,480 procedures, 4,398 (67%) were AH, 1,944 (30%) were VH, and 138 (2.1%) were TLH. In our hospital VH is preferred in patients with pelvic relaxation and no known malignancy. VH has performed about 90 min in our institute. If other interventions such as anterior and posterior colporrhapy have been added to the surgery operation time is extended about 35 min. AH is preferred in patients with large uteruses (>12 weeks of gestation), previous pelvic surgery and malignancy suspicion. TLH is preferred in patients with benign adnexial masses, small uterus and no previous pelvic surgery. In our institute, THL has been performed since 2008. Only two surgeons could perform this kind of surgery because of its learning curve. Surgeons have learned the surgery by performing 20 THL operations in a 6-month period. In TLH surgeries, vaginal vaults have been closed laparoscopically in 91 patients (66%) and by vaginal interference in 47 patients (34%). None of the patient showed vaginal cuff perforation.
We compared the perioperative and early postoperative complications among the hysterectomy groups. Hemoglobin levels, incidence of complications including urinary tract injury (bladder and ureteral injury), bowel injury, and hemorrhage >500 ml were compared in the perioperative period. The reoperation rates among the groups were also assessed. Early postoperative period covered the complications within the first postoperative 7 days. Secondary outcomes as duration of the operations, uterus weight, hospital stay, analgesic need, and perioperative Hb levels were also assessed.
Data were processed via the SPSS software (version 11.0; SPSS Inc, Chicago, IL) statistic program. The Chi-square test and Student’s t test were used for statistical comparison and p < 0.05 was accepted as significant.
Results
Of the 6,480 hysterectomies, the choice of the procedure was AH in 4,398 (67.8%) cases, VH in 1,944 (30%), and TLH in 138 (2.1%). Indications for hysterectomy are shown in Table 1.
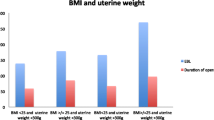
There found to be no significant difference among patients regarding their characteristics those undergone different hysterectomies, however, AH group had higher body mass index (>30) rates than the others (p = 0.04) (Table 2).
The most frequent concomitant procedures included in the VH were anterior colporrhapy (73%) and posterior colporrhapy (68%) (Table 3).
Perioperative major and minor complications of the different hysterectomy methods are shown in Table 4. Perioperative complication rate of the total group was 5.6% (n = 369). The most common intraoperative complication was blood transfusion which necessitated in 156 patients (2.4% of whole group), however 114 patients (2.6%) were in the AH group, 40 patients (2.1%) in the VH group, and 2 patients (1.4%) in the TLH group. VH group patients had less transfusion need comparing AH and TLH groups (p < 0.05).
Bladder injury occurred in 38 patients (0.5% of whole group), including 30 patients (0.7%) in the AH group, 7 patients (0.4%) in the VH group, 1 patient (0.7%) in TLH group. AH group had the same bladder injury rate with TLH.
Ureteral injury occurred in ten patients (0.1% of whole group) and composed of eight patients (0.2%) in the AH group and two patients (0.1%) in the VH group. Ureteral injury was not encountered in TLH group, however, AH group had higher ureteral injury rates than the others (p < 0.05).
Bowel injury occurred in six patients (0.09% of whole group), composed of four patients (0.1%) in the AH group, two patients (0.1%) in the VH group. There was no bowel injury in TLH group.
Of the whole group, 22 patients (0.3%) underwent reoperation and it composed of 18 patients (0.4%) from the AH group, 4 patients (0.2%) from the VH group. The indication for reoperations was intraabdominal bleeding.
Additionally, there were 12 (0.2%) abdomen wall problems, 4 (0.09%) necrotizing fasciitis, 6 (0.1%) hematoma and 2 (0.04%) patients had dehiscence in AH group.
Secondary outcomes regarding operations are shown in Table 5.
There was no mortality in the study group.
Discussion
Hysterectomy is the most frequent gynecologic operation and AH (67.9%) is still the mostly preferred approach for hysterectomy in our hospital. AH rates are reported to be 63% in USA [13] and 80% in Denmark [14]. In our retrospective study, we compared the complication rates of AH, VH and TLH in the selected patient group at the single center where different surgical approaches are applied up to the preference of the surgeon. The purpose of TLH is not to replace VH but rather to avoid the need for AH in endometriosis and adnexial tumors. Sesti et al. [16] reported the VH as the fastest operative technique and favored to be associated with less blood loss when compared with TLH, in their randomized trial. Similar to Sesti’s study, our findings revealed that VH serves less blood loss compared to TLH and AH. VH is the choice of procedure for patients with small uterus, and without other adnexal pathologies and previous surgery, because VH is a cost-effective, time-saving procedure with short recovery period [9, 17]. In our study group, as AH was the choice of the procedure in patients with large uterus volume and/or had previous pelvic surgery, the major complication rates were higher in this group. Notwithstanding, TLH operations need an experience that would settle in time for a center, and for this reason, our group had limited number of cases underwent TLH which also limits our study.
Johnson et al. [9] published a meta-analysis of prospective randomized trials and stated that the rate of urinary complications was higher with laparoscopy. Garry et al. [18] in their randomized prospective trial found higher bladder injury rates in the laparoscopy group, but they noticed that their group had considerable amount of previous caesarean section and endometriosis. These selection biases can affect complication rates. Previous caesarean section has already been shown as a risk factor for VH [19] and AH [20]. In our study, there were no urinary complications in TLH group. To make a proper estimation on the urinary complication rates of hysterectomy types, study groups should be homogeneous regarding aforementioned risk factors.
Donnez et al. [21] favored laparoscopic hysterectomy as having multiple advantages over AH and VH, and with no increase in major complication rates regarding their series of 3,190 laparoscopic hysterectomy cases. Walsh et al. [22] highlighted the laparoscopic approach as offering advantages over the AH for benign diseases particularly with respect to minor perioperative complications, blood loss and hospital stay, however they also noted the need for larger studies to address the major complications and long term outcomes like pelvic organ prolapsus and bladder dysfunction. Young et al. [15] reviewed 39 papers and found that the outcome of TLH was not better than AH. Our series suggests better outcomes for TLH and VH than AH. These two approaches are less invasive than AH, however, they cannot replace AH in all circumstances.
Conclusion
Regarding our study, there is no clear evidence on the superiority of the hysterectomy methods one to another. However, VH seems to be advantageous over other methods in the centers with sufficient surgical experience. Prospective randomized trials including large number of patients are required to make clear definitions on the optimum surgical approach for hysterectomy.
References
Garry R (2005) The future of hysterectomy. BJOG 112(2):133–139
McCracken G, Hunter D, Morgan D, Price JH (2006) Comparison of laparoscopic-assisted vaginal hysterectomy, total abdominal hysterectomy and vaginal hysterectomy. Ulster Med J 75(1):54–58
Hwang JL, Seow KM, Tsai YL, Huang LW, Hsieh BC, Lee C (2002) Comparative study of vaginal, laparoscopically assisted vaginal and abdominal hysterectomies for uterine myoma larger then 6 cm in diameter or uterus weighting at least 450 g: a prospective randomized study. Acta Obstet Gynecol Scand 81(12):1132–1138
Ottosen C, Lingman A, Ottosen L (2000) Three methods for hysterectomy: a randomized, prospective study of short term outcome. BJOG 107(11):1380–1385
Sutton C (1997) Hysterectomy: a historical perspective. Baillieres Clin Obstet Gynaecol 11(1):1–22
Reich H (1989) New techniques in advanced laparoscopic surgery. Baillieres Clin Obstet Gynaecol 3(3):655–681
Gyr T, Ghezzi F, Arslanagic S, Leidi L, Pastorelli G, Franchi M (2001) Minimal invasive laparoscopic hysterectomy with ultrasonic scalpel. Am J Surg 181(6):516–519
Makinen J, Johansson J, Tomas C, Tomas E, Heinonen PK, Laatikainen T et al (2001) Morbidity of 10 110 hysterectomies by type of approach. Hum Reprod 16(7):1473–1478
Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R (2005) Methods of hysterectomy: systematic review and meta-analysis of randomised controlled trials. BMJ 330(7506):1478
HoVman CP, Kennedy J, Borschel L, Burchette R, Kidd A (2005) Laparoscopic hysterectomy: the Kaiser Permanente San Diego experience. J Minim Invasive Gynecol 12(1):16–24
Schindlbeck C, Klauser K, Dian D, Janni W, Friese K (2008) Comparison of total laparoscopic, vaginal and abdominal hysterectomy. Arch Gynecol Obstet 277(4):331–337
Soriano D, Goldstein A, Lecuru F, Daraï E (2001) Recovery from vaginal hysterectomy compared with laparoscopic-assisted vaginal hysterectomy: a prospective, randomized, multicenter study. Acta Obstet Gynecol Scand 80(4):337–341
Farquhar CM, Steiner CA (2002) Hysterectomy rates in the United States 1990–1997. Obstet Gynecol 99(2):229–234
Gimbel H, Settnes A, Tabor A (2001) Hysterectomy on benign indication in Denmark 1988–1998. A register based trend analysis. Acta Obstet Gynecol Scand 80(3):267–272
Young W, Cohen MM (1997) Laparoscopically assisted vaginal hysterectomy. A review of current issues. Int J Technol Assess Health Care 13(2):368–379
Sesti F, Calonzi F, Ruggeri V, Pietropolli A, Piccione E (2008) A comparison of vaginal, laparoscopic-assisted vaginal, and minilaparotomy hysterectomies for enlarged myomatous uteri. Int J Gynaecol Obstet 103(3):227–231
Silva-Filho AL, Werneck RA, de Magalhaes RS, Belo AV, Triginelli SA (2006) Abdominal vs vaginal hysterectomy: a comparative study of the postoperative quality of life and satisfaction. Arch Gynecol Obstet 74(1):21–24
Garry R, Fountain J, Mason S, Hawe J, Napp V, Abbott J, Clayton R, Phillips G, Whittaker M, Lilford R et al (2004) The evaluate study: two parallel randomised trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ 328:129
Boukerrou M, Lambaudie E, Collinet P, Crepin G, Cosson M (2004) Previous caesarean section is an operative risk factor in vaginal hysterectomy. Gynecol Obstet Fertil 32(6):490–495
Carley ME, McIntire D, Carley JM, Schaffer J (2002) Incidence, risk factors and morbidity of unintended bladder or ureter injury during hysterectomy. Int Urogynecol J Pelvic Floor Dysfunct 13(1):18–21
Donnez O, Jadoul P, Squifflet J, Donnez J (2009) A series of 3190 laparoscopic hysterectomies for benign disease from 1990 to 2006: evaluation of complications compared with vaginal and abdominal procedures. BJOG 116(4):492–500
Walsh CA, Walsh SR, Tang TY, Slack M (2009) Total abdominal hysterectomy versus total laparoscopic hysterectomy for benign disease: a meta-analysis. Eur J Obstet Gynecol Reprod Biol 144(1):3–7
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doğanay, M., Yildiz, Y., Tonguc, E. et al. Abdominal, vaginal and total laparoscopic hysterectomy: perioperative morbidity. Arch Gynecol Obstet 284, 385–389 (2011). https://doi.org/10.1007/s00404-010-1678-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-010-1678-8