Abstract
This study aimed to evaluate the effect of surgical risk factors, including type of surgery, body mass index, uterine size and presence of adhesions, on perioperative outcomes and complication rates in laparoscopic hysterectomy (LH). This was a retrospective cohort study of 264 LH cases performed between 2005 and 2013 at a London University Hospital. One hundred sixty six (62.9 %) underwent laparoscopic subtotal hysterectomy (LASH) and 98 (37.1 %) total laparoscopic hysterectomy (TLH). Mean operation duration was 77 (±35) min and mean estimated blood loss (EBL) was 196 (±128) ml. Mean specimen weight was 323 g (range 46–1765 g). There were no conversions to laparotomy. Patients undergoing LASH were older than TLH patients (46.7 vs 42.8 years, p < 0.0001) and with larger uterine size (16.9 vs 11.0 weeks, p < 0.0001). There were no differences in operation duration, EBL or hospital stay. Bladder injury occurred in 3 LASH cases (1.8 %) and no TLH cases. Presence of adhesions increased operative duration (95.2 vs 71.5 min, p < 0.0001). Preoperative uterine size correlated positively with specimen weight (p < 0.001), operation duration (p < 0.001) and EBL (p < 0.001). There was a linear relationship between BMI and EBL and operation duration (EBL r 2 0.028, p = 0.006; operative duration r 2 0.017, p = 0.038). This study shows that overall, LH is a safe procedure with low risk of major complications, even in patients with significant surgical risk factors. This study has highlighted particular groups which might be at increased surgical risk, particularly those with a combination of elevated BMI and large uterus, which can aid preoperative counselling.
Similar content being viewed by others
Introduction
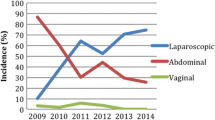
Despite a decline in hysterectomy rates over the past two decades, it remains the most frequently performed major gynaecological procedure [1, 2]. Laparoscopic hysterectomy (LH) was first described by Reich in 1989 [3] and developed as a minimally invasive alternative to the open abdominal or vaginal approach. The advantages of laparoscopic over open gynaecological surgery are well documented, including reduced postoperative pain, fewer surgical site infections, shorter hospital stay, quicker return to normal activity, a smaller fall in haemoglobin and a lower incidence of postoperative adhesions [4]. Despite these numerous benefits, LH has not replaced abdominal hysterectomy to the extent that may have been anticipated in the years after its advent and around 50 % of hysterectomies are still carried out abdominally [5]. Perceptions (not necessarily supported by available clinical data) surrounding traditionally high-risk surgical candidates (e.g. elevated body mass index (BMI), prior laparotomy or enlarged uteri) or lack of surgical expertise may have contributed to this. However, due to the many advantages of minimally invasive surgery, position statements continue to encourage the replacement of abdominal hysterectomy with minimally invasive options where possible [6].
Although rates of LH are increasing [5], controversy still exists surrounding the complication rates and the relative advantages and disadvantages of total laparoscopic hysterectomy (TLH) vs laparoscopic subtotal hysterectomy (LASH). Current recommendations regarding route of hysterectomy [4, 6] have acknowledged the lack of LH outcome data and suggested specifically that the different subcategories of LH warranted further evaluation.
The aim of this study was to evaluate the effect of different surgical risk factors, including type of surgery, body mass index, uterine size and presence of adhesions, on perioperative outcomes and complication rates in LH.
Methods
This was a retrospective cohort study involving data from patients who underwent laparoscopic hysterectomy in the laparoscopic surgical unit of a London University hospital between January 2005 and December 2013. The data were gathered as part of an ongoing database designed to evaluate clinical practice in the unit. Data were collected prospectively in a Microsoft Excel™ spreadsheet and with institutional approval from the hospital research and development department. The study was conducted in accordance with Caldicott guidance and Declaration of Helsinki standards. Formal ethical approval was not necessary as there was no deviation from normal clinical practice, and as the study was retrospective, formal consent was not required.
Preoperative assessment occurred at the initial consultation visit where baseline characteristics, presenting symptoms and medical and surgical history were recorded. Data collected included age, parity, BMI, prior abdominal surgery, uterine size and primary symptom or indication for surgery. Uterine size was assessed clinically on pelvic examination and equated to number of weeks of gestation. All patients underwent preoperative imaging in the form of pelvic ultrasound (US) or magnetic resonance imaging (MRI) and, where appropriate, endometrial sampling to assess for underlying pathology.
Exclusion criteria for LH included confirmed or suspected malignancy of any part of the genital tract and second- or third-degree uterine prolapse. There was no upper limit of uterine size as an exclusion criterion, and patients with endometriosis, pelvic inflammatory disease, previous abdominal surgery or obesity were not excluded.
Operative data recorded included duration of surgery, estimated blood loss, specimen weight, need for transfusion and length of hospital stay. Major perioperative complications were recorded including urinary tract or intestinal injuries, need for transfusion and incidence of reoperation. Adhesions were classified as flimsy or dense. For the analysis, complications were classified according to the Dindo Scale [7]. Operating time was defined as the duration from incision to wound closure. All laparoscopic hysterectomies were performed by the same surgeon (FO).
Laparoscopic hysterectomies were of two types, LASH or TLH, with or without removal of the ovaries. The technique for LH has been described previously [8, 9]. For large uteri, the surgery could be performed laparoscopically if it was technically possible to proceed with a modified five-port technique [8]. This technique requires adequate space to insert the primary port at Palmer’s point, an ancillary port in the contralateral abdominal fossa and a uterus sufficiently mobile to visualise the pedicles. Our technique for vault closure involves the use of Polysorb™ number 1 intracorporeal figure 8 sutures at each angle, incorporating the uterosacral component of the pericervical ring. Patients were reviewed 3 months postoperatively in the gynaecology outpatient clinic.
Statistical analysis
Statistical analysis was performed using SPSS Statistics Version 21.0. Data are presented as mean ± standard deviation (SD) or as a percentage. The normality of the distribution of the data was determined using the Kolmogorov–Smirnov test and normality plots (boxplots). Fisher’s exact test was used for categorical data, and the Student’s t test or Mann–Whitney U test was used for continuous data as appropriate. Analysis of variance (ANOVA) was used to compare means for continuous variables with multiple groups. Interdependencies between variables were explored using Spearman’s linear correlation analysis and linear and multivariate regression analysis. p values less than 0.05 were considered to be statistically significant.
Findings
During the study period, 264 LH cases were performed. Baseline characteristics of all cases can be seen in Table 1. Mean age was 45.3 (±5.2) years and mean BMI 30.2 (±6.3) kg/m2, which falls within the obese category as per WHO classification. Dysfunctional bleeding and heavy menstrual bleeding were the most common primary symptoms occurring in 90 % of women. Fifteen percent of patients had a prior laparotomy. All surgeries were performed for benign indications and histopathology confirmed no cases of endometrial carcinoma. The majority of women had fibroids resulting in significantly enlarged mean uterine size of 14.7 weeks (range 6–32 weeks).
All cases were completed laparoscopically with no conversions to laparotomy required. Thirty-five percent of patients also underwent oophorectomy. Mean operation duration was 77 (±35) min and mean estimated blood loss was 196 (±128) ml. Mean specimen weight was 323 g with a range of 46–1765 g.
Major complications were three (1.1 %) bladder injuries, all recognised at the time of surgery; one (0.4 %) injury to the inferior epigastric artery, one (0.4 %) secondary haemorrhage requiring blood transfusion and return to theatre and one (0.4 %) haematoma formation. There were no bowel or ureteric injuries and no estimated blood loss greater than 1000 ml. Mean length of hospital stay was 1.78 days.
Effect of type of surgery
Of the patients who underwent LH, 166 (62.9 %) were LASH and 98 (37.1 %) were TLH. Seventy four (28 %) also underwent BSO and 19 (7.2 %) USO, with the remaining 171 (64.8 %) having ovarian conservation.
Patients who had ovarian conservation were younger than those who also underwent BSO (44.5 ± 5.2 vs 46.9 ± 5.5 years, p = 0.002), but there was no significant difference in estimated blood loss (p = 0.669) or operative duration (p = 0.853).
Patients undergoing LASH were significantly older than TLH patients (46.7 ± 4.2 vs 42.8 ± 5.9 years, p < 0.0001) and had a larger preoperative estimated uterine size (16.9 ± 6.3 vs 11.0 ± 3.5 weeks, p < 0.0001). There were no differences in operation duration, estimated blood loss or hospital stay (see Table 1), and multivariate analysis did not identify type of LH as an independent predictor of blood loss, hospital stay or complications.
Short-term complications can be seen in Table 2. All cases were completed laparoscopically. Bladder injury occurred in three cases, all LASH. There was one return to theatre due to secondary haemorrhage in the TLH group (0.4 %) in the same patient that required a blood transfusion. Bleeding was found coming from the infundibulopelvic ligament and was managed laparoscopically.
Patients were reviewed 3 months postoperatively There were no cases of vaginal vault dehiscence in the TLH group. Two patients in the LASH group required cautery for vaginal bleeding and were subsequently discharged. One further patient in the LASH group required reoperation at 6 months for recurrent bleeding. The patient had a normal-sized uterus, and the sole indication for surgery was menorrhagia without dysmenorrhea. She returned at 3 months postoperatively with pelvic pain, which was managed conservatively and irregular bleeding, for which a laparoscopic trachelectomy was performed at 6 months. Of note, histopathology confirmed no adenomyosis in either the original uterine specimen or the cervical specimen.
Effect of adhesions
Sixty-two patients (23.5 %) had either dense adhesions, prior laparotomies or significant endometriosis (stage 3 or 4). The presence of any of these risk factors resulted in increased operative duration (95.2 vs 71.5 min, p < 0.0001) and a trend towards increased blood loss but which did not reach statistical significance (222.6 vs 187.2 ml, p = 0.056). This did not affect the length of hospital stay (p = 0.512) (Table 3). Multivariate regressions analysis showed that the presence of adhesions or prior surgery was an independent predictor of blood loss (p = 0.02) and operative duration (p < 0.001).
Of the three bladder injuries, two occurred in patients with no risk factors for adhesions and one occurred in a patient who had had two previous caesarean sections.
Effect of uterine size
Overall, this population had enlarged uterine size due to the high prevalence of fibroids. The largest estimated uterine size preoperatively was 32 weeks and specimen weight ranged from 46 to 1765 g.
The association of specimen weight and outcomes can be seen in Table 4. A greater specimen weight was associated with increased blood loss and length of operation but not hospital stay. Preoperative estimated uterine size correlated positively with specimen weight (r 2 0.766, sig <0.001), operation duration (r 2 0.211, sig <0.001) and estimated blood loss (r 2 0.101, sig <0.001). Specimen weight was confirmed to be an independent predictor for blood loss and operation length on multivariate analysis.
Effect of BMI
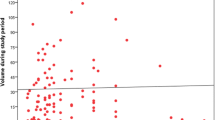
Analysis of the effect of BMI on estimated blood loss and operation duration showed a linear relationship (estimated blood loss (EBL) r 2 0.028, p = 0.006; operative duration r 2 0.017, p = 0.038). ANOVA comparison between BMI categories showed a significant increasing EBL with increasing BMI (Table 5). Operative duration was on average 16.2 min longer in the highest BMI category, and multivariate analysis showed that BMI was an independent predictor of blood loss and operation duration. BMI did not appear to affect the length of hospital stay.
In subgroup analysis, ANOVA comparison between BMI categories showed that the relationship between BMI and EBL only remained statistically significant in the TLH group (p = 0.025), but not the LASH group (p = 0.21). This is likely due the confounding factor of uterine size, as multivariate analysis demonstrated specimen weight was a stronger predictor of EBL than BMI.
Of note, the three bladder injuries occurred in women of BMI 18, 24 and 25, two of them had cervical fibroids obscuring the view of the cervix and the other had two previous lower caesarean sections with the bladder adherent to the mid portion of the uterus. The complication of inferior epigastric injury was in a patient with a BMI of 40 kg/m2 and a 14-week-sized uterus. Because of the adiposity, it was difficult to visualise the inferior epigastrics, and despite going more than 6 cm from the midline, bleeding was noticed on removal of a 5-mm ancillary port.
The combined effect of high BMI and a large uterus on blood loss and operation duration can be seen in Fig. 1 and Table 6. In patients who had an elevated BMI of ≥25 kg/m2 and uterine weight ≥300 g, there was a 94 % increase in blood loss and 66 % increase in operation duration compared to those with normal weight (BMI < 25 kg/m2) and uterine size less than 300 g.
Discussion
Controversy still exists surrounding the optimum route of hysterectomy in terms of patient safety and cost-effectiveness [10]. Current guidance suggests that the vaginal route is preferred to the laparoscopic route; however, LH allows a minimal-access route in situations where VH may not be possible, including enlarged uteri, lack of vaginal access or minimal uterine descent, immobile uterus, adnexal pathology and pelvic adhesions due to previous surgeries or endometriosis.
Meta-analyses into the route of hysterectomy have highlighted a lack of outcome data between the different types of LH [4]. Additionally, in women who opt for hysterectomy, controversy remains about whether or not the cervix should be removed. Concerns about retaining the cervix include the risk of cyclical bleeding or pain, cervical cancer and effect on sexual function. Much evidence about the effect of cervical removal is extrapolated from other surgical routes, and there is limited data assessing the laparoscopic route [11]. A recent cohort study has suggested that LASH may provide benefit in terms of sexual function compared to TLH [12], although further randomised data is needed. There are also RCT data that show no difference between TLH and LASH at 1 year postoperatively in terms of quality of life and patient satisfaction [13].
The current study compared perioperative outcomes between TLH and LASH. Despite differences in population demographics (LASH patients were significantly older, with higher BMI and larger uterine size), we observed no significant difference in blood loss or operation duration. These findings are in contrast to previous studies which associate LASH with reduced operation duration compared to TLH [14–17]. These contrasting results may be explained by the enlarged mean uterine size of LASH patients in the present study, as the enlarged uterus requires a longer time period for morcellation and specimen removal, thereby increasing the operation duration to that similar to TLH.
Unfortunately, randomised data comparing LASH and TLH is limited. In a small study of 141 patients randomised to TLH or LASH, there were no differences in complication rates or outcomes over 2 years of follow-up, other than women undergoing LASH had increased risk of hospital readmission [18]. Several previous cohort studies have compared TLH and LASH with conflicting results. A recent multicentre retrospective study in 390 women undergoing LH suggested that TLH was associated with more short-term complications such as urinary tract lesions, higher blood loss and infection, whereas LASH was associated with increased long-term problems such as dyspareunia and vaginal bleeding [19]. This increased risk of complications with TLH has also been observed in a prospective study by Wallwiener et al. [17] of 1952 women who underwent either TLH or LASH. They reported that TLH was associated with increased risk of conversion to laparotomy (6.5 % ct. 2.6 %), greater haemoglobin drop and longer hospital stay, but with no increased rates of intraoperative complications [17]. Other observational studies did not observe differences in complication rates [20, 21] or blood loss [16, 19, 20] between TLH and LASH.
In the present study, the rate of urinary tract injury appeared to be higher in LASH than TLH, although the small numbers preclude any definitive conclusions. Selection bias may have contributed to these results given that women in whom hysterectomy may be anticipated to be difficult, such as enlarged uteri or prior surgery (which also act as risk factors for bladder injury), are more likely to undergo LASH. Previous observational studies have reported urinary tract injuries occurring solely in TLH cases [15, 16], and so further large-scale randomised data are needed. None of the risk factors analysed independently predicted length of hospital stay or the risk of complications.
Effect of adhesions
Adhesions can pose a significant challenge in laparoscopic surgery as they can affect access and visualisation of the surgical field and cause anatomical distortion. In the present study, in the absence of an internationally agreed classification of adhesions, adhesions were documented as dense or flimsy. The dense adhesions are those where extra time and expertise would be required to lyse the adhesions in view of the vascularity within the adhesions and the degree of attachment between adjacent organs. Our data suggest that a history of prior laparotomy or caesarean section, dense adhesions or stage 3/4 endometriosis may be associated with increased surgical risk. Similar findings have been observed in earlier observational studies. In a retrospective analysis of complication rates in 1253 TLHs, Kobayashi et al. [22] report that a history of abdominal surgery was the only risk factor associated with the occurrence of major complications (OR 2.48, 95 % CI 1.23–6.49). In a series of 1501 LH cases, a history of CS (OR 4.33, 95 % CI 1.53–12.30) and previous laparotomy (OR 4.69, 95 % CI 1.59–13.8) were associated with higher risk of bladder injury [23]. Other studies have been more reassuring regarding the risks of LH in the presence of prior laparotomy [24, 25], and current guidance states that prior caesarean section should not be considered a contraindication to LH [6].
Effect of uterine size
Management of a large uterus is perhaps one of the key challenges of minimally invasive routes of hysterectomy and why many procedures are still carried out abdominally. We observed that uterine size had a significant effect on operative duration and blood loss, findings which have also been observed in other cohort studies [16, 26–28]. Despite this, the study highlights the feasibility of LH, even in the presence of large uteri, as complication rates were low and all cases were completed laparoscopically. Other authors have also reported the practicability of LH for large uteri with low overall complication rates [14, 29, 30].
Effect of BMI
Obese patients have potentially much to gain from laparoscopic over open surgery; however, the data on perioperative risks associated with LH in the obese patient have shown conflicting results. LH in patients with elevated BMI has been associated with increased blood loss [31–34], operative duration [32–34], risk of conversion to laparotomy [31] and overall complication rates [33–35]. In contrast, other studies reported that perioperative complications do not increase in cases with obesity [36], provided that the operating technique is meticulous [37].
Low BMI may have played a role in the aetiology of the bladder injuries in the present study. As reported, the three bladder injuries occurred in women with low to normal BMIs. These women also had significantly enlarged uteri of at least 20 weeks in size. We feel that the combination of low BMI and enlarged uteri may act as a risk factor for bladder injury as it restricts vision and access to the lower anterior part of the uterus; however, further large studies are required to confirm these findings.
Study limitations
The limitations of the present study include the lack of randomisation. Concerns have been raised regarding the lack of RCT data investigating LH outcomes [38]; however, in the absence of this data, it is important that units continue to monitor and report complication rates via other methods. Observational studies may be subject to inherent biases; of particular note in our population were the large mean uterine size and high BMI—both of which appear to affect higher surgical risk. Furthermore, the larger mean uterine size in LASH compared to that in TLH is most likely attributable to selection bias given the technical difficulties associated with TLH on particularly large uteri. Observational bias likely contributed to the finding of younger age in the TLH group. Younger patients were more likely to present with pain as well as menorrhagia and had a higher prevalence of endometriosis. In this group of patients, total laparoscopic hysterectomy was preferred to subtotal laparoscopic hysterectomy.
Although observational, this study hopefully provides useful clinical data in a more ‘real-world’, albeit high-risk, population. Although RCTs are considered the gold standard, they have inherent difficulties and it is difficult to control for variation in operator experience and surgical volume, which are known to significantly affect perioperative outcomes [16, 39]. This study has the advantage that all cases were operated on by one surgeon, thereby reducing differences due to surgical technique and operator experience.
This study has shown that overall, laparoscopic hysterectomy is a safe procedure with low risk of major complications, even in patients with significant surgical risk factors, and adds to the limited data available on the practicability of LH for large uteri. Continued improvements in instrumentation, energy sources, haemostatic agents and vaginal cuff closure techniques have expanded the use of LH with reducing complication rates [40]. This study has highlighted particular groups which might be at increased surgical risk, particularly those with a combination of elevated BMI and large uterus, and this should be taken into consideration when counselling patients preoperatively.
References
Reid PC, Mukri F (2005) Trends in number of hysterectomies performed in England for menorrhagia: examination of health episode statistics, 1989 to 2002–3. BMJ 330:938–9
Mukhopadhaya N, Manyonda IT (2013) The hysterectomy story in the United Kingdom. J Midlife Health 4:40–1
Reich H, Decaprio J, McGlynn F (1989) Laparoscopic hysterectomy. J Gynecol Surg 5:213–216
Nieboer TE, Johnson N, Lethaby A, Tavebder E, Curr E, Garry R, van Voorst S, Mol BW, Kluivers KB (2009) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 3, CD003677. doi:10.1002/14651858.CD003677.pub4
Wright JD, Ananth CV, Lewin SN, Burke WM, Lu YS, Neugut AI, Herzog TJ, Hershman DL (2013) Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA 309:689–698
Practice Report AAGL (2011) Route of hysterectomy to treat benign uterine disease. J Minim Invasive Gynecol 18:1–3
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Shahid A, Sankaran S, Odejinmi F (2011) Laparoscopic subtotal hysterectomy for large uteri using modified five port technique. Arch Gynecol Obstet 283:79–81
Hussain M, Odejinmi F (2012) Laparoscopic supracervical hysterectomy: impact of body mass index and uterine weight. Gynecol Surg 9:351–355
Drahonovsky J, Haakova L, Otcenasek M, Krofta L, Kucera E, Feyereisl J (2010) A prospective randomized comparison of vaginal hysterectomy, laparoscopically assisted vaginal hysterectomy, and total laparoscopic hysterectomy in women with benign uterine disease. Eur J Obstet Gynecol Reprod Biol 148:172–6
Practice Report AAGL (2014) Practice guidelines for laparoscopic subtotal/supracervical hysterectomy (LSH). J Minim Invasive Gynecol 21:9–16
Brucker SY, Taran FA, Bogdanyova S, Ebersoll S, Wallwiener CW, Schönfisch B, Krämer B, Abele H, Neis F, Sohn C, Gawlik S, Wallwiener D, Wallwiener M (2014) Patient-reported quality-of-life and sexual-function outcomes after laparoscopic supracervical hysterectomy (LSH) versus total laparoscopic hysterectomy (TLH): a prospective, questionnaire-based follow-up study in 915 patients. Arch Gynecol Obstet 290:1141–9
Berner E, Qvigstad E, Myrvold AK, Lieng M (2015) Pain reduction after total laparoscopic hysterectomy and laparoscopic supracervical hysterectomy among women with dysmenorrhea: a randomised controlled trial. BJOG. doi:10.1111/1471-0528.13362
Alperin M, Kivnick S, Poon KY (2012) Outpatient laparoscopic hysterectomy for large uteri. J Minim Invasive Gynecol 19:689–94
Cipullo L, De Paoli S, Fasolino L, Fasolino A (2009) Laparoscopic supracervical hysterectomy compared to total hysterectomy. JSLS 13:370–5
Twijnstra AR, Blikkendaal MD, van Zwet EW, van Kesteren PJ, de Froon CD, Jansen FW (2012) Predictors of successful surgical outcome in laparoscopic hysterectomy. Obstet Gynecol 119:700–8
Wallwiener M, Taran FA, Rothmund R, Kasperkowiak A, Auwärter G, Ganz A, Kraemer B, Abele H, Schönfisch B, Isaacson KB, Brucker SY (2013) Laparoscopic supracervical hysterectomy (LSH) versus total laparoscopic hysterectomy (TLH): an implementation study in 1,952 patients with an analysis of risk factors for conversion to laparotomy and complications, and of procedure-specific re-operations. Arch Gynecol Obstet 288:1329–39
Morelli M, Noia R, Chiodo D, Mocciaro R, Costantino A, Caruso MT, Cosco C, Lucia E, Curcio B, Gullì G, Amendola G, Zullo F (2007) Laparoscopic supra-cervical hysterectomy versus laparoscopic total hysterectomy: a prospective randomized study. Minerva Ginecol 59:1–10
Van Evert JS, Smeenk JM, Dijkhuizen FP, de Kruif JH, Kluivers KB (2010) Laparoscopic subtotal hysterectomy versus laparoscopic total hysterectomy: a decade of experience. Gynecol Surg 7:9–12
Boosz A, Lermann J, Mehlhorn G, Loehberg C, Renner SP, Thiel FC, Schrauder M, Beckmann MW, Mueller A (2011) Comparison of re-operation rates and complication rates after total laparoscopic hysterectomy (TLH) and laparoscopy-assisted supracervical hysterectomy (LASH). Eur J Obstet Gynecol Reprod Biol 158(2):269–73
Mueller A, Renner SP, Haeberie L, Lermann J, Oppelt P, Beckmann MW, Thiel F (2009) Comparison of total laparoscopic hysterectomy (TLH) and laparoscopy-assisted supracervical hysterectomy (LASH) in women with uterine leiomyoma. Eur J Obstet Gynecol Reprod Biol 144(1):76–9
Kobayashi E, Nagase T, Fujiwara K, Hada T, Ota Y, Takaki Y, Kanao H, Andou M (2012) Total laparoscopic hysterectomy in 1253 patients using an early ureteral identification technique. J Obstet Gynaecol Res 38:1194–200
Lafay Pillet MC, Leonard F, Chopin N, Malaret JM, Borghese B, Foulot H, Fotso A, Chapron C (2009) Incidence and risk factors of bladder injuries during laparoscopic hysterectomy indicated for benign uterine pathologies: a 14.5 years experience in a continuous series of 1501 procedures. Hum Reprod 24:842–9
Sinha R, Sundaram M, Lakhotia S, Hedge A, Kadam P (2010) Total laparoscopic hysterectomy in women with previous cesarean sections. J Minim Invasive Gynecol 17:513–517
Wang L, Merkur H, Hardas G, Soo S, Lujic S (2010) Laparoscopic hysterectomy in the presence of previous caesarean section: a review of one hundred forty-one cases in the Sydney West Advanced Pelvic Surgery Unit. J Minim Invasive Gynecol 17:186–191
Bonilla DJ, Mains L, Whitaker R, Crawford B, Finan M, Magnus MJ (2007) Uterine weight as a predictor of morbidity after a benign abdominal and total laparoscopic hysterectomy. Reprod Med 52:490–498
O’Hanlan KA, McCutcheon SP, McCutcheon JG (2011) Laparoscopic hysterectomy: impact of uterine size. J Minim Invasive Gynecol 18(1):85–91
Uccella S, Cromi A, Bogani G, Casarin J, Formenti G, Ghezzi F (2013) Systematic implementation of laparoscopic hysterectomy independent of uterus size: clinical effect. J Minim Invasive Gynecol 20:505–16
Yavuzcan A, Cağlar M, Ustün Y, Dilbaz S, Kumru S (2014) Evaluation of the outcomes of laparoscopic hysterectomy for normal and enlarged uterus (>280 g). Arch Gynecol Obstet 289:831–7
Uccella S, Cromi A, Serati M, Casarin J, Sturla D, Ghezzi F (2014) Laparoscopic hysterectomy in case of uteri weighing ≥1 kg: a series of 71 cases and review of the literature. J Minim Invasive Gynecol 21:460–5
Harmanli O, Esin S, Knee A, Jones K, Ayaz R, Tunitsky E (2013) Effect of obesity on perioperative outcomes of laparoscopic hysterectomy. J Reprod Med 58:497–503
Bardens D, Solomayer E, Baum S, Radosa J, Gräber S, Rody A, Juhasz-Böss I (2014) The impact of the body mass index (BMI) on laparoscopic hysterectomy for benign disease. Arch Gynecol Obstet 289:803–7
Siedhoff MT, Carey ET, Findley AD, Riggins LE, Garrett JM, Steege JF (2012) Effect of extreme obesity on outcomes in laparoscopic hysterectomy. J Minim Invasive Gynecol 19:701–7
Morgan-Ortiz F, Soto-Pineda JM, López-Zepeda MA, Peraza-Garay Fde J (2013) Effect of body mass index on clinical outcomes of patients undergoing total laparoscopic hysterectomy. Int J Gynaecol Obstet 120:61–4
McMahon MD, Scott DM, Saks E, Tower A, Raker CA, Matteson KA (2014) Impact of obesity on outcomes of hysterectomy. J Minim Invasive Gynecol 21:259–65
Kondo W, Bourdel N, Marengo F, Botchorishvili R, Pouly JL, Jardon K, Rabischong B, Mage G, Canis M (2012) What’s the impact of the obesity on the safety of laparoscopic hysterectomy techniques? J Laparoendosc Adv Surg Tech A 22:949–53
Chopin N, Malaret JM, Lafay-Pillet MC, Fotso A, Foulot H, Chapron C (2009) Total laparoscopic hysterectomy for benign uterine pathologies: obesity does not increase the risk of complications. Hum Reprod 24:3057–62
Ghandi S (2009) Have the safety concerns about laparoscopic hysterectomy been fully addressed? BJOG 116:1272
Wallenstein MR, Ananth CV, Kim JH, Burke WM, Hershman DL, Lewin SN, Neugut AI, Lu YS, Herzog TJ, Wright JD (2012) Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol 119:709–716
Ridgeway B, Falcone T (2014) Innovations in minimally invasive hysterectomy. Clin Obstet Gynecol 57:83–94
Authors’ contribution
K Maclaran conducted the data analysis and wrote the manuscript. F Odejinmi developed the project, performed data collection and management and wrote/edited the manuscript. N Agarwal developed the project, collected and managed the data and wrote/edited the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Statement of human rights
All procedures performed were in accordance with the ethical standards of the institution and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
For this type of retrospective study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Maclaran, K., Agarwal, N. & Odejinmi, F. Perioperative outcomes in laparoscopic hysterectomy: identifying surgical risk factors. Gynecol Surg 13, 75–82 (2016). https://doi.org/10.1007/s10397-015-0914-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10397-015-0914-4