Abstract
Purpose
The purpose of this study was to evaluate the short-term efficacy and complication rates of posterior intravaginal slingplasty (IVS) procedures.
Methods
Thirty-four patients who had advanced (grade 4) uterine prolapse were recruited. All patients underwent vaginal hysterectomy and the cuff was suspended with a posterior IVS operation. The mean follow-up duration was 12 months (range 3–20 months).
Results
Thirty-three patients (97.1%) had satisfactory level I support defined objectively as stage 0 or I for point C as described in the pelvic organ prolapse quantification system. There were no rectal, vesical, ureteric, or vascular injuries in this series. During the postoperative period no complications, including tape erosion, were seen.
Conclusions
Posterior IVS is a minimally invasive procedure for grade 4 genital prolapse with a high success rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is estimated that the lifetime risk of surgery for pelvic organ prolapse (POP) in women is 11% [1]. Since it is an age-related disease, the prevalence of POP is expected to further increase with the aging of the population [2]. The quality of life in women is negatively affected by POP [3]. Manual assistance to urinate, urge incontinence, frequency and urgency in urination as well as sex, and bowel function-related symptoms are frequently seen in these women [4–6].
For reconstructive pelvic surgery to correct POP, there are two primary surgical access routes: (1) the abdominal approach by laparotomy or laparoscopy [7, 8] and (2) the vaginal approach [9, 10]. However, among the commonly utilized abdominal and vaginal routes, the best approach for restoration of vaginal apical support remains controversial.
For the repair of vaginal vault prolapse, Petros described for the first time the technique called posterior intravaginal slingplasty (IVS) or infracoccygeal sacropexy [11]. It is a minimally invasive procedure [12] providing anatomic repair of vaginal vault prolapse using a permanent mesh with the benefits of the transvaginal approach. The multifilament polypropylene tape used in this technique reinforces the cardinal–uterosacral ligament complex to suspend the vaginal vault in a tension-free manner [13].
Since there are few studies related to the short-term efficacy and complication rates of the posterior IVS procedure, we aimed to report our experience with this technique over a 1.5-year period with emphasis on these points.
Patients and methods
Patients suffering from advanced (grade 4) uterine prolapse, who were treated in our clinic with vaginal hysterectomy and subsequent posterior IVS operations from September 2006 to May 2008 were recruited. The study was approved by the local ethics committee and only those women who gave written consent were included in the study.
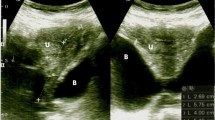
The patients were diagnosed clinically according to the International Continence Society (ICS) pelvic organ prolapse quantification (POPQ) staging system [14]. A direct history was obtained from all patients and a preoperative evaluation including a physical examination, postvoid residual measurement, and urodynamics with the prolapse reduced was performed in every patient.
After the preoperative assessment, all of the patients underwent vaginal hysterectomy and the cuff was suspended via posterior IVS operation as described by Petros [13]. The women who had urodynamically proven stress urinary incontinence also underwent a transobturator tape (TOT) procedure, concomitantly. In brief, the posterior IVS procedure was performed by making a vertical incision with a scalpel in the posterior vaginal wall just below the vault, leaving at least a 2-cm strip of vaginal epithelium to provide an intact surface for the attachment of the mesh. The rectovaginal space was dissected to free the rectocele and enterocele from adjacent tissues. On each side, the ischial spines were identified. Two small stab incisions were made in the skin of each buttock 3 cm lateral and inferior to the external anal sphincter. The IVS Tunneller trocar (Tyco Healthcare, USS, Norwalk, CT, USA) was inserted through the buttock incisions and directed through the ischiorectal fossa up to the level of the ischial spine. After piercing the iliococcygeus muscle 1 cm caudal to the ischial spine, the Tunneller was turned medially and emerged through the vaginal incision at the vaginal apex as guided by the surgeon’s finger placed in the vagina or rectum. The same procedure was performed on the other side as well. Then 8-mm wide polypropylene multifilament IVS tapes were attached to the trocars and brought out through the incisions in the buttocks. The tapes were secured to the vault with two interrupted 2-0 PDS sutures and the free ends of the tapes emerging from the buttock incisions were withdrawn so that the vaginal apex was restored. The excess tape was excised below the level of the skin. The vertical vaginal incision on the posterior wall was then closed with locked 2-0 or 3-0 polyglactin (Vicryl, Johnson & Johnson Gateway, Irvine, CA, USA) sutures.
The patients were followed up after surgery at 6 weeks, 6 months, and thereafter at yearly intervals. At each visit, symptoms related to the pelvic support defects were reviewed and a follow-up data form was completed. At the clinical examination, the POPQ staging system for prolapse was used to assess the anatomical restoration.
The results were expressed as the mean ± SD. All statistical analyses were performed with the SPSS 13.0 software (SPSS, Chicago, IL, USA).
Results
Thirty-four patients were included in the study. All of the patients were menopausal and none of them were taking hormone replacement therapy. Seven patients had hypertension. All of the patients had undergone vaginal hysterectomy and a subsequent posterior IVS operation. Five (14.7%) patients who had urodynamically confirmed stress urinary incontinence underwent an additional TOT procedure.
All demographic and personal details are tabulated in Table 1. The mean operating time for the entire surgery was 106.3 ± 11.1 min. The mean perioperative drop in hemoglobin level was 1.7 ± 0.5 g/dl and mean hospital stay was 4.2 ± 0.8 days. There were no rectal, vesical, ureteric, or vascular injuries in this series and none of the patients required intraoperative or postoperative blood transfusions.
The mean follow-up duration was 12 months (range 3–20 months). One patient had recurrent prolapse and she underwent sacral colpopexy 3 months after the posterior IVS procedure. Thirty-three patients (97.1%) had satisfactory level I support defined objectively as stage 0 or I for point C as described in the POPQ system. Four patients had grade 2 cystocele (Aa points were at the 0 position in relation to the hymeneal ring). Postoperative shortening of total vaginal length was 1.4 ± 0.3 cm. Preoperative and postoperative pelvic quantification scores are shown in Table 2. Three patients developed de novo stress incontinence. In the postoperative period no complications, including tape erosion, were seen.
Discussion
Weakness of the uterosacral and parametrial support of the cervix and upper vagina is the main reason for upper genital or vault prolapse [15]. Colporrhaphy, plication of the uterosacral ligaments, and sacrospinous and sacral colpopexies have been reported previously as methods for the surgical correction of POP. However, they were associated with high (up to 58%) recurrence rates when the patients were evaluated according to objective POPQ scoring and subjective symptoms related to the prolapse [16]. Various new surgical techniques such as modified vaginal or abdominal colposacral and colposacrospinal fixations, via laparotomy or laparoscopy, have also been proposed for the treatment of POP in the last decade and they focused mainly on reconstruction of the pelvic floor [2, 7–10, 15]. In 2001, Petros reported his experience with a new surgical technique of posterior IVS (or infracoccygeal sacropexy) for vaginal vault prolapse [13]. DeLancey reviewed the importance of connective tissue structures by specifying three levels of vaginal support: Level 1: superior attachment (cardinal/uterosacral ligament complex); Level 2: lateral attachments (superolateral insertion points of the anterior vaginal wall, rectovaginal fascia); and Level 3: distal attachments (perineal body, perineal membrane) [17]. Although it is controversial, infracoccygeal sacropexy has been proposed as a useful technique for repairing all the levels [13].
There are few studies reporting the short-term efficacy and complications of posterior IVS. In most of the previous studies using similar posterior IVS tapes and techniques, the success rates of this surgical method ranged from 91 to 97.8%, with an average follow-up time of 12 (range 2–24) to 18.7 (range 7–49) months [12, 18]. The overall short-term success rate of the posterior IVS was 95.6%, with a mean follow-up time of 33.0 ± 23.2 weeks and the median being 31.9 weeks in the study by Luck et al. [19]. However, Jordaan et al. have reported that the success rate was 75% in their small study group of patients having grades 3–4 uterine prolapse with a median follow-up time of 13 months (1–21 months) [20]. We have not found any study in the literature related only to grade 4 uterine prolapse treated with posterior IVS. In our study, recurrence of prolapse was observed in only one patient and the success rate was 97.1%. The high success rate in our study may be explained by the relatively short follow-up period [12 months (range 3–20 months)]; however, we can conclude that our results are not very different from those of most of the other studies having similar follow-up times except the study by Jordaan et al. [20]. However, anatomical success should not be the sole aim of prolapsus surgery. Pelvic organ functions and improvement of life quality should be also aimed. The severity of symptoms and their impact on the quality of life in women with urogenital prolapse may be assessed before and after the surgery with validated Prolapse Quality of Life questionnaire [21, 22].
The operative technique that we have used has distinct advantages. It is a minimally invasive procedure that is quick to perform and requires minor dissection of the pararectal space. It also has a low risk of intraoperative complications [23, 24]. No complications in terms of rectal, vesical, or ureteric injuries occurred and none of the patients required blood transfusions in this study. Smajda et al. have performed human cadaveric dissections and shown that the needle used for the procedure stays at a distance of 4 cm away from the major vessels, avoiding potentially life threatening hemorrhage [24]. The incidence of mesh erosion was between 0 and 10% in the literature. In the study by Farnsworth, tape rejection occurred in 5 of the 49 patients who had nylon tapes implanted. No rejections were evident in 44 patients in whom polypropylene tape was used [12]. We also used polypropylene multifilament tape in our study and did not observe any complication regarding mesh erosion. Absence of mesh erosion in our study may be due to insertion of mesh under rectovaginal fascia and short follow-up period in our patients. However, in the study by Luck et al., there was an 18% incidence of mesh erosion and it occurred late in the postoperative period.
The pathological cause of uterine prolapse is loss of integrity of the uterosacral–cardinal ligament complex and weakening of the pelvic diaphragm, allowing uterine descent below the levator plate. Hysterectomy alone fails to address this problem [25] and also leads to lose the beneficial opportunity to secure the apical support of the central pelvic floor compartment to the cervical ring and recruit the whole pelvic ligaments to the reconstruction. However, Neuman et al. have reported that uterine conservation or concomitant vaginal hysterectomy does not affect either the cure or the complication rates of the posterior IVS technique [26]. Our patients were all in the postmenopausal period and all of them had undergone vaginal hysterectomy before posterior IVS. In our study, we detected a vaginal shortening of 1.4 ± 0.3 in the postoperative period. In our opinion, when the vaginal length is short or uterine preservation is aimed, posterior IVS without vaginal hysterectomy may be a safe option.
Conclusions
Posterior IVS is a minimally invasive procedure for grade 4 genital prolapse with a high success rate.
References
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506. doi:10.1016/S0029-7844(97)00058-6
Cook JR, Seman EI, O’Shea RT (2004) Laparoscopic treatment of enterocele: a 3-year evaluation. Aust N Z J Obstet Gynaecol 44:107–110. doi:10.1111/j.1479-828X.2004.00174.x
Nygaard I, Bradley C, Brandt D (2004) Pelvic organ prolapse in older women: prevalence and risk factors. Obstet Gynecol 104:489–497
Burrows LJ, Meyn LA, Walters MD, Weber AM (2004) Pelvic symptoms in women with pelvic organ prolapse. Obstet Gynecol 104:982–988
Ghetti C, Gregory WT, Edwards SR, Otto LN, Clark AL (2005) Pelvic organ descent and symptoms of pelvic floor disorders. Am J Obstet Gynecol 193:53–57. doi:10.1016/j.ajog.2004.12.004
Marinkovic SP, Stanton SL (2004) Incontinence and voiding difficulties associated with prolapse. J Urol 171:1021–1028. doi:10.1097/01.ju.0000111782.37383.e2
Carter JE, Winter M, Mendehlsohn S, Saye W, Richardson AC (2001) Vaginal vault suspension and enterocele repair by Richardson-Saye laparoscopic technique: description of training technique and results. JSLS 5:29–36
Lovatsis D, Drutz HP (2003) Vaginal surgical approach to vaginal vault prolapse: considerations of anatomic correction and safety. Curr Opin Obstet Gynecol 15:435–437. doi:10.1097/00001703-200310000-00013
Flynn BJ, Webster GD (2002) Surgical management of the apical vaginal defect. Curr Opin Urol 12:353–358. doi:10.1097/00042307-200207000-00015
Neuman M, Zuckerman B, Lavie O, Beller U (2000) Vaginal vault prolapse: repair by sacrospinous ligament fixation. Harefuah 138:17–19
Petros PE (1997) New ambulatory surgical methods using an anatomical classification of urinary dysfunction improve stress, urge and abnormal emptying. Int Urogynecol J Pelvic Floor Dysfunct 8:270–277. doi:10.1007/BF02765483
Farnsworth BN (2002) Posterior intravaginal slingplasty (infracoccygeal sacropexy) for severe posthysterectomy vaginal vault prolapse—a preliminary report on efficacy and safety. Int Urogynecol J Pelvic Floor Dysfunct 13:4–8. doi:10.1007/s001920200001
Petros PE (2001) Vault prolapse II: Restoration of dynamic vaginal supports by infracoccygeal sacropexy, an axial day-case vaginal procedure. Int Urogynecol J Pelvic Floor Dysfunct 12:296–303. doi:10.1007/PL00004039
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17. doi:10.1016/S0002-9378(96)70243-0
DeLancey JO (2005) The hidden epidemic of pelvic floor dysfunction: achievable goals for improved prevention and treatment. Am J Obstet Gynecol 192:1488–1495. doi:10.1016/j.ajog.2005.02.028
Whiteside JL, Weber AM, Meyn LA, Walters MD (2004) Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol 191:1533–1538. doi:10.1016/j.ajog.2004.06.109
DeLancey JO (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166:1717–1724
Neuman M, Lavy Y (2008) Posterior intra-vaginal slingplasty for the treatment of vaginal apex prolapse: medium-term results of 140 operations with a novel procedure. Eur J Obstet Gynecol Reprod Biol 140:230–233. doi:10.1016/j.ejogrb.2006.07.035
Luck AM, Steele AC, Leong FC, McLennan MT (2008) Short-term efficacy and complications of posterior intravaginal slingplasty. Int Urogynecol J Pelvic Floor Dysfunct 19:795–799. doi:10.1007/s00192-007-0527-1
Jordaan DJ, Prollius A, Cronje HS, Nel M (2006) Posterior intravaginal slingplasty for vaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct 17:326–329. doi:10.1007/s00192-005-0007-4
Cam C, Sakalli M, Ay P, Aran T, Cam M, Karateke A (2007) Validation of the prolapse quality of life questionnaire (P-QOL) in a Turkish population. Eur J Obstet Gynecol Reprod Biol 135:132–135. doi:10.1016/j.ejogrb.2007.06.009
Digesu GA, Chaliha C, Salvatore S, Hutchings A, Khullar V (2005) The relationship of vaginal prolapse severity to symptoms and quality of life. BJOG 112:971–976. doi:10.1111/j.1471-0528.2005.00568.x
Biertho I, Dallemagne B, Dewandre JM, Markiewicz S, Monami B, Wahlen C, Weerts J, Jehaes C (2004) Intravaginal slingplasty: short term results. Acta Chir Belg 104:700–704
Smajda S, Vanormelingen L, Vandewalle G, Ombelet W, de Jonge E, Hinoul P (2005) Translevator posterior intravaginal slingplasty: anatomical landmarks and safety margins. Int Urogynecol J Pelvic Floor Dysfunct 16:364–368. doi:10.1007/s00192-004-1264-3
Marana HR, Andrade JM, Marana RR, Matheus de Sala M, Philbert PM, Rodrigues R (1999) Vaginal hysterectomy for correcting genital prolapse. Long-term evaluation. J Reprod Med 44:529–534
Neuman M, Lavy Y (2007) Conservation of the prolapsed uterus is a valid option: medium term results of a prospective comparative study with the posterior intravaginal slingoplasty operation. Int Urogynecol J Pelvic Floor Dysfunct 18:889–893. doi:10.1007/s00192-006-0262-z
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kolusari, A., Yildizhan, R., Adali, E. et al. Short-term results of posterior intravaginal slingplasty in grade 4 uterine prolapse. Arch Gynecol Obstet 281, 55–58 (2010). https://doi.org/10.1007/s00404-009-1062-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-1062-8