Abstract
Introduction and hypothesis
The aim of this study was to assess the safety and efficacy of vaginal native tissue repair and uterine suspension after a follow-up of at least 1 year.
Methods
We included all consecutive women with an anterior vaginal prolapse of stage II or higher and a concomitant uterine prolapse of stage II who underwent this surgical procedure. We considered women with a descensus with maximum point of less than −1 in any compartment as objectively cured. Overall success was defined as no prolapse symptoms, together with a Patient Global Impression of Improvement (PGI-I) score of 2 or less, prolapse of stage lower than II, and no need for other surgery.
Results
A total of 102 patients underwent this surgical procedure during the study period and met all the inclusion criteria for statistical analysis. The mean follow-up was 31 ± 8.2 months; no patient was lost to follow-up. Five patients (4.9%) showed postoperative complications. In terms of subjective outcomes, at the last available follow-up, failure of this surgical procedure was seen in 2% of patients. The objective cure rate and the overall cure rate were the 95.1%. No significant deterioration in objective cure rates was observed over time (p = 0.6).
Conclusions
Vaginal repair and hysteropexy appear to be an effective and safe option for women with advanced uterovaginal prolapse.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is a very common condition, and the prevalence is more than 40% in women over 45 years old [1]. A relevant proportion of younger women are also affected by this clinical condition. It is estimated that every woman has an 11–17% life-time risk of undergoing surgery for POP [2, 3]. In the vast majority of patients this pathology has important negative effects on quality of life and is associated with physical, psychological and sexual disorders [4]. Hysterectomy is the most commonly performed surgical treatment for POP in the world [5, 6], and is also performed when the uterine prolapse has only a passive role. Surprisingly, in spite of this scenario, scientific evidence does not support this clinical practice. In a very interesting study by Korbly et al. [7], women (of whom only 3% were fertile) with symptoms of POP clinically confirmed by urogynaecologist preferred a conservative surgical option with uterine preservation rather than hysterectomy, regardless of the probability of the effectiveness of the different surgical techniques. However, conflicting data exist regarding the role of hysterectomy in the treatment of POP, and many different uterus-sparing surgical procedures have been proposed [8]. Studies comparing hysterectomy with uterine suspension to the uterosacral-ligaments and sacrospinous hysteropexy have generally found no significant differences at 12 months of follow-up in terms of anatomical recurrence, surgical complications and quality of life [4, 8].
Maher et al. [8] were the first to describe an apical suspension procedure in which cervical tissue is included in the transverse plication of the pubocervical fascia; however, their procedure also involved sacrospinous suspension to the posterior cervix. A few years later, Huffaker et al. [9] described a procedure for transverse cystocele repair with uterine preservation using native tissue with anterior colporrhaphy, but they included only women with stage 0 or I apical prolapse. The aim of this study was to prospectively evaluate for the first time the safety and efficacy of the vaginal procedure of anterior and apical repair that includes closure of the transverse defect with cervical stroma and therefore uterine suspension in women with anterior vaginal prolapse of stage II or higher and concomitant stage II uterine prolapse, with a follow-up of at least 1 year.
Materials and methods
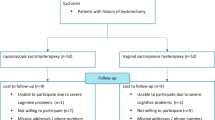
The present prospective study was conducted in a single urogynaecological unit at the University of Insubria in Varese, Italy, between January 2013 and June 2016. All consecutive women with symptomatic anterior compartment prolapse higher than stage II and a concomitant stage II uterine prolapse according to the Pelvic Organ Prolapse Quantification (POP-Q) system. Written informed consent was obtained preoperatively, and Institutional Review Board approval was obtained from our Institution before the start of the study. Preoperative evaluation included medical history, physical examination, a 3-day frequency/volume chart, urine analysis for the presence of infection, pelvic ultrasonography and urodynamic (UDS) evaluation. Physical examination was performed with the patient in the dorsal lithotomy position and POP was evaluated during a maximal Valsalva manoeuvre according to the POP-Q system [10]. Only women with a real uterine prolapse of stage II and not those with an elongated cervix simulating a prolapse were included. The UDS evaluation included uroflowmetry, filling cystometry and a pressure/flow study performed by a trained urogynaecologist using a standardized protocol in accordance with the Good Urodynamic Practice Guidelines of the International Continence Society (ICS) [11].
Women were identified as symptomatic for prolapse if they complained of any prolapse symptom and/or if, under direct questioning, they reported a sensation of “vaginal bulge” or a “lump of fullness in the vagina” the severity of which they recorded on a visual analogue scale (VAS). Each patient was asked to record the impact of the genital prolapse on her quality of life using a 0 to 10-cm horizontal VAS, with 0 cm indicating no impact and 10 cm the worst imaginable impact. Exclusion criteria were: abnormal uterine bleeding, endometrial abnormalities on ultrasonography and/or curettage, family history of cancer, prolapse of the posterior vaginal compartment higher than stage I, uterine prolapse with point C greater than +1 cm, previous pelvic reconstructive surgery, neurological disease, psychiatric disease, and pelvic disease requiring a concomitant abdominal procedure.
All women received a modified version of the surgical procedure as described by Huffaker et al. [9]. This intervention includes a transverse cystocele repair with uterine preservation, suspending the plicated pubocervical connective tissue to the cervical stroma. The same surgeon with an extensive background in urogynaecological surgery performed all the procedures.
The patients stayed in hospital for one night with a urinary catheter and a gauze in the vagina. After removal of the catheter, a urine culture was performed and the patient was evaluated at least twice ultrasonographically for the presence of a postvoid residual. Follow-up evaluations involving urogynaecological examination at 3 and 12 months after surgery and then every year were scheduled. The follow-up examinations were performed by two urogynaecological physicians who did not participate in the surgical procedures. At each follow-up visit, physical examination and a urinalysis were performed, and the presence of POP or urinary tract infection were recorded.
Patient satisfaction was assessed using the Patient Global Impression of Improvement (PGI-I) for urogenital prolapse, a seven-point Likert scale, with a range of responses from 1 (“very much improved”) to 7 (“very much worse”) [12]. A response of “very much improved” or “much improved” (PGI-I score ≤2) together with absence of bulge symptoms was considered objective success. A descensus with a maximum point of less than −1 in any compartment was considered objective cure. In some randomized trials, overall success was defined as absence of prolapse symptoms, a PGI-I score of 2 or less, prolapse stage lower than II, and no need for other surgery [13]. All patients completed the Prolapse Quality of Life (P-QOL) questionnaire [14, 15] both before surgery and at every follow-up visit. In the P-QOL questionnaire, the responses range from “none/not at all”, through “slightly/a little” and “moderately”, to “a lot”. Scores in each domain range from 0 to 100. A higher total score indicates a greater impairment of quality of life, while a lower total score indicates a better quality of life.
Surgical technique
Preoperative prophylactic intravenous antibiotics and spinal anaesthesia were administered to all patients. Using a tenaculum or Martin’s clamp on the cervix, examination under anaesthesia was performed prior to surgery to assess uterine and cervical support.
After instillation of one vial of methylene blue into the bladder, a series of Allis clamps were placed in the mid-longitudinal plane from the urethrovesical junction to the anterior lip of the cervix. A midline longitudinal colpotomy was performed and the vaginal epithelium was then dissected away from the underlying pubocervical connective tissue and bladder. The anterior wall of the uterine cervix was also dissected from the base of the bladder to expose the entire anterior isthmocervical portion. This portion was grasped bilaterally with two pieces of Vicryl 0.0 suture. The midline plication of the pubocervical connective tissue was then performed. To close the transverse defect and to suspend the isthmus of the uterus at the endopelvic tissue, the two previously inserted suspensory sutures in the cervical stroma to the side were attached to the repaired pubocervical fascia. If necessary, the vaginal epithelium was trimmed. Anterior colporrhaphy was completed with a series of simple side-to-side interrupted Vicryl 2.0 sutures. Following the procedure, a urinary Foley catheter and a vaginal gauze were placed for the night.
Statistical analysis
Statistical analysis was performed using SPSS for Windows, version 17 (SPSS, Chicago, IL) and GraphPad version 6 (GraphPad Software, San Diego, CA). The chi-squared and Fisher’s exact tests were used to analyse proportions, as appropriate. Student’s t test and the Mann–Whitney U test were used to compare continuous parametric and nonparametric variables, as appropriate. The chi-squared and the chi-squared test for trend were used to analyse and compare the surgical outcomes during follow-up. The chi-squared test is the most appropriate test to evaluate the tendency of the success of the surgical procedure to decrease over time by comparing the cure rates at the different follow-up visits (1 year, 2 years and 3 years). The null hypothesis was that there was no association between the cure rate of this surgical procedure and time. The Cox proportional hazards model was used for univariate analysis to evaluate factors potentially affecting the risk of recurrence (subjective or objective) during the study period. P values <0.05 were considered statistically significant.
Results
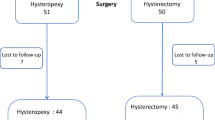
A total of 102 patients underwent transverse cystocele repair with suspension of the uterus during the study period and met all the inclusion criteria for statistical analysis; two patients were excluded because they did not accept a surgical treatment. The mean follow-up was 31 ± 8.2 months and no patient was lost to follow-up. Table 1 shows the baseline patient characteristics and their preoperative UDS data. The preoperative ICS POP stages in the apical and anterior compartments are shown in Table 2, and surgical data are shown in Table 3. No intraoperative complications were observed.
In the early postoperative period during hospitalization, complications occurred in five patients (4.9%): hypertension in one patient, urinary retention that resolved with an indwelling catheter for 24 h in two patients, deep vein thrombosis in two patients, and urinary tract E. coli infection in one patient. Long-term complications occurred in three patients (2.9%): recurrent urinary tract infection in one patient, sexual inactivity with synechiae between the posterior vaginal wall and the anterior cervical lip in one patient, and stress urinary incontinence in one patient. None of the patients reported relevant postoperative pain on day 1 (VAS 0 ± 1 cm).
In terms of subjective outcomes, at the last available follow-up, two patients (2%) showed anatomical prolapse recurrence of both the anterior compartment (point Ba at 0 and +1 cm, respectively) and the apical compartment (point C at 0 cm in both). These two patients required a second surgical procedure including vaginal hysterectomy. In terms of objective outcomes, another five patients (4.9%) showed asymptomatic recurrence in the anterior compartment (point Ba 0 cm in all five). The overall cure rate was the 95.1%. Three patients (2.9%) were pregnant during the study period. Two of these women underwent an elective caesarean section without any neonatal complications, and neither showed any recurrence of prolapse, and the other was 14 weeks pregnant at the time of this report.
Table 4 shows the Ba and C POP-Q point measurements before surgery and at the 12-month and last available follow-up visits. The other POP-Q points showed no statistically significant differences. These results indicate anatomical success both in the anterior and the central compartment that was statistically and clinically relevant and persisted over time. Table 5 shows the P-QOL scores. Table 6 shows the evolution of the subjective and objective cure rates over time. Subjective and objective cure rates persisted during the entire follow-up period. Evaluation of possible predictive factors associated with recurrence of prolapse showed that only a preoperative point C of +1 cm was a risk factor for failure (Table 7).
Discussion
This study showed that transverse cystocele repair with hysteropexy in women with a predominant anterior prolapse and a concomitant central compartment prolapse of II stage is a safe and effective procedure. It can be considered an alternative procedure for preserving the uterus, in particular in women who desire to preserve their uterus or in patients with severe comorbidities who are therefore poor candidates for hysterectomy. Hysterectomy is a traditional component of surgery for prolapse. Baden and Walker in 1992 [16] considered that “the first step in any anterior or posterior vaginal repair is to ensure grade 0 support at superior segmental and cul-de-sac sites”. Huffaker et al. [9] considered that a careful repair of the anterior compartment with an adequate transverse cystocele repair is able to offer a very high objective and subjective cure rate of POP in cases of moderate uterine prolapse (stage II or higher) without performing a large apical suspension. Madhu et al. [17] investigated the use of cervical traction under anaesthesia to measure the real stage of uterine prolapse in women with anterior vaginal descensus and mild uterine prolapse. They found that preoperative cervical traction is not necessary, as only anterior fascial repair with adequate transverse cystocele repair resulted in high postoperative cure rates of POP irrespective of the effect of forced uterine descensus [18].
Korbly et al. [7] conducted a multicentre, cross-sectional study in 213 women with symptomatic prolapse to evaluate patient preference for uterine preservation or hysterectomy. A significantly higher proportion of the women preferred uterine preservation over hysterectomy. Geographic region, education level, and belief that the uterus is important for a sense of self were independent predictors of preference for uterine preservation.
Our study clearly demonstrated that a procedure that includes a vaginal transverse cystocele repair with hysteropexy have a limited operating time, minimal morbidity, no significant blood loss and a very low overall rate of postoperative and intraoperative complications. It is relevant to underline that women who undergo this procedure do not feel any postoperative pain. Also other available studies have shown that a similar technique can provide a good outcome when adequate uterine and cervical support are recreated [9]. In our clinical practice, this procedure may be proposed and performed in particular in older women with several associated comorbidities and who have had “few stresses” to the pelvic floor during their life. However, it may also be useful in younger women desiring to preserve their uterus. It is recommended that a careful preoperative assessment is performed including a clinical and anamnestic history, and an intraoperative assessment of each vaginal compartment is also mandatory to determinate the appropriate procedure. For the uterus-preserving operative procedures described in the literature in which mesh is used, and for the laparoscopic, robotic, abdominal and vaginal procedures in which mesh is not used, there are no clear gold standards, and Gutman and Maher conclude that it is necessary to have more randomized studies [19].
The present study confirmed that our procedure is also safe and effective in the medium term without any worsening of the cure rate over time. It is very important to underline that the only independent risk factor for failure of this procedure and symptomatic recurrence of POP is uterine prolapse beyond the hymen (point C +1 cm), and in such patients it is therefore mandatory to perform very complete and careful counselling. However, it is interesting that in our population we obtained a very relevant improvement in the anatomy of the apical compartment (postoperative point C −5 cm); in our opinion postoperative retraction of the scar tissue also contributed to this result.
The strengths of this study are (1) the substantial follow-up period, (2) the assessment of subjective and objective outcomes obtained using validated tools, and (3) the fact that no patients were lost to follow-up. Conversely, we acknowledge that a limitation of this study could be that at the time of this report not all patients had completed a follow-up of at least a 3 years. Another possible limitation is that we did not evaluate sexual function in our patients.
In conclusion, our results seem to show that transverse cystocele repair with suspension of the uterus using native tissue is a safe and effective option over at least 12 months in patients with uterine prolapse of stage II or lower. We obtained high subjective and objective cure rates with few recurrences and with a very low complication rate. On the basis of these results, we will soon start a randomized study.
References
Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, Steegers-Theunissen RP, Burger CW, Vierhout ME. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:1037–45.
Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol. 2001;184:1496–501.
Wu JM, Hundley AF, Fulton RG, et al. Forecasting the prevalence of pelvic floor disorders in U.S. women: 2010 to 2050. Obstet Gynecol. 2009;114:1278–83.
Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6.
Detollenaere RJ, den Boon J, Kluivers KB, Vierhout ME, van Eijndhoven HW. Surgical management of pelvic organ prolapse and uterine descent in the Netherlands. Int Urogynecol J. 2013;24:781–8.
Korbly NB, Kassis NC, Good MM, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209:470.e1–6.
Maher CF, Cary MP, Slack MC, Murray CJ, Milligan M, Schluter P. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:381–4.
Huffaker RK, Kuehl TJ, Muir TW, Yandell PM, Pierce LM, Shull BL. Transverse cystocele repair with uterine preservation using native tissue. Int Urogynecol J. 2008;19:1275–81.
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26.
Schafer W, Abrams P, Liao L, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002;21:261–74.
Srikrishna S, Robinson D, Cardozo L. Validation of the Patient Global Impression of Improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21:523–8.
Chmielewski L, Walters MD, Weber AM, Barber MD. Reanalysis of a randomized trial of 3 techniques of anterior colporrhaphy using clinically relevant definitions of success. Am J Obstet Gynecol. 2011;205:69.e1–8.
Digesu GA, Khullar V, Cardozo L, Robinson D, Salvatore S. P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:176–81.
Digesu GA, Santamato S, Khullar V, et al. Validation of an Italian version of the prolapse quality of life questionnaire. Eur J Obstet Gynecol Reprod Biol. 2003;106:184–92.
Baden WF, Walker T. Surgical repair of vaginal defects. Philadelphia: Lippincott; 1992.
Madhu C, Foon R, Agur W, Smith P. Does traction on the cervix under anaesthesia tell us when to perform a concomitant hysterectomy? A 2-year follow-up of a prospective cohort study. Int Urogynecol J. 2014;25:1213–7.
Serati M, Rizk D, Savatore S. In the footsteps of Bonney and Nichols: hysterectomy during surgical repair of pelvic organ prolapse. Int Urogynecol J. 2017;28:823–5.
Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24:1803–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Serati, M., Braga, A., Cantaluppi, S. et al. Vaginal cystocele repair and hysteropexy in women with anterior and central compartment prolapse: efficacy and safety after 30 months of follow-up. Int Urogynecol J 29, 831–836 (2018). https://doi.org/10.1007/s00192-017-3498-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3498-x