Abstract
Introduction
Single-event multilevel surgery (SEMLS) is frequently used to correct pathological gait patterns in children with bilateral spastic cerebral palsy (BSCP) in a single session surgery. However, in-depth long-term evaluation reports of gait outcomes are limited. Therefore, we investigated if SEMLS is able to correct lower extremity joint and pelvic angles during gait towards typically developing gait patterns (TDC) in children with BSCP, and if so, if this effect is durable over a 10-year period.
Materials and methods
In total 13 children with BSCP GMFCS level II at time of index-surgery between the ages of 7.7–18.2 years at the time of SEMLS were retrospectively recruited. Three-dimensional gait data were captured preoperatively, as well as at short-, mid-, and long-term post-operatively, and used to analyze: movement analysis profile (MAP), gait profile score (GPS), and lower extremity joint and pelvic angles over the course of a gait cycle using statistical parametric mapping.
Results
In agreement with previous studies, MAP and GPS improved towards TDCs after surgery, as did knee extension during the stance phase (ɳ2 = 0.67; p < 0.001), while knee flexion in the swing phase (ɳ2 = 0.67; p < 0.001) and pelvic tilt over the complete gait cycle (ɳ2 = 0.36; p < 0.001) deteriorated; no differences were observed between follow-ups. However, further surgical interventions were required in 8 out of 13 of the participants to maintain improvements 10 years post-surgery.
Conclusions
While the overall gait pattern improved, our results showed specific aspects of the gait cycle actually deteriorated post-SEMLS and that a majority of the participants needed additional surgery, supporting previous statements for the use of multilevel surgery rather than SEMLS. The results highlight that the field should not only focus on the overall gait scores when evaluating treatment outcomes but should offer additional long-term follow-up of lower extremity function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Single-event multilevel surgery (SEMLS) is used to correct gait function and deteriorations of lower limb deformities in children suffering from bilateral spastic cerebral palsy (BSCP) as well as to avoid repeated episodes of surgery and rehabilitation [31]. The goal is to approach gait patterns of typically developing children and young adults (TDC) in a single-session surgery, albeit more intensive than a series of individual surgeries [19]. Research consistently shows that SEMLS is a safe and effective surgical intervention, which improves the overall kinematic gait patterns in the short- (1–2 years post-operation), mid- (5–7 years), as well as long-term (≥ 9 years) [7, 13, 21, 25]. By now, SEMLS is frequently used, and even considered a gold standard for treating gait dysfunction due to lower limb deformities in BSCP [15].
Despite the increasing research into SEMLS, most of the studies have been limited to short- and mid-term results [13, 15]. The few studies that have examined long-term outcomes, reported only on specific kinematic features [21, 28] or gait scores [7, 28], whereby the impact on the overall gait pattern remained unknown and clinically relevant information might have been overlooked [27]. Therefore, to address any possible shortcomings in gait over the long term, a more comprehensive approach to evaluate the effects of intervention after 10 years should be included over and above the currently reported gait scores. Here, approaches such as statistical parametric mapping (SPM) now open perspectives to perform hypothesis testing on kinematic waveforms in a more continuous manner compared to gait scores [23, 24]. For example, the application of this approach to evaluate the impact of botulinum toxin A (BTX-A) in BSCP [18] has been able to highlight differences at specific parts of the gait cycle compared to conventional analyses.
The main purpose of this retrospective case study was to evaluate whether lower extremity joint and pelvic angles during gait return towards TDC after SEMLS documented by the use of gait scores and SPM, as well as to examine whether these effects are durable over 10-years of follow-up-treatment. Since the index surgery often requires further surgical interventions to maintain the achieved gait corrections [7, 25, 32], the total number of additional surgeries performed within 10 years after SEMLS was also investigated.
Methods
Participants
Participants were selected from the motion analysis laboratory database of the local children’s hospital. Selected participants had undergone SEMLS between 2002 and 2010. Participants underwent pre- and post-operative three-dimensional gait analysis (3DGA) between 2000 and 2018. Participants were included for this study if they had a Gross Motor Function Classification System (GMFCS) level II at the time of operation, and had undergone 3DGA preoperatively (E0: before index surgery), short-term (E1: up to 2 years post-index surgery), mid-term (E2: 3–6 years) and long-term (E3: ≥ 8 years). Exclusion criteria were marked signs of movement disorders other than BSCP, over 20 years of age at the time of surgery, and/or selective dorsal rhizotomy (SDR) surgery before one of the 3DGA sessions. Patients who were treated with BTX-A prior to SEMLS were included if at least 6 months had elapsed between the last injection and the following 3DGA.
In total, 31 potentially eligible participants were identified. Overall, 3 participants were excluded due to previous SDR, an additional 14 due to missing gait assessments (E2 and/or E3), and 1 because the age at surgery was > 20 years. Finally, data from 13 participants aged between 7 and 18 years (mean: 13 years and 2 months) at index surgery were included in this study (1 out of these 13 had missing data for E1, the missing data was replaced by the mean of the whole group) (Table 1). Of these 13 patients, 12 had been included in a previous study [25] looking at E2 results following SEMLS. All measurements in this study, which was approved by the local ethical committee (EKNZ 304/08, amendment PB 2018-00168), were conducted according to the current version of the World Medical Association Declaration of Helsinki. All patients and/or their parents provided written informed consent that their data was used in this study.
3DGA outcomes from randomly selected TDC, age-matched with the participants at E3, are included as reference values in the figures. These data were extracted from the same database and processed similarly to the data of the participants.
Description of surgery
Information regarding indications for and implementation of SEMLS, as well as post-operative treatment procedures (e.g. pain management, hospital stay, casting, radiographs to check healing, rehabilitation program) were published previously [25]. All surgical interventions were carried out by 2 experienced paediatric orthopaedic surgeons. In total, participants had undergone 116 operative procedures, whereby 85 were performed as index surgeries [see Electronic Supplementary Material (ESM) 1].
Measurements performed
GMFCS level and anthropometric data were collected before each 3DGA to classify each patient’s functional mobility level and body mass index (BMI), and hence allow appropriate scaling of the kinematic gait outcomes.
Standardized 3DGA measurements were performed in the Laboratory for Movement Analysis by experienced movement scientists, using a VICON motion analysis system (VICON, Oxford, UK). Participants walked barefoot at their self-selected speed along an 8 m level walkway. The Helen Hayes marker set was used [10], and at least six trials were recorded per measurement, consistent with previous studies [25].
Data analysis
Pre-processing of the data was performed by an experienced assessor in the VICON Nexus software, and included a visual setting of gait events (foot strike and toe-off), filtering of the data using the built-in Woltring filter (mean squared error set to 10 mm2), and calculation of the joint kinematics using the Plug-in Gait model. Further analyses were performed in MATLAB (Math Works, Inc. Version R2015a, Natick, USA) with the open-source Biomechanical ToolKit package for MATLAB [4]. Trials with excessive soft tissue artefact, poor consistency, or signs of inaccurate marker placement were excluded. The first six valid gait cycles (GCs) of each limb, whenever possible from six different gait trials, were used for further analyses. A GC was defined as the time between two consecutive heel-strikes of the same leg.
Lower extremity joint and pelvic angles were used to calculate the movement analysis profile (MAP) and gait profile score (GPS) as described in [2, 3]. Based on existing data regarding gait deviations in BSCP, the following joint angles were selected for further in-depth analysis: sagittal and transversal joint (foot, knee, hip) and pelvic angles [17, 20]. These angles, reported in degrees, were time-normalized over each entire GC (0–100% GC) [9].
All analyses were performed for both the left and right sides; with results for the right limb presented in the results section, while those from the left side can be found in ESM 2.
Statistical analysis
Normal distribution of the kinematic data was verified visually by creating QQ-plots using SPSS version 25 (IBM SPSS Statistics for Macintosh, IMB Corp, Armonk, NY). Differences in MAP and GPS over time (4 levels, E0, E1, E2, E3) were determined using one-way repeated measures analysis of variance (rm-ANOVA), with post-hoc comparisons adjusted using Bonferroni corrections. To estimate the effect of age at index surgery had on GPS outcomes and amount of additional surgeries required in our cohort, the Spearman's rank correlation coefficient was calculated (as done in [29]). To examine in more detail whether the mean waveforms of the joint and pelvic angles differed significantly over the 4 time-periods, SPM with rm-ANOVA (SPM{F} and post-hoc paired t test SPM{t}: spm1d-package, version 0.4 http://www.spm1d.org/) was performed over the entire GC. Effect sizes for the ANOVAs were calculated as partial eta squared (η2) and are presented as mean values over the statistically significant regions of the GC [14]. Significance was set at α = 0.05.
Results
Evaluation of joint angles: MAP and GPS
MAP scores significantly improved over time (E0 vs E1/E2/E3) for hip flexion (HF) (p = 0.026, ɳ2 = 0.24), knee flexion (KF) (p < 0.001, ɳ2 = 0.55), ankle dorsiflexion (ADF) (p = 0.034, ɳ2 = 0.31), internal pelvic rotation (PR) (p = 0.043, ɳ2 = 0.27), and internal foot progression (p = 0.024, ɳ2 = 0.33) (Fig. 1). The overall GPS also significantly improved after the operation and during longitudinal care (E0 vs E1/E2/E3, p < 0.001; ɳ2 = 0.64). No significant differences were observed between the follow-ups. On an individual patient level, an improvement between E0 and E1 was observed above the clinically important difference (CID, ∆ > 1.6° GPS [2]) for 10 out of 13 participants (Fig. 2). Between E1 and E2, 7 participants showed further improvement above the CID, while 1 deteriorated. Between E2 and E3, 1 participant improved while 3 deteriorated. When comparing E0 to E3, and taking the average over left and right side, all participants improved above CID (median = 5.65, range 2.3–15.6). No significant correlation was found between age at index surgery and long-term GPS outcomes (r = 0.14, p = 0.63).
Movement analysis profile and gait profile score (GPS). The different follow-up results are given as E0 (pre-operative), E1 (1–2 years post-index surgery), E2 (3–6 years post-index surgery), and E3 (≥ 8 years post-index surgery); TDC represents norm values for typically developing children. *Indicates significant differences, p < 0.05, ***p < 0.001 for one-way repeated measures analysis of variance model. As similar results were obtained for both sides, only data for the right limbs are presented. For detailed results concerning the contralateral side, see Electronic Supplementary Material 2
Difference in Gait profile score (GPS) before and after SEMLS against age at index surgery. Star (*) indications difference between E0 (pre-operative) and E1 (1–2 years post-index surgery), circle (o) the difference between E0 and E2 (3–6 years post-index surgery), cross (x) the difference between E0 and E3 (≥ 8 years post-index surgery). When the symbol is in bold it indicates additional surgical interventions took place before the follow-up measurement. The dotted line indicated the clinically important difference (CID, ∆ > 1.6° GPS [2]) for change in GPS. As similar results were obtained for both sides, only data for the right limbs are presented. For detailed results concerning the contralateral side, see Electronic Supplementary Material 2
Evaluation of joint angles: SPM
SEMLS combined with longitudinal care significantly increased anterior pelvic tilt (APT) (over the entire GC over time, p < 0.001; ɳ2 = 0.36, Fig. 3). A significant decrease was found for KF (over the entire GC over time, p < 0.001; ɳ2 = 0.67). No significant differences were observed between follow-ups for any of the investigated angles.
SPM results for the sagittal and transversal joint and pelvic angles. The different follow-ups are given as E0 (pre-operative), E1 (1–2 years post-index surgery), E2 (3–6 years post-index surgery), and E3 (≥ 8 years post-index surgery). Top graph, shows the mean kinematic waveforms of the four investigated sagittal joint angles for all four measurements indicated as using thin lines, as well as one standard deviation of the mean values, illustrated as transparent stripes. The black bar directly below each angle represents significant differences in the gait phases, as detected using the statistical parametric mapping with F-distribution (SPM{F}). No significant differences were found by the post-hoc SPM{t}. As similar results were obtained for both sides, only data for the right limbs are presented. For detailed results concerning the contralateral side, see Electronic Supplementary Material 2
Evaluation of additional treatments after SEMLS
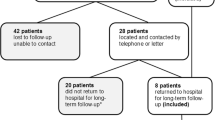
Overall, 8 out of 13 participants required additional surgery due to relapse (n = 3), newly developed biomechanical problems (n = 2) (NDBP), both relapse and NDBP (n = 2), or other non-gait related issues (n = 1) during the 10-year follow-up period (Fig. 4). Most additional surgeries were needed between E1 and E2 (5 due to relapse, 2 due to NDBP), while 2 participants required surgery between E2 and E3 (2 due to NDBP). After E3, 2 participants underwent additional operative interventions (1 due to NDBP and 1 due to a fall-related fracture of the femur). No significant correlation was found between age at index surgery and amount of additional surgical interventions required (r = − 0.16, p = 0.59). A more detailed description of the subsequent surgeries and additional treatment information can be found in ESM 1.
Additional surgical interventions performed after the index surgery. The different follow-up periods in which the additional interventions took place are given as E1–E2 (~ 2–5 years post-index surgery), E2–E3 (~ 5–8 years post-index surgery), > E3 (≥ 8 years), no additional surgeries were performed between SEMLS and E1
Discussion
Background and rationale
Currently, SEMLS is considered to be the gold standard therapy for correcting gait function and deterioration of lower limb deformities in BSCP [15, 32]. To the best of our knowledge, until now, an analysis of the gait pattern in a continuous manner after longitudinal care post-SEMLS has been missing. Therefore, our main goal was to investigate whether lower extremity joint and pelvic angles during gait return towards TDC after SEMLS, not only by means of gait scores but also by additionally using SPM. Our results have revealed that the overall gait patterns of SEMLS treated children with CP improve towards TDC, but improvements were mainly visible during the stance phase of gait, while deteriorations in swing phase were observed. Additional surgical interventions after SEMLS were required in 8 out of 13 of the participants to achieve satisfactory long-term results.
Limitations
The outcomes of this study provided a novel insight into the 10 years longitudinal treatment post-SEMLS; however, it had several limitations. First, the generalizability of the outcomes is limited due to a number of reasons, but mainly the small sample size, with only 13 participants. This is a common problem since indications for SEMLS are relatively uncommon and it is difficult to follow-up with participants long-term. Another reason for low generalizability of our outcomes is that they are likely to be relevant only to groups with BSCP for whom the two orthopaedic surgeons involved in this study established specific surgical indications. Due to the missing standardization for SEMLS indications, it is also difficult to compare the outcomes of our retrospective study to the results of other clinics. To improve the interpretation of the outcomes, we provide additional participant and treatment information in ESM 1. Second, multiple statistical tests were conducted that increased the risk of obtaining invalid significant results. To provide a clear understanding of whether a significant effect was also clinically relevant, it was decided to highlight the different levels of p values and include the effect size and CID whenever possible. Third, in two cases the time-gap between preoperative gait analysis (E0) and index surgery was up to 2 years (patients no. 5 and 7 in ESM 1). One could imagine that during this time-gap, the status of the patients might have changed, however, only in 1 of these patients additional surgical interventions were required, further information on this can be found in ESM 1. Fourthly, the age at which the index surgery was performed varied between the patients (7.7–18.2 years old), this is not ideal, as age at index surgery might effect long-term outcomes [29], but common within the field [33, 34]. In our cohort, the amount of additional procedures needed did not show to be dependent on the age at index surgery. Finally, this study lacked control groups of untreated and treated participants by means of non-operative methods. This is a common problem in the field, as not treating a patient, or not providing the best or most appropriate treatment for that patient is considered to be unethical. One needs to be aware when considering the presented outcomes that it remains unknown how these participants would have developed without the presented therapy, or indeed with other treatment options.
Evaluation of joint angles after SEMLS
Our results show that the patients’ overall gait patterns, evaluated using GPS, improved after surgery, which is in line with previous findings [1, 7, 25, 28, 31, 32]. These results appeared to be durable over a 10-year period when combined with longitudinal care (e.g. orthosis, physiotherapy, additional surgeries), as no differences were observed between the follow-ups. However, a more detailed examination of the joint and pelvic angles revealed some interesting findings:
Firstly, the pelvic tilt worsened over time when analysed using the SPM approach (Fig. 2), which is in line with the outcomes of Ancillao and co-workers [1], while the MAP results did not show a significant deterioration between pre- and post-surgery in this study, also in line with previous investigations [21, 28]. The SPM results would have been significant even with a Bonferroni correction and the effect size was moderate. As a result, the observed increased anterior pelvic tilt should not be ignored. The increased anterior pelvic tilt could be a result of the muscle tendon lengthening procedure that was performed to account for flexed knee gait, which is commonly observed in BSCP. Previous studies showed that such tendon lengthening leads to an excessive increase in anterior pelvic tilt [6, 8] and can be counteracted by supplementing the procedure with a rectus femoris transfer (RFT) [22]. Further research is needed to evaluate whether this additional procedure can prevent worsening of anterior pelvic tilt over time.
Significant differences were also observed in knee-flexion angle when using the SPM approach. Results revealed that adequate knee extension during stance phase seemed to happen at the expense of knee flexion during swing phase (Fig. 2). This is partly in line with previous findings [13] and could be explained by the hamstring lengthening procedure performed without RFT [16].
For the other angles, no significant differences were found after Bonferroni correction of the SPM results. This was in contrast to the MAP results, which showed improvements for hip flexion, ankle dorsiflexion, pelvic rotation, and foot progression. The discrepancy between MAP and SPM outcomes might be due to the more conservative approach of the SPM when using a Bonferroni correction. However, considerable differences could be observed when comparing the outcomes from these angles to previous reports [13]. As not all studies provided detailed information towards the specific corrections that were made during SEMLS, nor about the participants who underwent SEMLS, it is difficult to understand why the outcomes of the studies differ.
Evaluation of additional treatments after SEMLS
The second aim of our study was to investigate the number of additional operative procedures performed within the 10 years following SEMLS. Additional surgeries (n = 11 total; 5 relapse, 5 NDBP, 1 other) after E1 were required for 8 out of 13 of the participants, which is more than the rate described by Terjesen and co-workers (14 out of 34, 5 years follow-up) [30] as well as Dreher and co-workers (91 out of 231, 9 years follow-up) [7], but comparable to that reported by Thomason and co-workers (12 out of 18, 5 years follow-up) [32]. 7 out of 11 interventions were performed between E1–E2, which was mainly driven by the number of relapses. When comparing the present findings with the former study of Rutz and co-workers [25], only three further operative events were needed following E2. This provides some evidence that despite the additional procedures, most of the achieved effects were long lasting when longitudinal care was provided, which is in line with previous studies [7, 11, 12, 26, 30, 32]. It should be noted that BSCP without treatment most probably shows a trend of deterioration with age [5], which may account for the need for additional surgeries.
Conclusion
The current findings demonstrate that despite the natural course of deterioration in BSCP over time, outcomes after SEMLS are maintained over 10 years when combined with longitudinal care (orthosis, physiotherapy, and additional operations in 8 out of 13 participants). As over half of the participants in our study needed additional surgical interventions, it may not be appropriate to focus on a single-stage surgery as also concluded by Dreher and co-workers [7]. Furthermore, the detailed and comprehensive analysis showed that while the joint angles improved during stance phase, these improvements were at the cost of deteriorations during swing phase, highlighting that the investigation should not only focus on the overall gait scores when evaluating treatment outcomes but should additionally consider more continuous forms of analysis.
References
Ancillao A, Van Der Krogt MM, Buizer AI et al (2017) Analysis of gait patterns pre- and post-single event multilevel surgery in children with cerebral palsy by means of offset-wise movement analysis profile and linear fit method. Hum Mov Sci 55:145–155
Baker R, Mcginley JL, Schwartz M et al (2012) The minimal clinically important difference for the Gait Profile Score. Gait Posture 35:612–615
Baker R, Mcginley JL, Schwartz MH et al (2009) The gait profile score and movement analysis profile. Gait Posture 30:265–269
Barre A, Armand S (2014) Biomechanical ToolKit: open-source framework to visualize and process biomechanical data. Comput Meth Prog Bio 114:80–87
Bell KJ, Õunpuu S, Deluca PA et al (2002) Natural progression of gait in children with cerebral palsy. J Pediatr Orthop 22:677–682
Bohm H, Hosl M, Doderlein L (2017) Predictors for anterior pelvic tilt following surgical correction of flexed knee gait including patellar tendon shortening in children with cerebral palsy. Gait Posture 54:8–14
Dreher T, Thomason P, Svehlik M et al (2018) Long-term development of gait after multilevel surgery in children with cerebral palsy: a multicentre cohort study. Dev Med Child Neurol 60:88–93
Dreher T, Vegvari D, Wolf SL et al (2013) Long-term effects after conversion of biarticular to monoarticular muscles compared with musculotendinous lengthening in children with spastic diplegia. Gait Posture 37:430–435
Hof AL (1996) Scaling gait data to body size. Gait Posture 4:222–223
Kadaba MP, Ramakrishnan HK, Wootten ME (1990) Measurement of lower extremity kinematics during level walking. J Orthop Res 8:383–392
Klausler M, Speth BM, Brunner R et al (2017) Long-term follow-up after tibialis anterior tendon shortening in combination with Achilles tendon lengthening in spastic equinus in cerebral palsy. Gait Posture 58:457–462
Kuchen DB, Eichelberger P, Baur H et al (2020) Long-term follow-up after patellar tendon shortening for flexed knee gait in bilateral spastic cerebral palsy. Gait Posture 81:85–90
Lamberts RP, Burger M, Du Toit J et al (2016) A systematic review of the effects of single-event multilevel surgery on gait parameters in children with spastic cerebral palsy. PLoS ONE 11:e0164686
Levine TR, Hullett CR (2006) Eta squared, partial eta squared, and misreporting of effect size in communication research. Hum Commun Res 28:612–625
Mcginley JL, Dobson F, Ganeshalingam R et al (2012) Single-event multilevel surgery for children with cerebral palsy: a systematic review. Dev Med Child Neurol 54:117–128
Moreau N, Tinsley S, Li L (2005) Progression of knee joint kinematics in children with cerebral palsy with and without rectus femoris transfers: a long-term follow up. Gait Posture 22:132–137
Nieuwenhuys A, Papageorgiou E, Desloovere K et al (2017) Statistical parametric mapping to identify differences between consensus-based joint patterns during gait in children with cerebral palsy. PLoS ONE 12:e0169834
Nieuwenhuys A, Papageorgiou E, Pataky T et al (2016) Literature review and comparison of two statistical methods to evaluate the effect of botulinum toxin treatment on gait in children with cerebral palsy. PLoS ONE 11:e0152697
Norlin R, Tkaczuk H (1985) One-session surgery for correction of lower extremity deformities in children with cerebral palsy. J Pediatr Orthop 5:208–211
Ounpuu S, Gorton G, Bagley A et al (2015) Variation in kinematic and spatiotemporal gait parameters by Gross Motor Function Classification System level in children and adolescents with cerebral palsy. Dev Med Child Neurol 57:955–962
Ounpuu S, Solomito M, Bell K et al (2015) Long-term outcomes after multilevel surgery including rectus femoris, hamstring and gastrocnemius procedures in children with cerebral palsy. Gait Posture 42:365–372
Park MS, Chung CY, Lee SH et al (2009) Effects of distal hamstring lengthening on sagittal motion in patients with diplegia: hamstring length and its clinical use. Gait Posture 30:487–491
Pataky TC (2010) Generalized n-dimensional biomechanical field analysis using statistical parametric mapping. J Biomech 43:1976–1982
Pataky TC, Robinson MA, Vanrenterghem J (2013) Vector field statistical analysis of kinematic and force trajectories. J Biomech 46:2394–2401
Rutz E, Baker R, Tirosh O et al (2013) Are results after single-event multilevel surgery in cerebral palsy durable? Clin Orthop Relat Res 471:1028–1038
Rutz E, Gaston MS, Tirosh O et al (2012) Hip flexion deformity improves without psoas-lengthening after surgical correction of fixed knee flexion deformity in spastic diplegia. Hip Int 22:379–386
Simon-Martinez C, Jaspers E, Mailleux L et al (2017) Negative influence of motor impairments on upper limb movement patterns in children with unilateral cerebral palsy. A statistical parametric mapping study. Front Hum Neurosci 11:482
Sung KH, Chung CY, Lee KM et al (2013) Long term outcome of single event multilevel surgery in spastic diplegia with flexed knee gait. Gait Posture 37:536–541
Svehlik M, Steinwender G, Kraus T et al (2011) The influence of age at single-event multilevel surgery on outcome in children with cerebral palsy who walk with flexed knee gait. Dev Med Child Neurol 53:730–735
Terjesen T, Lofterod B, Skaaret I (2015) Gait improvement surgery in ambulatory children with diplegic cerebral palsy. Acta Orthop 86:511–517
Thomason P, Baker R, Dodd K et al (2011) Single-event multilevel surgery in children with spastic diplegia: a pilot randomized controlled trial. J Bone Jt Surg Am 93:451–460
Thomason P, Selber P, Graham HK (2013) Single event multilevel surgery in children with bilateral spastic cerebral palsy: a 5 year prospective cohort study. Gait Posture 37:23–28
Vogel-Tgetgel ND, Klausler M, Brunner R et al (2020) Short-term outcome of double-shelled braces in neuromuscular scoliosis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03600-6
Tomaszewski R, Rutz E, Mayr J et al (2020) Surgical treatment of benign lesions and pathologic fractures of the proximal femur in children. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03687-x
Acknowledgements
The authors thank the Ralf-Loddenkemper Stiftung for their financial support to this project and they thank the members of the gait analysis lab at the University Children’s Hospital Basel for their assistance in data collection and their continuous support.
Author information
Authors and Affiliations
Contributions
ER, RB, MF, NH and RV contributed to the study conception and design. Material preparation, data collection and analysis were performed by MF, NH and RV. The first draft of the manuscript was written by NH and RV, all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study, approved by the local ethical committee (EKNZ 304/08, PB_2018-00168), was conducted according to the current version of the World Medical Association Declaration of Helsinki.
Consent to participate
All participants and/or their parents gave written informed consent for the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Visscher, R., Hasler, N., Freslier, M. et al. Long-term follow-up after multilevel surgery in cerebral palsy. Arch Orthop Trauma Surg 142, 2131–2138 (2022). https://doi.org/10.1007/s00402-021-03797-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03797-0