Abstract
Background
Gait and function may deteriorate with time in patients with spastic diplegia. Single-event multilevel surgery often is performed to either improve gait or prevent deterioration. However it is unclear whether the presumed gait improvements are durable.
Questions/purposes
We therefore determined whether (1) single-event multilevel surgery improves gait in patients with spastic diplegia and (2) whether the improved function is durable.
Methods
We retrospectively reviewed the data of 14 patients with spastic diplegia. At the time of surgery, one patient had gross motor Level I function, 10 patients had Level II function, and three patients had Level III function. There were four females and 10 males with a mean age of 13 years (range, 7–18 years). The mean number of orthopaedic procedures per single-event multilevel surgery session was 7.4 ± 2.8 (median, 6.5; range, 4–15). We used instrumented gait analysis to determine joint ROM, movement analysis profiles, and the gait profile score. The minimum followup was 1 year (mean, 2 years; range, 1–3 years).
Results
At last followup, movement analysis profiles for knee flexion, for ankle dorsiflexion, and for foot progression improved as did the gait profile score. Additional surgery after the index procedure was performed in nine of the 14 patients because of relapse of the original or new gait problems. Major surgical adverse events occurred in one of the 14 patients.
Conclusions
Severe gait dysfunction in patients with spastic diplegia can be improved short-term in one operative session by single-event multilevel surgery, but to preserve the early improvements many patients require additional surgery. It is unknown whether the improvements will last for decades.
Level of evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Without intervention, gait and function in patients with spastic diplegia may deteriorate with time, especially during the pubertal growth spurt [4, 14, 22]. In one study, deterioration in gait parameters occurred in all 18 subjects after a mean followup of only 32 months [14]. In another natural history study, temporal gait parameters and gait kinematics deteriorated in all 28 patients with cerebral palsy, including 19 with spastic diplegia, seven with hemiplegia, and two with quadriplegia [4].
Management of gait dysfunction in patients with cerebral palsy may include nonoperative measures, such as physiotherapy [45], orthotics [5], casting [19], and injections of botulinum toxin type A [17]. Despite appropriate nonoperative management, however, the majority of patients with spastic diplegia will have fixed contractures and bony deformities develop which require surgical correction to maintain gait or even sitting functions. To achieve sagittal plane balance and avoid repeated episodes of surgery and rehabilitation, multiple surgical interventions may be combined in one session, known as single-event multilevel surgery [7, 23]. This approach may be particularly important to improve gait in patients with spastic diplegia [11, 12, 37].
Single-event multilevel surgery was first described by Norlin and Tkaczuk in 1985 [23] and Browne and McManus in 1987 [7]. In these studies the concept of single-event multilevel surgery was introduced and the advantages of one-session surgery such as reduction in the number of operations and, possibly, reduced chance of reoperation and complications are mentioned. Norlin and Tkaczuk reported a 5-year followup of the original cohort in 1992 [24]. They reassessed 23 subjects by means of video-analysis rather than three-dimensional (3-D) gait analysis. In their cohort none of the patients had recurrences of the deformities and they had normal growth-related development of their gaits. However, these studies predated the widespread availability of instrumented gait analysis and the development of valid functional scales. Using a combination of gait parameters and the physiologic cost index, Nene et al. [21] in 1993 reported the function of 18 patients who had single-event multilevel surgery. Improvements in a predominance of gait parameters after multilevel surgery were reported for independent [36, 40, 47] and assisted walkers [18, 46]. Thomason et al. [42] published a pilot report of the first randomized clinical trial of single-event multilevel surgery. In a subsequent report of the same study [43], Thomason et al., reported statistically significant and clinically important improvements: at 12 months after surgery they noted absence of joint contractures, correct muscle lengths and lever arms, and gait kinematics. However, functional improvements, such as Gross Motor Function Measure (GMFM66), were not seen until 2 years after surgery. These improvements in gait and function were maintained at 5 years after surgery. The most comprehensive of recent studies reporting single-event multilevel surgery is a prospective, multicenter study with a control group, performed by Gorton et al. [10]. They included a group of outcome measures, including a summary statistic of gait (the Gillette gait index) [38], a measure of gross motor function (the Gross Motor Function Classification System or GMFCS) [26], a measure of health-related quality of life, and measurements using the Pediatric Outcomes Data Collection Instrument [10]. The authors showed on the basis of a matched concurrent data set of 75 patients with spastic cerebral palsy (age 4 to 18 years), an improvement in function after 1 year for a surgical group compared with a nonsurgical group.
Instrumented clinical gait analysis consists of various combinations of kinematic, kinetic, and EMG data and is interpreted with supporting clinical data. It provides essential biomechanical data for decision-making and objective outcome assessment [9]. The movement analysis profile and gait profile score [3] were developed to provide graphic and quantitative summaries of kinematic gait data, and a single summary statistic of gait. The individual movement analysis profile domains show which gait parameters have changed and by how much. The gait profile score provides a single measure to help determine if overall gait function has improved or deteriorated. The movement analysis profile domains highlight specific gait deviations but they have not replaced detailed data interpretations required for surgical decision-making [9]. The movement analysis profile describes the magnitude of deviation of nine kinematic variables over the gait cycle. The gait profile score [3] reduces all information to one number that reflects the quality of the gait pattern with respect to normality; it is a summary statistic of gait, which quantifies the subject’s gait abnormalities relative to normative data. A higher figure indicates a more abnormal gait pattern with respect to normality, and a lower value indicates an improvement toward normal gait function. Based on an analysis of the difference in median gait profile score for patients classified at different levels of the Functional Assessment Questionnaire [25], the minimal clinically important difference for the gait profile score is 1.6° [2].
The purposes of this study were to determine whether (1) single-event multilevel surgery improved gait in patients with spastic diplegia; and (2) whether the improved function is durable.
Patients and Methods
We retrospectively studied all 14 patients with cerebral palsy and severe gait dysfunction who underwent single-event multilevel surgery between September 2004 and June 2008. Inclusion criteria were a confirmed diagnosis of spastic diplegia, GMFCS Levels I, II, or III, and ages 6 to 18 years. Prior injection of botulinum toxin A was allowed, as long as 6 months had elapsed since the last injection. Eligible subjects had to have had a preoperative gait analysis and most had short-term (ie, 1 to 3 years; n = 13) and mid-term (ie, 4 to 6 years; n = 12) followup gait studies. Exclusion criteria were a diagnosis other than cerebral palsy, dystonic or mixed movement disorder, outside the age range, and GMFCS Levels IV and V. There were four females and 10 males included in the study. They had a mean age of 13 years (median, 12.5; range, 7–18 years) at the time of preoperative 3-D gait analysis. One patient had GMFCS Level I function, 10 had Level II function, and three had Level III function. One patient had previous surgical procedures (Table 1). The mean age of the patients at the time of single-event multilevel surgery was 14 years (median, 13 years; range, 8–18 years). No patients were lost to followup. The minimum followup was 1 year (mean, 1.8 years; range, 1–3 years). No patients were recalled specifically for this study; all data were obtained from medical records. The change in the gait profile score was 10°, and this change, in relation to the minimum clinically important difference, was seven times. All patients and/or parents gave written consent for participation in the study in accordance with local ethical committee requirements. The study was performed according to the declaration of Helsinki.
Three-dimensional data were collected preoperatively for all 14 patients. One patient (Patient 10) missed the first postoperative gait analysis leaving 13 patients with short-term data at a mean followup of 2 years (range, 1–3 years). For 12 patients followup data were collected with a mean followup of 5 years (range, 4–6 years). Two patients were followed not long enough to have mid-term followup gait studies (Patients 9 and 13). The examination in our gait laboratory was performed by a physiotherapist and a human movement scientist trained in gait analysis. The clinical assessment included examining passive ROM by using a goniometer, the spasticity assessment using the Modified Ashworth Scale Instructions [6] (scale, 0–4), and the manual muscle strength test [8, 20] (scale, 0–5) of the lower limb muscles. The instrumented gait analysis included kinematics, kinetics, and dynamic EMG data using a motion capture system (6-camera Vicon 460 system™, Oxford Metrics Ltd, Oxford, UK), two force plates (Kistler Instruments AG, Winterthur, Switzerland), and an eight-channel surface EMG system (Zebris®, Tübingen, Germany). The patients walked at their self-selected speed. The Helen Hayes marker set [15] was used, and at least six trials were recorded. Anthropometric data were collected for appropriate scaling. Surface EMG readings were recorded simultaneously. Bipolar Ag/AgCl surface electrode pairs (electrode diameter 10-mm and interelectrode spacing of 22-mm) were placed bilaterally over the medial gastrocnemius, tibialis anterior, rectus femoris, and semitendinosus muscles. For electrode placement the Surface ElectroMyoGraphy for the Non-Invasive Assessment of Muscles (SENIAM) [13] recommendations for surface EMG were followed. The ground electrode was placed over the tibial tuberosity. The EMG signals were band-pass filtered (10–700 Hz) and collected at a sampling rate of 2500 Hz. All data were expressed as a percentage of gait cycle, using the Polygon software (Vicon Polygon, Oxford Metrics Ltd, Oxford, UK). From the 3-D gait data, temporal parameters (cadence, stride length, and walking speed), the movement analysis profile, and gait profile score were calculated [3]. All patients underwent at least one preoperative and one postoperative gait analysis. All data were uploaded into GaitaBase (http://gaitabase.rch.org.au) [44]. The mean interval between preoperative gait analysis and surgery was 0.8 years.
All patients had preoperative botulinum toxin test injections before muscle lengthening surgery [33]. Surgical indications were based on comprehensive biomechanical and clinical assessments, including an instrumented gait analysis and clinical and radiologic evaluations. The indications for single-event multilevel surgery were: (1) documented deterioration in gait and function during the last 12 months, (2) fixed musculoskeletal deformities (contracture, torsion, joint instability), (3) evidence from the diagnostic matrix, including 3-D gait analysis, that deformity correction at two different anatomic levels (the hip, knee, or ankle) on both sides of the body had a realistic chance of improving gait and function (Appendix 1). The contraindications were: (1) severe weakness, (2) uncontrolled spasticity or dystonia, (3) progressive neurologic disorder (eg, hereditary spastic paraparesis), (4) a patient who was unable to perform postoperative rehabilitation because of cognitive, behavioral, geographic, financial, or social factors. For the purposes of this study, single-event multilevel surgery was defined as at least one surgical procedure that was performed on two different anatomic levels (hip, knee, or ankle) on both sides of the body. The surgical procedure did not need to be symmetric and was not uniform, but individually tailored to the patient’s needs. All operations were performed with the patient receiving general anesthesia. The mean number of orthopaedic procedures was seven (median, 6.5; range, 4–15 procedures). All operative procedures were performed or supervised by the junior (ER) or senior author (RB). Perioperative antibiotics were used and postoperative epidural infusions were administered to all the patients for pain control. All patients remained as inpatients for 5 to 10 days after surgery and were discharged wearing below-the-knee plaster casts (except in case of isolated tibialis posterior lengthenings) with knee immobilizers and use of appropriate assistive devices as indicated by their GMFCS level.
The patients were first assessed 6 weeks postoperatively with radiographs to check healing of the surgical incisions and consolidation of the osteotomies and bony procedures. Custom-fitted ankle-foot orthoses were provided for all patients with surgery at the ankle level. After 6 weeks all patients followed an intensive rehabilitation program performed three to five times per week for 12 weeks or 4 to 6 weeks as inpatients in a rehabilitation center. The aim of this postoperative rehabilitation was to improve ROM, strength, balance, and function. After this time all patients had semiannual clinic visits.
Adverse events related to surgery were classified as mild if they resolved spontaneously, moderate if they resolved completely after simple treatment, or severe if there was a permanent deficit [42].
Paired data were assessed using the paired t-test and sequential data were assessed using repeated ANOVA with Bonferroni post hoc analysis (SPSS® software, Version 15.0; SSPS Inc, Chicago, IL, USA). We determined differences in walking speed, cadence, and stride length between preoperative and the two followup times using t-tests. We determined differences in each movement analysis profile and the gait profile score between the preoperative and postoperative assessments using ANOVA.
Results
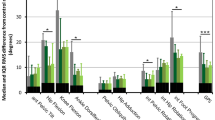
After single-event multilevel surgery there was an improvement in gait: the movement analysis profile for knee flexion, ankle dorsiflexion, and foot progression improved. The temporal parameters for baseline versus short-term postoperative gait (Table 2) are shown, and the temporal parameters for baseline versus mid-term postoperative gait were compared (Table 3). The parameters for short-term versus mid-term postoperative gait are shown (Table 4). The preoperative, short-term, and mid-term kinematics (Fig. 1), and movement analysis profile are shown (Fig. 2). The mean gait profile score improved from 20° to 13° (Table 2). The change was 7° and this change, in relation to the minimum clinically important difference, was five times. There was improvement in walking speed and stride length. The movement analysis profile for hip flexion, knee flexion, ankle dorsiflexion, and foot progression showed remarkable improvements (Table 3). The mean gait profile score improved from 21° to 11°. Nine patients (64%) had additional surgery after single-event multilevel surgery for further gait correction (Table 5) combined with plate removal (when indicated). New problems were found in five patients (Patient 1, hip flexion deformity; Patient 2, unilateral hip displacement; Patient 11, severe pes planovalgus; Patient 13, over-lengthening of the tibialis anterior tendon; Patient 14, short adductors) (Table 5), and one of the procedures needed revision because of relapses in four patients (Patients 3, 4, 7, and 8). Therefore no important changes were noted between short-term and mid-term followups (Table 4). The mean gait profile score at short-term was 13° and at mid-term 11°. The change in gait profile score was 2°, and this change, in relation to minimal clinically important difference, was two times.
These graphs illustrate the preoperative sagittal plane kinematics at the short-term and mid-term followups. The gray band is the normal reference range. The dotted line is the mean kinematic for the study group. The substantial improvements in the sagittal plane kinematic scan be seen; these are more clearly and quantitatively illustrated in Figure 2.
One patient (Patient 4) had a deep infection develop after tendoachilles lengthening. The deep infection rate was 1% for all interventions. No other complications occurred and this was the only adverse event.
Discussion
The advantages of single-event multilevel surgery for gait dysfunction in patients with spastic diplegia include less time spent in the hospital and the necessity of a single period of rehabilitation. This may result in cost savings, but we are not aware of any cost benefit analyses. The first reports of single-event multilevel surgeries had a narrow focus on safety and feasibility [7, 23, 24]. Efficacy has been established in studies [10, 18, 21, 32, 34–36, 40, 43, 46, 47] which have included gait data and functional outcomes. Most studies have lacked coherent methods to determine if specific procedures have been effective and the effectiveness of the overall single-event multilevel surgery and rehabilitation package [7, 11, 21, 24, 36, 37]. The aim of our study was to investigate (1) whether single-event multilevel surgery improved gait in patients with spastic diplegia, and (2) whether the improved function is durable. A previous study by Norlin and Tkaczuk assessed 23 subjects at the 5-year followup to determine the long-term success of single-event surgery [24]. However, their study only included video recordings as a means of assessment, whereas our results are based on gait analysis. After 5 years they did not find any recurrences. In contrast, in our study 2/3 of the patients required additional surgery because of relapses or new biomechanical problems.
Our study has numerous limitations. First, we had a small sample size of 14 patients. The indications for single-event multilevel surgery are relatively uncommon; we did include all patients who had this sort of surgery. Second, we lacked control groups of untreated patients and patients treated by nonoperative methods such as orthotics and botulinum toxin injections. Third, we had incomplete followups for some patients because one patient missed the first postoperative gait analysis and two patients did not yet have the final examination. Fourth, our findings are likely relevant only to a specific group of patients with spastic diplegia for which we established specific surgical indications. Finally, we had no measure of function. However, we note most single-event multilevel surgery outcome studies have a retrospective study design and the evidence base is limited by only one published randomized clinical trial at the moment [1, 11, 12, 30, 33, 37, 42, 43].
We found severe gait dysfunction in patients with spastic diplegia can be improved for the short-term in one operative session by single-event multilevel surgery. These findings are in accordance with reported findings [10, 11, 40, 42]. In our study the preoperative gait profile score of 20° was 5.1° higher than reported by Thomason et al. [43]. References to the kinematic graphs and surgical prescription show the procedures for correction of excessive knee flexion and equinus contributed most to the overall surgical outcomes (Fig. 1). Changes in other movement analysis profile domains were made toward improved gait except for pelvic tilt, which increased only slightly (Fig. 2). Increased anterior tilt was a negative outcome of one study of single-event multilevel surgery, and more work is required to further reduce this problem [18]. It also may be that study was underpowered and could not detect noteworthy changes in some of the movement analysis profile domains. The mean age (13.6 years) of the patients at the time of the single-event multilevel surgery in our cohort was older than patients in other studies (mean, 6.4 [12], 12.0 [16], and 8.5 years [26]). The mean interval of our study (0.8 years) between the first gait analysis and surgery was comparable to the interval reported by Gough et al. (0.7 years) [12]. The surgical complication rate of 1.1% in our series was lower than that reported by Rodda et al. (10 surgical complications in four of 10 patients) [28].
The need for additional procedures after single-event multilevel surgery for treatment of spastic diplegia was first reported by Aiona and Sussman [1, 41]. After short-term followup in our gait laboratory, nine patients had additional surgeries after single-event multilevel surgery for further gait corrections (Table 5), combined with plate removal (when indicated). In our study, additional surgery was indicated for 2/3 of the patients because of relapses (n = 4) or new problems (n = 5). This number of additional surgeries is similar to that of Thomason et al. [43], who reported 22 subsequent surgeries were needed in 12 patients. A reduction in gait profile score from 20.7° to 11.1° at mid-term followup indicated 47% improvement toward normal gait; major improvements in the movement analysis profile for hip flexion, knee flexion, ankle dorsiflexion, and foot progression contributed to this. It probably is unrealistic to expect a single episode of surgery to provide lasting correction of all musculoskeletal problems and enhance and preserve gait function in all patients with spastic diplegia. It also may not be appropriate to focus on a single-event paradigm in all subjects. Staging surgery (and offering revision surgery when necessary) in this study achieved 47% improvement toward normal gait, but to preserve the early improvements 2/3 of our patients required additional surgery. In our study, the gait profile score was used to measure the overall gait disorder. The median value of the gait profile score for healthy patients is 5.2°. The improvement in our patients represents reductions of 47% (from preoperative to short-term), 62% (from preoperative to mid-term), and 31% (from short-term to mid-term) in the difference between abnormal and healthy gait patterns. The gait profile score [3] can be calculated independently of the feature analysis on which the gait deviation index is based [3, 39]. The movement analysis profile summarizes much of the complex information contained in the kinematic data and shows which parameters contributed to the change of gait. Measuring the outcomes of surgery in patients with cerebral palsy is difficult. Other factors such as the motivation of each patient and their abilities to participate in the postoperative rehabilitation program are likely to be important, although these are more difficult to quantify.
Single-event multilevel surgery, including lengthening of the contracted agonist, antagonist shortening [29], and selected bony procedures with stable fixation [30–32], improves gait dysfunction in patients with spastic diplegia. To preserve early improvements however, 2/3 of our patients required additional surgery because of relapses or new problems. It is unknown whether the improvements will last for decades.
References
Aiona MD, Sussman MD. Treatment of spastic diplegia in patients with cerebral palsy: Part II. J Pediatr Orthop B. 2004;13:S13–38.
Baker R, McGinley JL, Schwartz M, Thomason P, Rodda J, Graham HK. The minimal clinically important difference for the Gait Profile Score. Gait Posture. 2012;35:612–615.
Baker R, McGinley JL, Schwartz MH, Beynon S, Rozumalski A, Graham HK, Tirosh O. The gait profile score and movement analysis profile. Gait Posture. 2009;30:265–269.
Bell KJ, Ounpuu S, DeLuca PA, Romness MJ. Natural progression of gait in children with cerebral palsy. J Pediatr Orthop. 2002;22:677–682.
Bennett BC, Russell SD, Abel MF. The effects of ankle foot orthoses on energy recovery and work during gait in children with cerebral palsy. Clin Biomech (Bristol, Avon). 2012;27:287–291.
Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67:206–207.
Browne AO, McManus F. One-session surgery for bilateral correction of lower limb deformities in spastic diplegia. J Pediatr Orthop. 1987;7:259–261.
Cuthbert SC, Goodheart GJ Jr. On the reliability and validity of manual muscle testing: a literature review. Chiropr Osteopat. 2007;15:4.
Gage JR. Gait analysis: an essential tool in the treatment of cerebral palsy. Clin Orthop Relat Res. 1993;288:126–134.
Gorton GE 3rd, Abel MF, Oeffinger DJ, Bagley A, Rogers SP, Damiano D, Romness M, Tylkowski C. A prospective cohort study of the effects of lower extremity or orthopaedic surgery on outcome measures in ambulatory children with cerebral palsy. J Pediatr Orthop. 2009;29:903–909.
Gough M, Eve LC, Robinson RO, Shortland AP. Short-term outcome of multilevel surgical intervention in spastic diplegic cerebral palsy compared with the natural history. Dev Med Child Neurol. 2004;46:91–97.
Gough M, Schneider P, Shortland AP. The outcome of surgical intervention for early deformity in young ambulant children with bilateral spastic cerebral palsy. J Bone Joint Surg Br. 2008;90:946–951.
Hermens HJ, Freriks B, Merletti R, Stegeman D, Blok J, Rau G, et al. European Recommendations for Surface Electromyography (SENIAM). Enschede Roessingh Research and Development. Available at: http://seniam.org/. Accessed October 17, 2012.
Johnson DC, Damiano DL, Abel MF. The evolution of gait in childhood and adolescent cerebral palsy. J Pediatr Orthop. 1997;17:392–396.
Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392.
Khan MA. Outcome of single-event multilevel surgery in untreated cerebral palsy in a developing country. J Bone Joint Surg Br. 2007;89:1088–1091.
Love SC, Novak I, Kentish M, Desloovere K, Heinen F, Molenaers G, O’Flaherty S, Graham HK; Cerebral Palsy Institute. Botulinum toxin assessment, intervention and after-care for lower limb spasticity in children with cerebral palsy: international consensus statement. Eur J Neurol. 2010;17(suppl 2):9–37.
Ma FY, Selber P, Nattrass GR, Harvey AR, Wolfe R, Graham HK. Lengthening and transfer of hamstrings for a flexion deformity of the knee in children with bilateral cerebral palsy: technique and preliminary results. J Bone Joint Surg Br. 2006;88:248–254.
McNee AE, Will E, Lin JP, Eve LC, Gough M, Morrissey MC, Shortland AP. The effect of serial casting on gait in children with cerebral palsy: preliminary results from a crossover trial. Gait Posture. 2007;25:463–468.
Mendell JR, Florence J. Manual muscle testing. Muscle Nerve. 1990;13(suppl):S16–20.
Nene AV, Evans GA, Patrick JH. Simultaneous multiple operations for spastic diplegia: outcome and functional assessment of walking in 18 patients. J Bone Joint Surg Br. 1993;75:488–494.
Norlin R, Odenrick P. Development of gait in spastic children with cerebral palsy. J Pediatr Orthop. 1986;6:674–680.
Norlin R, Tkaczuk H. One-session surgery for correction of lower extremity deformities in children with cerebral palsy. J Pediatr Orthop. 1985;5:208–211.
Norlin R, Tkaczuk H. One session surgery on the lower limb in children with cerebral palsy: a five year follow-up. Int Orthop. 1992;16:291–293.
Novacheck TF, Stout JL, Tervo R. Reliability and validity of the Gillette Functional Assessment Questionnaire as an outcome measure in children with walking disabilities. J Pediatr Orthop. 2000;20:75–81.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–223.
Robb JE, Brunner R. A Dega-type osteotomy after closure of the triradiate cartilage in non-walking patients with severe cerebral palsy. J Bone Joint Surg Br. 2006;88:933–937.
Rodda JM, Graham HK, Nattrass GR, Galea MP, Baker R, Wolfe R. Correction of severe crouch gait in patients with spastic diplegia with use of multilevel orthopaedic surgery. J Bone Joint Surg Am. 2006;88:2653–2664.
Rutz E, Baker R, Tirosh O, Romkes J, Haase C, Brunner R. Tibialis anterior tendon shortening in combination with Achilles tendon lengthening in spastic equinus in cerebral palsy. Gait Posture. 2011;33:152–157.
Rutz E, Brunner R. The pediatric LCP hip plate for fixation of proximal femoral osteotomy in cerebral palsy and severe osteoporosis. J Pediatr Orthop. 2010;30:726–731.
Rutz E, Gaston MS, Camathias C, Brunner R. Distal femoral osteotomy using the LCP pediatric condylar 90-degree plate in patients with neuromuscular disorders. J Pediatr Orthop. 2012;32:295–300.
Rutz E, Gaston MS, Tirosh O, Brunner R. Hip flexion deformity improves without psoas-lengthening after surgical correction of fixed knee flexion deformity in spastic diplegia. Hip Int. 2012;22:379–386.
Rutz E, Hofmann E, Brunner R. Preoperative botulinum toxin test injections before muscle lengthening in cerebral palsy. J Orthop Sci. 2010;15:647–653.
Rutz E, Passmore E, Baker R, Graham HK. Multilevel surgery improves gait in spastic hemiplegia but does not resolve hip dysplasia. Clin Orthop Relat Res. 2012;470:1294–1302.
Rutz E, Tirosh O, Thomason P, Barg A, Graham HK. Stability of the Gross Motor Function Classification System after single event multi level surgery in cerebral palsy. Dev Med Child Neurol. 2012;Oct 16. [Epub ahead of print].
Saraph V, Zwick EB, Auner C, Schneider F, Steinwender G, Linhart W. Gait improvement surgery in diplegic children: how long do the improvements last? J Pediatr Orthop. 2005;25:263–267.
Saraph V, Zwick EB, Zwick G, Steinwender C, Steinwender G, Linhart W. Multilevel surgery in spastic diplegia: evaluation by physical examination and gait analysis in 25 children. J Pediatr Orthop. 2002;22:150–157.
Schutte LM, Narayanan U, Stout JL, Selber P, Gage JR, Schwartz MH. An index for quantifying deviations from normal gait. Gait Posture. 2000;11:25–31.
Schwartz MH, Rozumalski A. The Gait Deviation Index: a new comprehensive index of gait pathology. Gait Posture. 2008;28:351–357.
Schwartz MH, Viehweger E, Stout J, Novacheck TF, Gage JR. Comprehensive treatment of ambulatory children with cerebral palsy: an outcome assessment. J Pediatr Orthop. 2004;24:45–53.
Sussman MD, Aiona MD. Treatment of spastic diplegia in patients with cerebral palsy. J Pediatr Orthop B. 2004;13:S1–12.
Thomason P, Baker R, Dodd K, Taylor N, Selber P, Wolfe R, Graham HK. Single-event multilevel surgery in children with spastic diplegia: a pilot randomized controlled trial. J Bone Joint Surg Am. 2011;93:451–460.
Thomason P, Selber P, Graham HK. Single Event Multilevel Surgery in children with bilateral spastic cerebral palsy: a 5 year prospective cohort study. Gait Posture. 2012 Jul 18. [Epub ahead of print].
Tirosh O, Baker R, McGinley J. GaitaBase: Web-based repository system for gait analysis. Comput Biol Med. 2010;40:201–207.
van Wely L, Becher JG, Balemans AC, Dallmeijer AJ. Ambulatory activity of children with cerebral palsy: which characteristics are important? Dev Med Child Neurol. 2012;54:436–442.
Yngve DA, Scarborough N, Goode B, Haynes R. Rectus and hamstring surgery in cerebral palsy: a gait analysis study of results by functional ambulation level. J Pediatr Orthop. 2002;22:672–676.
Zwick EB, Saraph V, Strobl W, Steinwender G. [Single event multilevel surgery to improve gait in diplegic cerebral palsy: a prospective controlled trial][in German]. Z Orthop Ihre Grenzgeb. 2001;139:485–489.
Acknowledgments
We thank Mary Sheedy and H. Kerr Graham, MD, FRCS (Ed), FRACS for help with preparation of this manuscript. In addition we thank Alejandra Speiser for help in copyediting the final version of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Murdoch Childrens Research Institute, Victoria, Australia
Appendix 1. The Basle Concept for Single-event Multilevel Surgery in Cerebral Palsy
Appendix 1. The Basle Concept for Single-event Multilevel Surgery in Cerebral Palsy
Demographics and surgical prescription for each patient
-
1.
Based on instrumented three-dimensional gait analysis
-
2.
Preoperative botulinum toxin test injections in all muscles planned for lengthening
-
3.
Single-event multilevel surgery:
-
Bilateral simultaneous surgical correction of all bony and soft tissue deformities
-
Individual procedures
-
Calcaneal lengthening osteotomy (Evans) or calcaneocuboid fusion with lengthening were performed in patients with clinical and radiologic evidence of a midfoot break, depending on stability of the Chopart joint.
-
Fixed equinus deformities (involving gastrocnemius and soleus) were managed by open Z-lengthening of the Achilles tendon.
-
In patients with excessively long triceps surae, the Achilles tendon was shortened by open plication.
-
In patients with clinical and kinematic evidence of deficient tibialis anterior function, the tendon was shortened by fixing the tendon at the ankle level and pulling it down to the insertion.
-
In patients with spastic equinovarus deformities attributable to documented tibialis posterior over-activity, the tibialis posterior was lengthened by open Z-lengthening below the medial malleolus.
-
When the fixed flexion deformity at the knee was less than 25°, distal medial hamstring lengthening and supracondylar extension osteotomy were performed.
-
When the fixed flexion deformity at the knee exceeded 25°, distal medial hamstring lengthening was performed 3 months before single-event multilevel surgery to avoid late recurvatum in gait.
-
When the fixed flexion deformity at the knee exceeded 40° and/or the knee extension lag was greater than 10°, patellar tendon shortening was performed.
-
When there was radiologic evidence of hip subluxation (a migration percentage greater than 30%) with coexisting acetabular dysplasia, reconstructive hip surgery was performed, including femoral varus derotation osteotomy and a modification of the peri-ilial pelvic osteotomy [27]. This was done before single-event multilevel surgery to avoid an overly long surgical session.
-
Fixed flexion deformity at the hip was considered secondary to walking in crouch gait and knee flexion and was not corrected primarily but allowed to resolve gradually during the rehabilitation period.
-
4.
Rehabilitation
-
Reconstructive surgery at the foot and ankle level was managed by below knee cast immobilization for 6 weeks.
-
Acute shortening of the knee extensor mechanism was treated with 6 weeks immobilization in extension in a knee brace, limiting flexion to less than 40°.
-
Rotational osteotomies of the femur and tibia were fixed with LCP plates, allowing for early mobilization and weightbearing.
-
At 6 weeks postoperative, a 4- to 6-week period of inpatient rehabilitation was provided, including gait training, mobilization, and strengthening, or an intensive rehabilitation program with at least three sessions of physiotherapy every week was provided.
-
-
5.
Short-term results (1 to 3 years followup)
Before removal of fixation plates, another three-dimensional gait analysis was performed to judge the effectiveness of the original intervention and to detect unresolved gait issues or new problems.
-
6.
Second operative intervention
-
Removal of fixation plates and any additonal procedures as required
-
-
7.
Mid-term result (4–6 years after surgery)
-
A full biomechanical assessment, including instrumented three-dimensional gait analysis.
-
About this article
Cite this article
Rutz, E., Baker, R., Tirosh, O. et al. Are Results After Single-event Multilevel Surgery in Cerebral Palsy Durable?. Clin Orthop Relat Res 471, 1028–1038 (2013). https://doi.org/10.1007/s11999-012-2766-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2766-9