Abstract
Purpose
The biomechanical impact of undergoing a single-event multilevel surgery (SEMLS) for children with cerebral palsy (CP) presenting an intoeing gait pattern has been widely documented. However, past studies mostly focused on gait quality rather than efficiency. Thus, there is a need to determine the impact of undergoing a SEMLS on gait quality and efficiency in children with CP presenting an intoeing gait pattern.
Methods
Data from 16 children with CP presenting an intoeing gait pattern who underwent a SEMLS were retrospectively selected. Gait kinematics was quantified before (baseline) and at least 1 year after the surgery (follow-up). Gait quality was investigated with the Gait Profile Score (GPS), hip internal rotation angle and foot progression angle (FPA). Gait efficiency was analysed using clinically accessible variables, namely the normalised gait speed and medio-lateral and vertical centre of mass excursions (COMp). Dependent variables were compared between sessions with paired t-tests.
Results
At the follow-up, children with CP exhibited a more outward FPA and GPS as well as a decreased hip internal rotation angle. No changes in normalised gait speed and vertical COMp excursion were observed, and medio-lateral COMp excursion was slightly decreased.
Conclusion
Children with CP presenting an intoeing gait pattern who underwent a SEMLS exhibited an increased gait quality, but gait efficiency was only minimally improved at the follow-up compared to baseline. Further studies are needed to identify contributors of gait efficiency in children with CP, and the best treatment modalities to optimise both their gait quality and efficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral palsy (CP) is the most common cause of motor disability in children in Europe [1] affecting between 1.5 and 3 per 1000 births [2]. CP is characterised by permanent motor disorders attributed to non-progressive disturbances in the developing brain [3]. Individuals with CP exhibit many physical impairments known to diminish gait abilities, such as loss of selective motor control [4], bony deformities [5], muscle weakness [6] and spasticity [7]. Thus, since several decades, clinical gait analysis (CGA) provides objective useful information about the gait of the ambulatory patients with CP [8]. Lots of studies showed diminished gait quality for children with CP as highlighted by a greater step width, trunk and pelvis movements and smaller step length and knee range of motion compared to healthy counterparts [9]. Among the reported interventions to improve this diminished gait quality, the single-event multilevel surgery (SEMLS), defined as a single operative event aiming to correct soft tissue and/or bone deformities at two or more anatomical levels of one or both lower limbs, is considered the standard care [10]. To further reduce the internal rotation profile of the lower limbs, the SEMLS can include a femoral derotational osteotomy (FDO), conducted either at the intertrochanteric or subtrochanteric level (proximal FDO), or at the supracondylar level (distal FDO) [10]. Within this context, the SEMLS aims to correct the static and dynamic contributors of the gait impairments, namely the excessive femoral anteversion [11], the muscle weakness [6], spasticity and contracture [7].
From CGA, several biomechanical outcomes (i.e. kinematics and kinetics) and gait scores (e.g. Gait Profile Score (GPS)) summarising the gait quality of patients with CP can be calculated to evaluate the treatments’ effects [12]. These scores are often considered as the main outcome for clinical studies evaluating treatments [8]. However, even though these scores reflect the overall gait quality, they may not be optimal to determine its efficiency, defined as the amount of energy that is used to do mechanical work on the body’s centre of mass (COM) from a given metabolic energy supply [13]. Analysing gait efficiency could be useful to evaluate the real-life impact of undergoing a SEMLS, especially as children with CP present a low efficiency conversion of metabolic energy into useful COM work and consequently have a 31% lower gait efficiency than their healthy counterparts [13]. However, the results of previous studies on the effects of undergoing a SEMLS on gait efficiency are scarce and contradictory. For example, at the 1-year follow-up after a SEMLS, children with CP exhibit decreased oxygen consumption during gait but no changes in efficiency of work production [14]. Most importantly, calculating the metabolic energy supply in clinical contexts is challenging. Thus, previous studies used biomechanical outcomes, easily implemented by clinicians, such as COM displacement [15] and gait speed [16] to indirectly estimate gait efficiency as a surrogate.
Among the impairments of children with CP, intoeing gait is observed in more than 60% [17]. This foot position during gait, assessed with the foot progression angle (FPA) during CGA, seems to be generated by greater hip internal rotation to compensate for the decreased abductor level arm in the frontal plane induced by excessive femoral anteversion [11]. Also, the intoeing gait allows reducing the degrees of freedom of the lower limb joints in order to facilitate the forward propulsion [11]. Even though the prevalence of intoeing gait decreases with growth, numerous cases do not resolve spontaneously [17], and many children with CP undergo a SEMLS that may include a derotational osteotomy at the femur and/or tibia level to improve gait quality [18] with good long-term outcomes [8]. Within this context, the SEMLS aims to correct the static and/or the dynamic contributors of gait impairments, namely the excessive femoral anteversion [11], muscle weakness [6], spasticity and contracture [7]. The increased hip abductor moment may take more than 3 years to be observed after undergoing these surgical procedures [19].
However, the improvement of gait quality could perhaps be at the expense of gait efficiency as the SEMLS could remove the biomechanical compensations used by children with CP. Thus, there is a need to better understand the impact of undergoing a SEMLS on both gait quality and gait efficiency in children with CP. Improving our knowledge on gait quality and efficiency could allow better clinical care for this population when surgically addressing their gait abnormalities.
The objective of this study was to investigate the impact of undergoing a SEMLS on gait quality and efficiency in children with CP presenting an intoeing gait pattern. It was hypothesised that the intoeing gait pattern observed in children with CP is an adaptation to allow a more efficient gait pattern. Consequently, undergoing a SEMLS will improve gait quality at the expense of efficiency.
Methods
This longitudinal retrospective study included part of the data available in the current CP cohort of the Willy Taillard Laboratory of Kinesiology, Geneva University Hospitals, Switzerland. Gait quality and efficiency analyses of children with ambulant CP were carried using two CGA time points, before and after a SEMLS. The present study was approved by the local ethics committee.
Patients
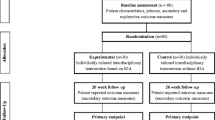
Sixteen children with CP, who were treated with a SEMLS to correct an intoeing gait pattern between 2000 and 2020, were included in this study (see Fig. 1). The inclusion criteria were the following: (1) diagnosis of CP; (2) a SEMLS approach was used on an individual basis and included a derotational osteotomy at the distal or proximal aspect of the femur/tibia and/or soft tissue procedures; (3) CGA was performed before (baseline) and at least 1 year after undergoing the SEMLS procedure (follow-up); (4) age under 18 at the time of the surgery; (5) categorised as level I or II to the Gross Motor Function Classification System (GMFCS) at the time of the surgery; (6) intoeing gait (FPA < 0°) and (7) walking without external aids.
The exclusion criteria were a past history of surgery to the lower limbs, subluxed hips, a previous selective rhizotomy or injections of botulinum toxin A less than 6 months before the baseline data collection and additional surgeries between CGA. Medical charts of all eligible participants were analysed, and demographic data were extracted from electronic medical records: age, sex, height, weight, body mass index (BMI) average follow-up period, GMFCS scores and surgical procedure specificities.
Surgical procedure
All femoral osteotomies were subtrochanteric and internally fixed with plates or intramedullary nail when growth plates were closed. The intraoperative amount of derotation was monitored with K-wires placed proximal and distal to the osteotomy and measured with a goniometer. Internal hip rotation was limited to 30°. Postoperative care consisted of early mobilization with light weight-bearing as soon as possible if only femur osteotomy was done. If knee or foot surgery was added, knee and foot immobilisation for 6 weeks without weight bearing was prescribed. Rehabilitation consisted of intensive physiotherapy sessions, 3 to 4 times a week. No complications related to the femoral derotation were reported.
Objective gait assessment
Before 2008, a six-camera motion analysis system (VICON 460; Vicon-Peak, Oxford, UK) set at a sampling frequency of 50 Hz was used to collect whole-body kinematic data during CGA. Between 2008 and 2015, a 12-camera motion analysis system (VICON Mx3 ViconPeak, Oxford, UK) set at a sampling frequency of 100 Hz was used to collect data. After 2015, a 12-camera motion analysis system (Qualisys Oqus7 + , Gothenburg, Sweden) set at a sampling frequency of 100 Hz was used. For all data collection sessions, a total of 34 retroreflective markers, aligned to anatomical landmarks on the head, trunk, arms, pelvis, thighs, shanks and feet, were positioned on each participant according to the Conventional Gait Model [20]. Participants were asked to walk barefoot at a self-selected speed. Up to eight trials per participant were averaged and used for the analyses. All available trials were used in the analyses in order to decrease the intra-individual variability of the biomechanical outcomes. PyCGM2 [21] and open-source Biomechanical ToolKit [22] were used for data analyses.
Biomechanical outcomes
The dependent variables used to analyse gait quality during the stance phase were: mean FPA, FPA at initial contact (IC), mean hip internal rotation angles, hip internal rotation angles at IC and GPS. Negative values for the FPA angles refer to internal rotation, and decreased GPS should be interpreted as an improvement of gait quality. The minimal clinically important difference for the GPS is 1.60° [23]. Gait variable scores [12] are calculated and reported as descriptive data in Table 1.
Dependent variables used to analyse gait efficiency were: gait speed (normalised to leg length) [24], medio-lateral (ML) and vertical excursion of the COM (normalised to leg length and expressed as a percentage). ML and vertical displacement of the sacral marker were used as a proxy to quantify COM movements (COMp) [25]. When the patients underwent bilateral SEMLS procedures, the lower limb that presented the most inward FPA at baseline was used in the data analyses, as pooling data from both lower limbs could induce statistical problems [26].
Statistical analysis
The normality of the demographic and biomechanical outcomes was assessed with Shapiro–Wilk’s tests. To compare the outcomes at baseline and at the follow-up, paired t-tests were performed, and Cohen’s d effect sizes and bootstraps mean differences’ 95% confidence intervals were calculated. Pearson’s correlations were computed to assess relationships between GPS change and GPS at baseline, gait speed change and gait speed at baseline, ML COMp excursion change and ML COMp excursion at baseline as well as vertical COMp excursion change and vertical COMp excursion at baseline. Pearson’s correlations were also computed to assess relationships between age and change in GPS, gait speed, ML and vertical COMp excursions. Correlation coefficients between 0 and 0.3 were considered weak, 0.3 and 0.5 were fair, 0.5 and 0.7 were good and > 0.7 were high [27]. The level of statistical significance was set at p < 0.05. All analyses were implemented in IBM SPSS (version 27.0.0.1, SPSS Inc., Chicago, Illinois, USA).
Results
Patient characteristics
At the follow-up, height (157.0 ± 16.5 cm vs 144.9 ± 19.1 cm, p = 0.009) was increased compared to baseline, but no statistically significant difference was observed for mass (47.5 ± 15.5 kg vs 39.2 ± 14.6 kg, p = 0.058) and BMI (18.0 ± 3.5 kg/m2 vs 18.8 ± 3.8 kg/m2, p = 0.318). The mean follow-up time was 39.9 ± 30.1 months (see Table 2). Individualised information and surgical procedures undergone by each participant are available in Supplementary material.
Gait quality outcomes
At the follow-up, children with CP exhibited a more external mean FPA (5.65 ± 8.30° vs − 10.54 ± 8.15°, p = 0.001) and FPA at IC (6.81 ± 8.36° vs − 9.05 ± 7.77°, p = 0.001) compared to baseline. They also exhibited decreased GPS (9.55 ± 2.68° vs 12.85 ± 3.13°, p = 0.001). Out of 16 children with CP, 15 exhibited a decreased GPS with 10 reaching the minimal clinically important difference (> 1.60°). Children with CP also exhibited a decreased hip internal rotation at IC (− 6.39 ± 12.57° vs 3.94 ± 13.17°, p = 0.037) at the follow-up. No difference was observed for mean hip internal rotation (2.57 ± 12.05° vs 9.82 ± 13.57°, p = 0.118) at the follow-up.
Gait efficiency outcomes
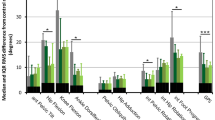
At the follow-up, ML COMp excursion (6.12 ± 1.23% vs 7.01 ± 1.42%, p = 0.014) was decreased compared to baseline. No differences in normalised gait speed (0.37 ± 0.07 vs 0.39 ± 0.07, p = 0.506) and vertical COMp excursion (5.96 ± 1.38% vs 7.59 ± 3.54%, p = 0.201) were observed at the follow-up compared to baseline. A summary of all biomechanical findings are given in Table 3. FPA and hip rotation curves as well as ML and vertical COMp displacement and interaction are displayed in Fig. 2.
Correlations
Pearson’s correlation coefficients showed significant negative correlations between GPS change and GPS at baseline (r = 0.62, p = 0.011), normalised gait speed change and normalised speed at baseline (r = − 0.57, p = 0.02), ML COMp excursion change and ML COMp excursion at baseline (r = − 0.58, p = 0.019) as well as vertical COMp excursion change and vertical COMp excursion at baseline (r = − 0.92, p < 0.001).
Pearson’s correlation coefficient showed non-significant correlations between GPS change (r = 0.11, p = 0.694), normalised speed change (r = 0.32, p = 0.231), ML COMp excursion change (r = − 0.13, p = 0.630) and age at baseline. Vertical COMp excursion change was positively correlated with age at baseline (r = 0.51, p = 0.043).
Discussion
Our findings do not confirm our hypothesis that undergoing a SEMLS will improve gait quality at the expense of efficiency. The changes in biomechanical outcomes demonstrate that the overall gait quality improves after undergoing a SEMLS in children with CP presenting an intoeing gait pattern as highlighted by the decreased GPS. This score compares the gait quality of an individual with the average walking pattern of healthy counterparts [12]. In our study, children with CP had a lower GPS (− 3.30°) at the follow-up compared to the baseline data collection session. This difference is over the minimal clinically important difference of 1.60° [23] and, as the Cohen’s d effect size of the difference was strong (d = − 1.11), our results suggest that the gait quality of children with CP is statistically and clinically improved after undergoing a SEMLS. The correlation analyses also revealed that greater GPS at baseline were associated with greater improvement at the follow-up (r = 0.62, p = 0.011), as was already reported by Bonnefoy-Mazure et al. [8]. Furthermore, as the participants presented an intoeing gait pattern at baseline, this study also focused on their lower limb rotational profile to evaluate gait quality changes after undergoing a SEMLS. The mean FPA progressed from 10.54° (± 8.15) inward to 5.65° (± 8.30) outward at the follow-up, which falls into the normality range of 4 to 12° outward [28]. This is consistent with previous results also showing a more outward FPA during gait after undergoing a SEMLS [18]. Our study showed that the improvement in FPA seems driven by a decreased hip internal rotation at IC (10.33°) which is consistent with previous results [29, 30].
Even though the gait quality was improved after undergoing a SEMLS for children with CP, the improvement in gait efficiency, assessed with gait speed and COMp displacement, was minimal. No change in normalised gait speed was observed at the follow-up which is consistent with previous results with a similar follow-up time [16]. This result is worrisome as gait speed typically increases with age in normally developing children [31]. However, as no control group was included in our study, we are not able to determine the effects of time on gait speed for our participants. The correlation analyses revealed that greater gait speeds at baseline were associated with smaller changes in gait speed (r = − 0.57, p = 0.02) and that greater ML (r = − 0.58, p = 0.019) and vertical (r = − 0.92, p < 0.001) COMp excursion at baseline were associated with greater decreases after undergoing the SEMLS. These results suggest that children with CP with a less efficient gait would benefit more from undergoing a SEMLS compared to those with a more efficient gait, which is consistent with previous results [32]. Vertical COMp displacement seems less likely to improve in older children. Also, no changes in vertical COMp displacement and only a small improvement in ML COMp displacement (− 0.88%) were found at the follow-up (see the interaction between these two variables in Fig. 2). These suggest that the gait efficiency only slightly improves after undergoing a SEMLS, especially as the mechanical work performed during gait seems mainly associated with the vertical displacement of the COM in children with CP [15]. It is still unclear to what extent a slight decrease in ML COMp displacement without changes in vertical COMp displacement will translate into clinically significant improvements of gait efficiency in children with CP. Thus, further studies should focus on determining gait biomechanical parameters that are significant contributors of gait efficiency improvements (physiological and biomechanical) and patient-reported outcomes in children with CP after undergoing a SEMLS in order to ultimately inform the development of better treatment modalities. Improving gait quality and gait efficiency is crucial as gait performance in ambulatory children with CP is associated with the physical domain of the quality of life [33] and most importantly, physical activity is a key predictor of happiness and quality of life for these children [34].
Treatments of children with CP based on CGA seek to normalise their gait relative to healthy counterparts even though their impairments are irreversible. Instead, it would be preferable to seek the best possible treatment according to these impairments. Also, some adaptations are seen as gait impairments when they are in fact effective compensations to maintain adequate gait efficiency. For example, internal rotation of the lower limbs could reduce gait complexity (e.g. fewer degrees of freedom, progress of the step easier to manage) and may be an advantage for efficiency [11]. A challenge for those taking care of these patients based on the results of the CGA will be to maintain the beneficial adaptations and address the deleterious impairments. Some adaptations could likely be beneficial in the short term and detrimental in the long term. Thus, the compromise between quality and efficiency will have to be found for each patient, taking into account their expectations and long-term development.
There are limitations to consider when interpreting the results of this study. Inherently to its retrospective design, the first limitation is the heterogeneity of the patients’ demographic data (age, time between the baseline and the follow-up, surgical specificities). However, the results will be relevant to clinicians also dealing with a heterogeneous patient base. A prospective design using the same follow-up time and more homogeneous surgical specificities across participants would significantly decrease the variability of the biomechanical outcomes. The second limitation is the lack of consensus on the definition of gait quality and gait efficiency, affecting the external validity of our results. The third limitation is the relatively small sample size in our study. The fourth limitation is related to the utilisation of the Conventional Gait Model to calculate the hip and knee internal rotations during gait. Previous results showed that the reproducibility of these measures could be problematic during CGA [35].
Conclusions
Children with CP presenting an intoeing gait pattern who underwent a SEMLS exhibited an increased gait quality, but gait efficiency, assessed with COMp displacement and speed, was only minimally improved at the follow-up. Even though their gait pattern is more normal after undergoing a SEMLS, the children with CP may still need substantial effort and energy to move forward. Further studies are needed to identify the best treatment modalities with the objective to optimise gait quality but also efficiency.
References
Sellier E, Platt MJ, Andersen GL, Krageloh-Mann I, De La Cruz J, Cans C (2016) Decreasing prevalence in cerebral palsy: a multi-site European population-based study, 1980 to 2003. Dev Med Child Neurol 58:85–92
Oskoui M, Coutinho F, Dykeman J, Jette N, Pringsheim T (2013) An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 55:509–519
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B (2007) A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl 109:8–14
Chruscikowski E, Fry NRD, Noble JJ, Gough M, Shortland AP (2017) Selective motor control correlates with gait abnormality in children with cerebral palsy. Gait Posture 52:107–109
Lee KM, Chung CY, Sung KH, Kim TW, Lee SY, Park MS (2013) Femoral anteversion and tibial torsion only explain 25% of variance in regression analysis of foot progression angle in children with diplegic cerebral palsy. J Neuroeng Rehabil 10:56
Neyroud D, Armand S, De Coulon G, Sarah RDDS, Maffiuletti NA, Kayser B, Place N (2017) Plantar flexor muscle weakness and fatigue in spastic cerebral palsy patients. Res Dev Disabil 61:66–76
Beckung E, Hagberg G, Uldall P, Cans C (2008) Probability of walking in children with cerebral palsy in Europe. Pediatrics 121:e187–e192
Bonnefoy-Mazure A, De Coulon G, Lascombes P, Armand S (2020) Follow-up of walking quality after end of growth in 28 children with bilateral cerebral palsy. J Child Orthop 14:41–49
Malone A, Kiernan D, French H, Saunders V, O’brien T, (2015) Do children with cerebral palsy change their gait when walking over uneven ground? Gait Posture 41:716–721
Niklasch M, Boyer ER, Novacheck T, Dreher T, Schwartz M (2018) Proximal versus distal femoral derotation osteotomy in bilateral cerebral palsy. Dev Med Child Neurol 60:1033–1037
Arnold AS, Komattu AV, Delp SL (1997) Internal rotation gait: a compensatory mechanism to restore abduction capacity decreased by bone deformity. Dev Med Child Neurol 39:40–44
Baker R, McGinley JL, Schwartz MH, Beynon S, Rozumalski A, Graham HK, Tirosh O (2009) The Gait Profile Score and movement analysis profile. Gait Posture 30:265–269
Ries AJ, Schwartz MH (2018) Low gait efficiency is the primary reason for the increased metabolic demand during gait in children with cerebral palsy. Hum Movement Sci 57:426–433
Marconi V, Hachez H, Renders A, Docquier P-L, Detrembleur C (2014) Mechanical work and energy consumption in children with cerebral palsy after single-event multilevel surgery. Gait Posture 40:633–639
Bennett BC, Abel MF, Wolovick A, Franklin T, Allaire PE, Kerrigan DC (2005) Center of mass movement and energy transfer during walking in children with cerebral palsy. Arch Phys Med Rehabil 86:2189–2194
Dreher T, Vegvari D, Wolf SI, Geisbusch A, Gantz S, Wenz W, Braatz F (2012) Development of knee function after hamstring lengthening as a part of multilevel surgery in children with spastic diplegia: a long-term outcome study. J Bone Joint Surg Am 94:121–130
Rethlefsen SA, Blumstein G, Kay RM, Dorey F, Wren TA (2017) Prevalence of specific gait abnormalities in children with cerebral palsy revisited: influence of age, prior surgery, and Gross Motor Function Classification System level. Dev Med Child Neurol 59:79–88
Saglam Y, Ekin Akalan N, Temelli Y, Kuchimov S (2016) Femoral derotation osteotomy with multi-level soft tissue procedures in children with cerebral palsy: does it improve gait quality? J Child Orthop 10:41–48
Boyer ER, Novacheck TF, Schwartz MH (2017) Changes in hip abductor moment 3 or more years after femoral derotation osteotomy among individuals with cerebral palsy. Dev Med Child Neurol 59:912–918
Davis RB, Õunpuu S, Tyburski D, Gage JR (1991) A gait analysis data collection and reduction technique. Hum Movement Sci 10:575–587
Leboeuf F, Baker R, Barré A, Reay J, Jones R, Sangeux M (2019) The conventional gait model, an open-source implementation that reproduces the past but prepares for the future. Gait Posture 69:235–241
Barre A, Armand S (2014) Biomechanical toolKit: open-source framework to visualize and process biomechanical data. Comput Methods Programs Biomed 114:80–87
Baker R, McGinley JL, Schwartz M, Thomason P, Rodda J, Graham HK (2012) The minimal clinically important difference for the Gait Profile Score. Gait posture 35:612–615
Hof AL (1996) Scaling gait data to body size. Gait Posture 4:222–223
Yang F, Pai YC (2014) Can sacral marker approximate center of mass during gait and slip-fall recovery among community-dwelling older adults? J Biomech 47:3807–3812
Menz HB (2004) Two feet, or one person? Problems associated with statistical analysis of paired data in foot and ankle medicine. Foot 14:2–5
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum, Hillsdale, N.J.
Lamberts RP, Burger M, du Toit J, Langerak NG (2016) A systematic review of the effects of single-event multilevel surgery on gait parameters in children with spastic cerebral palsy. PLoS ONE 11:e0164686
Desailly E, Badina A, Khouri N (2020) Kinematics after unilateral femoral derotation osteotomy in children with diplegic cerebral palsy. Orthop Traumatol Surg Res 106:1325–1331
Dohin B, Haddad E, Zagorda-Pallandre B, Zemour M (2020) Outcomes of isolated soft tissue surgery for in-toeing gait in patients with ambulatory cerebral palsy. Orthop Traumatol Surg Res 106:1367–1371
Voss S, Joyce J, Biskis A, Parulekar M, Armijo N, Zampieri C, Tracy R, Palmer AS, Fefferman M, Ouyang B, Liu Y, Berry-Kravis E, O’Keefe JA (2020) Normative database of spatiotemporal gait parameters using inertial sensors in typically developing children and young adults. Gait Posture 80:206–213
Rutz E, Donath S, Tirosh O, Graham HK, Baker R (2013) Explaining the variability improvements in gait quality as a result of single event multi-level surgery in cerebral palsy. Gait Posture 38:455–460
Mann K, Tsao E, Bjornson KF (2016) Physical activity and walking performance: influence on quality of life in ambulatory children with cerebral palsy (CP). J Pediatr Rehabil Med 9:279–286
Maher CA, Toohey M, Ferguson M (2016) Physical activity predicts quality of life and happiness in children and adolescents with cerebral palsy. Disabil Rehabil 38:865–869
Naaim A, Bonnefoy-Mazure A, Armand S, Dumas R (2019) Correcting lower limb segment axis misalignment in gait analysis: a simple geometrical method. Gait Posture 72:34–39
Funding
This study was funded by the Fonds de Recherche du Québec-Santé (FRQS) through postdoctoral scholarship received by the first author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Moisan, G., Bonnefoy-Mazure, A., De Coulon, G. et al. Assessment of gait quality and efficiency after undergoing a single-event multilevel surgery in children with cerebral palsy presenting an intoeing gait pattern. Childs Nerv Syst 38, 1523–1530 (2022). https://doi.org/10.1007/s00381-022-05548-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05548-x