Abstract
Background
The pelvic INFIX technique has been proposed as a useful alternative to symphyseal plating for management of unstable pelvic ring injuries. The minimally invasive nature of the procedure, shorter operative time and less perioperative blood loss have been purported as potential advantages.
Questions/purposes
This systematic review and meta-analysis were conducted to determine the outcomes and complications of the INFIX technique for unstable pelvic ring injuries.
Methods
A systematic review of literature was performed on the PubMed, EMBASE and Scopus databases. Prospective and retrospective studies in all languages, whether comparative or non-comparative, pertaining to the use of INFIX in pelvic fractures were included. Studies which did not evaluate INFIX, case reports, conference abstracts and those with less than 10 cases were excluded. Cadaveric studies, technique papers and studies that did not describe the prespecified outcome measures were also excluded. Meta-analysis consisted of two different arms: a comparative arm, to compare INFIX to symphyseal plating, and a non-comparative meta-analysis arm, to determine pooled rates of outcomes and complications. Risk of bias was determined by the Methodological Index for Non-Randomised Studies (MINORS) tool.
Results
A total of 22 studies were included in the systematic review, of which 7 were comparative and 15 were non-comparative. 746 patients were included for qualitative analysis and pooled analysis done for 589 patients. The average follow-up of these studies ranged from a minimum of 5.4 months to a maximum of 54 months. Comparative meta-analysis (n = 3 studies) of plating and INFIX showed significantly lesser blood loss (mean difference = 176.46 mL; 95% CI − 207.54 to − 145.38) and shorter operative time (mean difference = 26.43 min, 95% CI − 31.79 to − 21.07) with INFIX, but no significant difference in the overall complication rates (OR 1.59, 95% CI 0.83–3.05) and functional outcome scores (mean difference = − 2.51, 95% CI − 5.73 to 0.71). Pooled analysis showed overall good radiological (mean percentage of excellent to good reduction = 91.4%, 95% CI 0.860–0.969) and functional outcomes (mean Majeed score = 86.48, 95% CI 83.34–89.61) with INFIX. The most common complications were lateral femoral cutaneous nerve (LFCN) injury (overall rate 28%, 95% CI 15.1–41%) and heterotopic ossification (HO) (overall rate 9.4%, 95% CI 5.5–13.3%); rates of other complications were low. Significant heterogeneity was noted in the pooled analysis of blood loss, operative time, functional outcome, HO and LFCN injury. The overall strength of evidence was found to be weak.
Conclusion
The INFIX technique can be considered as a viable alternative to symphyseal plating for unstable pelvic ring injuries. It has the advantages of shorter operative times and less blood loss, along with comparable functional outcomes, when compared to plating. Overall, good functional outcomes can be expected. However, well-designed, multi-center randomized controlled trials are needed to conclusively prove the benefit of this technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic ring injuries are potentially life threatening and necessitate multidisciplinary care [1]. Surgical management of these injuries has revolved around the use of open reduction and internal fixation with plates, iliosacral screws and external fixation [2]. Simple injury patterns like diastasis can be managed well with plates, but complex anterior ring fractures were traditionally managed with external fixation as these can be quite challenging. However, external fixators have been associated with complications like pin site infection, limited access to the abdomen, decreased patient mobility, loosening and nerve damage, and are therefore not tolerated well by patients [3].
To overcome these limitations, the anterior subcutaneous internal fixator (ASIF) was developed from spine surgery instrumentation. This modality, termed as the INFIX or the pelvic bridge technique, utilizes pedicle screws that are placed into the ilium on either side, and connected to each other with a subcutaneous rod, with or without fixation into the symphyseal region [4]. The proposed potential benefits include fewer soft tissue infections, better pain control and patient mobilization and hence faster rehabilitation. Moreover, this technique is minimally invasive and therefore thought to be less time-consuming and associated with less blood loss.
This technique has been used for more than a decade, and several studies have reported clinical and functional outcomes with this technique. However, there is a need to critically analyze the available evidence in a comprehensive fashion so as to determine its efficacy and safety in routine surgical practice, as well as to refine its indications. Therefore, the aim of this study was to conduct this systematic review and meta-analysis to determine the outcomes and complications of the INFIX technique for unstable pelvic ring injuries following high-velocity trauma.
Methods
Objectives
-
1.
To determine the clinical and radiological outcomes of the INFIX technique for unstable pelvic ring injuries.
-
2.
To determine the complication rates of the INFIX technique for unstable pelvic ring injuries.
Study design
A systematic review and meta-analysis of literature were planned and in accordance with the PRISMA guidelines [5].
Inclusion and exclusion criteria
Prospective and retrospective studies in all languages, whether comparative or non-comparative, pertaining to the use of INFIX in pelvic fractures, with a minimum of 10 cases were included. Studies which did not evaluate INFIX, case reports, conference abstracts and those with less than 10 cases were excluded. Cadaveric studies and technique papers that did not describe the prespecified outcome measures were also excluded. Since this study involved unstable pelvic ring injuries with high-velocity trauma, INFIX used for fragility fractures of the pelvis were not included.
Search methodology
Using a well-defined search strategy, a primary search was conducted on PubMed, Scopus and Embase on 18 May 2020 (Table 1). A total number of 384 results were obtained. The secondary search was conducted by screening the references from included studies and other relevant publications on the subject.
Study selection
The selection of studies was done independently by two reviewers (SP and KJ). Titles and abstracts of the search results were screened initially. This was followed by retrieval of the full texts of relevant articles. Articles were included if they fulfilled the pre-specified inclusion criteria. For studies reported by the same author, all studies were included in the systematic review, but the study with maximum number of patients was included for analysis. Discrepancies were resolved by mutual agreement.
Data collection, data items and outcome measures
Data collection was performed by KJ and SS on a pre-piloted data collection sheet; all entries were cross-checked by SP to ensure accuracy. The following baseline data items were extracted: Journal and year of publication, language, gender, age, injury severity score (ISS and fracture classification).
Outcome measures that were extracted included perioperative blood loss and time, functional and radiological outcomes, Majeed scoring and complications.
Risk-of-bias assessment
The Methodological Index for Non-Randomised Studies (MINORS) tool [6] was used to assess the risk-of-bias for all studies by 2 independent observers (SS and VK) (Table 2). This tool is a 12-item questionnaire that can be used for both comparative and non-comparative studies. Grading is done from a score of 16 for non-comparative and 24 for comparative studies.
Data synthesis and analysis
Qualitative and quantitative analyses were performed after data extraction. For qualitative analysis, the data were organized in appropriate tables. Quantitative data synthesis consisted of two different arms: a comparative meta-analysis arm and a non-comparative meta-analysis arm.
The comparative meta-analysis arm was conducted to determine the differences in outcomes and complications between INFIX and plating for unstable pelvic ring injuries. A random-effects model was employed for this purpose; measures of treatment effects included mean difference (MD) for continuous variables (such as functional outcome score, perioperative blood loss, operative time) and odds ratio (OR) for dichotomous variables (such as complications). 95% confidence intervals (CI) were calculated for each outcome of interest. The I2 test was used to assess statistical heterogeneity. Forest plots were constructed to provide a visual summary for each outcome of interest. The RevMan 5.4 software was used for these analyses [7].
The non-comparative meta-analysis arm was conducted to determine the pooled effect size for outcomes and complication rates. Outcome measures included event rate for dichotomous variables and mean for continuous variables; 95% CI were calculated for each outcome of interest. The I2 test was used to assess statistical heterogeneity. Forest plots were constructed to provide a visual summary for each outcome of interest. All analyses were performed by the Open MetaAnalyst software [8].
Exploration of heterogeneity
For outcomes which showed high statistical heterogeneity (I2 > 75%), leave-one-out meta-analysis and meta-regression (by a random-effects model) were performed. To facilitate meta-regression, the following covariates were studied:
(a) the percentage of complex cases in the study (defined as the percentage of vertical shear and/or combined mechanism injuries, or Tiles C) (continuous variable).
(b) total cases (continuous variable).
(c) ethnicity—Asian versus non-Asian study population (dichotomous variable).
Subgroup analysis
Subgroup analysis was done by dividing the studies into those with patients of Asian ethnicity versus those of non-Asian ethnicity.
Results
Literature search
The PRISMA flowchart for the study has been presented in Fig. 7. A total of 384 records were identified, and full text retrieved for 49 studies. Twenty-seven studies were excluded as per the exclusion criteria, and a total of 22 studies were included for qualitative analysis [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30]. The details of these studies are presented in Table 3. Comparative meta-analysis was performed on 3 studies that compared INFIX with plating [12, 25, 30] and pooled analysis was performed on 18 studies.
Characteristics of study
A summary of the studies included in the review has been presented in Table 4. A total of 746 patients were included for qualitative analysis; of these, pooled analysis was done for 589 patients. The average follow-up of these studies ranged from a minimum of 5.4 months to a maximum of 54 months. The mean time to radiological union was reported in 3 studies with an average time of 4.1 months [11, 15, 18].
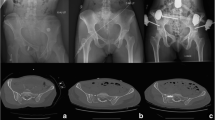
Comparative meta-analysis—plating versus INFIX (Fig. 1)
Comparative meta-analysis revealed significantly less blood loss with the INFIX procedure as compared to plating (mean difference = 176.46 mL; 95% CI − 207.54 to − 145.38) and significantly shorter operative time (mean difference = 26.43 min, 95% CI − 31.79 to − 21.07) and no significant difference in the overall complication rates (OR 1.59, 95% CI 0.83–3.05) and functional outcome score (MD − 2.51, 95% CI − 5.73 to 0.71).
Pooled analysis
Perioperative events
The pooled mean operative time estimated from 12 studies (330 patients) was 52.1 min (95% CI 43.69–60.51); the heterogeneity for this estimate was high (I2 = 99.42%, p < 0.01) (Fig. 2). Meta-regression revealed that the high heterogeneity was not explained by the percentage of complex pelvic injury cases, total number of cases or the surgical volume (less than or more than 25 cases).
The pooled mean blood loss estimated from 10 studies (266 patients) was 65.425 mL (95% CI 51.022–79.828); the heterogeneity for this estimate was high (I2 = 99.61%, p < 0.001) (Fig. 2). Covariate analysis for the percentage of complex cases (vertical shear or combined type/tiles type C) showed significant increase in blood loss with the increase in complex cases (p = 0.03).
Outcomes (Table 5)
Radiological outcomes
The quality of reduction was reported as per Matta’s criteria [31] by 7 studies in 161 patients. Pooled analysis showed an excellent to good reduction in 91.4% of the cases (95% CI 0.860–0.969), with a moderate heterogeneity (I2 = 45.26%, p = 0.09) (Fig. 3).
Functional outcomes
Majority of the studies reported Majeed scoring [32]. Only 1 study [10] used the Iowa pelvic score as they consider it to have the best correlation with SF-36 and is a good tool for measuring outcomes in severe pelvic injury. Pooled analysis of 8 studies reporting Majeed score showed an average score of 86.48 (95% CI 83.34–89.61); the heterogeneity for this event was high (I2 = 92.37%, p < 0.01) (Fig. 3). Meta-regression analysis showed that better Majeed score was obtained with complex fracture patterns (p = 0.001).
Outcome scoring classified as excellent or good was reported in 82.8% cases in 10 studies with 228 patients (95% CI 73.7–91.9%); the heterogeneity for this event was high (I2 = 82.24%, p < 0.001) (Fig. 3). Meta-regression showed a trend of poorer results with complex patterns but was not statistically significant (p = 0.118). Leave-one-out analysis excluding Kuttner et al. [27] improved overall estimate from 82.8 to 88.2% (95% CI 81.9–94.5%).
Complications
The complications of the INFIX procedure have been presented in Table 6.
Non-union
Only 2 cases of non-union have been reported in literature. Muller et al. [22] reported nonunion in a schizophrenic non-compliant patient while Dahill et al. [29] reported 1 asymptomatic nonunion. Pooled analysis showed an overall nonunion rate of 1.2% (95% CI 0.4–2.1%); the heterogeneity for this event was low (I2 = 0%, p = 1.000) (Fig. 4).
Infection
The overall rate of infection with INFIX was seen to be 2.3% (95% CI 1.1–3.4%); the heterogeneity for this event was low (I2 = 0%, p = 0.971). Seventeen cases of infections have been reported overall in the studies (Fig. 4).
Loosening
Loosening of implant is a rare complication reported in 7 cases. The overall rate of loosening was found to be 1.3% (95% CI 0.4–2.2%); the heterogeneity for this event was low (I2 = 0%, p = 0.995) (Fig. 4).
HO
HO though usually asymptomatic is a commonly associated complication with an overall rate of 9.4% (95% CI 5.5–13.3%); the heterogeneity for this event was high (I2 = 87%, p < 0.001). High number of cases of HO have been reported by Vaidya et al. [23] (n = 32), Hoskins et al. [21] (n = 14) and Yin et al. [12] (n = 12) in their studies (Fig. 4). Subgroup analysis was done according to ethnicity (Asians and non-Asians), and it was seen that non-Asians were more susceptible (23.6% versus 4.2% in Asians). Meta-regression according to ethnicity showed a strong correlation (p = 0.01).
LFCN injury
LFCN injury, mostly self-limiting is the most commonly seen complication with INFIX. Pooled analysis showed an overall rate of LFCN injury as 28% (95% CI 15.1–41%); the heterogeneity for this event was high (I2 = 95.7%, p < 0.001). Vaidya et al. [23] reported 27 LFCN injuries in a series of 96 patients, while Hoskin et al. [21] reported 20 nerve injuries in 21 cases (42 screws) (Fig. 5). Cumulative meta-analysis shows that from the year 2018, the complication rate of LFCN injury is similar, but despite 9-year experience, the complication rate is stationary around 30%. Subgroup analysis was done according to ethnicity (Asians and non-Asians), and it was seen that non-Asians were more susceptible to LFCN injury (40.9% versus 18.9% in Asians). However, meta-regression according to ethnicity showed a weak correlation (p = 0.053).
Deep venous thrombosis (DVT)
Pooled analysis showed that the overall rate of DVT was 1.2% (95% CI 0.3–2.1%); the heterogeneity for this event was low (I2 = 0%, p = 0.926). A total of 8 cases of DVT have been reported in literature (Fig. 6).
Femoral nerve injury
Pooled analysis showed that overall rate of femoral nerve injury was 1.3% (95% CI 0.4–2.2%); the heterogeneity for this event was low (I2 = 0%, p = 0.998) (Figs. 6, 7).
Loss of reduction
Loss of reduction has been reported in 6 cases with overall rate of 1.8% (95% CI 0.7–2.8%); the heterogeneity for this event was low (I2 = 0%, p = 1.000). This loss of reduction has been reported in the immediate post-operative phase, and no study has reported any loss of reduction post-implant removal (Fig. 6).
Early removal
Early implant removal due to loosening, infection or nerve injury was done in 18 patients with overall rate of 2.1% (95% CI 0.9–3.2%); the heterogeneity for the event was low (I2 = 0%, p = 0.761). However, studies have reported that despite the early removal of implant in these cases, the patients have satisfactory functional outcomes (Fig. 6).
Risk of bias assessment
The risk of bias assessment is depicted in Table 2 using MINORS tool. For non-comparative studies, 7 studies had a score of 12, 5 had a score of 11, 3 had a score of 10 and 1 had a score of 9. For comparative studies, 1 study had a score of 21, 3 had a score of 20, 1 had a score of 19 and 1 had a score of 18. There were no randomized control trials reported.
Discussion
Pelvic fractures are complex injuries with disruption of multiple bony or ligamentous components. The indications for anterior fixation with INFIX are unstable pelvic ring injuries (Tiles B and C or Young and Burgess-LC 2 and 3, APC 2 and 3, Vertical Shear and Combined) in conjunction with posterior fixation. Symphyseal injuries are conventionally treated with plating [19, 21]. However, in Types B and C injuries it is associated with extensive exposure and increased complications, and thus the role of INFIX has been developed as a useful modality. The sequence of fixation is usually posterior fixation followed by anterior fixation. However, Gardner et al. [24] demonstrated that anterior fixation should be considered first for pelvic reduction.
Biomechanical studies done by Vaidya et al. [33], Osterhoff et al. [34], Eagan et al. [35] show that mechanical stiffness of an INFIX construct is similar or superior to that of an external fixator. Monoaxial screws are 26% more rigid than polyaxial screws but are technically more difficult. However, Vigdorchik [36] showed that internal fixation of the anterior ring with plates was still the strongest when compared to INFIX or an external fixator. As such, in patients with pure symphyseal injury, internal fixation is still the preferred treatment.
INFIX being a subcutaneous procedure was associated with relatively low blood loss (mean 65.425 mL). However, no study reported the method of estimation of blood loss which could account for the variability. Moreover, few studies have reported blood loss for anterior and posterior fixation combined which could be a possible cause of high heterogeneity in our analysis.
The duration of INFIX fixation was seen to be an average of 52.1 min. The pooled analysis shows that it a short procedure with excellent results. However, the need for a concomitant surgical procedure such as spino-pelvic fixation by Du et al. [9] increased the operative time in their series. We also observed that being a percutaneous procedure with only indirect reductions being done, the operative time does not increase significantly with complex anterior ring injuries.
Only 2 nonunion cases have been reported in literature which is indicative of a very high union rate, which is also true for pelvic fractures in general. Adequate reduction of fracture fragments is the key for a successful outcome. Outcome scores have mainly reported excellent to good results. These are better in comparison with those studies where anterior external fixators were applied or when injuries were left conservatively to heal on their own [15]. However, many pelvic ring injuries are associated with multiple other injuries that affect the overall outcome and make it impossible to assess treatment [19]. For these, patient-reported outcome scores have been developed which may need to be reported more in the forthcoming studies.
No procedure is without complications and INFIX has been associated with LFCN injury, HO, vascular injury, DVT, femoral nerve palsy and surgical site infection.
LFCN injury is a common complication but is usually self-limiting. Rudin et al. [37] studied in detail the anatomical variations of LFCN in 18 cadavers and saw different pathways. They observed that it crossed the level of the inguinal ligament just superficial to the ASIS in 29%, lateral to ASIS in 11% and medial to ASIS in 69%. Osterhoff et al. [38] observed that the LFCN is found to run 13.49 mm from lateral end of bar. Thus, a very short lateral end of the bar prevents the irritation of LFCN. However, we observed that the incidence of LFCN injury remains as high as up to 30% and thus proper identification of the nerve by careful dissection up to the bone and extending the incision as per comfort is important to minimize its occurrence. We also noticed that non-Asians were more susceptible to LFCN injury (40.9% versus 18.9% in Asians) and this could be because of anatomical variations.
HO though common is usually asymptomatic. Vaidya et al. in their study [19] found older age and higher injury severity score as risk factors for developing HO. However, no significant relation was found with sex, race, Majeed score and Glasgow coma scale in their study. This can be usually removed at the time of implant removal in cases of excessive bone formation. In our pooled analysis we observed a higher incidence of HO in non-Asian population and this could be related to the genetics as incidence of HO is known to be influenced by race [39]. HO was usually Grade 1 or 2 and no active intervention was required.
Femoral nerve palsy has also been reported as a rare complication. Hesse et al. [40] in their study reported 8 femoral nerve palsies in 6 patients. They said that injury is likely due to limited space available for the psoas muscle and femoral nerve and that sinking screws or under contouring of the rod is a possible cause of compression. Thus studies by Scherer et al. [41] recommended bar to bone distance of 20–25 mm to avoid compression. Vaidya et al. [23] recommended the screw head to be kept at the level of the sartorius such that the subcutaneous bar remains above the level of deep fascia.
Smith et al. [42] reported a case of bilateral compression of the external iliac artery after the application of INFIX. They identified on CT angiogram the bulging of the rectus muscle underneath the INFIX and subsequent compression against the bar which resolved by increasing the arc of curvature. Merriman et al. [43] calculated average bar to vessel distance of 2.2 cm and rod to bladder distance of 2.6 cm. Thus, it can be usually avoided by proper implant placement and adequate contouring of the anterior bar.
Surgical site infection was seen in 17 cases (2.3%) with no evidence of osteomyelitis. Pelvic INFIX is seen to be associated with low rates of infection and is a safe procedure.
The rates of DVT have been seen to be low with the application of INFIX (1.2%). This may be due to early mobilization with this implant and the routine use of thromboprophylaxis.
There is an inherent risk of abdominal wall perforation with errant rod placement. It is important to maintain the rod in a subcutaneous position without violation of the abdominal fascia. This can be performed reliably by tunneling a path below the abdominal wall before rod insertion. Jain et al. [44] reported a rare case of bladder incarceration following application of INFIX in a case of pubic diastasis. This occurred at the time of compression of the diastasis after application of INFIX. Thus, an index of suspicion is warranted and timely INFIX removal with open reduction and stabilization is warranted.
Patients with INFIX have “awareness” about their implants due to its subcutaneous position which is a cause of uneasiness as compared to conventional plating [39]. Thus, most of the implants require removal after radiological union. However, as opposed to an external fixator, the subcutaneous nature of this construct requires removal in an operating room.
Some modifications have been applied to INFIX technique with time. Few studies such as Bi et al. [28] and Wu et al. [16] have added a 3 cm Pfannenstiel incision 2 cm above the pubic symphysis and inserted a polyaxial pedicle screw through the ipsilateral or contralateral pubic tubercle to the inferior ramus. They believe that it forms a stable geometric triangle allowing better fit of the rod with the anatomy of the anterior pelvic ring. It also helps in better restriction of relative micro-movement between the sites of the fractured pubis. Wang et al. [30] used the modified INFIX technique for cases of pubic diastasis by inserting 4 screws (one each in pubic tubercle) in a series of 29 cases and reported excellent to good outcomes in 27 patients. Robot-assisted placement of screws has also been reported by Du et al. [9] and Liu et al. [11]. Liu et al. in their study compared robot-assisted INFIX with the conventional technique and showed shorter duration of surgery, need for lesser fluoroscopy, and reduced blood loss with the robotic technique.
There are some limitations in this study. The included studies as mentioned are all case series or comparative studies with no randomized control trial. There were only 3 studies available for comparative meta-analysis. Secondly, a high statistical heterogeneity was noted for some of the outcomes reported in our analysis. We have, however, performed meta-regression and subgroup analysis to try and identify the reasons for heterogeneity.
From our systematic review and meta-analysis, it appears that INFIX is a valuable tool for reduction and fixation in unstable pelvic ring fractures and is well tolerated by the patient, allowing good mobility with acceptable complications and outcomes. It is a minimally invasive technique with less blood loss and surgical time in comparison with conventional plating with comparable complications and similar outcomes.
Conclusion
INFIX is a biomechanically stable and effective minimally invasive surgical technique for management of unstable pelvic ring fractures. However, it is imperative to stabilize the posterior ring first if required with use of plates and screws.
References
Davarinos N, Ellanti P, Morris S, Mc Elwain JP (2012) Epidemiology of pelvic and acetabular trauma in a Dublin tertiary hospital: a 10-year experience. Ir J Med Sci 181(2):243–246. https://doi.org/10.1007/s11845-011-0791-4
Tile M (1988) Pelvic ring fractures: should they be fixed? J Bone Jt Surg Br 70(1):1–12
Cole PA, Gauger EM, Anavian J, Ly TV, Morgan RA, Heddings AA (2012) Anterior pelvic external fixator versus subcutaneous internal fixator in the treatment of anterior ring pelvic fractures. J Orthop Trauma 26(5):269–277. https://doi.org/10.1097/BOT.0b013e3182410577
Cole PA, Hesse DK, Dugarte AJ, Dyskin E (2017) The pelvic bridge: a subcutaneous approach for anterior pelvic fixation. JBJS Essent Surg Tech 7(3):e20. https://doi.org/10.2106/jbjs.St.15.00085
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clin Res Ed) 350:g7647. https://doi.org/10.1136/bmj.g7647
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Review Manager (RevMan) (2020) [Computer Progrman]. Version 5.4. 5.4 edn. The Cochrane Collaboration, 2020
Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH (2012) Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw 49(5):1–15
Du W, Sun T, Ding Y, Jiang C, Qu W, Zhang S (2020) Robot-assisted treatment of unstable pelvic fractures with a percutaneous iliac lumbar double rod fixation combined with a percutaneous pelvic anterior ring INFIX fixation. Int Orthop 44(6):1223–1232. https://doi.org/10.1007/s00264-020-04522-z
Steer R, Balendra G, Matthews J, Wullschleger M, Reidy J (2019) The use of anterior subcutaneous internal fixation (INFIX) for treatment of pelvic ring injuries in major trauma patients, complications and outcomes. SICOT-J 5:22. https://doi.org/10.1051/sicotj/2019019
Liu HS, Duan SJ, Liu SD, Jia FS, Zhu LM, Liu MC (2018) Robot-assisted percutaneous screw placement combined with pelvic internal fixator for minimally invasive treatment of unstable pelvic ring fractures. Int J Med Robot Comput Assist Surg 14(5):e1927. https://doi.org/10.1002/rcs.1927
Yin Y, Luo J, Zhang R, Li S, Jiao Z, Zhang Y, Hou Z (2019) Anterior subcutaneous internal fixator (INFIX) versus plate fixation for pelvic anterior ring fracture. Sci Rep 9(1):2578. https://doi.org/10.1038/s41598-019-39068-7
Hua X, Yan SG, Cui Y, Yin Z, Schreiner AJ, Schmidutz F (2019) Minimally invasive internal fixator for unstable pelvic ring injuries with a pedicle screw-rod system: a retrospective study of 23 patients after 135 months. Arch Orthop Trauma Surg 139(4):489–496. https://doi.org/10.1007/s00402-018-3094-7
Ding S, He X, Zhang G, Ruan Z, Wu X (2019) Modified internal fixator for anterior pelvic ring fractures versus conventional two-screw fixation. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-019-01164-8
Shetty AP, Bosco A, Perumal R, Dheenadhayalan J, Rajasekaran S (2017) Midterm radiologic and functional outcomes of minimally-invasive fixation of unstable pelvic fractures using anterior internal fixator (INFIX) and percutaneous iliosacral screws. J Clin Orthop Trauma 8(3):241–248
Wu XT, Liu ZQ, Fu WQ, Zhao S (2018) Minimally invasive treatment of unstable pelvic ring injuries with modified pedicle screw-rod fixator. J Int Med Res 46(1):368–380. https://doi.org/10.1177/0300060517715529
Wang Q, Wang Q, Wang J (2017) Treatment of type B pelvic fracture using anterior subcutaneous internal fixator with triple pedicle screws: a new surgical technique. Arch Orthop Trauma Surg 137(7):887–893
Fang C, Alabdulrahman H, Pape HC (2017) Complications after percutaneous internal fixator for anterior pelvic ring injuries. Int Orthop 41(9):1785–1790. https://doi.org/10.1007/s00264-017-3415-4
Vaidya R, Martin AJ, Roth M, Tonnos F, Oliphant B, Carlson J (2017) Midterm Radiographic and Functional Outcomes of the Anterior Subcutaneous Internal Pelvic Fixator (INFIX) for pelvic ring injuries. J Orthop Trauma 31(5):252–259. https://doi.org/10.1097/bot.0000000000000781
Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A (2012) Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma 26(1):1–8. https://doi.org/10.1097/BOT.0b013e318233b8a7
Hoskins W, Bucknill A, Wong J, Britton E, Judson R, Gumm K, Santos R, Sheehy R, Griffin X (2016) A prospective case series for a minimally invasive internal fixation device for anterior pelvic ring fractures. J Orthop Surg Res 11(1):135. https://doi.org/10.1186/s13018-016-0468-9
Müller FJ, Stosiek W, Zellner M, Neugebauer R, Füchtmeier B (2013) The anterior subcutaneous internal fixator (ASIF) for unstable pelvic ring fractures: clinical and radiological mid-term results. Int Orthop 37(11):2239–2245. https://doi.org/10.1007/s00264-013-2032-0
Vaidya R, Kubiak EN, Bergin PF, Dombroski DG, Critchlow RJ, Sethi A, Starr AJ (2012) Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: a multicenter study. Clin Orthop Relat Res 470(8):2124–2131. https://doi.org/10.1007/s11999-011-2233-z
Gardner MJ, Mehta S, Mirza A, Ricci WM (2012) Anterior pelvic reduction and fixation using a subcutaneous internal fixator. J Orthop Trauma 26(5):314–321. https://doi.org/10.1097/BOT.0b013e318220bb22
Vaidya R, Martin AJ, Roth M, Nasr K, Gheraibeh P, Tonnos F (2017) INFIX versus plating for pelvic fractures with disruption of the symphysis pubis. Int Orthop 41(8):1671–1678. https://doi.org/10.1007/s00264-016-3387-9
Zhang Y, Liu Y, Wu C, Song L, Ren D, Zhang Y, Peng A (2016) Treatment of unstable pelvic ring injuries with an internal anterior fixator: initial clinical series. Int J Clin Exp Med 9(9):18637–18644
Kuttner M, Klaiber A, Lorenz T, Füchtmeier B, Neugebauer R (2009) The pelvic subcutaneous cross-over internal fixator. Der Unfallchirurg 112(7):661–669. https://doi.org/10.1007/s00113-009-1623-0
Bi C, Wang Q, Wu J, Zhou F, Zhang F, Liang H, Lyu F, Wang J (2017) Modified pedicle screw-rod fixation versus anterior pelvic external fixation for the management of anterior pelvic ring fractures: a comparative study. J Orthop Surg Res 12(1):185. https://doi.org/10.1186/s13018-017-0688-7
Dahill M, McArthur J, Roberts GL, Acharya MR, Ward AJ, Chesser TJS (2017) The use of an anterior pelvic internal fixator to treat disruptions of the anterior pelvic ring: a report of technique, indications and complications. Bone Jt J 99(9):1232–1236. https://doi.org/10.1302/0301-620x.99b9.Bjj-2016-1025.R2
Wang J, Cao L, Wu J, Wang Q, Bi C (2018) Clinical and radiological short-term outcomes of pubic symphysis diastasis treated with modified pedicle screw-rod fixation. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-018-1050-4
Tornetta P 3rd, Matta JM (1996) Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res 329:186–193. https://doi.org/10.1097/00003086-199608000-00022
Majeed SA (1989) Grading the outcome of pelvic fractures. J Bone Jt Surg Br 71(2):304–306
Vaidya R, Onwudiwe N, Roth M, Sethi A (2013) Monoaxial pedicle screws are superior to polyaxial pedicle screws and the two pin external fixator for subcutaneous anterior pelvic fixation in a biomechanical analysis. Adv Orthop. https://doi.org/10.1155/2013/683120
Osterhoff G, Tiziani S, Ferguson SJ, Spreiter G, Scheyerer MJ, Spinas GL, Wanner GA, Simmen HP, Werner CM (2014) Mechanical testing of a device for subcutaneous internal anterior pelvic ring fixation versus external pelvic ring fixation. BMC Musculoskelet Disord 15:111. https://doi.org/10.1186/1471-2474-15-111
Eagan M, Kim H, Manson TT, Gary JL, Russell JP, Hsieh AH, O’Toole RV, Boulton CL (2015) Internal anterior fixators for pelvic ring injuries: do monaxial pedicle screws provide more stiffness than polyaxial pedicle screws? Injury 46(6):996–1000. https://doi.org/10.1016/j.injury.2015.01.040
Vigdorchik JM, Esquivel AO, Jin X, Yang KH, Onwudiwe NA, Vaidya R (2012) Biomechanical stability of a supra-acetabular pedicle screw internal fixation device (INFIX) vs external fixation and plates for vertically unstable pelvic fractures. J Orthop Surg Res 7:31. https://doi.org/10.1186/1749-799x-7-31
Rudin D, Manestar M, Ullrich O, Erhardt J, Grob K (2016) The anatomical course of the lateral femoral cutaneous nerve with special attention to the anterior approach to the hip joint. J Bone Jt Surg Am 98(7):561–567. https://doi.org/10.2106/jbjs.15.01022
Osterhoff G, Aichner EV, Scherer J, Simmen HP, Werner CML, Feigl GC (2017) Anterior subcutaneous internal fixation of the pelvis—what rod-to-bone distance is anatomically optimal? Injury 48(10):2162–2168. https://doi.org/10.1016/j.injury.2017.08.047
Slone HS, Walton ZJ, Daly CA, Chapin RW, Barfield WR, Leddy LR, Hartsock LA (2015) The impact of race on the development of severe heterotopic ossification following acetabular fracture surgery. Injury 46(6):1069–1073
Hesse D, Kandmir U, Solberg B, Stroh A, Osgood G, Sems SA, Collinge CA (2015) Femoral nerve palsy after pelvic fracture treated with INFIX: a case series. J Orthop Trauma 29(3):138–143. https://doi.org/10.1097/bot.0000000000000193
Scherer J, Tiziani S, Sprengel K, Pape H-C, Osterhoff G (2019) Subcutaneous internal anterior fixation of pelvis fractures—which configuration of the InFix is clinically optimal?—a retrospective study. Int Orthop 43(9):2161–2166
Smith A, Malek I, Lewis J, Mohanty K (2017) Vascular occlusion following application of subcutaneous anterior pelvic fixation (INFIX) technique. J Orthop Surg 25(1):2309499016684994
Merriman DJ, Ricci WM, McAndrew CM, Gardner MJ (2012) Is application of an internal anterior pelvic fixator anatomically feasible? Clin Orthop Relat Res 470(8):2111–2115. https://doi.org/10.1007/s11999-012-2287-6
Jain M, Nanda SN, Mohapatra SS, Samal BP (2017) Bladder incarceration following anterior pelvic infix of a traumatic pubic symphysis diastasis treated with immediate open reduction and internal fixation. J Clin Orthop Trauma 8:S11–S16
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, S., Aggarwal, S., Jindal, K. et al. Outcomes and complications of the INFIX technique for unstable pelvic ring injuries with high-velocity trauma: a systematic review and meta-analysis. Arch Orthop Trauma Surg 142, 787–803 (2022). https://doi.org/10.1007/s00402-020-03742-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03742-7