Abstract
Introduction
To evaluate the clinical outcomes of anterior subcutaneous internal fixator using triple pedicle screws (ASIF/TPS) in the treatment of unstable type B pelvic fracture compared with open reduction internal fixation (ORIF).
Materials and methods
This was a retrospective cohort study of 26 patients with type B unstable fractures that underwent ASIF/TPS and 26 similar patients that underwent ORIF using plates and screws. Intraoperative blood loss, operating time, and post operation hospitalization duration were compared. Anteroposterior, inlet, and outlet X-rays and 3D computed tomography were obtained. Pain, numbness, sexual dysfunction, and activity were evaluated at every follow-up visit until the implants were removed. The Majeed score was used to assess the clinical and radiological outcomes.
Results
Blood loss, operating time, and hospitalization duration were less (all P < 0.001) in the ASIF/TPS group compared with the ORIF group. The clinical and radiological outcomes of the ASIF/TPS group after a mean follow-up of 6 months were excellent and good in 80.8%, and moderate in 19.2%. In comparison, the results of the ORIF group were excellent and good in 65.4%, moderate in 29.0%, and poor in 5.6%. No patient experienced nonunion, delayed union, superficial infection, or deep surgical wound infection. No urethral injury or dysuria occurred in the ASIF/TPS group. Two patients had temporary lateral femoral cutaneous nerve numbness after operation. There were two superficial wound infections in the ORIF group.
Conclusions
The use of ASIF/TPS with triple pedicle screws could be a reasonable option for the treatment of type B unstable pelvic fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic fractures result from high energy trauma that can be caused by falls and road traffic accidents [1, 2], and results in pain and loss of mobility [3]. The mortality from type B unstable pelvic fractures can be as high as 25% [4]. Anterior pelvic external fixation for the initial treatment of unstable, complex pelvic injuries with hemodynamic instability remains an effective treatment for trauma patients with a severe pelvic fracture [5]. However, pin site infection rates are high with external fixation (around 18%) [6, 7] and other severe complications include fixator loosening, and impingement of the fixator on the skin [8]. According to the position of fixation, external fixation can be divided into two types: iliac crest fixation and anterior inferior iliac spine (AIIS) fixation. Compared with iliac crest fixation, AIIS external fixation improves biomechanical strength, but the complications listed above remain, and because the external fixator is fixed without incision, injury to the lateral femoral cutaneous nerve can occur.
Open reduction internal fixation (ORIF) with plates and screws provides rigid internal fixation, but may lead to massive soft tissue injury, longer surgery time, longer rehabilitation time, and increased bleeding [9]. A novel method of internal fixation has been recommended using an anterior subcutaneous internal fixator (ASIF) with pedicle screws [10, 22, 23]. ASIF combines the advantages of external fixation for anterior ring stabilization with the advantages of internal fixation (e.g., decreased risk of pin-track infection, pin site pain, and bowel obstruction) [11]. Cole et al. [12] also reported a method of anterior pelvic internal fixation applied by locking pelvic plates, during which one or two plates are chosen depending on whether unilateral or bilateral anterior lesions are present. There are still some limitations of the technique, such as its use on pelvic fractures that cannot achieve reduction directly through plates and screws.
To find a method that combines the advantage of ASIF and ORIF with minimal invasive surgery, we modified the ASIF technique by adding the pubic symphysis pedicle screw, which should increase the biomechanical strength of ASIF. Therefore, the aim of this report is to describe and to demonstrate the effectiveness of this new ASIF technique using triple pedicle screws (ASIF/TPS), compared with ORIF.
Materials and methods
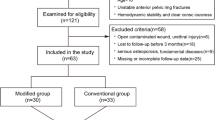
Study design and patients
This was a retrospective study of 26 consecutive patients with type B pelvic fractures that underwent definitive anterior fixation with ASIF/TPS between August 2013 and June 2014. The patients in the control group were matched for gender and age and included 26 patients with type B pelvic fracture that underwent ORIF with plates and screws according to standard procedures. All surgeries were performed by the same two surgeons (Jiandong Wang and Qian Wang). The choice of the surgical approach was made after discussion between the surgeon and the patient and between the two surgeons.
This study was approved by the medical ethics committee of Shanghai First People’s Hospital (approval 2014KY004). Written informed consent was obtained from each participant. The study was conducted in compliance with the Declaration of Helsinki.
Surgical technique
The surgical procedure for ORIF was based on standard techniques, as previously described [9]. A graphical representation of the ASIF/TPS procedure drawn with the 3DMAX software (2009 version, Autodesk, Inc. Mill Valley, CA, USA) is shown in Fig. 1. The surgery was performed supine on a radiolucent operational table (MAQUET Holding B.V. & Co. KG, Rastatt, Germany). The patient`s bilateral hips were put in flexion, abduction, and external rotation position, so that it was easy to relax the bilateral iliopsoas and sartorius muscles.
3D drawings representing the Judet oblique view (a) and outlet view (b) of anterior subcutaneous internal fixation and the relationship of internal fixation with blood vessels, nerves, spermatic cord, muscles, and bones. Since screws of the bilateral anterior inferior iliac spine and pubic bone were not clung, vascular or nerve compression from the connecting rods could be avoided. During the operation, interactions between the connecting rods and vessels and nerves could be avoided via the subcutaneous tunnel. When necessary, intraoperative B-type ultrasound could be performed to check the interactions between the connecting rods and vessels and nerves
A mark was made on the skin at the AIIS and pubis symphysis, and the medial line of the pubis symphysis was also marked (Fig. 2). An incision was made over each AIIS and a 3–4 cm incision was cut over the pubic symphysis (left or right side according to the surgery design). The AIIS was explored from the medial space of the sartorius and the lateral space of the iliopsoas in a longitudinal direction to avoid the lateral femoral cutaneous nerve being injured. A tunnel in the AIIS bone was prepared. Probes and bone taps were marked and 80-mm pedicle screws were inserted under the space of the sartorius and lateral side of the iliopsoas. Height and cranial tilt of the pedicle screws were confirmed with the iliac oblique view, and penetration was assessed with the inlet-obturator oblique view.
Skin marking and position of the patient. The bilateral anterior superior iliac spines were marked preoperatively. Bilateral oblique incision markings (about 3 cm each) were made along the bilateral anterior inferior iliac spines and direction of the dermatoglyph. The midline was marked at the pubic symphysis, and an incision of about 3 cm was made above the pubic symphysis, slightly left or right to the midline
A middle pedicle screw was inserted into the pubic ramus. For unilateral pubic ramus fractures, the middle pedicle screw was fixed on the fracture side if the fracture lines were far from the pubic symphysis. For comminuted pubic ramus fractures, the middle pedicle screw was inserted into the uninjured side. For bilateral pubic ramus fractures, the pedicle screw was fixed on the less damaged side. In all cases, the middle pedicle screw was inserted parallel to the pubic symphysis, and the screw was not inserted too deep to avoid injury to the posterior bladder and inferior urethra. In cases with an inclination of the pubic body, the middle pedicle screw was inserted following the same inclination to avoid injury to adjacent organs. Importantly, it was observed that when the patients were put into a hip flexion and abduction position, the pubic body was in a much more inclined position.
For male and female patients, the length of the middle pedicle screw was 50 and 45 mm, respectively. The inlet and outlet views were used to ensure that the pedicle screws were placed correctly.
Titanium connecting model rods were placed over the body surface to confirm the appropriate length of the connecting rods. From the anteroposterior (AP) view of the pelvis, the appropriate rod length was confirmed and cut, leaving 1 cm free at each end. A large-sized vessel clamp was used to penetrate the soft tissue subcutaneously from the middle incision to both sides. The femoral nerve is the structure mostly at risk of compression by the INFIX rod, so we should leave some space between the screw and rectus fascia [20]. A distraction or compression device was used to deal with closed book or open book pelvic ring fractures [13]. In that way, the pelvic facture was indirectly reduced. The screw heads were threaded to capture the rod. An AP view was taken to confirm fracture reduction. The wounds were washed with saline and the subcutaneous tissue and skin were closed in layers.
The subcutaneous internal fixation was removed during follow-up when the fracture was healed. Internal fixation was not removed in the ORIF group after operation.
Follow-up
First follow-up was at 2 weeks post-operation for a wound evaluation and suture removal, and the patients were subsequently seen at 4, 8, 12, and 16 weeks. A three-view series (AP, inlet, and outlet) and three-dimensional computed tomography (3D-CT) were obtained. The patients completed a questionnaire about pain, numbness, sexual dysfunction, and activity at each follow-up visits until the implants were removed. The Majeed score was also applied to assess the clinical and radiological outcomes. It consists of seven assessments: (1) pain (30 points); (2) work (20 points); (3) sitting (10 points); (4) sexual intercourse (4 points); (5) standing, walking aids (36 points); (6) standing, gait unaided (12 points); and (7) standing, walking distance (12 points) [14]. For patients working before injury, excellent is defined as >85 points, good as 70–84 points, fair as 55–69 points, and poor as <55. For patients not working before injury, excellent is defined as >70 points, good as 55–69 points, fair as 45–54 points, and poor as <45 [14].
Data collection
Intraoperative blood loss was estimated based on the content in the drainage bottle and the blood infiltrating the gauze dressings. Operating time was defined as the time between skin incision and the end of suturing. Post-operation hospitalization duration was defined as the time between operation and discharge.
Statistical analysis
Data were analyzed using SPSS 17.0 (IBM, Armonk, NY, USA). Data are presented as mean ± standard deviation (SD) or actual number. Comparisons were made using the Student t test. A P value <0.05 was considered statistically significant.
Results
Characteristics of the patients
Table 1 presents the characteristics of the patients. The mean age of the patients was 39.3 ± 17.0 years. There were 16 men and 10 women. All patients had type B pelvic fractures according to Tile classification. There were 8 cases of type B1, 13 cases of type B2, and 5 cases of type B3. The mean age of the controls was 38.2 ± 13.1 years. There were 15 men and 11 women. There were 4 type B1 cases, 15 B2 cases, and 7 B3 cases.
Characteristics of the surgeries
The subcutaneous internal fixation was removed at 4.3 months postoperation (range from 3.2 to 7.3 months). Despite having undergone two surgeries, the patients in the ASIF/TPS group had less blood loss (57.5 ± 16.9 vs. 186.5 ± 92.8 ml, P < 0.001), shorter operation time was (91.2 ± 13.0 vs. 114.1 ± 19.7 min, P < 0.001), and shorter hospitalization duration (14.2 ± 3.0 vs. 17.9 ± 0.7 days, P < 0.001) (Table 2).
Follow-up
Patients were followed up for a mean of 8.2 months (range 6.0–10.5 months) for the ASIF/TPS group and 9.3 months (range 7.3–11.5 months) for the ORIF group. In the ASIF/TPS group, there was no clinical or radiographic evidence of delayed healing or nonunion in any patients. An example of X-rays and CT results from a patient with B-type fracture caused by internal rotation of the hemipelvis treated with ASIF/TPS is shown in Fig. 3. Clinical and radiological outcomes were excellent and good in 21 of 26 patients (80.8%), and moderate in 5 patients (19.2%). Eighteen of the 26 patients (69.2%) could flex their bilateral hips over 95°. Sixteen patients (61.5%) could perform deep squats 1.5 months after surgery (Fig. 4).
Preoperative X-ray (a), CT 3D-reconstruction (b) and postoperative X-ray (c) anteroposterior views. For patients with complete pubic bone, we implanted the screws from the lesioned side. For patients with comminuted fractures, we placed the screws from the healthy side to reduce the moment arms and increase stability of the screw–rod system. This patient had a B-type fracture caused by internal rotation of the hemipelvis, but after assessment, it was determined that the middle screw could not be fixed on the fracture side. During operation, we restored the lesioned hemipelvis, achieved reduction of the fracture, and increased the stability of the lesioned hemipelvis
In the ORIF group, there was no clinical or radiographic evidence of delayed healing or nonunion in any patients. Clinical and radiological outcomes were excellent and good in 17 of 26 patients (65.4%), moderate in 7 (26.9%), and poor in 2 (7.7%).
Complications
None of the patients had non-union or delayed union, superficial or deep surgical wound infection, or bladder, urethral canal, spermatic cord, or vaginal injury. Two patients had temporary lesions to the lateral femoral cutaneous nerve in the ASIF/TPS group. Two patients had superficial wound infection in the ORIF group.
Discussion
Compared with patients who underwent ORIF, more patients who underwent ASIF/TPS had excellent or good clinical and radiological outcomes. The intraoperative blood loss was lower, and the operation time and postoperative hospitalization were shorter in the ASIF/TPS group compared with the ORIF group. As these results suggest that outcomes and complications are more favorable with ASIF/TPS than ORIF, this modified technique should be considered for treatment of patients with type B pelvic fractures.
This method is probably not suitable for unstable patients with multiple traumas where immediate fast fixation is a lifesaving procedure since the application of ASIF/TPS lasts about 60 min, whereas that of external fixation or use of Gantz clamp is about 10–15 min. Despite different characteristics of the B1, B2, and B3 pelvic fractures, all were characterized by rotation, which was dealt with the support point at the pubic symphysis to correct the pelvic rotation. However, this approach cannot be used for bilateral comminuted ramus fractures because it is impossible to implant a screw at the pubic symphysis in these cases.
The sturdy horizontal ring of the pelvic girdle is surmounted by the framework of the greater pelvis and is supported by the ischiopubic framework [15]. Vaidya et al. [17] reported that an internal fixator device constructed with polyaxial or monoaxial pedicle screws is stiffer than the 2-pin external fixator in distraction testing. In our previous clinical work, we found that after patients with type B pelvic fractures were fixed with two pedicle screws, some of them complained about suprapubic pain. We speculated that this was because of micro-movements between the pubic fracture sites. Fixing a third pedicle screw on the superior pubic ramus decreases the elasticity of the connecting rod resulting in decreased micro-movement between fracture sites, and decreased rates of suprapubic pain.
Hiesterman et al. [16] introduced a percutaneous method of subcutaneous fixation for the anterior pelvic ring using reconstruction plates and locking screws. But in patients that have a pure symphyseal lesion, they recommended ORIF of the pubic symphysis to achieve anatomic reduction. In the same way as in spinal operations, we used a distraction device or compression device in the reduction of pubic symphysis. For open book type B pelvic fractures, a compression device can be used to reduce the pubic symphysis separation. For closed book type B pelvic fracture, a distraction device is used as an effective reduction tool.
Plates and screws are always used in the fixation of the pubic body. The safety of the pubic body pedicle screw may be of some concern because of bladder, urethral canal, spermatic cord, and vaginal injury. For male or female patients, the length of the middle pedicle screw should be 50 or 45 mm, respectively. The inclination between the pubic symphysis and the horizontal plane is 40–45°. Pedicle screws should neither be inserted into the pubic symphysis, nor be put too close to the lateral pubis to prevent injury to the spermatic cord for males or to the round ligament of the uterus for females.
The indication for ASIF/TPS is for type B unstable pelvic fractures except for bilateral comminuted rami fractures. The technique is especially suited to type B (Tile classification) pelvic fractures. A minimally invasive operation cannot be performed by plates and screws, therefore, this kind of fracture cannot be reduced indirectly. On the other hand, pedicle screws can be used as a reduction tool and achieve definitive fixation. The relative contraindications for ASIF/TPS are for open pelvic fractures, comminuted bilateral rami fractures, and hemodynamically unstable patients. But because ASIF/TPS is a minimally invasive surgery, bladder or urethral injury should not be considered as an absolute contraindication to anterior internal fixation. We performed two ASIF/TPS operations after superpubic cystostomy, and no complications occurred. Extreme caution is needed to avoid the short distance between the upper margin of the symphysis pubis and the stoma.
In our study, there were no superficial or deep incision infections. The ilioinguinal approach and Stoppa approach are both widely used for the treatment of pelvic ring fractures [17, 18]. In our ASIF/TPS group, the mean operating time of first operation was 57.9 ± 11.5 min, the mean intraoperative blood loss of first operation was 34.8 ± 12.1 ml, no patient needed a blood transfusion, and the post operation hospitalization duration was 14.2 ± 3.0 days. Ponsen et al. [18, 22] reported that pelvic ring fractures accounted for only 24% of the patients and that as a minimally invasive surgery, ASIF/TPS greatly reduces the intraoperative blood loss, operating time, and duration of bed rest. Pavelka et al. [19] reported treatment of 257 patients with pelvic ring fractures. A total of 40 intra-operative complications were found in 31 (16%) patients, and the most frequent complications included malreduction in 14 patients (5%), nerve injury in 12 (5%), erroneous insertion of an implant in seven (3%), and vascular injury in six (2%). In our ASIF/TPS group, except for the two patients that had temporary lateral femoral cutaneous nerve numbness, no complication was found. As a minimally invasive surgery, ASIF/TPS can be performed safely based on the familiar anatomy of the pelvis. Heisterman et al. [16] reported that for bilateral pelvic lesions bilateral plates need to be implanted, a plate was subcutaneously fixed to each side of the midline, overlapping the length of the pubic tubercles at the pubic symphysis. One or two locking screws were placed into the pubic tubercles. In this case, the fracture cannot attain reduction indirectly, and a minimally invasive operation cannot be performed by plates and screws, while the pedicle screw system can be used as a reduction tool and achieve definitive fixation. Discrepancies among studies could be due to number of factors such as the types of fracture, the surgeon experience, the general state of the patient, and the characteristics of the healthcare systems.
The ASIF/TPS technique used in this study was different from the previously reported ASIF/TPS technique that places the connecting rod transverse at the AIIS level [10, 21]. Indeed, we placed the connecting rod in the oblique frontal plane. The connecting rod is bent along the upper side of the superior pubic rami. The benefits of this technique are: (1) avoiding compressing the abdomen; (2) convenient for the patient placed in a prone position; and (3) the direction of the polyaxial pedicle screws are limited, as it is difficult to put the connecting rod into the transverse level in morbidly obese patients.
For patients requiring anterior approach operations, ASIF/TPS can provide sufficient anterior stability and does not affect the prone position of the operation. Compared with ORIF using plates and screws, the advantages of ASIF/TPS are avoiding plate bending and the convenience of fracture reduction with compression or distraction devices.
The limitation of ASIF/TPS is apparent in its need of a second operation to remove the implant, thus in that respect it is not as convenient as an external fixation. Nevertheless, blood loss and length of operation and hospitalization are significantly shorter than that of single-procedure ORIF [7, 9, 17]. This study as an early clinical presentation of results is limited by the small number of patients. In addition, there was no comparator group using two pin internal fixator or other external fixator technique. Further studies with larger sample sizes and in multiple centers would add more support to these results.
In conclusion, minimally invasive fixation with ASIF/TPS could be an alternative technique for stabilizing type B pelvic fractures. ASIF/TPS decreases the risk of pin infection, and decreases operation time and blood loss.
References
Grover M, Edwards F, Hitchcock K, Stevens MM (2007) Clinical inquiries. What steps can reduce morbidity and mortality caused by hip fractures? J Fam Pract 56:944–946
Brunner LC, Eshilian-Oates L, Kuo TY (2003) Hip fractures in adults. Am Fam Physician 67:537–542
Templeman DC, Simpson T, Matta JM (2005) Surgical management of pelvic ring injuries. Instr Course Lect 54:395–400
Tachibana T, Yokoi H, Kirita M, Marukawa S, Yoshiya S (2009) Instability of the pelvic ring and injury severity can be predictors of death in patients with pelvic ring fractures: a retrospective study. J Orthop Traumatol 10:79–82
Biffl WL, Smith WR, Moore EE, Gonzalez RJ, Morgan SJ, Hennessey T, Offner PJ, Ray CE Jr, Franciose RJ, Burch JM (2001) Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Ann Surg 233:843–850
Mason W, Khan S, James C, Chesser T, Ward A (2005) Complications of temporary and definitive external fixation of pelvic ring injuries. Injury 36:599–604
Tucker MC, Nork SE, Simonian PT, Routt ML Jr (2000) Simple anterior pelvic external fixation. J Trauma 49:989–994
Palmer S, Fairbank AC, Bircher M (1997) Surgical complications and implications of external fixation of pelvic fractures. Injury 28:649–653
Mardanpour K, Rahbar M (2013) The outcome of surgically treated traumatic unstable pelvic fractures by open reduction and internal fixation. J Inj Violence Res 5:77–83
Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A (2012) Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma 26:1–8
Jiang ZL, Chen G (2011) Stabilization of unstable pelvic fractures with a novel internal–external fixator. Chin Med J (Engl) 124:4112–4114
Cole PA, Gauger EM, Anavian J, Ly TV, Morgan RA, Heddings AA (2012) Anterior pelvic external fixator versus subcutaneous internal fixator in the treatment of anterior ring pelvic fractures. J Orthop Trauma 26:269–277
Baque P, Trojani C, Delotte J, Sejor E, Senni-Buratti M, de Baque F, Bourgeon A (2005) Anatomical consequences of “open-book” pelvic ring disruption: a cadaver experimental study. Surg Radiol Anat 27:487–490
Majeed SA (1989) Grading the outcome of pelvic fractures. J Bone Joint Surg Br 71:304–306
Lierse W (1987) Applied anatomy of the pelvis. Springer, Berlin
Hiesterman TG, Hill BW, Cole PA (2012) Surgical technique: a percutaneous method of subcutaneous fixation for the anterior pelvic ring: the pelvic bridge. Clin Orthop Relat Res 470:2116–2123
Matta JM (1996) Indications for anterior fixation of pelvic fractures. Clin Orthop Relat Res 329:88–96
Ponsen KJ, Joosse P, Schigt A, Goslings JC, Luitse JS (2006) Internal fracture fixation using the Stoppa approach in pelvic ring and acetabular fractures: technical aspects and operative results. J Trauma 61:662–667
Pavelka T, Salasek M, Weisova D (2013) Complications associated with surgical treatment of pelvic ring fractures. Acta Chir Orthop Traumatol Cech 80:208–215
Apivatthakakul T, Rujiwattanapong N (2016) “Anterior subcutaneous pelvic internal fixator (INFIX), Is it safe?” A cadaveric study. Injury 47:2077–2080
Sellei RM, Dienstknecht T, Brücken D, Pfeifer R, Pape H-C (2013) Percutaneous anterior internal pelvic fixator. Oper Tech Orthop 23:33–37
Chaus GW, Weaver MJ (2015) Anterior subcutaneous internal fixation of the pelvis: placement of the INFIX. Oper Tech Orthop 25:262–269
Cole Peter A, Dyskin Evgeny A, Gilbertson Jeffrey A (2015) Minimally- invasive fixation for anterior pelvic ring disruptions. Injury 6:S27–S34
Acknowledgements
We thank Yilin Zhou for the 3D drawings. This work was financially supported by the Department of Major Projects of the Shanghai Science and Technology Committee Foundation (Grant No. 11JC1410400), the Shanghai Health System Important Disease Joint Research Project (Grant No. 2013 ZYJB0005), the Shanghai Shenkang Hospital Development Center Clinical Management Optimization Project (Grant No. SHDC20136031), and the State Key Program of National Natural Science Foundation of China (Grant No. 71432007).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work was financially supported by the Department of Major Projects of the Shanghai Science and Technology Committee Foundation (Grant No. 11JC1410400), the Shanghai Health System Important Disease Joint Research Project (Grant No. 2013 ZYJB0005), the Shanghai Shenkang Hospital Development Center Clinical Management Optimization Project (Grant No. SHDC20136031), and the State Key Program of National Natural Science Foundation of China (Grant No. 71432007).
Ethical approval
This study was approved by the medical ethics committee of Hospital (Approval 2014KY004). The study was conducted in compliance with the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wang, Q., Wang, Q. & Wang, J. Treatment of type B pelvic fracture using anterior subcutaneous internal fixator with triple pedicle screws: a new surgical technique. Arch Orthop Trauma Surg 137, 887–893 (2017). https://doi.org/10.1007/s00402-017-2701-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2701-3