Abstract
Introduction
Surgical treatment of unstable burst fractures of the thoracolumbar spine in the elderly population is highly variable with combined posterior and anterior stabilization (CPAS) and posterior augmented stabilization with cementation of the vertebral body (hybrid) being two commonly used techniques. The aim of this study was to compare the clinical and radiographic outcomes of CPAS versus hybrid stabilization for the treatment of unstable burst fractures of the thoracolumbar spine in patients aged between 60 and 70 years.
Materials and methods
A retrospective analysis was performed of all thoracolumbar burst fractures treated surgically in a single level I trauma center between June 2013 and February 2015. Two commonly used strategies of surgical stabilization were compared; the first consisted of initial posterior reduction and bisegmental stabilization, followed by additional anterior spondylodesis (CPAS); the second method comprised a hybrid technique with a posterior cement augmented bisegmental minimally invasive stabilization and kyphoplasty of the fractured vertebral body. Patients were evaluated clinically after a minimum follow-up of 18 months. The primary endpoint was the Oswestry Disability Index (ODI) at the latest follow-up. Secondary parameters of interest were length of in-hospital stay (LIHS), duration of surgery (DS), surgical revisions (SR), pain level (P-VAS), satisfaction level and the SF-36 score (PSC, MSC), the bisegmental postoperative Cobb angle, the reduction loss (RL), and all alignment parameters (pelvic tilt, pelvic incidence, sacral slope, lumbar lordosis, C7 plumb line).
Results
A total of 29 patients were included (17 females, 12 males, mean age 65.6 years ± 3.4 years). The following vertebral bodies were fractured: thoracic level (T) 12: n = 6; lumbar (L) 1: n = 14; L 2: n = 6; L 3: n = 3. CPAS was performed in 10 patients (34%), whereas the hybrid was carried out in 19 patients (66%). There were no statistical significant differences between both study groups regarding age, gender, trauma energy, fracture level, and fracture morphology. The latest follow-up was performed after a mean of 27 months (range 18–53 months). The LIHS between the treatment methods was statistically significant (p < 0.01); CPAS—mean 24 days versus hybrid—mean 12 days. DS was also significantly longer in patients treated with CPAS, 254 versus 95 min for the hybrid group (p < 0.01). No SR were necessary in either group. No significant differences were found regarding the clinical and radiological outcomes between the groups. The mean ODI score was 13.6 in the CPAS patients compared to 10.8 in the hybrid patients without significant differences between the groups. The majority of patients had no (80%) or minor (13%) limitations according to the ODI score. The P-VAS was 2.8 in CPAS and 2.9 in the hybrid group. RL was 7.1° in CPAS and 4.2° in the hybrid group.
Conclusions
CPAS and hybrid stabilization provide safe and promising short- and middle-term results in patients between 60 and 70 years of age. The majority of patients demonstrated no disability or minimal limitations with either technique. CPAS resulted in prolonged inpatient hospital stays, longer duration of surgery compared to hybrid stabilization without significant differences in clinical and radiological outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Operative reduction and stabilization is indicated in unstable vertebral body fractures of the thoracolumbar spine [1, 2]. Several strategies have been reported ranging from posterior-only stabilization to combined posterior and anterior stabilization (CPAS) [2,3,4,5]. CPAS with or without fusion is typically recommended in those fractures with relative destruction of the anterior column [6]. This is largely due to a study by McCormack et al. [1] in which a high number of implant failures were reported in patients with vertebral body fractures with significant comminution, severe kyphotic deformity, and/or a high degree of vertebral body involvement with posterior stabilization alone. One explanation for this is the presence of a concomitant intervertebral disc lesion, which are often associated with these fractures and disrupt osseous healing in many cases.
However, it should be considered that intervertebral disc lesions are mainly seen in young and adult patients [7]. In contrast, these lesions are uncommon in older patients, which is believed to be as a result of two main reasons; a greater intervertebral disc sclerosis and a reduced fracture threshold based on the impaired bone quality [8, 9]. As such, it is possible that intraosseous stabilization might be sufficient to maintain anterior column stability in the absence of disc pathology [10]. Therefore, performing a true CPAS, including discectomy, partial corpectomy, and anterior fusion in an elderly population may constitute overtreatment, particularly considering the potential-associated complications [3]. And perhaps, a less-invasive method of hybrid stabilization, consisting of cement augmentation of the fractured vertebral body in combination with short-segmental posterior stabilization might offer a solution with decreased morbidity in this patient group.
Therefore, the aim of this study was to compare the clinical and radiographic outcomes of CPAS versus hybrid strategy for the treatment of unstable burst fractures of the thoracolumbar spine in patients aged between 60 and 70 years. The hypothesis was that CPAS was more debilitating compared to hybrid stabilization but offered superior clinical and radiographic outcomes in the short to medium term.
Materials and methods
This retrospective study was performed at a single level I trauma center. The study was approved by the regional ethic committee. All patients admitted with spinal injury between June 2013 and February 2015were examined clinically and received conventional radiographs.
Computer tomography (CT) was carried out in all patients. In addition, magnetic resonance imaging (MRI) of the whole spine was performed in those patients without MRI contraindications.
Spinal stability was assessed using the new AO spine classification and the McCormack classification [1, 11]. All patients underwent a thorough neurological examination in accordance with the ASIA protocol. Patients with any neurologic deficit were excluded. Stable fractures were treated conservatively by adequate analgesia based on WHO [12] and physiotherapy-supervised mobilization without a corset or brace. Conventional radiographs were performed prior to and following mobilization and after 1 week in the standing position. Unstable fractures were treated by CPAS or the hybrid method. Instability was determined in all patients with type B-fractures as well as type A3 and A4 fractures with an associated load-share index of five and higher and in those patients with relevant reduction loss after mobilization [1, 11]. Inclusion and exclusion criteria are listed in Table 1.
Surgical techniques
The decision making regarding the method of treatment was carried out by the heads of the department (CEH, CJ) or in cases of immediate surgery by the spine surgeon on duty. CPAS consisted of posterior stabilization by an open approach using mainly monoaxial implants (USS II less common Viper, DepuySynthes) with cement augmentation of the pedicle screws. Anterior fusion was done by a minimally invasive thoracoscopic approach or by mini-lumbotomy using extandable titanium cages (Obelisc, Fa. Ulrich) (Fig. 1). Hybrid stabilization was performed by minimally invasive techniques using posterior cement augmented, bisegmental instrumentation (Matrix, DepuySynthes), and bilateral transpedicular kyphoplasty of the fractured vertebral body (Fig. 2).
69-year-old male patient who suffered from a bursting fracture of the second lumbar vertebral body type A 4 (McCormack 6) after falling from a ladder (a, b). Initially, a dorsal short-segmental cemented stabilization was performed (c, d). An anterior spondylodesis was performed afterward (e, f). At the latest follow-up after 26 months the patient was satisfied with low pain level (VAS: 2), low limitations (ODI: 10), and correct sagittal alignment (g)
68-year-old male patient who suffered incomplete burst split fracture of the second lumbar vertebral body type A 4 (McCormack 5) after falling from a ladder (a, b). A hybrid stabilization with additional kyphoplasty of the second lumbar vertebral body was performed 3 days after the accident (c, d). At the latest follow-up after 3 years the patient was happy without any pain (VAS: 0), low limitations (ODI: 10), and correct coronal and sagittal alignment (e, f)
Postoperative managemen
Postoperatively, all patients received conventional radiographs while standing. An additional CT scan was taken in cases of uncertainty of correct screw placement or anatomic reduction or in symptomatic patients. No brace or corset was used. Physiotherapy was initiated on the day after surgery to improve mobility and muscle strength. Clinical and conventional radiological assessment was performed at 2 and 6 weeks, and 3 and 12 months, and at the latest follow-up of at least 18 months postoperatively. A CT scan was performed in cases of moderate to high pain levels and uncertainty regarding bony fusion or on suspicion of screw loosening.
Outcome parameters
All patients were followed up for a minimum of 18 months after primary surgery. Initially the patients were contacted and asked if they were willing to participate. Scores were mailed to those patients who were willing to participate but did not wish further radiographs or did not want to visit the clinic. A total of three patients (12%) were not seen clinically and sent back their scores per mail. The others were evaluated clinically and radiologically and filled out the scores. An anterior-posterior X-ray centered on the injured vertebral body and lateral 36 in. views while standing were performed.
Outcome measures
The primary parameter of interest was the Oswestry Disability Index (ODI) at the most recent follow-up. Further outcome measures were length of in-hospital stay (LIHS: sum of in-hospital stays if there were more than one stay), duration of surgery (DS: sum of durations of all surgeries if there were more than one surgery), surgical revisions (SR), level of pain (P-VAS) (VAS 0–10 scale; 0: no pain, 10: maximal pain), level of satisfaction (S-VAS) (VAS 0–10 scale; 0: lowest satisfaction, 10: highest), and SF-36 score [physical summary component (PSC) and mental summary component (MSC)]. In addition, radiological parameters were measured in each case, which included postoperative and latest bisegmental sagittal Cobb angles, loss of reduction (LR), pelvic tilt, pelvic incidence, sacral slope, lumbar lordosis, thoracic kyphosis, C7 plumb line, and any signs of hardware loosening.
Statistical analysis
Statistical analysis was performed using standardized SPSS software 17.0 (SPSS®, Inc. Chicago, USA). Descriptive statistics were used. Two-sample Wilcoxon signed-rank tests were employed to compare outcomes parameters comparing differences between CPAS and hybrid. Fisher’s exact test was used to evaluate any associations between clinical outcome parameters and radiological outcome parameters as well as between regional radiological outcome parameters and alignment parameters. A significance level of 0.05 was used.
Results
A total of 29 patients met all inclusion criteria. The average age was 65.6 years (range 60–70 years) and the majority of patients were males (59%). Eight patients suffered from moderate- to high-energy traumas; 13 patients each had a history of low energy trauma. Most fractures were located at L 1 (n = 14) and T 12 (n = 6), less commonly at L 2 (n = 6) and L3 (n = 3). Most fractures were incomplete burst fractures A3 (n = 18). In addition, seven patients had A4 fractures, three patients A2 fractures with persistent pain or reduction loss during the first week after conservative treatment, and one patient suffered from a B-type lesion [11].
A total of ten patients (34%) were treated by CPAS. The other 19 patients were treated by hybrid stabilization. No significant differences were seen between both study groups (Table 2). The mean follow-up period was 27 months (range 18–53 months). The total loss of follow-up was 13.8% (n = 4; CPAS: 10.0%; hybrid: 15.8%; Table 3). In addition, three patients (12.0%: CPAS-group: 1; hybrid group: 2) were not willing to come to a clinical re-evaluation but filled out all clinical scores (ODI, SF 36, VAS) and sent it by mail.
Primary outcome
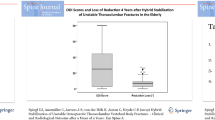
The ODI scores between both study groups are presented in Fig. 3. The vast majority of patients had no (CPAS: 55.6%; hybrid: 87.5%) or mild limitations (CPAS: 44.4%; hybrid: 6.3%). Moderate limitations were seen in one patient after hybrid stabilization (5.3%).
Secondary outcomes
Table 4 displays the results of the clinical outcome parameters. The pain situation was low to moderate in both study groups with mean pain scores, which were almost identical between both study groups. Similarly, the PSC and MSC of the SF 36 score were very similar in both study groups (PSC: 39.1 after CPAS and 37.3 after hybrid; MSC: 49.8 after CPAS and 47.7 after hybrid). The patient satisfaction was high in both study groups with a mean score of 8.0 after CPAS and 7.2 after hybrid without significant differences between both study groups. DS was significantly longer in patients treated by CPAS. Similarly, LIHS was significantly longer after CPAS. No significant differences were seen in loss of reduction between the study groups. All relevant radiologic outcome parameters are presented in Table 5. Pelvic tilt was significant higher in patients treated by CPAS. No further significant differences were seen between both study groups without any sagittal dysbalance. Altogether, there were no significant correlations between loss of reduction and clinical outcome scores as well as loss of reduction and all alignment parameters.
Discussion
The main finding of this study was that there were no statistically significant mid-term clinical differences between CPAS and hybrid stabilization for the treatment of unstable burst vertebral fractures of the thoracolumbar junction in a cohort of patients aged between 60 and 70 years. Most notably, CPAS was associated with a significantly longer inpatient stay and operative time. In general, the clinical outcomes were good or excellent in each treatment group with only moderate reduction loss and compensated alignment. The pain levels were low to moderate in both treatment groups with a mean pain level below three based on the VAS. In accordance to that, both the PSC and the MSC were only slightly lower compared to a norm collective of the same age group [13].
Two key considerations in the selection of the appropriate stabilization strategy in an elderly population with unstable burst vertebral fractures of the thoracolumbar spine are to maintain long-term structural stability while also endeavoring to limit the morbidity of invasive surgery. A combined posterior and minimal invasive thoracoscopic anterior stabilization has been found to provide excellent structural stability but, unfortunately, this comes at the cost of prolonged inpatient stays and an increased rate of complication [14]. It has since been shown that the stabilization of the anterior column in patients without intervertebral disc pathology with minimally invasive techniques and with intraosseous cement augmentation of the fractured vertebral body is capable of providing sufficient anterior support [10]. This is supported by Uchida et al. [5] who found no statistical differences in loss of reduction after anterior stabilization and hybrid stabilization in patients with osteoporotic thoracolumbar fractures. The key advantage of hybrid stabilization is that this can be performed in combination with the posterior stabilization through a posterior approach, which potentially carries less risk to the patient [10]. One of the potential additional risks of this technique is the possibility of clinical relevant cement embolism [15]. The findings of the current study would support the argument that hybrid stabilization provides equivalent structural support at short-term follow-up of 2 years. In addition, the surgery was consistently less time consuming that the CPAS surgery and resulted in a shorter hospital stay. Also, there were no reports of clinically relevant cement embolisms in the cohort examined.
Interestingly, patients treated with CPAS had a statistically significant higher pelvic tilt at the latest follow-up compared to patients treated with hybrid. A more pronounced pelvic tilt indicates increased pelvic retroversion [16], which might be compensation mechanism to avoid sagittal imbalance. Unfortunately, no lateral 36 in. views were done initially. Thus, it is unknown, if this difference is trauma related or a consequence of CPAS. No further statistically significant differences of any global and regional radiological parameters could be seen between both study groups. Particularly no higher reduction loss after CPAS was observed. Thus, a negative effect of CPAS on the sagittal balance is unlikely. In general, no effect on the clinical outcome was visible. It will be interesting follow the further course to evaluate any consequences in the long run.
It is important to recognize the technical differences between both study groups. There was a contrast between the invasiveness of each approach; patients treated with hybrid stabilization underwent a minimally invasive approach using polyaxial implants, whereas an open midline approach was utilized in all patients treated by CPAS using mainly monoaxial implants. The extent of soft tissue violation in the latter approach is likely to influence outcome. This is supported by a recent meta-analysis which demonstrated better clinical outcomes following minimally invasive dorsal stabilization [17] as a result of less tissue damage. Interestingly, the authors reported a better surgical reduction using an open approach but higher reduction loss afterwards. The authors argued that impaired functional control of posterior musculature in the postoperative period may be responsible for this. However, several of the included studies used a polyaxial screw-rod construct after both percutaneous and open approaches, which could explain these high rates of reduction loss [18].
Although structural stability is critical in spinal stabilization, the fate of the intervertebral disc is of paramount importance also. One of the arguments against the use of hybrid stabilization is that it fails to address the possibility of traumatic disc breakdown leading to persistent pain and regional kyphosis at a later stage. Sanders et al. [19] reported a 70% chance of development of severe intervertebral disc lesions during the first year after trauma despite healthy posttraumatic intervertebral disc morphology. The findings of the current study would conflict with these results as none of the patients within the hybrid stabilization group had clinical or radiological signs of relevant intervertebral disc pathology at the latest follow-up. It is possible that intervertebral disc lesions deteriorate; however, there were no signs for it on the conventional radiographs. These results are perhaps due to the age group contained within the cohort studied and the pathophysiological response of the intervertebral disc which occurs with aging. It would be very interesting to evaluate the accompanied intervertebral disc after hybrid stabilization by an additional MRI at the latest follow-up in further studies.
The indication for surgery in this patient cohort is of critical importance. There has been longstanding debate between operative and non-operative intervention in patients with thoracolumbar vertebral fractures [20,21,22]. Studies have demonstrated comparable clinical outcomes without surgery albeit with inferior radiological results, and therefore this must be considered on a case-by-case basis [2, 21]. In the current study, the indications for surgery were strictly adhered to and based on the likelihood of thoracolumbar spinal instability. Surgery was indicated in patients with unstable vertebral fracture and relevant destruction of the anterior column defined by McCormack scores 5 and higher according to the literature or those with relevant reduction loss during the first week of non-operative therapy including physiotherapeutic mobilization [23].
The authors acknowledge this study has limitation. This is a retrospective study and, therefore, it lacks randomization raising the possibility of selection bias. Patients treated with by CPAS might have been the more severely injured patients or more demanding patients leading to the indication of a more complex treatment strategy. Besides, the technical differences of surgery between both study groups regarding the invasiveness of approach and the chosen implants have to be mentioned, which can influence the clinical and radiological outcome. Next, the small patient number needs to be taken into account. In addition, this study deals with a short-term follow-up of 2 years. It is possible that the clinical outcome may deteriorate in the long run; however, longer follow-up periods are often associated with lower follow-up rates, particularly in an older patient cohort. In contrast, this study was able to achieve a high follow-up rate.
Conclusion
CPAS and hybrid stabilization provide safe and promising short- and middle-term results in patients between 60 and 70 years of age suffering from unstable thoracolumbar vertebral fractures. The majority of the ODI scores showed no or minimal limitations. Thereby, CPAS compared to hybrid stabilization gives rise to prolonged inpatient hospital stays, longer duration of surgery without significant differences in clinical and radiological outcomes. Thus, randomized studies are needed to rule out any relevant clinical differences between both therapy strategies for specific fracture types.
References
McCormack T, Karaikovic E, Gaines RW (1994) The load sharing classification of spine fractures. Spine (Phila Pa 1976) 19(15):1741–1744
Reinhold M, Knop C, Beisse R, Audige L, Kandziora F, Pizanis A, Pranzl R, Gercek E, Schultheiss M, Weckbach A, Buhren V, Blauth M (2010) Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, Internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur Spine J 19(10):1657–1676. https://doi.org/10.1007/s00586-010-1451-5
Spiegl UJ, Josten C, Devitt BM, Heyde CE (2017) Incomplete burst fractures of the thoracolumbar spine: a review of literature. Eur Spine J. https://doi.org/10.1007/s00586-017-5126-3
Uchida K, Kobayashi S, Matsuzaki M, Nakajima H, Shimada S, Yayama T, Sato R, Baba H (2006) Anterior versus posterior surgery for osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine. Eur Spine J 15(12):1759–1767. https://doi.org/10.1007/s00586-006-0106-z
Uchida K, Nakajima H, Yayama T, Miyazaki T, Hirai T, Kobayashi S, Chen K, Guerrero AR, Baba H (2010) Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: comparisons with posterior surgery without vertebroplasty and anterior surgery. J Neurosurg Spine 13(5):612–621. https://doi.org/10.3171/2010.5.SPINE09813
Denis F (1983) The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 8(8):817–831
Sander AL, Laurer H, Lehnert T, El Saman A, Eichler K, Vogl TJ, Marzi I (2013) A clinically useful classification of traumatic intervertebral disk lesions. AJR Am J Roentgenol 200(3):618–623. https://doi.org/10.2214/AJR.12.8748
Adams MA, McNally DS, Dolan P (1996) ‘Stress’ distributions inside intervertebral discs. The effects of age and degeneration. J Bone Jt Surg Br 78(6):965–972
Josten C, Heyde CE, Spiegl UJ (2016) Complex Pathologies of the Spine: Trauma meets Degeneration. Zeitschrift fur Orthopadie und Unfallchirurgie. https://doi.org/10.1055/s-0042-108344
Spiegl U, Jarvers JS, Heyde CE, Josten C (2017) Osteoporotic vertebral body fractures of the thoracolumbar spine: indications and techniques of a 360 degrees -stabilization. Eur J Trauma Emerg Surg 43(1):27–33. https://doi.org/10.1007/s00068-016-0751-9
Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, Reinhold M, Aarabi B, Kandziora F, Chapman J, Shanmuganathan R, Fehlings M, Vialle L, Injury AOSC, Trauma Knowledge F (2013) AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 38(23):2028–2037. https://doi.org/10.1097/BRS.0b013e3182a8a381
WHO (1996) Cancer pain relief: with a guide to opioid availability. World Health Organization, Geneva
Ellert U, Kurth B-M (2004) Methodological views on the SF-36 summary scores based on the adult German population. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 47:1027–1032
Hoffmann C, Spiegl UJ, Hauck S, Buhren V, Gonschorek O (2013) What is the effect of ventral thoracoscopic spondylodesis (VTS) on elderly patients and what is the medium-term outcome?. Zeitschrift fur Orthopadie Unfallchirurgie 151(3):257–263. https://doi.org/10.1055/s-0032-1328522
Riesner HJ, Kiupel K, Lang P, Stuby F, Friemert B, Palm HG (2016) Clinical relevance of cement leakage after radiofrequency kyphoplasty vs. balloon kyphoplasty: a prospective randomised study. Zeitschrift fur Orthopadie Unfallchirurgie 154(4):370–376. https://doi.org/10.1055/s-0042-104069
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20(4):451–462
Sun XY, Zhang XN, Hai Y (2017) Percutaneous versus traditional and paraspinal posterior open approaches for treatment of thoracolumbar fractures without neurologic deficit: a meta-analysis. Eur Spine J 26(5):1418–1431. https://doi.org/10.1007/s00586-016-4818-4
Kubosch D, Kubosch EJ, Gueorguiev B, Zderic I, Windolf M, Izadpanah K, Sudkamp NP, Strohm PC (2016) Biomechanical investigation of a minimally invasive posterior spine stabilization system in comparison to the universal spinal system (USS). BMC Musculoskelet Disord 17:134. https://doi.org/10.1186/s12891-016-0983-1
Sander AL, Lehnert T, El Saman A, Eichler K, Marzi I, Laurer H (2014) Outcome of traumatic intervertebral disk lesions after stabilization by internal fixator. AJR Am J Roentgenol 203(1):140–145. https://doi.org/10.2214/AJR.13.11590
Wood KB, Buttermann GR, Phukan R, Harrod CC, Mehbod A, Shannon B, Bono CM, Harris MB (2015) Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective randomized study with follow-up at sixteen to twenty-two years. J Bone Jt Surg 97(1):3–9. https://doi.org/10.2106/JBJS.N.00226
Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, Rommens PM, ten Duis HJ, Patka P (2006) Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) 31(25):2881–2890
Scholz M, Kandziora F, Tschauder T, Kremer M, Pingel A (2017) Prospective randomized controlled comparison of posterior vs. posterior-anterior stabilization of thoracolumbar incomplete cranial burst fractures in neurological intact patients: the RASPUTHINE pilot study. Eur Spine J. https://doi.org/10.1007/s00586-017-5356-4
Spiegl UJ, Jarvers JS, Heyde CE, Glasmacher S, Von der Hoh N, Josten C (2015) Delayed indications for additive ventral treatment of thoracolumbar burst fractures: What correction loss is to be expected. Der Unfallchirurg. https://doi.org/10.1007/s00113-015-0056-1
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spiegl, U.J., Devitt, B.M., Kasivskiy, I. et al. Comparison of combined posterior and anterior spondylodesis versus hybrid stabilization in unstable burst fractures at the thoracolumbar spine in patients between 60 and 70 years of age. Arch Orthop Trauma Surg 138, 1407–1414 (2018). https://doi.org/10.1007/s00402-018-2993-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2993-y