Abstract
Background
The purpose of this retrospective study was to report on the functional outcome after both open and arthroscopic rotator cuff (RC) repair in normal weight, pre-obese and obese patients. It was hypothesized that obesity is a negative prognostic factor for clinical outcome and failure for the RC repair.
Methods
One hundred and forty-six patients who underwent either open or arthroscopic rotator cuff repair between 2006 and 2010 were included in this study. Seventy-five patients (56.7 ± 10.1 years of age) after open RC repair and 71 patients (59.0 ± 9.1 years of age) treated arthroscopically were available for evaluation. In both groups a double-row reconstruction was performed. Patients were divided in three groups according to their body-mass index. The mean follow-up was at 43 ± 16 (minimum 24) months. At follow-up, the clinical outcome was assessed by the DASH and Constant score. An ultrasound of both shoulders was performed in all patients.
Results
The mean BMI was 28.3 ± 5.3 in the arthroscopic group and 27.7 ± 4.3 in the open group. Overall, in both groups similar clinical results were noted [Constant–Murley score 78.3 ± 18.2 arthroscopic vs. 77.0 ± 21.8 for open surgery; DASH 12.7 ± 18.2 arthroscopic vs. 15.6 ± 21.6 for open surgery (p = 0.81)]. Both the failure rate and the clinical outcome were significantly worse for obese patients (BMI > 30, p = 0.007). The failure rate was 15.8% for the normal-weight patients, 8.2% in the pre-obese group and in the obese group 28.6%. The RC repair failure occurred in 11 cases in both groups after arthroscopic or open treatment (15.0%).
Conclusions
Both the arthroscopic and the open approach showed equivalent clinical results and failure rates. Obesity (BMI > 30) causes less favorable results in the Constant and DASH scores and showed higher re-tear rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotator cuff (RC) lesions are the most common reason for shoulder pain, dysfunction and discomfort [1, 2]. It is commonly acknowledged that the prevalence of rotator cuff tears increases with age [3,4,5]. Various reports indicate that rotator cuff lesions occur in up to 22% of all patients over 65 years of age [6]. Partial thickness tears remain difficult to identify both in clinical tests and with magnetic resonance imaging [7]. However, the lesion size increases without surgical treatment [8]. Initially repairable lesions develop to irreparable lesions, while the acromio-humeral distance decreases with an increase of gleno-humeral arthritis after 4–5 years. However, the ideal therapy of RC lesions is still controversial including conservative and operative treatment, while in case of an operation the arthroscopic approach has advantages over an open and mini-open technique [9, 10]. This includes less soft tissue damage, reduced pain, faster rehabilitation, lower postoperative infection rates avoiding accordingly partial deltoid muscle insufficiencies and shoulder stiffness. At later stages the clinical results do not show significant differences in comparison of open or arthroscopic surgery [11].
The results of operatively reconstructed RC lesions are in general good and have been improved during the last 15 years using improved anchor systems with lower re-tear rates using newer self-reinforcing knotless systems [12]. There is still an ongoing intense research effort to understand biomechanics, treatment results and prognostic factors making RC lesions one of the most highly investigated orthopedic pathology. This fact is reflected obviously in the review article by McElvany et al. including 2.383 studies with 108 inclusion criteria from 1980 till 2012 [13].
A major concern after RC repair is still the occurrence of re-tears or biomechanical healing failure with a rate of 27 up to 46% depending on rupture patterns, RC morphology and surgical technique, such as single and double-row reconstruction [14,15,16]. This is of specific interest as RC re-tears seem to occur between 12 and 24 months postoperatively as recently shown in a MRI based follow-up study [17].
Additionally, many biomechanical studies have been performed to optimize stability and, therefore, reduce healing failure. Moreover, animal studies examining tendon-to-bone healing showed that the repair tissue differs dramatically from the native bone–tendon interface. This might also correlate with healing failures in human shoulders [18,19,20].
Identified negative prognostic factors for RC re-tears after reconstruction are fatty degeneration of the RC muscle according to Goutailler et al. [21] and according to Thomazeau [22]. Relevant further factors are the tear size according to Bateman et al. and the tendon retraction according to Patte et al. leading to impaired clinical outcome and higher re-tear rates for greater lesion sizes [21, 23, 24]. Another independent negative prognostic factor was identified by Chung et al. showing that osteoporosis is accompanied with higher failure rates [25].
The aim of this study was to correlate, if obesity was a risk factor for RC repair as obesity was proven to be a significant negative prognostic factor for postoperative complications in orthopedic trauma surgery [26]. The hypothesis of this study was, therefore, that obesity causes poorer Constant and DASH scores and also provokes higher re-tear rates after mini-open and arthroscopic double-row RC reconstruction.
To the best to our knowledge there are no comparable studies available, yet.
Materials and methods
Study population
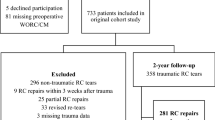
Inclusion criteria were a complete rupture of one of the RC tendons, a reconstruction with anchors and a non-operated contra-lateral shoulder as well as surgery between 2006 and 2010. Two hundred and fifty-three patients were identified of which 146 patients with RC tears were included retrospectively in this case–control study of operatively treated RC tears. Exclusion criteria for the study were death (3), severe illness (7), residence abroad (21) or travel distance to our clinic of more than 2 h (76).
Seventy-five patients were treated using a mini-open technique and 71 patients arthroscopically by two different surgeons in a single-center for sports injuries and arthroscopic surgery. The operative procedure was standardized and identical for the mini-open and arthroscopic group using for the medial row resorbable Bio-Corkscrew FT Anchors (Arthrex) and for the lateral strutting row the knotless resorbable SwiveLock© Anchor (Arthrex). In all cases simultaneous subacromial decompression and a tenotomy or tenodesis of the long biceps tendon was performed. The ages of the subgroups were similar with 59.0 ± 9.1 years in the arthroscopy group and 56.7 ± 10.1 in the mini-open group. The analysis and classification of the body-mass index (BMI) was performed according to the WHO definition with three categories [27]: BMI normal (n = 38 patients, BMI between 18.5 and 25), BMI pre-obese (n = 73 patients, BMI between 25 and 30) and BMI obese (n = 30 patients, BMI over 30). Table 1 shows more detailed information of the patients' weight pattern.
The tear size (TS) was categorized in four types: TS group 1 (n = 36): small rupture of a single tendon up to Bateman I/Patte (1) TS-group 2 (n = 56): rupture of a single tendon up to Bateman II/Patte (2) TS-group 3 (n = 44): rupture of several tendons up to Bateman III/Patte (3) TS-group 4 (n = 10): rupture of several tendons up to Bateman IV/Patte 3.
Follow-up examinations took place at a mean of 43 ± 16 months after initial surgery (minimum of 24 months).
None of the patients had relevant body-weight change overtime from surgery to time of examination.
The study was performed with the consent of the local ethical committee.
Outcome measures
RC integrity was examined by means of a high-resolution ultrasound of all patients using a Siemens Sono site with 13.5 MHz linear-array probe. In all patients both shoulders were examined and the integrity was judged in a standardized multi-planar manner as previously recommended [28, 29].
The follow-up examination included the DASH score and Constant–Murley shoulder score [30]. The range of motion was noted and shoulder pain was assessed by using the VAS (visual analogue scale).
Statistical analysis
The statistical analysis was performed with Stata software v.10.0. Nonparametric tests were used depending on the sample size. Quantitative variables were tested by the Wilcoxon test for paired groups. A “p” value of less than 0.05 was considered to be statistically significant.
Results
Figure 1 shows a homogeneous distribution of the TS in each BMI group (Fig. 1). This analysis was necessary to objectify an independent influence of the BMI on the clinical outcome and re-tear rate.
In the clinical examinations obese patients had significantly worse results in the DASH and Constant–Murley score at the follow-up examination (Fig. 2). Interestingly there were no differences between normal-weight patients and pre-obese patients (Constant–Murley p = 0.22; DASH p = 0.47).
In comparison, there are similar clinical results with no significant differences for both the arthroscopic and the open treatment: Constant–Murley score 78.3 ± 18.2 arthroscopic vs. 77.0 ± 21.8 for open surgery; DASH 12.7 ± 18.2 arthroscopic vs. 15.6 ± 21.6 for open surgery (p = 0.81). The subjective results showed a median of 27.6 ± 4.4 points after arthroscopic reconstruction and 27.4 ± 4.4 after mini-open procedure. The objective results revealed a median score of 39.2 ± 3.7 (arthroscopic) vs. 38.5 ± 3.6 (mini-open) without significant differences. A detailed overview is provided in Table 2.
The length of surgery was not longer in obese patients (57.2 min ± 10.2) compared to the other groups (normal 67.9 min ± 22.3/pre-obese 74.3 min ± 25.3).
The ultrasound results between mini-open and arthroscopic surgery were equivalent without relevant differences. An overview of the ultrasound follow-up is given in Table 3 [28, 29].
The re-tear rate revealed 15.8% in BMI-group normal; 8.2% in BMI-group pre-obese and 28.6% in the BMI-group obese (p = 0.0086), respectively. However, there was no significant difference between the BMI-group normal and the BMI-group pre-obese (p = 0.12). In addition, the range of motion (ROM) was significantly limited in the obese group in comparison to the pre-obese group for abduction (p = 0.0401), flexion (p = 0.0007), outward rotation (p = 0.0155), inward rotation 90° (p = 0.008) and outward rotation 90° (p = 0.0151)—(Fig. 3).
The analysis of postoperative quality of life due to the SF-36 and EQ-5D showed also significantly impaired results for obese patients (Fig. 4).
The independent analysis of the RC repair failure according to TS showed for group TS 1 a re-tear rate of 11.1%, and for the group TS 2 a re-tear rate of 12.5% (TS 1 vs. TS2 p = 1.00). Bigger lesions as for TS 3 had a re-tear rate of 18.2% (TS 1 vs. TS3 p = 0.53), and for the group TS 4 a re-tear rate of 30.0% (TS 1 vs. TS 4 p = 0.16).
Discussion
The key finding of this study was that obesity causes less favorable results in the Constant and DASH scores and showed higher re-tear rates after rotator cuff repair. The same negative influence was found for a BMI > 30 for the mini-open as well as the arthroscopic RC repair.
Risk factors for rotator cuff tears can be grouped in anatomical, therefore, mechanical, sports and lifestyle factors, metabolic and epidemic factors. Anatomic risk factors are accepted to derive from outlet and inlet shoulder impingement [31]. Inlet impingement meaning shoulder dysfunction due to dysbalanced rotator cuff tears, tendinitis calcarea or shoulder instability. As reported by Bigliani osteoarthritis of the AC joint, an overhanging acromion and a narrow subacromial space are accepted mechanical outlet risk factors [32].
Sportsman affected by rotator cuff lesions are mainly reported to be found in sports where a rotation in the shoulder is an essential element such as in handball, baseball, javelin or in gymnastics [33, 34].
Nowadays the focus is also on metabolic factors for the prevalence of RC tears. There is an interesting published case–control study of 381 patients with RC tears treated by arthroscopy and 220 control patients. This study proofed that obesity, measured through BMI and body fat is a significant risk factor for the occurrence and severity of a rotator cuff tear [35]. A possible explanation might be that higher mechanical strain due to arm weight on the shoulder joint and consecutively on the RC tendons may have negative effects.
In a recently published study with 206 patients Djerbi et al. reported on cardiovascular risk factors for the appearance of RC tears. This study identified smoking, high blood pressure, diabetes (DM), alcoholism, dyslipidemia, obesity and cardiovascular history as such factors [14].
Other recent studies report that also hypertension [36] and body fat [35] are proven risk factors for RC tears.
Kim et al. reported on postoperative outcomes after RC repair of patients suffering from metabolic syndrome with a high BMI, DM and dyslipidemia [37]. Significantly higher re-tear rates were seen in this study group of 180 patients for such patients. However, as obese patients tend to have DM and dyslipidemia it is difficult to separate BMI, DM and dyslipidemia as independent factors.
Warrender et al. already described obesity as having a negative impact on the functional outcomes and recovery in patients with a BMI > 30 [38]. Furthermore, it is generally known that DM and hypercholesterolemia have a negative influence on tendon healing [39]. However, although DM and dyslipidemia can negatively affect clinical outcomes, Dhar et al. found no difference in re-tear rates [40]. This is in contrast to our results as this analysis revealed that evident obesity causes in general inferior clinical results and reduced multi directional range of motion as well as higher re-tear rates.
The presented study has certain limitations. The retrospective design provides less evidence than prospective studies. As aforementioned healing after RC repair is multi-factorial and does also depend on other measurable factors such as tear size, tendon quality and muscle atrophy or as in this study BMI. Simple mechanical deficits such as poor bone quality or inadequate suture fixation as well as intense or early active mobilization may be further reasons for healing failure. The preoperative fatty degeneration of the RC was not measured and ultrasound was used as reference to control cuff integrity. Therefore, a logically consistent study should prospectively evaluate RC integrity after double-row repair by MRI performing a multi-factorial analysis (RC size, muscle atrophy, anatomic patterns etc.) to objectivize a hierarchy of these aforementioned risk and influencing factors. However, in this study, obesity could be identified as an independent negative factor with higher re-tear rates after cuff repair.
Conclusion
Obesity (BMI > 30) showed higher re-tear rates for both mini-open and arthroscopic RC repair. In addition, obesity causes less favorable results in ROM as well as in the Constant and DASH scores.
Bearing these results in mind, one must reflect indications for cuff repair in obese patients and also motivate these patients for a healthier lifestyle.
References
Bhatia S, Greenspoon JA, Horan MP, Warth RJ, Millett PJ (2015) Two-year outcomes after arthroscopic rotator cuff repair in recreational athletes older than 70 years. Am J Sports Med 43(7):1737–1742
Mascarenhas R, Chalmers PN, Sayegh ET, Bhandari M, Verma NN, Cole BJ, Romeo AA (2014) Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: a systematic review of overlapping meta-analyses. Arthroscopy 30(9):1156–1165
Pauly S, Stahnke K, Klatte-Schulz F, Wildemann B, Scheibel M, Greiner S (2015) Do patient age and sex influence tendon cell biology and clinical/radiographic outcomes after rotator cuff repair? Am J Sports Med 43(3):549–556
Charousset C, Bellaiche L, Kalra K, Petrover D (2010) Arthroscopic repair of full-thickness rotator cuff tears: is there tendon healing in patients aged 65 years or older? Arthroscopy 26(3):302–309
Loew M, Magosch P, Lichtenberg S, Habermeyer P, Porschke F (2015) How to discriminate between acute traumatic and chronic degenerative rotator cuff lesions: an analysis of specific criteria on radiography and magnetic resonance imaging. J Shoulder Elbow Surg 24(11):1685–1693
Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB (1995) Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Jt Surg Am 77(1):10–15
Brockmeyer M, Schmitt C, Haupert A, Kohn D, Lorbach O (2017) Limited diagnostic accuracy of magnetic resonance imaging and clinical tests for detecting partial-thickness tears of the rotator cuff. Arch Orthop Trauma Surg 137(12):1719–1724
Zingg PO, Jost B, Sukthankar A, Buhler M, Pfirrmann CW, Gerber C (2007) Clinical and structural outcomes of nonoperative management of massive rotator cuff tears. J Bone Jt Surg Am 89(9):1928–1934
Severud EL, Ruotolo C, Abbott DD, Nottage WM (2003) All-arthroscopic versus mini-open rotator cuff repair: a long-term retrospective outcome comparison. Arthroscopy 19(3):234–238
Walton JR, Murrell GA (2012) A two-year clinical outcomes study of 400 patients, comparing open surgery and arthroscopy for rotator cuff repair. Bone Jt Res 1(9):210–217
Bayle X, Pham TT, Faruch M, Gobet A, Mansat P, Bonnevialle N (2017) No difference in outcome for open versus arthroscopic rotator cuff repair: a prospective comparative trial. Arch Orthop Trauma Surg 137(12):1707–1712
Millett PJ, Espinoza C, Horan MP, Ho CP, Warth RJ, Dornan GJ, Christoph Katthagen J (2017) Predictors of outcomes after arthroscopic transosseous equivalent rotator cuff repair in 155 cases: a propensity score weighted analysis of knotted and knotless self-reinforcing repair techniques at a minimum of 2 years. Arch Orthop Trauma Surg 137(10):1399–1408
McElvany MD, McGoldrick E, Gee AO, Neradilek MB, Matsen FA 3rd (2015) Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Med 43(2):491–500
Djerbi I, Chammas M, Mirous MP, Lazerges C, Coulet B, French Society For S, Elbow (2015) Impact of cardiovascular risk factor on the prevalence and severity of symptomatic full-thickness rotator cuff tears. Orthop Traumatol Surg Res 101 (6 Suppl):S269-273
Saccomanno MF, Sircana G, Cazzato G, Donati F, Randelli P, Milano G (2015) Prognostic factors influencing the outcome of rotator cuff repair: a systematic review. Knee Surg Sports Traumatol Arthrosc 24 (12):3809–3819
Kim YK, Moon SH, Cho SH (2013) Treatment outcomes of single- versus double-row repair for larger than medium-sized rotator cuff tears: the effect of preoperative remnant tendon length. Am J Sports Med 41(10):2270–2277
Stahnke K, Nikulka C, Diederichs G, Haneveld H, Scheibel M, Gerhardt C (2016) Serial MRI evaluation following arthroscopic rotator cuff repair in double-row technique. Arch Orthop Trauma Surg 136(5):665–672
Kovacevic D, Rodeo SA (2008) Biological augmentation of rotator cuff tendon repair. Clin Orthop Relat Res 466(3):622–633
Cheung EV, Silverio L, Sperling JW (2010) Strategies in biologic augmentation of rotator cuff repair: a review. Clin Orthop Relat Res 468(6):1476–1484
Rodeo SA (2007) Biologic augmentation of rotator cuff tendon repair. J Shoulder Elbow Surg 16(5 Suppl):S191-197
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res (304):78–83
Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F (1996) Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand 67(3):264–268
Park JS, Park HJ, Kim SH, Oh JH (2015) Prognostic factors affecting rotator cuff healing after arthroscopic repair in small to medium-sized tears. Am J Sports Med 43(10):2386–2392
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res (254):81–86
Chung SW, Oh JH, Gong HS, Kim JY, Kim SH (2011) Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med 39(10):2099–2107
Whiting PS, White-Dzuro GA, Avilucea FR, Dodd AC, Lakomkin N, Obremskey WT, Collinge CA, Sethi MK (2017) Body mass index predicts perioperative complications following orthopaedic trauma surgery: an ACS-NSQIP analysis. Eur J Trauma Emerg Surg 43(2):255–264
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, Batsis JA, Sert-Kuniyoshi FH, Lopez-Jimenez F (2008) Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes 32(6):959–966
Roy JS, Braen C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, Bureau NJ, Fremont P (2015) Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med 49(20):1316–1328
Collin P, Yoshida M, Delarue A, Lucas C, Jossaume T, Ladermann A, French Society for S Elbow (2015) Evaluating postoperative rotator cuff healing: prospective comparison of MRI and ultrasound. Orthop Traumatol Surg Res 101(6 Suppl):S265–S268
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res (214):160–164
Balke M, Banerjee M, Vogler T, Akoto R, Bouillon B, Liem D (2014) Acromial morphology in patients with calcific tendinitis of the shoulder. Knee Surg Sports Traumatol Arthrosc 22 (2):415–421
Nicholson GP, Goodman DA, Flatow EL, Bigliani LU (1996) The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg 5(1):1–11
Doyscher R, Kraus K, Finke B, Scheibel M (2014) Acute and overuse injuries of the shoulder in sports. Der Orthop 43(3):202–208
Beitzel K, Zandt JF, Buchmann S, Beitzel KI, Schwirtz A, Imhoff AB, Brucker PU (2016) Structural and biomechanical changes in shoulders of junior javelin throwers: a comprehensive evaluation as a proof of concept for a preventive exercise protocol. Knee Surg Sports Traumatol Arthrosc 24(6):1931–1942
Gumina S, Candela V, Passaretti D, Latino G, Venditto T, Mariani L, Santilli V (2014) The association between body fat and rotator cuff tear: the influence on rotator cuff tear sizes. J Shoulder Elbow Surg 23(11):1669–1674
Gumina S, Arceri V, Carbone S, Albino P, Passaretti D, Campagna V, Fagnani C, Postacchini F (2013) The association between arterial hypertension and rotator cuff tear: the influence on rotator cuff tear sizes. J Shoulder Elbow Surg 22(2):229–232
Kim YK, Jung KH, Kim JW, Kim US, Hwang DH (2017) Factors affecting rotator cuff integrity after arthroscopic repair for medium-sized or larger cuff tears: a retrospective cohort study. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2017.11.016
Warrender WJ, Brown OL, Abboud JA (2011) Outcomes of arthroscopic rotator cuff repairs in obese patients. J Shoulder Elbow Surg 20(6):961–967
Abtahi AM, Granger EK, Tashjian RZ (2015) Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop 6(2):211–220
Dhar Y, Anakwenze OA, Steele B, Lozano S, Abboud JA (2013) Arthroscopic rotator cuff repair: impact of diabetes mellitus on patient outcomes. Physician Sports Med 41(1):22–29
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ateschrang, A., Eggensperger, F., Ahrend, M.D. et al. Obesity causes poorer clinical results and higher re-tear rates in rotator cuff repair. Arch Orthop Trauma Surg 138, 835–842 (2018). https://doi.org/10.1007/s00402-018-2921-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-2921-1