Abstract
Introduction
The reliable diagnosis of partial-thickness tears of the rotator cuff is still elusive in clinical practise. Therefore, the purpose of the study was to determine the diagnostic accuracy of MR imaging and clinical tests for detecting partial-thickness tears of the rotator cuff as well as the combination of these parameters.
Materials and methods
334 consecutive shoulder arthroscopies for rotator cuff pathologies performed during the time period between 2010 and 2012 were analyzed retrospectively for the findings of common clinical signs for rotator cuff lesions and preoperative MR imaging. These were compared with the intraoperative arthroscopic findings as “gold standard”. The reports of the MR imaging were evaluated with regard to the integrity of the rotator cuff. The Ellman Classification was used to define partial-thickness tears of the rotator cuff in accordance with the arthroscopic findings. Descriptive statistics, sensitivity, specificity, positive and negative predictive value were calculated.
Results
MR imaging showed 80 partial-thickness and 70 full-thickness tears of the rotator cuff. The arthroscopic examination confirmed 64 partial-thickness tears of which 52 needed debridement or refixation of the rotator cuff. Sensitivity for MR imaging to identify partial-thickness tears was 51.6%, specificity 77.2%, positive predictive value 41.3% and negative predictive value 83.7%. For the Jobe-test, sensitivity was 64.1%, specificity 43.2%, positive predictive value 25.9% and negative predictive value 79.5%. Sensitivity for the Impingement-sign was 76.7%, specificity 46.6%, positive predictive value 30.8% and negative predictive value 86.5%. For the combination of MR imaging, Jobe-test and Impingement-sign sensitivity was 46.9%, specificity 85.4%, positive predictive value 50% and negative predictive value 83.8%.
Conclusions
The diagnostic accuracy of MR imaging and clinical tests (Jobe-test and Impingement-sign) alone is limited for detecting partial-thickness tears of the rotator cuff. Additionally, the combination of MR imaging and clinical tests does not improve diagnostic accuracy.
Level of evidence
Level II, Diagnostic study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Different pathologies of the rotator cuff are known, including tendinosis, partial-thickness tears, full-thickness tears of the tendon and rotator cuff arthropathy. The incidence of partial-thickness tears of the rotator cuff is not clearly defined and varied within the recent literature [1]. Sher et al. [2] describe a prevalence of 20% for a partial-thickness tear of the rotator cuff within their study examining 96 asymptomatic shoulders by MR imaging. Tendinosis and partial-thickness tears of the supraspinatus tendon occur in heavy sporting activity and in middle-aged patients. The incidence for partial-thickness tears seems to increase with increasing age of the patients [1]. Especially in patients aged 50–60 years, partial-thickness tears may be diagnosed frequently. Commonly, the anterior parts of the supraspinatus tendon are affected. The surgical treatment of symptomatic partial-thickness tears of the supraspinatus tendon is controversial with different arthroscopic treatment options depending on extent of the partial-thickness tear, quality of the tendon and individual patient characteristics. Treatment options include arthroscopic debridement, acromioplasty, transtendon in situ suture repair, and full-thickness tear conversion and repair. If the non-operative treatment fails and 50% or more of the tendon thickness is involved, it is accepted practise to perform surgical repair of the rotator cuff tendon [1]. The accurate diagnosis of partial-thickness tears of the rotator cuff, in contrast to full-thickness tears of the rotator cuff, remains difficult for the clinical examination as well as the diagnostic imaging procedures like MR or sonographic imaging [3, 4]. MR imaging has shown high diagnostic accuracy for full-thickness tears of the rotator cuff [4]. False-positive or false-negative results for MR imaging concerning partial-thickness tears of the rotator cuff are frequently seen [5]. Within the clinical examination, the Impingement-signs and the clinical tests for the supraspinatus tendon might be positive. Several studies have previously examined the diagnostic accuracy of MR imaging or clinical tests to detect tears of the rotator cuff [6, 7], but the results of correlating these parameters with each other are rare. Therefore, the purpose of the present study was to evaluate the diagnostic accuracy of the clinical examination and MR imaging, and especially the combination of clinical tests (Jobe-test and Impingement-sign) and MR imaging, to determine partial-thickness tears of the rotator cuff in comparison to the surgical findings.
Materials and methods
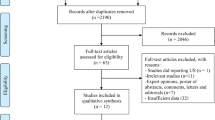
This study retrospectively analyzed 334 consecutive patients who underwent shoulder arthroscopy for rotator cuff pathologies between January 2010 and December 2012 at our institution. The study was approved by the Institutional Research Coordinator and the head of the department in January 2013. Arthroscopic revision surgeries and arthroscopic joint lavages in cases of septic shoulder arthritis were excluded. The results of different preoperatively determined common clinical tests for rotator cuff pathologies, the preoperative MR imaging, and the arthroscopic findings as “gold standard”, were fully recorded for 270 cases. Within the clinical testing, the Jobe-test and the Impingement-signs were performed. The radiology reports of the MR imaging were evaluated with regard to the integrity of the rotator cuff categorizing the rotator cuff as intact, partially or completely torn (Fig. 1). All radiologists who were involved within the study are specialists in musculoskeletal radiology. The Ellman Classification [8] (Fig. 2 and Table 1) was used to grade partial-thickness tears of the rotator cuff in accordance with the arthroscopic diagnosis. The data required were taken from the patient file and the surgical report. Descriptive statistics for MR imaging, clinical tests and arthroscopic findings concerning the integrity of the rotator cuff were performed. Further statistical analysis was determined for the sensitivity, specificity, positive predictive value, and negative predictive value of the MRI findings, the Impingement-test and the Jobe-test as well as the combination of these parameters. Statistical analysis was performed by using Microsoft Excel® and IBM SPSS Statistics®.
Results
For 270 patients (175 men and 95 women) the relevant data were completely registered. The mean age of this cohort was 54 years [19–81]. MR imaging showed 80 partial-thickness and 70 full-thickness tears of the rotator cuff. The rotator cuff tendon was described as intact in 120 cases. The arthroscopic diagnosis verified 64 partial-thickness tears of which 52 needed specific surgical treatment (debridement: n = 33; refixation n = 19). In addition 95 full-thickness tears of the rotator cuff were confirmed arthroscopically and in 111 cases the rotator cuff tendon was classified as intact (Table 2). The results for the clinical tests and arthroscopic findings concerning the integrity of the rotator cuff are shown in Table 3a, b. The frequency distribution regarding the Ellman Classification is presented in Table 4. The sensitivity for MR imaging to identify a partial-thickness lesion of the rotator cuff was 51.6%, the specificity 77.2%. The positive predictive value was 41.3% and the negative predictive value was 83.7%. The sensitivity for the Jobe-test was 64.1% and the specificity was 43.2%. For the Jobe-test, a positive predictive value of 25.9% and a negative predictive value of 79.5% were found. The sensitivity for the Impingement-sign was 76.7% and the specificity was 46.6%. For the Impingement-sign, a positive predictive value of 30.8% and a negative predictive value of 86.5% were calculated. For the combination of MR imaging, Jobe-test and Impingement-sign sensitivity was 46.9%, specificity was 85.4%, positive predictive value was 50% and negative predictive value was 83.8% (Table 5).
Discussion
The most important results of the present study are that there was limited accuracy of MR imaging and clinical examination (Jobe-test, Impingement-sign) for diagnosing partial-thickness lesions of the rotator cuff. Low values were found for the sensitivity, specificity as well as the positive predictive value for the MR imaging findings, the Jobe-test and the Impingement-test. Additionally, the combination of positive clinical tests for a rotator cuff pathology (Jobe-test and Impingement-sign) and a partial-thickness tear of the rotator cuff found in the MR imaging based on the radiology report does not improve the diagnostic accuracy except for specificity.
Several previous studies have been done to examine the diagnostic accuracy of MR imaging or clinical tests to detect tears of the rotator cuff [6, 7], whereas the present study compared both in one survey and additionally correlated these parameters with each other. Thus, the present results add new clinically relevant information to the recent literature. When comparing the findings of the present study to those of the recent literature for detecting partial-thickness tears of the rotator cuff, similar results were found for the sensitivity and specificity of the MR imaging and the Impingement-sign.
Balich et al. [5] assessed the diagnostic accuracy of analyzing the integrity of the rotator cuff on MR images. Five radiologists analysed MR images of 222 symptomatic patients. The results were verified by arthroscopic findings. A sensitivity of 35–44%, a specificity of 85–97% and an accuracy of 77–87% for the MR imaging to determine partial-thickness tears of the rotator cuff were found. High inter- and intra-observer variability was described for the evaluation of MR imaging concerning the rotator cuff lesion, especially for partial-thickness tears and for radiologists as well as orthopaedic surgeons who are not experienced in analyzing MR imaging of the rotator cuff [3, 9].
Neer [10] as well as Dinnes et al. [11] described a sensitivity of 70–80% and specificity of 40–60% for the Impingement-sign to detect partial-thickness tears of the rotator cuff. These findings were confirmed by the results of the present study and underline especially the fact that the Impingement-sign is too general and is lacking specificity. It is known as the most reliable clinical sign for detecting any form of subacromial impingement syndrome [12]. Kelly et al. [12] tested the value of different physical tests for subacromial impingement syndrome and they pointed out that the most precise clinical examination for determining partial-thickness tears of the rotator cuff was pain on external rotation against resistance.
Villafane et al. [13] also tested the diagnostic accuracy of different clinical tests for diagnosing partial-thickness tears of the supraspinatus tendon. The results of their study were inconsistent to the results of the present study and showed different values for the diagnostic accuracy of the Jobe-test and the Impingement-signs.
Differing results can also be found concerning the sensitivity and specificity of the Jobe-test for detecting partial-thickness tears of the rotator cuff. Park et al. [14] evaluated the diagnostic value of various clinical examination techniques for the different categories of subacromial impingement syndrome. They described a sensitivity of 32.1% and a specificity of 67.8% for the Jobe-test to determine partial-thickness tears of the rotator cuff. In contrast to these results, the present findings show a higher sensitivity (64.1%) and a lower specificity (43.2%). Jain et al. [6] found higher values for diagnostic accuracy of the Jobe-test to detect tears of the supraspinatus tendon compared to the present results, but they did not distinguish in detail between partial-thickness and full-thickness tears of the rotator cuff.
Within the present study, the results of MR imaging and clinical tests for detecting partial-thickness tears of the rotator cuff were additionally combined with each other finding no improvement in diagnostic accuracy except for specificity.
Some limitations of this study should be mentioned. This was a retrospective study design with an inhomogeneous sample of patients. A lack of standardization of the quality of the MR imaging was noted; a standardized “cuff protocol” was not used in every case. The analysis of the MR imaging findings was done on the basis of the documented radiology report, an independent and separate evaluation of the MR imaging to detect the intra- and inter-observer reliability was not performed. It might be interesting to go further into detail and to differentiate between subgroups as Ellman I° lesions versus Ellman II° and Ellman III° lesions. Especially Ellman III° lesions might be better detectable by MR imaging than Ellman I° lesions and that might lead to better results concerning sensitivity and specificity.
The valid diagnosis of partial-thickness tears of the rotator cuff by clinical tests and MR imaging procedures remains challenging. Halma et al. [9] found that orthopaedic surgeons and radiologists varied in evaluation of shoulder MR images concerning ligamentous tears. The orthopaedic surgeons showed significantly higher precision in diagnosing impingement. Therefore, the MR imaging should be evaluated by the orthopaedic surgeon on their own, taking into consideration the background of the clinical examination, the history, and current complaints of the patient. The three dimensional extension of partial-thickness tears of the rotator cuff (thickness of the tear, retraction in mediolateral direction, extent in anteroposterior direction) should be noted while analyzing and evaluating MR imaging of the rotator cuff in the clinical setting. Ultrasonographic examination under dynamic conditions should also be part of the diagnostic process in addition to MR imaging. This might further improve the diagnostic accuracy for detecting partial-thickness tears of the rotator cuff.
In summary the exact and reliable diagnosis of partial-thickness tears of the rotator cuff by clinical examination and by MR imaging remains challenging at this time. The combination of MR imaging findings and clinical tests (Jobe-test and Impingement-sign) does not lead to higher diagnostic accuracy for detecting partial-thickness tears of the rotator cuff in clinical practise.
Conclusion
The reliable diagnosis of partial-thickness tears of the rotator cuff remains challenging as the diagnostic accuracy of MR imaging and clinical examination (Jobe-test, Impingement-sign) is still limited. The combination of positive clinical tests for a rotator cuff lesion (Jobe-test and Impingement-sign) and a partial-thickness tear of the rotator cuff found in MR imaging based on the radiology report does not improve diagnostic accuracy.
References
Matthewson G, Beach CJ, Nelson AA, Woodmass JM, Ono Y, Boorman RS, Lo IK, Thornton GM (2015) Partial thickness rotator cuff tears: current concepts. Adv Orthop 2015:458786
Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB (1995) Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 77:10–15
Grant JA, Miller BS, Jacobson JA, Morag Y, Bedi A, Carpenter JE (2013) Intra- and inter-rater reliability of the detection of tears of the supraspinatus central tendon on MRI by shoulder surgeons. J Shoulder Elbow Surg 22:725–731
Roy JS, Braen C, Leblond J, Desmeules F, Dionne CE, MacDermid JC, Bureau NJ, Fremont P (2015) Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med 49:1316–1328
Balich SM, Sheley RC, Brown TR, Sauser DD, Quinn SF (1997) MR imaging of the rotator cuff tendon: interobserver agreement and analysis of interpretive errors. Radiology 204:191–194
Jain NB, Luz J, Higgins LD, Dong Y, Warner JJ, Matzkin E, Katz JN (2017) The diagnostic accuracy of special tests for rotator cuff tear: the ROW cohort study. Am J Phys Med Rehabil 96:176–183
Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NC, Faloppa F (2013) Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev 9:CD009020
Ellman H (1990) Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res 254:64–74
Halma JJ, Eshuis R, Krebbers YM, Weits T, de Gast A (2012) Interdisciplinary inter-observer agreement and accuracy of MR imaging of the shoulder with arthroscopic correlation. Arch Orthop Trauma Surg 132:311–320
Neer CS (1983) Impingement lesions. Clin Orthop Relat Res 173:70–77
Dinnes J, Loveman E, McIntyre L, Waugh N (2003) The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review. Health Technol Assess 7:iii, 1–iii166
Kelly SM, Brittle N, Allen GM (2010) The value of physical tests for subacromial impingement syndrome: a study of diagnostic accuracy. Clin Rehabil 24:149–158
Villafane JH, Valdes K, Anselmi F, Pirali C, Negrini S (2015) The diagnostic accuracy of five tests for diagnosing partial-thickness tears of the supraspinatus tendon: a cohort study. J Hand Ther 28:247–251
Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG (2005) Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am 87:1446–1455
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The manuscript has been read and approved by all authors. The authors believe that this manuscript represents honest work. The authors report no conflict of interest.
Funding
There is no funding source.
Ethical approval
As this is a retrospective analysis of medical and radiological data files no ethical approval was obtained. Approval was given by the Institutional Research Coordinator and the head of the Department of Orthopaedics and Orthopaedic Surgery, Saarland University Medical Center, in January 2013.
Informed consent
As this is a retrospective analysis of medical and radiological data files no informed consent was signed from the patients. Patient data were anonymized.
Rights and permissions
About this article
Cite this article
Brockmeyer, M., Schmitt, C., Haupert, A. et al. Limited diagnostic accuracy of magnetic resonance imaging and clinical tests for detecting partial-thickness tears of the rotator cuff. Arch Orthop Trauma Surg 137, 1719–1724 (2017). https://doi.org/10.1007/s00402-017-2799-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2799-3