Abstract
Introduction
Sacroiliac (SI) screws are used for osteosynthesis in unstable posterior pelvic ring injuries. In the cases of “sacral dysplasia”, in which the elevated upper sacrum does not allow a secure SI screw insertion into the S1 level, the S2 segment must be used to achieve stable fixation. The bone quality of the S2 segment is thinner compared to that of the S1 vertebra and may cause biomechanical weakness. An additional SI screw insertion into the S3 level may improve stability. With respect to the anatomical conditions of the posterior pelvic ring, there have been no anatomical investigations to date regarding SI screw placement into the third sacral segment.
Materials and methods
CT raw datasets from 125 patients (ø59 years, ø172 cm, ø76 kg) were post-processed using Amira 5.2 software to generate 3D pelvic models. A program code implemented in C++ computed a transverse bone corridor for the first, second and third sacral segments for a typical SI screw diameter of 7.3 mm. Volume, sagittal cross-section, iliac entrance area and length of the determined screw corridors were measured. A confidence interval of 95 % was assumed (p < 0.05).
Results
The fully automatic computation revealed a possible transverse insertion for one 7.3-mm screw in the third sacral segment in 30 cases (24 %). The rate (60 %) of feasible S3 screw placements in the cases of sacral dysplasia (n = 25) is significantly higher compared to that (15 %) of “normal” sacra (n = 100). With regard to the existence of transverse iliosacroiliac corridors as a function of sacral position in between the adjacent iliac bone bilaterally, a new classification of three different shape conditions can be made: caudad, intermediate minor, intermediate major, and cephalad sacrum. Gender, age, body height and body weight had no statistically significant influence on either possible screw insertion or on the calculated data of the corridors (p > 0.05).
Conclusion
SI screw insertion into the third sacral level deserves discussion in the cases of sacral dysplasia. Biomechanical and practical utility must be verified.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sacroiliac (SI) screw placement is an effective method for fixing unstable posterior pelvic ring injuries with minimal soft-tissue dissection. The majority of SI screws are placed into the first sacral body [3, 17]. For higher stability, especially in fatigue fractures, which have been growing in number [9, 19, 22], the insertion of two screws either in the first sacral segment or in the first and second sacral levels is recommended [18, 21]. However, SI screw anchorage remains problematic and screw loosening or pull-out in osteoporotic bone is a common phenomenon even in young patients [9, 23]. Therefore, long screws (>100 mm) that cross the sacral body are required in the cases of an unilateral sacroiliac lesion or central sacral fractures [2]. Moreover, bilateral lesions of the posterior pelvic ring require complete iliosacroiliac fixation [10]. Vanderschot et al. and Mehling et al. [9, 23] concluded that the trans-iliac-sacral-iliac bar procedure is a valuable and elegant method for rigid fixation of insufficiency fractures of the dorsal pelvis. For both purposes, the osteosynthesis must be performed in a strict horizontal fashion through a secure transverse bone corridor whereby the bilateral sacral isthmus embodies the limiting region of the bony canal.
In regards of anatomic, ontogenetic and traumatological point of view, the term “Sacral dysplasia” is used for various applications. In Traumatology, “Sacral dysplasia” occurs with an incidence of 25–54 % [1, 20]. It is defined as a more cephalad position of the upper sacral segments in relation to the iliac crests that makes a SI screw placement into the first sacral segment more difficult and even an osteosynthesis performed in a strict horizontal fashion in S1 impossible [1, 3, 13, 20]. In such a situation, the S2 segment must be considered for screw implantation to achieve stable fixation. However, the bone density of the S2 lateral mass and S2 vertebral body is obviously lower compared with that of the S1 vertebra and may cause biomechanical weakness [5]. Hence, additional SI screw insertion into the S3 level might improve stability in the cases of “sacral dysplasia” when the elevated upper sacrum does not allow a secure transverse SI screw insertion into the S1 segment.
With respect to the anatomical conditions of the posterior pelvic ring, there have been no anatomical investigations to date regarding a realisable SI screw placement into the third sacral segment. The purpose of the current study was to determine the feasibility of a secure transverse screw insertion through the third sacral segment in pelvises with and without sacral dysplasia. To this end, a fully automatic computation of secure sacroiliac transverse bone corridors for the first, second and third sacral segment in 3D pelvic models was accomplished.
Materials and methods
For the radiomorphometric study, pelvic CT datasets were collected from a representative Caucasian population treated in our hospital. The CT scans were primarily generated to diagnose individual diseases. Informed patient consent for further research applications of individual images data was obtained. Pelvic bones showing residual trauma as well as tumorous, inflammatory or high-grade degenerative alterations were excluded. A total of 125 data sets were used for further analysis. All CT scans were performed on a Siemens SOMATOM Sensation multislice CT scanner (Siemens AG, Erlangen, Germany). Scanning parameters included image resolution of 512 × 512 pixels, slice distance of 0.6 mm and kernel B45f.
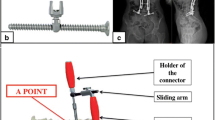
DICOM files of the anonymised CT raw data were post-processed by Amira 5.2 software (Visage Imaging GmbH, Berlin, Germany). The software computed triangulated bone surfaces in the STL (Standard Triangulated Language) format. The 3D data were then transformed into a common coordinate system following fluoroscopic standard Matta projections (outlet, inlet and lateral). For this purpose, several standard pre-processing and semi-automatic segmentation operations of the CT data were performed; these have been described in detail elsewhere [11, 14, 16]. After this, the transformed pelvis surfaces were converted into a volumetric representation resulting in a binary 3D image or label field with an isotropic voxel size of 0.5 × 0.5 × 0.5 mm3. The voxel value “1” represented bone and the value “0” conformed to structures exterior to the pelvic bone, including neurovascular structures (Fig. 1).
The program code computed transverse bone corridors acquiring data transitions from “bone” to “no bone” in the 2D lateral projection to detect bony material boundaries. In this process, voxels representing bone were labelled with the value of “1”, whereas voxels exterior of the pelvis were defined by a value of “0”
The program code was developed in C++ within the Amira framework and computed transverse bone corridors for the first, second and third sacral segments in each pelvis. In the 2D lateral projection, data transitions from “bone” to “no bone” were acquired to detect bony material boundaries. Hence, the projected area with the lowest number of cortical transitions (1st transition—left ilium in, 2nd transition—right ilium out) represented the oval footprint of the later transverse 3D corridor [12]. This workflow assumed that the script incorporated only the safe bone area that was limited by the narrow pedicular regions between the sacral ala superiorly, the 1st, 2nd and 3rd neural foramina and the iliac bone protuberance posterior to the iliac notch. Finally, the plane shape was corrected using a disc-like structuring element with a radius close to the commonly used SI screw diameter of 7.3 mm, resulting in a corresponding 3D transverse corridor for each of the three sacral segments. This procedure excluded the marginal narrow zones of the corridor that could lead to a partial cortical exit of marginal screw positions. In the end, volume, sagittal cross-section, screw entrance area and length of the determined screw corridors were measured and analysed.
Statistical analysis was performed with SPSS® 13 software (SPSS Inc., Chicago, USA) using the t test and the Chi-square test. A confidence interval of 95 % was assumed (significance level p < 0.05).
Results
CT raw datasets of 125 patients (50 females, 75 males) of a representative Caucasian population were collected to examine the feasibility of secure transverse SI screw insertion through the first, second and third sacral segments. The patients’ mean age was 59 ± 16 years (range 18–89) with a mean body height of 172 ± 11 cm (range 147–196 cm) and a mean body weight of 76 ± 13 kg (50–125 kg). The mean body mass index was calculated to be 26 ± 5 kg/m2 (range 15–39 kg/m2). The fully automatic computation revealed a possible transverse insertion for one 7.3-mm screw in the third sacral segment in 30 of 125 pelvises (24 %). Twenty-five pelvises (20 %) did not allow any implantation of a transverse 7.3-mm screw in the first sacral segment. These pelvises were defined as dysplastic and their third sacral segment could be safely implanted with a transverse 7.3-mm screw in 15 cases (60 %). This reveals a significant difference (p < 0.05) regarding to non-dysplastic pelvises with 100 consistently existing screw corridors in S1. Among these cases, an additional S3 corridor was detected in only 15 cases and an S2 transverse corridor was observed in 124 pelvises. Solely in 1 specimen a singular S1-bone bath was registered whereas there was no corridor at the S2- and S3- segmental level. The complete transverse corridor contribution in our population is illustrated in Fig. 2. Our data show that the craniocaudal position of the entire sacrum between the adjacent iliac bone bilaterally represents the crucial condition for the existence of transverse SI corridors throughout the corresponding sacral levels. With regard to this anatomical dependency, iliosacroiliac shape variants can be classified into 4 different shape conditions representing the possibilities of secure transverse SI screw insertion (Fig. 3):
-
1.
Intermediate minor sacrum: without S1 and S3; S2 corridor present, central sacrum position, small iliac wings encompassing just the central S2 segment, but not the S1 and the S3 sacral level
-
2.
Caudad sacrum: without S3 corridor, the adjacent ilium does not span the sacrum at the S3 sacral level
-
3.
Intermediate major sacrum: S1, S2 and S3 corridors present, central sacrum position, prominent iliac wings encompassing the S1, S2, and S3 sacral level
-
4.
Cephalad sacrum: without S1 corridor, the adjacent ilium does not span the sacrum at the S1 sacral level.
The bone corridors determined for the third sacral segment were limited by the bilateral isthmus bordered by the second neural foramen cranially and the third foramina and the posterior iliac bone protuberance caudally. The screw entry areas on the posterolateral ilium were situated directly posterior to the greater sciatic notch limited by the posterior inferior iliac spine.
S3 transverse corridors are consistently smaller compared to corridors of the S1 and S2 levels. Comparing the screw entry areas of S3 on both sides, there were only marginal differences with 96.2 ± 35.0 mm2 left and 94.4 ± 31.7 mm2 right. The sagittal cross-sectional area of the S3 corridor averaged 74.5 ± 29.8 mm2. In comparison, the 7.3-mm screw cross-section amounted to 41.8 mm2. Consequently, there is no extensive safety distance to the limiting cortical structures. The average length of the S3 corridors between the surfaces of the right and left ilia was 11.6 ± 0.9 cm and the volume measured was 8.9 ± 4.0 cm3. There was no significant gender difference for all parameters of the determined screw corridors in S3 (p > 0.05). Age, body height and body weight had no statistically significant influence on the calculated data of the corridors (p > 0.05). All measurement data of the S1 and S2 corridors are shown in Table 1.
Discussion
Sacroiliac screws are commonly used for osteosynthesis of unstable posterior pelvic ring injuries. Therefore, screws are commonly inserted into the S1 segment because of an acceptable fluoroscopic presentation and the assumption of larger SI bone corridor in S1 compared to S2. Biomechanical investigations have shown that an additional SI screw in S2 gives more posterior stability [21]. However, the high anatomical shape variation of the upper sacrum frequently leads to a complicated screw insertion or even prevents screw placement in S1. Such dysplastic pelvises occur at a considerable rate of up to 35 % in European [20] and as high as 54 % in Asian cohorts [8]. A minimally invasive method of SI screw placement can be accomplished at S2. The feasibility of percutaneous fixation with iliosacral screws in S2 has been shown in several anatomical and clinical studies and case reports. This has now become a valuable procedure after it had previously been largely avoided [1, 6, 7, 21].
SI screw fixation at the S3 segmental level is still a theoretical notion and to our knowledge, previous researchers have not considered this option. We feel that this lack of attention is due to the insufficient body of anatomical knowledge about the posterior pelvic ring. Indeed, a more cephalad position of the first sacral segment has been observed previously in sacral dysplasia [1, 11, 20]. This cephalic orientation within the pelvis involves the complete sacrum and results in the third segment being enclosed by adequate bone stock of both right and left ilia. The cephalad sacrum may present a sufficient S3 transverse corridor. According to this anatomical dependency, our data suggest a distinction of the 4 iliosacroiliac shape variants described here. Our results indicate that SI screw fixation into the S2 and S3 segments could be considered for a two-level sacroiliac screw fixation in the “intermediate major” (12 %) or “cephalad” (12 %) sacral variants. The latter variant is equivalent to the commonly used but inaccurate term “sacral dysplasia”; its anatomical limitations are the isthmus between the second and third sacral foramina and the iliac bone stock that is constrained by the posterior inferior iliac spine. The number of feasible S3 screws in the cases of sacral dysplasia is significantly higher in comparison to “normal” non-elevated sacra. We believe that screw insertion into S3 deserves discussion for dysplastic cases in consideration of this incidence. This presupposes that the surgeon is able to detect sacral dysplasia preoperatively and recognises whether screw insertion in S3 can be performed. Until now, several investigations revealed indicators for dysplastic conditions based on fluoroscopy or computed tomography [1, 11, 20]. Recently, Mendel et al. described the lateral sacral triangle as an accurate predictive value allowing the surgeon to decide whether the insertion of one or more 7.3-mm SI screws with a strict transverse vector in S1 is possible using one planar image in the strict lateral pelvic projection. However, in the cases of sacral dysplasia, the feasibility of secure transverse SI screw insertion through the third sacral segment cannot be evaluated with these methods. Thus, a preoperative imaging study, preferably a computed tomography scan, is necessary to assess the anatomical situation at S1, S2 and S3. The radiologists should mandatorily generate oblique coronal CT scans to determine preoperatively the sacral position in between the adjacent iliac bone bilaterally showing the existence of transverse iliosacroiliac corridors (Fig. 3).
Furthermore, our method provides an individual CT-based computation and visualisation of secure transverse SI corridors for the upper sacrum confirming whether SI screw insertion can be safely performed based on the anatomy. However, this study has shown that the S3 transverse corridor has a minimal safety distance to the limiting cortical structures. The risk of screw protrusion increases tremendously by missing the optimal transverse screw path and places the adjacent superior gluteal vessels and the gluteal neural ramus at potential risk. In addition to the anatomical conditions of the upper sacrum, bone quality must not be disregarded. The bone density of certain parts of the sacrum is variable and decreases caudally [4, 5, 15]. With respect to the expected weaker bone quality and biomechanics, an insertion in S3 should be performed with long SI screws, preferably ending in the contralateral ilium. However, many remain sceptical regarding the feasibility of a screw insertion into this small corridor. In sum, the biomechanical and practical feasibility of transverse SI screw insertion in the third sacral segment of dysplastic sacra must still be verified.
One major limitation of our study is the fact that the 125 pelvises were intact, whereas in the clinical situation, this may not be the case. The extent of residual (ilio)-sacral fracture dislocation may change the anatomical situation and potentially prevent SI screw insertion into S3.
Conclusion
Sacral dysplasia occurs reasonably often and can make transverse SI screw insertion into the first sacral segment impossible. Therefore, the S2 body has to be used optionally to achieve SI screw implantation. An additional SI screw placement into the S3 body might improve stability in elderly and in osteoporotic bone and could be performed regularly in the cases of dysplastic sacra. Our experimental study has shown that SI screw insertion into S3 could be considered, especially in the cases of sacral dysplasia. Furthermore, a more appropriate classification of four anatomical types is introduced describing the existence of transverse corridors at the S1, S2 and the S3 levels as a function of sacral position relative to the adjacent iliac bones. Biomechanical and practical feasibility must still to be verified in future research endeavours.
References
Carlson DA, Scheid DK, Maar DC, Baele JR, Kaehr DM (2000) Safe placement of S1 and S2 iliosacral screws: the “vestibule” concept. J Orthop Trauma 14(4):264–269
Culemann U, Scola A, Tosounidis G, Pohlemann T, Gebhard F (2010) Concept for treatment of pelvic ring injuries in elderly patients. A challenge. Unfallchirurg 113(4):258–271
Day CS, Prayson MJ, Shuler TE, Towers J, Gruen GS (2000) Transsacral versus modified pelvic landmarks for percutaneous iliosacral screw placement—a computed tomographic analysis and cadaveric study. Am J Orthop 29(9 Suppl):16–21
Ebraheim N, Sabry FF, Nadim Y, Xu R, Yeasting RA (2000) Internal architecture of the sacrum in the elderly. An anatomic and radiographic study. Spine (Phila Pa 1976) 25(3):292–297
Ebraheim NA, Lin D, Xu R, Stanescu S, Yeasting RA (1999) Computed tomographic evaluation of the internal structure of the lateral mass in the upper sacra. Orthopedics 22(12):1137–1140
Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S (2006) Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma 20(1 Suppl):S30–S36
Hinsche AF, Giannoudis PV, Smith RM (2002) Fluoroscopy-based multiplanar image guidance for insertion of sacroiliac screws. Clin Orthop Relat Res 395:135–144
Kim JJ, Jung CY, Oh HK, Chang JS (2007) Measurement of optimal pelvic tilt angle for iliosacral screw fixation using 3-D CT scan. 8th EFORT Congress, Florence, Italy
Mehling I, Hessmann MH, Rommens PM (2012) Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury 43(4):446–451
Mendel T, Noser H, Kuervers J, Goehre F, Hofmann GO, Radetzki F (2013) The influence of sacral morphology on the existence of secure S1 and S2 transverse bone corridors for iliosacroiliac screw fixation. Injury 44(12):1773–1779
Mendel T, Noser H, Wohlrab D, Stock K, Radetzki F (2011) The lateral sacral triangle—a decision support for secure transverse sacroiliac screw insertion. Injury 42(10):1164–1170
Mendel T, Radetzki F, Wohlrab D, Stock K, Hofmann GO, Noser H (2013) CT-based 3-D visualisation of secure bone corridors and optimal trajectories for sacroiliac screws. Injury 44(7):957–963
Moed BR, Geer BL (2006) S2 iliosacral screw fixation for disruptions of the posterior pelvic ring: a report of 49 cases. J Orthop Trauma 20(6):378–383
Noser H, Radetzki F, Stock K, Mendel T (2011) A method for computing general sacroiliac screw corridors based on CT scans of the pelvis. J Digit Imaging 24(4):665–671
Peretz AM, Hipp JA, Heggeness MH (1998) The internal bony architecture of the sacrum. Spine (Phila Pa 1976) 23(9):971–974
Radetzki F, Mendel T, Noser H, Stoevesandt D, Rollinghoff M, Gutteck N et al (2013) Potentialities and limitations of a database constructing three-dimensional virtual bone models. Surg Radiol Anat 35(10):963–968
Reilly MC, Bono CM, Litkouhi B, Sirkin M, Behrens FF (2003) The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma 17(2):88–94
Rommens PM (2007) Is there a role for percutaneous pelvic and acetabular reconstruction? Injury 38(4):463–477
Rommens PM, Hofmann A (2013) Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury 44(12):1733–1744
Routt ML Jr, Simonian PT, Agnew SG, Mann FA (1996) Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma 10(3):171–177
van Zwienen CM, van den Bosch EW, Snijders CJ, Kleinrensink GJ, van Vugt AB (2004) Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma 18(9):589–595
Vanderschot P (2007) Treatment options of pelvic and acetabular fractures in patients with osteoporotic bone. Injury 38(4):497–508
Vanderschot P, Kuppers M, Sermon A, Lateur L (2009) Trans-iliac-sacral-iliac-bar procedure to treat insufficiency fractures of the sacrum. Indian J Orthop 43(3):245–252
Acknowledgments
The authors would like to thank the AO Research Institute Davos/Switzerland for supporting this project and Prof. Dr. Andreas Wienke, PhD for assistance of the statistical analysis.
Conflict of interest
The authors confirm that there are no financial and personal relationships with any other people or organisations that could inappropriately influence the content or the statements of the submitted article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Radetzki, F., Wohlrab, D., Goehre, F. et al. Anatomical conditions of the posterior pelvic ring regarding bisegmental transverse sacroiliac screw fixation: a 3D morphometric study of 125 pelvic CT datasets. Arch Orthop Trauma Surg 134, 1115–1120 (2014). https://doi.org/10.1007/s00402-014-2022-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-014-2022-8