Abstract
Purpose
To evaluate the feasibility of transverse iliosacral (TIS) screw placement in different segments of the sacrum and measure the parameters of the unilateral iliosacral (IS) screw in the case that cannot be inserted the TIS screw.
Methods
This study used 100 pelvic continuous computed tomography images. Mimics (Materialise Interactive Medical Image Control System) was used to reconstruct the three-dimensional pelvis model. All sacrums were divided into the normal group and dysmorphic group. Any difference in osseous fixation pathway (OFP) diameter in the first two segments between both groups was investigated. In dysmorphic sacrums, the optimal inserting angle and length of the unilateral S1 screw were measured. The number of foramen in every sacrum was recorded.
Results
Thirty-two sacrums had sacral dysmorphism. The OFP diameter for the S2 TIS screw in the dysmorphic group was larger than that in the normal group (p = 0.02). Receiver operating characteristic curve analysis indicated the cutoff values as 20.55 mm and 15.18° for the S1 front edge height and S1S2 angle, respectively. In the dysmorphic case, the unilateral S1 IS screw should be inserted with a cephalad incline angle of 36.14 ± 5.97° and a ventrally incline angle of 37.33 ± 4.64°. S3 TIS screw placement rate was 53.1% in the dysmorphic group.
Conclusions
The most common cause of sacral dysmorphism is the fusion of the L5 to the true S1. In dysmorphic sacrums, the unilateral IS screw should be placed obliquely in the S1 segment, and the S2 segment usually has a sufficient OFP for the TIS screw. Using S3 TIS screw and two TIS screws in the first segment technique is not recommended because of a high risk.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Unstable pelvic ring injuries have been associated with a high mortality rate. Several fixation techniques can treat unstable injuries of the posterior pelvic ring. However, percutaneous iliosacral (IS) screw fixation is a reliable and effective method to stabilize pelvic fractures with minimal soft tissue invasion [1]. With improved understanding of the sacral anatomy, the technique of transverse iliosacral (TIS) screw insertion was applied. TIS screw is a single lengthened screw traversing through bilateral sacroiliac joints and the entire sacral body. Compared with the standard unilateral IS screw, the TIS screw was proved to provide improved resistance to vertical shear forces both biomechanically [2, 3] and clinically [4, 5], owing to its increased length, transversal of more sacral body bones, more cortices of fixation, and a longer lever arm to resist vertical shear forces. The indications for the use of the TIS screw are evolving and include bilateral IS joint injuries, comminuted and displaced posterior pelvic ring injuries, spinopelvic dissociations, and revision surgery for nonunion cases [4,5,6].
The sacrum exhibits a complex anatomical structure with high variations [7, 8]. Sacral dysmorphism is defined as the first sacral segment (S1) infeasible for TIS screw placement [9]. Considering the potential risks of percutaneous IS fixation, such as neurovascular damage [10], some surgeons in this field have attempted to quantify the upper sacral morphology by computed tomography (CT)-based studies [11,12,13]. A 7–8-mm scale was utilized previously as a simple pre-operative indicator that has been proven safe through an extensive clinical series [14,15,16].
Prior studies investigating the size and orientation of the sacral osseous fixation pathway (OFP) have focused on the S1 and the second sacral segment (S2). The cross section of the OFP differs between the normal and dysmorphic sacrum, and the S2 is recommended as the substitute segment for fixation of dysmorphic sacrum [9, 11]. Understanding anatomical variations of the sacrum in a three-dimensional (3D) model is essential to prevent intra-operative complications of TIS screw insertion.
Jeong et al. [13] conducted a computational study based on the cadaveric sacra. In order to further analyze the sacral anatomy and measure the IS screw parameters more accurately, the in vivo intact pelvis CT data were selected as the research objects in the current study. The aims of this study were to explore the possibility of TIS screw fixation in different sacral segments and to measure the parameters of the S1 unilateral iliosacral (IS) screw in the case of sacral dysmorphism.
Methods
The study was approved by the Regional Ethics Board. All patient information was anonymized in this retrospective study. A retrospective review of patients who visited our hospital (level 1 trauma center) from January 2016 to October 2017 was performed by utilizing the picture archiving and communication system (PACS). Computed tomography (CT) scans of these patients were primarily carried out to diagnose individual disease. Inclusion criteria were age 18–85 years, skeletal maturity, and a pelvic CT scan with serial axial images of 1.5 mm or less. Any pelvic bones with prior history or current evidence of trauma, tumor, or severe degenerative alterations were excluded. After screening, 100 adult patients (57 men and 43 women) were enrolled. Demographic data were collected from the PACS, including age and sex.
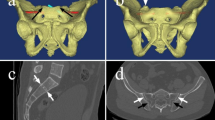
CT data in Digital Imaging and Communications in Medicine format were imported into the Mimics software (Materialise Interactive Medical Image Control System; Materialise, Antwerp, Belgium) to reconstruct 3D pelvis models, including the sacrum and two iliac bones (Fig. 1a). After the 3D pelvis model was generated, hide the two iliac bones and adjust the transparency mode of the sacrum to “high.” Then, the cancellous bone was distinguished from the sacral foramen and cortical bone (Fig. 1b).
a Reconstruction of the sacrum and iliac model in Mimics software. b 3-Matic software was used to remove the bilateral iliac bone. Then, the sacrum was set as a high transparency. Three OFPs are visible and marked with light green. c, d A 7.0-mm-sized transverse cylinder representing the TIS screw cylinders was inserted into the S1 segment
Two orthopaedic traumatologists with a clinical focus on pelvic and acetabular trauma evaluated each patient’s CT image identically. Average values measured by both researchers were used as the final result. For each subject, sacral segments were defined and numbered beginning with the first sacral segment which has a full articulation with the ilium. The defined boundary between normal and dysmorphic was determined by whether a 7.0-mm TIS screw could be placed intraosseously at the S1 segment. The sacrum that cannot be inserted with a TIS screw without perforating the cortex at the S1 level was defined as dysmorphic sacrum.
To simulate TIS screw insertion, a straight cylinder was generated by the 3-Matic software (Materialise). A 7.0-mm-sized transverse cylinder representing the TIS screw cylinders was inserted into the S1 segment (Fig. 1c, d). It was positioned from the outer cortex of one iliac bone to the outer cortex of the contralateral iliac bone. If the placement of the 7.0-mm S1 transverse cylinder was not possible, then the sacrum was dysmorphic. The same method was utilized to evaluate the presence of a potential S3 OFP. The length of this cylinder is the longest TIS screw we can place in the corresponding segment. The diameter of the cylinder that mimics the TIS screw was adjusted to maximum and ensured that it does not penetrate the cortex at the same time. Then, the diameter of the cylinder is exactly the OFP diameter of the TIS screw (Fig. 2).
In the true lateral projection of the opaque sacrum, the S1 front edge height was measured as the distance of the S1 front edge beyond the sacral wings (Fig. 3a). A vertical line on the S1 upper edge and S2 lower edge was drawn in the sagittal plane of the sacrum. The intersection of two perpendicular lines forming an angle (∠α) was defined as the S1S2 angle (Fig. 3b). In dysmorphic sacrum, the cephalad incline angle and ventrally incline angle of the unilateral S1 screw were measured from the CT coronal and axial scans (Fig. 3c, d). Furthermore, the number of foramen in each sacrum was recorded.
a From the true lateral view, the distance of the S1 front edge beyond the sacral wings is defined as the S1 front edge height (in this case, the S1 front edge height is 26.22 mm). b Draw the vertical line of S1 upper edge and S2 lower edge, respectively. The intersection of two perpendicular lines forming an angle (∠α) is defined as S1S2 angle. c, d Measurement of cephalad inclined angle (c) and ventral inclined angle (d) of the unilateral S1 screw in dysmorphic sacrum
Statistical analysis
All data were collected and inputted into SPSS Statistics 23.0 (SPSS Inc., Chicago, IL, USA) statistical software. The Kolmogorov-Smirnov test was used to determine the normality of the distribution. Chi-square test and two-sample t test were used to compare means between both groups. A confidence interval of 95% was assumed (significance level p < 0.05). Receiver operating characteristic (ROC) curve analysis was performed to identify the association between a dysmorphic sacrum and anatomical parameters.
Results
Between January 1, 2016, and October 1, 2017, 100 patients who met the above inclusion criteria were identified. Of these patients, 57 were men and 43 were women with an average age of 48.87 ± 15.64 years. Of the 100 patients, 32 (32%) had sacral dysmorphism. No statistically significant difference was found in age, sex, height, and weight (p > 0.05) between both groups. Of the 32 patients in the dysmorphic group, 17 patients (53.13%) had an S3 OFP that could accommodate a 7.0-mm TIS screw. Then, five of the 68 patients in the normal group (7.35%) had sufficient OFP for S3 TIS screw placement (Table 1).
On the basis of the number of sacral foramen, one model had a sacrum with three foramina. Two models in the normal group had five foramina. However, the sacrum with five foramina accounted for 62.5% (20/32) of the dysmorphic group. A statistically significant difference was observed between the two groups (p = 0.00) (Table 1).
The average OFP diameters at the S1 level in the dysmorphic and normal groups were 4.82 ± 1.72 mm and 13.67 ± 3.65 mm, respectively (p = 0.00). The average length of the S1 TIS screw in the normal group was 153.55 ± 9.98 mm. A statistically significant difference was found in the S2 OFP diameter between the dysmorphic group and the normal group (p = 0.02). However, the average length of the S2 TIS screw in the dysmorphic group was not significantly different (p = 0.44) from that in the normal group (Table 1). In the dysmorphic group, the optimal insertion angle of the unilateral S1 screw was cephalad inclined at 36.14° ± 5.97° and ventrally inclined at 37.33° ± 4.64°, with an average length of 90.45 ± 4.8 mm (Table 2).
The average S1 front edge height was 23.38 ± 4.60 mm in the dysmorphic group and 14.42 ± 4.34 mm in the normal group (p = 0.00). The average S1S2 angle was 17.35° (11.12°, 21.52°) in the dysmorphic group and 8.43° (3.23°, 15.10°) in the normal group (p = 0.00). ROC curve analysis using the S1 front edge height revealed an area under the curve of 0.922 (95% CI, 0.869–0.975). The S1 front edge height cutoff value was 20.55 mm (sensitivity 0.971, specificity 0.750). ROC curve analysis based on the S1S2 angle revealed an area under the curve of 0.745 (95% CI, 0.645–0.845). The cutoff value of S1S2 angle was 15.18° (sensitivity 0.765, specificity 0.656) (Fig. 4).
Discussion
The IS screw has made important progress in the treatment of unstable posterior pelvic ring disruptions and has been evaluated extensively [1, 2, 16,17,18,19]. Previous reports showed that TIS screws may provide a better stability compared to the conventional unilateral IS, especially in the treatment of vertical sacral fractures [2, 20, 21]. Thus, this study was performed using 3D software (Mimics) to explore the anatomical parameters of different sacrum segments. The results showed that dysmorphic sacrum accounted for about one third of the cohort we studied. The lumbar sacralization constitutes almost 2/3 of the dysmorphic sacrums. The S1 front edge height and S1S2 angle were two predictable indicators for the feasibility of TIS screw placement. For the patients with a dysmorphic sacrum, the S2 segment usually has a sufficient OFP for a 7.0-mm TIS screw. The unilateral IS screw could also be placed obliquely in the S1 segment to strengthen the fixation if needed.
In some previous studies, pelvic CT data were post-processed by medical image processing software, such as Amira, Mimics, and 3-Matic [12, 13, 15, 22]. Jeong et al. [13] measured the surrounding surface area by an imaginary line in the true lateral view and used this anatomical variable in the statistical analysis. However, this “safe zone” is only the surface area of the sacrum, not the cross section of the bone tunnel, which will affect the accuracy of the study. Mendel et al. [12] calculated the volume and sagittal cross section of the transverse corridors of the sacral segment to describe the spatial extent. However, both studies measure the area or volume of irregular patterns, and the true trajectory of the screw is a cylinder trajectory. A larger area of irregular cross section does not mean that a larger diameter screw could be placed. In the current study, the OFP diameter was measured in true lateral view using the 3-Matic software at the time when the stimulated cylinder is about to break through the cortical bone. The results of our study were consistent with the previous study. The sacral dysmorphic group has a notably small S1 OFP, which does not allow for TIS screw placement. The S2 OFP diameter in dysmorphic sacrum is much larger than that in the normal sacrum. In the normal group, the diameter of the S1 OFP is larger than that of the S2 OFP.
The importance of preoperative identification of the first sacral segment boundary ratio was emphasized by Mendel et al. [14]. They suggested that when the ratio of the superior width to the anterior height of the first sacrum is greater than 1.5, a sufficient OFP for screws usually exists. Jeong et al. [13] introduced the horizontal distance of the safe zone and the anterior height of the first sacral segment to predict the possibility of TIS screw placement. The ROC analysis of the current study revealed that the cutoff value of S1 front edge height was 20.55 mm, which is consistent with Jeong’s study. Except for the S1 front edge height, a new anatomical parameter “S1S2 angle” was introduced in our study to express the retroversion of the first sacrum. The results reveal that if the S1S2 angle is larger than 15.18°, the pelvis would be likely a dysmorphic sacrum. All of these anatomical parameters, such as S1S2 angle, anterior height, and width/height ratio, are descriptions of the upper sacrum. Further studies should be conducted to explore anatomical indicators that can more accurately determine the sacral dysmorphic.
The qualitative characteristics of upper sacral segment dysplasia were described by Rout et al. firstly [23]. They reported six key characteristics to define sacral dysmorphism: (1) the upper sacrum is more collinear with the iliac crest, (2) hypertrophic mammillary at the sacral mid-alar area, (3) misshaped upper foramina, (4) residual disk space between the first two segments, (5) an acute alar slope, and (6) a “tongue-in-groove” sign. The recent study showed that 62.5% of the sacrums have five foramina in the dysmorphic group. In other words, almost 2/3 of the dysmorphic sacrum has a sacralized L5, which is placed over the true S1 and fused with S1. The sacralized L5 usually has a projecting vertebra, in which a shorter unilateral IS screw could be inserted obliquely. Dubory et al. [24] collected 30 pelvic CT scans and performed a computed tomographic anatomical study of the upper sacrum. They demonstrated that the gender, weight, and height have correlation with the anatomy of the upper sacrum. However, no statistical significant was found in these demographic variables between the normal group and dysmorphic group in the current study. Recently, researchers have proved the genetic factors were responsible for the development of lumbosacral segments [25, 26].
Eastman et al. [27] conducted an experiment that enrolled 250 patients to explore the feasibility of S3 TIS screw insertion. Their study demonstrated that 15.2% of the pelvis has adequate OFP to accommodate an S3 TIS screw. In our cohort, 53.1% of dysmorphic sacrums possessed an S3 pathway that could safely accommodate a TIS screw. By contrast, only 7.4% of the sacrums in the normal group allows an S3 TIS screw. While a pathway may exist at the S3 level, the start site for an S3 TIS screw is significantly more caudal than that of an S1 screw. This means that anatomical variations of the superior gluteal artery or other neurovascular structures close to the greater sciatic notch will be at risk when inserting an S3 TIS screw. Salazar et al. noted a significant difference in the bone quality between the first and second sacral segments and questioned the quality of fixation achieved in the second sacral segment [28]. The bone quality of the S3 segment was not investigated in the present study. Further, bone quality and biomechanical studies could be investigated whether these clinical concerns exist when inserting an S3 TIS screw.
Previous studies described a technical trick of inserting two TIS screws into the upper sacral segment [5, 29]. However, the present study results show that the average OFP diameter for upper segment was about 14 mm, which was just appropriate to accommodate two 7.0-mm TIS screws. Although better biomechanical stability was provided, this technique increased the duration of intra-operative fluoroscopy and the risk of surgery greatly. Instead, using two TIS screws in the first two segments is a safer choice than using two parallel screws in the first segment.
Several limitations should be noted in the present study. First, all subjects were selected from one institution. However, the anatomical parameters of the sacrum may vary among different ethnicities. Second, this study was based on the 3D model generated using normal pelvic CT data. Simulating the TIS screw placement in the 3D software is an ideal situation. The posterior pelvic ring injuries is often accompanied by different degrees of sacroiliac joint dislocation. An anatomic reduction of the sacroiliac joint must be performed before the TIS or IS screw placement. Otherwise, the damage of blood vessels and nerves will also occur in the incompletely anatomical reduction cases.
Conclusions
Sacral dysmorphism occurs in 32% adults. The most common cause of sacral dysmorphism is the fusion of L5 to the first sacrum, which constitutes almost 2/3 of the cases. The S1 front edge height and S1S2 angle can be used to predict the feasibility of TIS screw placement. In sacral dysmorphism, the unilateral IS screw should be placed obliquely in the S1 segment, and the S2 segment usually has a sufficient OFP for the 7.0-mm TIS screw. Using a S3 TIS screw and two TIS screws in the first segment is not recommended because theoretically, the risk is high.
References
Enninghorst N, Toth L, King KL, McDougall D, Mackenzie S, Balogh ZJ (2010) Acute definitive internal fixation of pelvic ring fractures in polytrauma patients: a feasible option. J Trauma 68(4):935–941
Tabaie SA, Bledsoe JG, Moed BR (2013) Biomechanical comparison of standard iliosacral screw fixation to transsacral locked screw fixation in a type C zone II pelvic fracture model. J Orthop Trauma 27(9):521–526
Zhao Y, Li J, Wang D, Liu Y, Tan J, Zhang S (2012) Comparison of stability of two kinds of sacro-iliac screws in the fixation of bilateral sacral fractures in a finite element model. Injury 43(4):490–494
Heydemann J, Hartline B, Gibson ME, Ambrose CG, Munz JW, Galpin M, Achor TS, Gary JL (2016) Do transsacral-transiliac screws across uninjured sacroiliac joints affect pain and functional outcomes in trauma patients? Clin Orthop Relat Res 474(6):1417–1421
Gardner MJ, Routt ML Jr (2011) Transiliac-transsacral screws for posterior pelvic stabilization. J Orthop Trauma 25(6):378–384
Mehling I, Hessmann MH, Rommens PM (2012) Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury 43(4):446–451
Wu LP, Li YK, Li YM, Zhang YQ, Zhong SZ (2009) Variable morphology of the sacrum in a Chinese population. Clin Anat 22(5):619–626
Mahato NK (2010) Variable positions of the sacral auricular surface: classification and importance. Neurosurg Focus 28(3):E12
Miller AN, Routt ML Jr (2012) Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg 20(1):8–16
Conflitti JM, Graves ML, Chip Routt ML, Jr (2010) Radiographic quantification and analysis of dysmorphic upper sacral osseous anatomy and associated iliosacral screw insertions. J Orthop Trauma 24(10):630–636
Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt ML, Jr (2010) Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma 24(10):622–629
Mendel T, Noser H, Kuervers J, Goehre F, Hofmann GO, Radetzki F (2013) The influence of sacral morphology on the existence of secure S1 and S2 transverse bone corridors for iliosacroiliac screw fixation. Injury 44(12):1773–1779
Jeong JH, Jin JW, Kang BY, Jung GH (2017) Can the possibility of transverse iliosacral screw fixation for first sacral segment be predicted preoperatively? Results of a computational cadaveric study. Injury 48(10):2074–2079
Mendel T, Noser H, Wohlrab D, Stock K, Radetzki F (2011) The lateral sacral triangle--a decision support for secure transverse sacroiliac screw insertion. Injury 42(10):1164–1170
Chon CS, Jeong JH, Kang B, Kim HS, Jung GH (2017) Computational simulation study on ilio-sacral screw fixations for pelvic ring injuries and implications in Asian sacrum. Eur J Orthop Surg Traumatol 28(3):439–444
Lucas JF, Routt ML Jr, Eastman JG (2017) A useful preoperative planning technique for transiliac-transsacral screws. J Orthop Trauma 31(1):e25–e31
van Zwienen CM, van den Bosch EW, Snijders CJ, Kleinrensink GJ, van Vugt AB (2004) Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma 18(9):589–595
Rommens PM (2007) Is there a role for percutaneous pelvic and acetabular reconstruction? Injury 38(4):463–477
Shaw JC, Routt MLC Jr, Gary JL (2017) Intra-operative multi-dimensional fluoroscopy of guidepin placement prior to iliosacral screw fixation for posterior pelvic ring injuries and sacroiliac dislocation: an early case series. Int Orthop 41(10):2171–2177
Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S (2003) Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma 17(6):399–405
Keating JF, Werier J, Blachut P, Broekhuyse H, Meek RN, O'Brien PJ (1999) Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma 13(2):107–113
Radetzki F, Wohlrab D, Goehre F, Noser H, Delank KS, Mendel T (2014) Anatomical conditions of the posterior pelvic ring regarding bisegmental transverse sacroiliac screw fixation: a 3D morphometric study of 125 pelvic CT datasets. Arch Orthop Trauma Surg 134(8):1115–1120
Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA (1995) Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma 9(3):207–214
Dubory A, Bouloussa H, Riouallon G, Wolff S (2017) A computed tomographic anatomical study of the upper sacrum. Application for a user guide of pelvic fixation with iliosacral screws in adult spinal deformity. Int Orthop 41(12):2543–2553
Paik NC, Lim CS, Jang HS (2013) Numeric and morphological verification of lumbosacral segments in 8280 consecutive patients. Spine (Phila Pa 1976) 38(10):E573–E578
Di-Poi N, Montoya-Burgos JI, Miller H, Pourquie O, Milinkovitch MC, Duboule D (2010) Changes in Hox genes’ structure and function during the evolution of the squamate body plan. Nature 464(7285):99–103
Eastman JG, Adams MR, Frisoli K, Chip Routt ML, Jr (2018) Is S3 a viable osseous fixation pathway? J Orthop Trauma 32(2):93–99
Salazar D, Lannon S, Pasternak O, Schiff A, Lomasney L, Mitchell E, Stover M (2015) Investigation of bone quality of the first and second sacral segments amongst trauma patients: concerns about iliosacral screw fixation. J Orthop Traumatol 16(4):301–308
Kenawey M (2017) Surgical considerations with the operative fixation of unstable paediatric pelvic ring injuries. Int Orthop 41(9):1791–1801
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 81572162).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The study was approved by the Regional Ethics Board.
Conflict of interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Yin, Y., Zhang, R., Li, S. et al. Computational analysis on the feasibility of transverse iliosacral screw fixation for different sacral segments. International Orthopaedics (SICOT) 43, 1961–1967 (2019). https://doi.org/10.1007/s00264-018-4109-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4109-2