Abstract
Introduction
Minimally invasive total hip arthroplasty (THA) is claimed to be superior to the standard technique, due to the potential reduction of soft tissue damage via a smaller and tissue-sparing approach. As a result of the lack of objective evidence of fewer muscle and tendon defects, controversy still remains as to whether minimally invasive total hip arthroplasty truly minimizes muscle and tendon damage. Therefore, the objective was to compare the influence of the surgical approach on abductor muscle trauma and to analyze the relevance to postoperative pain and functional recovery.
Materials and methods
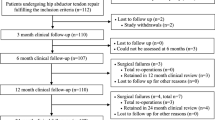
Between June 2006 and July 2007, 44 patients with primary hip arthritis were prospectively included in the study protocol. Patients underwent cementless unilateral total hip arthroplasty either through a minimally invasive anterolateral approach (ALMI) (n = 21) or a modified direct lateral approach (mDL) (n = 16). Patients were evaluated clinically and underwent MR imaging preoperatively and at 3 and 12 months postoperatively. Clinical assessment contained clinical examination, performance of abduction test and the survey of a function score using the Harris Hip Score, a pain score using a numeric rating scale (NRS) of 0–10, as well as a satisfaction score using an NRS of 1–6. Additionally, myoglobin and creatine kinase were measured preoperatively, and 6, 24 and 96 h postoperatively. Evaluation of the MRI images included fatty atrophy (rating scale 0–4), tendon defects (present/absent) and bursal fluid collection of the abductor muscle.
Results
Muscle and tendon damage occurred in both groups, but more lateral gluteus medius tendon defects [mDL 3/12mth.: 6 (37%)/4 (25%); ALMI: 3 (14%)/2 (9%)] and muscle atrophy in the anterior part of the gluteus medius [mean-standard (12): 1.75 ± 1.8; mean-MIS (12): 0.98 ± 1.1] were found in patients with the mDL approach. The clinical outcome was also poorer compared to the ALMI group. Significantly, more Trendelenburg’s signs were evident and lower clinical scores were achieved in the mDL group. No differences in muscle and tendon damage were found for the gluteus minimus muscle. A higher serum myoglobin concentration was measured 6 and 24 h postoperatively in the mDL group (6 h: 403 ± 168 μg/l; 24 h: 304 ± 182 μg/l) compared to the ALMI group (6 h: 331 ± 143 μg/l; 24 h: 268 ± 145 μg/l).
Conclusion
Abductor muscle and tendon damage occurred in both approaches, but the gluteus medius muscle can be spared more successfully via the minimally invasive approach and is accompanied by a better clinical outcome. Therefore, going through the intermuscular plane, without any detachment or dissection of muscle and tendons, truly minimizes perioperative soft tissue trauma. Furthermore, MRI emerges as an important imaging modality in the evaluation of muscle trauma in THA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Minimally invasive total hip arthroplasty (THA) is well established in orthopedic surgery and is frequently applied. The assumed reduction of soft tissue trauma was decisive for the euphoric introduction of the minimally invasive surgery (MIS) technique at the beginning of this century. Many studies have reported that the minimally invasive implantation technique leads to essential benefits compared to conventional techniques, which might be attributed to the purported lack of muscle and tendon damage [3, 4, 7, 10, 13]. In contrast, some authors see the only gain of MIS as a smaller skin incision and cosmetic benefit [26], while others even report a higher complication rate with a minimally invasive approach [22, 27, 34]. Consequently, controversy has arisen in the orthopedic society over the potential and actual efficacy of MIS [6, 16, 32].
A variety of minimally invasive approaches have been described, including mini-incision approaches, muscle-sparing approaches or a combination of the two, with a single or two incisions [4, 7, 8, 10, 24, 35]. Anatomical studies have shown that muscle damage occurs in all approaches [20, 21]. However, cadaveric tissue may not possess the same physical and mechanical properties as in vivo tissue and may not respond like living tissue during the procedure. Furthermore, the relative value of each type of structural damage and its individual relevance to postoperative pain and functional recovery cannot be examined either.
One of the single incision MIS approaches to the hip is the minimally invasive anterolateral (ALMI) approach. This approach uses the intermuscular plane between the gluteus medius and the tensor fasciae latae, the muscle integrity of which remained unaffected [8]. Due to the lack of objective evidence of unaffected muscle and tendons, it remains unclear whether and to what extent total hip arthroplasty performed using the anterolateral minimally invasive muscle-sparing approach truly minimizes muscle and tendon damage.
For the evaluation of muscle damage and function, different tests and methods are available. Clinical examination, scoring systems, blood indices and dynamometric muscle testing are established analyses. To study soft tissue structures and corresponding pathologies in vivo, one of the most useful tools is magnetic resonance imaging (MRI). Improvements regarding artifact-reducing techniques and utilization of titanium prostheses now enable good-quality imaging [23, 28, 30].
Therefore, the aim of the present study was to investigate abductor muscle trauma in relation to the surgical approach and the individual relevance to postoperative pain and functional recovery. Potential differences between the standard and the minimally invasive approach will be clearly indicated. In view of the postulated reduction of soft tissue trauma of a muscle-sparing approach, we hypothesize that less conspicuous pathological findings in MRI and better functional outcome will occur in the MIS approach compared to the direct lateral approach.
Materials and methods
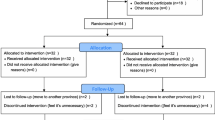
Between June 2006 and July 2007, 44 patients with primary hip arthritis were prospectively included in the study protocol. The study protocol was approved by the institutional review board (EA 1/068/06) and registered in a clinical trial registry (GCTR, registry number: DRKS00000152). Informed consent was obtained from all patients.
Patients were randomly matched either into a minimally invasive anterolateral or a modified direct lateral group. Randomization was done by throwing a dice, whereby an uneven number meant the standard approach and an even number the minimally invasive approach. A sealed envelope opened before surgery was used to determine the patient group.
Exclusion criteria were major architectural malformations (Crowe type II and beyond), fractures of the hip, necessity for femoral osteotomy, a history of previous surgery to the affected hip, inflammatory polyarthritis, arthrosis or arthroplasty of the contralateral side or any physical or mental disability. Demographic data, body mass index, side, operative time and incision length are given in Table 1. The dropout rate was 16%. This was mainly the result of failed MRI examinations due to claustrophobia (five patients). One patient failed to appear for follow-up examinations and another withdrew his/her consent without giving a reason.
Surgery was performed using either a modified direct lateral (transgluteal) approach of Hardinge or a minimally invasive anterolateral approach by two experienced surgeons (S.T. and C.P.) who had each previously done more than 1,500 arthroplasties. We chose the modified lateral approach, because it has been well established for over 30 years and is commonly used in orthopedic surgery.
The lateral approach was described initially by Bauer and Hardinge [2, 15]. Compared to the approach of Bauer and Hardinge, in the modified form [25, 31] the skin incision was minimized to approximately 10 cm. The gluteus medius was incised along the fiber course to a maximum length of 3 cm to protect the inferior branch of the superior gluteal nerve. To expose the joint capsule, the anterior third of the gluteus medius was detached together with the underlying gluteus minimus in toto ventrally from the trochanter major. Lengthening of the incision into the vastus lateralis was strictly avoided. The glutei tendons were refixed to the trochanter with two or three periosteal sutures (2.0, Ethibond, Ethicon, Somerville, US).
The minimally invasive anterolateral approach is a modified Watson–Jones approach and was introduced by Bertin and Rottinger [8]. This approach uses the intermuscular plane between the gluteus medius and the tensor fascia latae and provides good exposure to the hip joint while preserving muscle integrity.
The patients were treated with a straight cementless titanium stem (Zweymüller, Smith and Nephew®, Rotkreuz, Switzerland) and an uncemented titanium press-fit cup (Allofit®, Zimmer®, Warsaw, Indiana, US).
All randomly included patients experienced the same standardized postoperative care, narcotic protocol, pain management and rehabilitation. Mechanical foot pumps and pharmacological antithrombotic prophylaxis were used. Physical therapy was initiated on the 1st postoperative day. The goals of therapy were to enable the patients to independently transfer, ambulate with full weight bearing using two crutches and negotiate stairs. All patients were transferred after successful completion of wound healing to a rehabilitation clinic for a 3 week standardized recovery program. This includes exercises for the entire lower extremity, the ankle, knee and all the muscles surrounding the hip. The goals for the patients were to regain full ROM/flexibility, regain strength and endurance, and nearly all proprioception. Crutches had to be used for at least 6 weeks, depending on the preoperative muscular condition of each patient. No further therapy was provided after the rehabilitation program.
Patients were evaluated clinically and underwent MR imaging preoperatively and 3 and 12 months postoperatively. Clinical assessment included clinical examination and the survey of a function score using the Harris Hip Score (15), a pain score using a numeric rating scale (NRS) of 0–10 (0, no pain to 10, severe pain) and a satisfaction score using an NRS of 1–6 (1, very satisfied to 6, no satisfaction). Trendelenburg’s sign was evaluated to test the function of the abductor muscles. It was rated as either negative, slight positive (wobbly, unstable one leg stand, but without limping) or severe positive (unable to stand on one leg, with limping). Additionally, hip abduction strength of the affected side was assessed preoperatively and 3 and 12 months postoperatively, using a handheld dynamometer. Therefore, the patient was in an upright position and the pelvis was stabilized by the investigator. The dynamometer was fixed on the standing leg, high on the ankle joint. The affected limb was connected with a belt to the dynamometer in 10 degrees of abduction. The patient was instructed to push against the dynamometer with the affected limb, for approximately 2–4 s with maximal effort. All analysis of the clinical data was carried out by the same single observer (M.M.) who was blinded to the patients. As a blood index of muscle damage, serum myoglobin concentration and creatine kinase (CK) activity were measured preoperatively and 6, 24 and 96 h postoperatively.
MR imaging
MR imaging was performed using a 1.5-Tesla MRI (Symphony; Siemens Medical Solutions, Erlangen, Germany) according to a standardized protocol. A flexible wraparound phased-array coil was applied. Coronal T1-weighted turbo spin-echo [TSE, 667/12 ms (repetition time (TR)/echo time (TE)), 5 mm section thickness, flip angle (FA) of 150°, 400 × 400 mm field of view (FOV), 512 × 256 matrix, 195 Hz//Px bandwidth (BW), 0.8 × 1.6 × 5.0 mm3 voxel size, 12 echo train length (ETL), 3:51 min:s acquisition time (AT), 27 slices), transverse T1-weighted TSE sequence (667/12 ms (TR/TE), 6 mm section thickness, 420 × 275.52 mm field of view, 512 × 168 matrix, 195 Hz//Px BW, 0.8 × 1.6 × 6.0 mm3 voxel size, 12 ETL, 2:32 min:s AT, 28 slices], turbo-inversion recovery magnitude (TIRM) coronal T2-weighted fast spin echo [6040/30/150 ms (TR/TE/inversion time), 6 mm section thickness, FA of 150°, 400 × 400 mm FOV, 512 × 256 matrix, 130 Hz//Px BW, 0.8 × 1.6 × 6.0 mm3 voxel size, 15 ETL, 7:35 min:s AT, 23 slices], transverse TIRM sequence [5260/59/150 ms (TR/TE/inversion time), 6 mm section thickness, 360 × 270 mm FOV, 512 × 154 matrix, 130 Hz//Px BW, 0.7 × 1.8 × 6.0 mm3 voxel size, 15 ETL, 7:55 min:s AT, 39 slices] and coronal T2-weighted fast spin echo [6040/30/150 ms (TR/TE/inversion time), 6 mm section thickness, FA of 150°, 400 × 400 mm FOV, 512 × 256 matrix, 300 Hz//Px BW, 2.0 × 3.3 × 5.0 mm3 voxel size, 6 ETL, 0:28 min:s AT, 30 slices] MR images were obtained. The frequency encoding gradient was always parallel to the long axis of the prosthesis (craniocaudal direction).
Image analysis
All MR images were independently analyzed by a radiologist (M.D.) and a research assistant (I.S.). The readers were blinded to whether the patients were in the minimally invasive or standard group. After the independent readings, intraobserver differences were resolved by consensus.
Fatty atrophy of the abductor muscles was assessed on the transverse T1-weighted MR images using the following grading system. Grade 0 indicated that no intramuscular fat was present; grade 1: that some fat streaks were present; grade 2: that fat was evident, but there was less fat than muscle tissue; grade 3: that there were equal amounts of fat and muscle tissue; and grade 4: that there was more fat than muscle tissue. This grading system has already been introduced in the evaluation of gluteus muscle and corresponds to a classification system that is commonly used to categorize the rotator cuff muscles [14, 28]. Fatty atrophy was assessed on transverse T1-weighted MR images at the lower one-third of the distance between the iliac crest and the tip of the greater trochanter. The anterior, middle and posterior portions of the gluteus medius and gluteus minimus muscles were evaluated separately.
Tendon defects were evaluated for the gluteus minimus tendon, the lateral part of the gluteus medius tendon and the superior–posterior part of the gluteus medius separately. Tendon tears or detachments were defined as hyperintense signals on images obtained with fluid-sensitive sequences. Tendon signal intensity was graded on the T1-weighted MR images as normal (hypointense) or abnormal (increased signal intensity) compared with the signal intensity of a normal tendon. Bursal fluid collections were documented as absent or present using fluid-sensitive MR imaging.
Statistics
SPSS (version 15, SPSS Inc., Chicago, USA) was used for statistical analysis. In testing for statistically significant differences in the frequencies of findings between two patient groups, χ2 analysis was used and an exact Fischer–Yates test when the expected theoretical figures were lower than 5 (e.g. tendon defects, fatty atrophy, Trendelenburg’s sign). Pre- and postoperative continuously and normally distributed variables were compared with a Student’s t test (e.g. age, BMI). In the event that the variables were not normally distributed between the two groups, the Mann–Whitney U test was used (e.g. Harris Hip, satisfaction and pain score, abduction strength and blood parameters). A P value of 0.05 was considered to indicate a significant difference. Kappa (κ) statistics were calculated for interobserver agreement according to the method of Landis and Koch [19].
Results
Clinical assessment
In general, the patients of the minimally invasive group attained higher Harris Hip Scores, better satisfaction scores and lower pain scores at both 3 and 12 months (Table 2). But this was not statistically significant.
A statistically significant difference was seen concerning Trendelenburg’s sign. At 12 months, there was a significantly higher rate of positive Trendelenburg’s signs in the mDL group, compared to the ALMI group (P < 0.05, χ2) (Table 3).
Abduction strength
Higher values of abduction strength of the affected hip, measured preoperatively and at 3 and 12 months were obtained in the ALMI group [ALMI: pre/3/12Mo: 7.9 ± 2.7/8.1 ± 2.8/8.9 ± 2.5 (Nm); mDL: pre/3/12Mo: 7.8 ± 3.4/7.0 ± 2.5/7.9 ± 2.2 (Nm)], but without statistical significance (3 Mo: P = 0.23; 12Mo: P = 0.24; Mann–Whitney U test).
Blood parameters
A higher serum myoglobin concentration was measured 6 and 24 h postoperatively in the mDL group (6 h: 403 ± 168 μg/l; 24 h: 304 ± 182 μg/l) compared to the ALMI group (6 h: 331 ± 143 μg/l; 24 h: 268 ± 145 μg/l), but without statistical significance. No differences of the creatine kinase activity were seen between the two groups (Fig. 1).
Image analysis
Interobserver agreement for assessment of the fatty atrophy and tendon defects was moderate to excellent (kappa, 0.51–0.89).
Fatty atrophy
The means and the standard deviation for the rated fatty atrophy of the gluteus medius muscle are shown in Table 4. Significantly more fatty atrophy was found in the anterior part of the gluteus medius muscle at 3 and 12 months for the direct lateral approach (P = 0.007, χ2). Table 5 gives a detailed overview of the ratings for each approach. Figure 2 shows axial T1 FSE-MR images of a patient with a direct lateral approach and from a patient with a minimally invasive anterolateral approach. A grade 4 atrophy was seen in the anterior part of the gluteus medius in the patient with the mDL approach. We did not see any changes between the fatty atrophy at 3 and 12 months. The preoperative fatty atrophy was significantly less in both groups and only a few patients showed some fat between the muscle fibers.
MRI axial T1 FSE image sections of patients with an mDL approach (a, b) and a minimally invasive anterolateral approach (c, d), preoperatively (a, c) and 12 months postoperatively (b, d). The gluteus medius muscle (short black arrows) clearly shows fatty atrophy, grade 4, in the anterior part (b, long black arrow) in the patient with an mDL approach after 12 months. In contrast, the gluteus medius muscle of the patient with an ALMI approach was completely intact without any sign of atrophy (d). Also, the gluteus minimus muscle (white star) clearly shows fatty atrophy in the patient with an mDL approach, while the minimus in the minimally invasive anterolateral patient is completely uninjured
The fatty atrophy of the gluteus minimus muscle was rated higher than for the gluteus medius muscle in both groups (Table 4). There were no significant differences between the two patients groups.
Tendon defects
More lateral gluteal tendon defects were seen in the mDL group than in the minimally invasive group concerning the gluteus medius muscle (P = 0.13, χ2), (Table 6). The tendon at the posterior–superior trochanter region was almost intact in both groups. In terms of the gluteus minimus tendon, defects were equally distributed, without any difference between the two techniques. In both groups, a recovery of the tendon defects was recognizable at 12 months.
Figure 3 shows coronal T1-weighted FSE and fluid-sensitive IR-MR images of a patient who underwent the direct lateral technique and of a patient who underwent minimally invasive surgery.
Coronal MR images showing the greater trochanter region at the level of the insertion of the lateral gluteus medius tendon, preoperatively and 12 months postoperatively in two different patients with an mDL approach (a, b) and ALMI approach (c, d), respectively. Images a and c are T1-weighted FSE sequences; b and d are fluid-sensitive IR sequences. In the postoperative image b, a tendon defect is visible (white arrow). In image D, the patient with an ALMI approach shows the same anatomical situation as preoperatively, without any damage
Figure 4 shows the coronal and axial preoperative and postoperative (3 months) MR images of a patient who underwent THA via a minimally invasive anterolateral approach. A tendon defect of the gluteus minimus tendon and corresponding fatty atrophy are depicted.
Bursal fluid
Of the 16 patients in the mDL group, 5 (31%) showed a clear trochanteric bursitis at 3 months (P = 0,009, χ2). Two of these five patients still had a bursa at 12 months (P = 0.171, χ2). In no patient of the ALMI group was a bursa evident.
Incision length
The median incision length was 10.4 cm (range 8–13.5 cm) for the direct lateral approach and 8.0 cm (range 7–12.5 cm) for the minimally invasive anterolateral approach (P = 0.043, Mann–Whitney U test).
Discussion
The results of this study demonstrate that there is a trend, with higher and better values, in scoring systems, muscle enzyme analysis and in abduction test, for the mini-invasive approach. However, these tests may not be sufficiently sensitive to detect statistical significant differences between the two techniques. The results may be limited by the relatively small number of patients.
In contrast, the MRI turns out to be the most sensitive method in the depiction of differences in the contributory effects of surgical approach on muscle damage.
The results of MRI evaluation demonstrate that abductor muscle and tendon damage occur in both the ALMI approach and the mDL approach, but significantly more pathological findings for the gluteus medius muscle were found in patients with the mDL approach. The gluteus minimus muscle was damaged equally in both groups.
In particular, tendon defects and fatty atrophy in the anterior part of the gluteus medius muscle were more evident in the mDL group. In other words, the gluteus medius can be spared more effectively via the minimally invasive anterolateral approach, while the lateral approach is associated with an increased risk of tendon and muscle damage. The higher rate of gluteus medius muscle and tendon damage via the mDL approach is obviously caused by the partial dissection and detachment of the gluteus medius muscle and tendon from the greater trochanter during the initial preparation. The partially detached tendon was always reattached to the greater trochanter with sutures, but this does not seem to guarantee stable ingrowth in all cases. A persistent tendon defect and lack of integrity in association with fatty muscle atrophy may result. Unfavorable effects of the lateral approach on the postoperative integrity of the gluteus medius tendon have also been described in a radiographical analysis, where metal markers were placed in the tendon for measurements of tendon separation [33].
Furthermore, the pathological findings are correlated with the clinical outcome, because significantly more positive Trendelenburg signs were found in the mDL patient group. The depicted gluteus medius damage seems also to be reflected in gait pattern, pain and satisfaction of the patient, and therefore appears to be clinically relevant, at least in the early rehabilitation period. Patients with the minimally invasive anterolateral approach had a slightly better clinical outcome, higher clinical scores and lower rate of Trendelenburg signs, corresponding to significantly fewer muscle and tendon defects. Concerning this matter, in an MRI study of the abductor muscle and tendon in symptomatic and asymptomatic patients after THA, it was shown that abductor tendon defects and fatty atrophy of the gluteus medius muscle are more common in symptomatic patients and also most frequently found after lateral THA [28]. A more frequent occurrence of a positive Trendelenburg test after a direct lateral approach to the hip is described by several authors and attributed to either injuries of the superior gluteal nerve or muscle and tendon damage [1, 17, 29, 33]. Because we have strictly limited the division of the gluteus medius to the safe zone of 3–5 cm proximal to the greater trochanter tip, the possibility of superior gluteal nerve injury was minimized [9, 12]. Therefore, we see the direct relationship between the poorer clinical outcome of the lateral group and the MRI findings of muscle and tendon damage. Nearly all patients had completely recovered after 12 months and there were no significant differences between the two groups. In six patients of the lateral group, a slight positive Trendelenburg sign was apparent, but without any restrictions on gait pattern (limping). This is consistent with other studies where a reduction of the initial Trendelenburg sign after lateral THA was also described [1, 33]. We attribute this to the time-dependent compensation of other muscles and muscle units of the abductor muscle. We saw a recovery of the abductor tendon in some cases, but this was not statistically significant. A regression of fatty atrophy between 3 and 12 months was not seen. The longer recovery time of standard patients may be explained by the beneficial effects of rapid rehabilitation in the early postoperative period in patients undergoing minimally invasive total hip arthroplasty [4, 7, 10]. The rehabilitation time by itself could not be focused on in this study, since the study protocol was the same for both study groups.
In contrast to the gluteus medius muscle, no significant differences between the two approaches were seen for the gluteus minimus muscle. Although a certain number of minimally invasive anterolateral patients showed a lower rate of fatty atrophy compared to the standard group, the percentage of rating score 3 and 4 was nearly equally distributed between the two groups. Also, there were no apparent differences in the occurrence of tendon defects. In general, the gluteus minimus muscle showed the highest rate of fatty atrophy in both groups, compared to the gluteus medius muscle. Similar findings were reported in literature [23].
This higher rate of minimus muscle damage seems to be a result of the stem-related implantation technique, which has to be done from the most lateral femur side. We used a tapered, rectangular, uncemented straight Zweymüller stem in this study. For adequate placement of this stem model, the femur cut surface has to be well prepared, especially from the lateral side so that femoral preparation can begin in direct line with the shaft of the femur, to avoid varus or valgus malposition. During this preparation, the minimus muscle and tendon are at the highest risk of damage in the anterolateral and lateral approach.
The results of the MRI evaluation support and verify the presumption that minimally invasive THA causes less muscle damage. Because there is a variety of traditional and MIS approaches, the results of this study have to be seen rather as a specific comparison between the minimally invasive anterolateral and the lateral approach. We selected these approaches because the lateral approach is a well-established, traditional approach, while the minimally invasive anterolateral approach is consistent with the demands of an MIS technique: approaching the hip without detachment and dissection of muscles. Despite the clear advantage of minimization of muscle trauma via the ALMI approach, the associated possible risk of peroperative complications such as fractures of the greater trochanter or varus malalignment of the more demanding ALMI-technique have to be taken into account [5, 18].
Because myoglobin and creatine kinase are found in skeletal muscle and are released into the circulation when muscle is damaged, the measurement may allow for an objective evaluation of the potential difference among minimally invasive and standard THA techniques. The use of minimally invasive approach theoretically disrupts less of the muscle surrounding the hip and thus may have less of an effect on these serum markers. We found peak values of CK and myoglobin 6 h postoperatively for both approaches and observed a measurable trend in serum myoglobin level relating to the approach. However, the difference was not sufficiently great to reach statistical significance. The higher myoglobin level for the standard approach at 6 h may be justified with the different amount of skeletal muscle damage. In a recent investigation, different muscle enzyme levels were measured, also dependent on the respective THA technique and the associated muscle trauma. The mean myoglobin level at 6 h for the ALMI (331 ± 143 μg/l) was similar to that at 8 h reported by Cohen et al. [11] for the same approach (346 ± 144 μg/l). This supports the reliability of the measurements of this study. It is interesting that the level of myoglobin in the mDL group at 6 h (403 ± 168 μg/l) was as high as that in the MIS-II incision group (427.6 ± 247.3) in the study of Cohen et al. at 8 h.
In conclusion, the present study has demonstrated that damage to the abductor muscles and tendons is significantly less in minimally invasive total hip arthroplasty than when using a direct lateral approach. More fatty atrophy, tendon defects and bursal fluid collection concerning the gluteus medius muscle were observed when using the direct lateral approach, compared to the minimally invasive anterolateral approach. These findings are in line with the clinical outcome, although not reflected with the same significance. MRI emerges as an important imaging modality in the evaluation of patients with total hip arthroplasties. The minimization of muscle trauma in THA can be achieved best by going through the intermuscular plane, without any detachment or dissection of muscles and tendons.
References
Baker AS, Bitounis VC (1989) Abductor function after total hip replacement. An electromyographic and clinical review. J Bone Joint Surg Br 71:47–50
Bauer R, Kerschbaumer F, Poisel S et al (1979) The transgluteal approach to the hip joint. Archives of orthopaedic and traumatic surgery 95:47–49
Berger RA (2004) The technique of minimally invasive total hip arthroplasty using the two-incision approach. Instr Course Lect 53:149–155
Berger RA (2003) Total hip arthroplasty using the minimally invasive two-incision approach. Clin orthopaed Relat Res:232–241
Bernasek TL, Lee WS, Lee HJ et al (2010) Minimally invasive primary THA: anterolateral intermuscular approach versus lateral transmuscular approach. Archives of orthopaedic and traumatic surgery
Berry DJ (2005) “Minimally invasive” total hip arthroplasty. J Bone Joint Surg 87:699–700
Berry DJ, Berger RA, Callaghan JJ et al (2003) Minimally invasive total hip arthroplasty. Development, early results, and a critical analysis. Presented at the Annual Meeting of the American Orthopaedic Association, Charleston, South Carolina, USA, June 14, 2003. J Bone Joint Surg 85-A:2235–2246
Bertin KC, Rottinger H (2004) Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Rel Res:248–255
Bos JC, Stoeckart R, Klooswijk AI et al (1994) The surgical anatomy of the superior gluteal nerve and anatomical radiologic bases of the direct lateral approach to the hip. Surg Radiol Anat 16:253–258
Chimento GF, Pavone V, Sharrock N et al (2005) Minimally invasive total hip arthroplasty: a prospective randomized study. J Arthroplasty 20:139–144
Cohen RG, Katz JA, Skrepnik NV (2009) The relationship between skeletal muscle serum markers and primary THA: a pilot study. Clin Orthopaed Rel Res 467:1747–1752
Comstock C, Imrie S, Goodman SB (1994) A clinical and radiographic study of the “safe area” using the direct lateral approach for total hip arthroplasty. J Arthroplasty 9:527–531
Digioia AM 3rd, Plakseychuk AY, Levison TJ et al (2003) Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty 18:123–128
Goutallier D, Postel JM, Bernageau J et al. (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Related Res:78–83
Hardinge K (1982) The direct lateral approach to the hip. J Bone Joint Surg Br 64:17–19
Hungerford DS (2004) Minimally invasive total hip arthroplasty: in opposition. J Arthroplasty 19:81–82
Kenny P, O’brien CP, Synnott K et al (1999) Damage to the superior gluteal nerve after two different approaches to the hip. J Bone Joint Surg 81:979–981
Laffosse JM, Chiron P, Molinier F et al (2007) Prospective and comparative study of the anterolateral mini-invasive approach versus minimally invasive posterior approach for primary total hip replacement. Early results. Int Orthop 31:597–603
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Mardones R, Pagnano MW, Nemanich JP et al (2005) The Frank Stinchfield Award: muscle damage after total hip arthroplasty done with the two-incision and mini-posterior techniques. Clin Orthop Rel Res 441:63–67
Meneghini RM, Pagnano MW, Trousdale RT et al (2006) Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Rel Res 453:293–298
Mow CS, Woolson ST, Ngarmukos SG et al (2005) Comparison of scars from total hip replacements done with a standard or a mini-incision. Clin Orthop Rel Res 441:80–85
Muller M, Tohtz S, Winkler T et al (2010) MRI findings of gluteus minimus muscle damage in primary total hip arthroplasty and the influence on clinical outcome. Archives of orthopaedic and traumatic surgery
Nakamura S, Matsuda K, Arai N et al (2004) Mini-incision posterior approach for total hip arthroplasty. Int Orthop 28:214–217
O’brien DA, Rorabeck CH (2005) The mini-incision direct lateral approach in primary total hip arthroplasty. Clin Orthop Related Res 441:99–103
Ogonda L, Wilson R, Archbold P et al (2005) A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg 87:701–710
Peck CN, Foster A, Mclauchlan GJ (2006) Reducing incision length or intensifying rehabilitation: what makes the difference to length of stay in total hip replacement in a UK setting? Int Orthop 30:395–398
Pfirrmann CW, Notzli HP, Dora C et al (2005) Abductor tendons and muscles assessed at MR imaging after total hip arthroplasty in asymptomatic and symptomatic patients. Radiology 235:969–976
Picado CH, Garcia FL, Marques W Jr (2007) Damage to the superior gluteal nerve after direct lateral approach to the hip. Clin Orthop Rel Res 455:209–211
Potter HG, Foo LF, Nestor BJ (2005) What is the role of magnetic resonance imaging in the evaluation of total hip arthroplasty? HSS J 1:89–93
Roth A, Layher F, Venbrocks RA (2006) Transgluteal mini-incision. Technique and our own results. Der Orthopade 35(744):746–750
Sculco TP (2003) Is smaller necessarily better? American journal of orthopedics Belle Mead, NJ, 32:169
Svensson O, Skold S, Blomgren G (1990) Integrity of the gluteus medius after the transgluteal approach in total hip arthroplasty. J Arthroplasty 5:57–60
Woolson ST, Mow CS, Syquia JF et al (2004) Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg 86-A:1353–1358
Wright JM, Crockett HC, Delgado S et al (2004) Mini-incision for total hip arthroplasty: a prospective, controlled investigation with 5-year follow-up evaluation. J Arthroplasty 19:538–545
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Müller, M., Tohtz, S., Springer, I. et al. Randomized controlled trial of abductor muscle damage in relation to the surgical approach for primary total hip replacement: minimally invasive anterolateral versus modified direct lateral approach. Arch Orthop Trauma Surg 131, 179–189 (2011). https://doi.org/10.1007/s00402-010-1117-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-010-1117-0