Abstract
Introduction
Open reduction and internal fixation has been the gold standard for displaced fracture involving weightbearing dome and fractures with intra-articular fragments. However, extensile exposure can lead to complications. Fracture with minimal displacement can be fixed by a minimally invasive method. Percutaneous screwing for an anterior column fracture of acetabulum under conventional 2D fluoroscopy is a demanding technique. With fluoroscopic-based computerized navigation, we can determine the position of a screw real time intra-operatively with less exposure to radiation. We proposed that a fluoroscopy-based computerized navigational system would simplify operation procedures. The purpose of this study is to test the application of the fluoroscopy-based computerized navigational system for anterior column fracture of acetabulum.
Materials and methods
A prospective cohort study was conducted. Three patients with mildly displaced or non-displaced anterior column fracture of acetabulum were treated with a retrograde lag screw under a fluoroscopy-based computer navigation system. There were two males and one female with a mean age of 39 years and all patients were followed up for more than 1 year. Patients were allowed to perform joint movement exercises and to walk with partial weightbearing on the first day post-operatively.
Results
The mean operation time was 40 min (range 30–45 min) from the use of fluoroscopy to wound closure and the mean total fluoroscopy time was 38 s (range 35–45 s). Total blood loss was less than 10 ml. The patients were pain free 1 week after the operation and had good functional recovery thereafter. No complication was noted postoperatively.
Conclusion
Though the indication for this procedure is limited, we think that there should be potential to apply the screw with less radiation by fluoroscopic-based computerized navigation. Once anatomic reduction can be achieved by the close method in the anterior column fracture of the acetabulum, percutaneous screw fixation under fluoroscopic-based computerized navigation could be a reliable method; however; validating the position of the guide pin and screw by fluoroscopy is suggested.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgical treatment of acetabular fractures is one of the most challenging techniques for orthopedic surgeons. Open reduction and internal fixation has been the gold standard for displaced fractures involving weightbearing dome and fractures with intra-articular fragments [3, 5]. The goal of treatment relies on restoration of articular anatomy with stable internal fixation, allowing early mobilization of the patient [3, 5]. In most situations, the fixation of the displaced fracture requires extensive exposure, which may lead to complications including blood loss, neural or vascular injury, postoperative infection, wound healing problems and heterotopic bone formation. However, fractures with mild displacement in the weightbearing area or fractures through the non-weightbearing area can be treated with percutaneous screwing with the advent of fluoroscopy and even with a computerized navigation system. The conventional fluoroscopy used in percutaneous screwing of acetabular fractures requires multiple images in different projections for screw placement [6, 7, 9, 10]. This leads to prolonged surgical and radiation time. With the help of a fluoroscopy-based computerized navigational system, radiation exposure and surgical time can be reduced prominently with good accuracy [1, 6]. We had nine patients with mildly displaced anterior column fractures or transverse fracture of the acetabulum fixed with cannulated screws under conventional fluoroscopy; however; we did not have any experience with the advanced intraoperative imaging including 3D-flouroscopy and CT in our prior practice. We proposed that a fluoroscopy-based computerized navigational system would simplify operation procedures. The purpose of this study is to test the application of the fluoroscopy-based computerized navigational system for anterior column fracture of the acetabulum.
Materials and methods
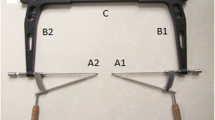
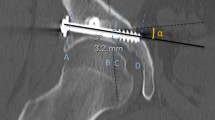
A prospective cohort study was conducted from September 2005 to March 2006. All patients with acutely nondisplaced anterior column fractures of the acetabulum or mildly displaced fractures that could be reduced on fracture table by close method were included. Initial fixation with an anterior lag screw under a fluoroscopy (GE OEC FlexiView 8800™ Image Gallery)-based computer navigation system (BrainLab Vectorvision® trauma ver 2.5.0) was performed. If the fracture could not be reduced by the close method, open reduction and internal fixation was performed. Patients receiving open reduction and internal fixation were excluded. In total, three patients treated with this method and followed up for more than 1 year were included in this study (Table 1). There were two males and one female with a mean age of 39 years (range 25–58). No other associated injuries were noted except initial loss of consciousness in two patients. Anterior column fracture with minimal displacement and mild widening of the acetabular socket in the anteroposterior direction on CT imaging were noted in 2 patients and non-displaced linear fracture was noted in one patient (Fig. 1a, b). Surgery was performed after the symptoms of head injury subsided. During surgery, the patient lay on the fracture table with traction in a supine position. Two fiducial screws with tracers were placed in the iliac crest on the same side of the fracture for registration. Intra-operative planning of screwing was performed with a fluoroscopy-based computer navigation system after close reduction under fluoroscopy. The skin was incised about 3 cm center at the point extended from the planned screw. Pin insertion was guided under the computer navigation system. Then the position of the pin was validated with conventional 2D fluoroscopy in different views. The length of the screw was measured by the computer after application of the guided pin. An AO Synthes® 6.5 mm cannulated screw was applied with compression over the fracture interface and the position of screw was validated by fluoroscopy. All screws were placed in the medullary canal of the anterior column without penetrating the cortex. Patients were allowed to perform joint movement exercises and to walk with partial weightbearing on the first day post-operatively. All patients were seen at 6 weeks, 3 months, 6 months and 1 year after the operation.
Radiography and computer tomography of a 25-year-old female with anterior column fracture of the left acetabulum. a Minimal displacement of the fracture is noted on the plain film. b Computer tomography shows mild widening of the acetabular socket in the anterior–posterior direction. c Solid union in anatomic position is noted in the follow-up radiography 1 year after operation
Results
The mean operation time was 40 min (range 30–45 min) from the use of fluoroscopy to wound closure and the mean total fluoroscopy time was 38 s (range 35–45 s). Total blood loss was less than 10 ml. All patients felt pain free 1 week after the operation and could walk without any aid 4 weeks postoperatively. No complication was noted postoperatively. Radiography revealed callus formation at 6 weeks without loss of reduction in all patients (Fig. 1c)
Discussion
In our study, we successfully applied the screw in the minimally displaced anterior column fracture of the acetabulum by fluoroscopic-based computerized navigation. All the screws were placed in the medullary canal of the anterior column without penetrating the cortex. All fractures healed smoothly without loss of reduction. All patients got pain relief and good functional recovery in short term after operation through a minimally invasive approach.
The treatment goal of acetabular fracture is anatomic or near-anatomic reduction of the articular surface [3, 5]. At the same time, prevention of complications related to surgical exposure is as important as quality of reduction of articular surface. Therefore, it is reasonable to develop a method to fix minimally displaced fractures requiring fixation with limited surgical exposure [2, 12].
Gay et al. [2] were the first to report on successful percutaneous fixation of mildly displaced acetabular fracture under CT guidance. Good reduction was achieved in five of six patients. Routt et al. [10] showed percutaneous screwing for superior ramus fracture under fluoroscopy, although it is a demanding technique. Parker and Copeland reported of eight patients with displaced acetabular fracture being treated with closed reduction and percutaneous screwing. Starr et al. [12] revealed about three displaced acetabular fractures fixed with cannulated screws under fluoroscopic guidance. Norris et al. [8] provided the idea that intra-operative fluoroscopy was as useful as CT for the evaluation of reduction and confirmation of extra-articular placement of implants. Crowl and Kahler [1] reported on nine patients treated with percutaneous screwing under computer-assisted virtual fluoroscopy guidance. However, only few cases were of patients having anterior column fractures. Percutaneous screwing for anterior column fractures in the acetabulum is a demanding procedure [4, 9, 12]. Surgeons who perform this kind of procedure must be familiar with the 3D anatomy of the pelvis and pelvic radiographic anatomy in multiple planes including inlet, outlet, iliac oblique and obturator oblique views. At the same time, it requires simultaneous multi-planar radiographic confirmation of pin and screw intra-operatively, which increases the difficulty of this procedure. Mouhsine et al. [7] reported a mean fluoroscopic time of 62 s and a mean operative time of 30 min in percutaneous screwing by flouoroscopy only. Starr et al. [11] revealed a mean operative time of 75 min in percutaneous screwing of displaced fracture of the acetabulum. Crowl and Kahler [1] reported an average of 73 s of fluoroscopy in percutaneous screw fixation of anterior column acetabular fractures with fluoroscopy only, and the fluoroscopy time decreased to less than 45 s with computer-assisted image. In our study, the fluoroscopy time was 30–45 s, the operation time was 35–45 min and blood loss was less than 10 ml. This is our initial experience in performing this kind of surgery. With fluoroscopic-based computerized navigation, we can determine the position of the guide pin and screw real time intra-operatively. Moreover, the entry point of the screw can be settled by the extended line of the planned screw, which makes it easier to incise the wound properly. Besides, radiation exposure and operative time could be reduced to a great extent. Complications associated with surgery could be decreased, as the position of the guide pin and screw would be proper and surgical exposure limited. Once anatomic reduction could be achieved by the close method in the anterior column fracture of the acetabulum, based on our limited experience, we infer that with increasing experience, percutaneous screw fixation under fluoroscopic-based computerized navigation may be a reliable method. Though the indication for this procedure is limited, we think that there should be potential to apply the screw with less radiation by fluoroscopic-based computerized navigation. Based on our experience, the navigation system should be safe if all the fiducial screws and tracers do not change their position during the operation, but we also think it is necessary to validate the position of the guide pins and the screw by fluoroscopy.
The limitation of this study is that we performed this kind of surgery in only three patients. More cases are needed to reach a more convincing conclusion. In addition, the computer navigation system is quite expensive, maybe more than 300,000 USD. Not every hospital can afford this type of equipment. Validation by fluoroscopy should be always needed, because some minimal changes in fiducial screws or tracers may lead to incorrect guidance. It would be easier to apply the guide pin by the computerized navigation system than by percutaneous screwing under fluoroscopy only because of monitoring of multiple planes simultaneously; however, the computerized navigation system cannot completely replace fluoroscopy.
In conclusion, in some selected patients with mildly displaced acetabular fracture, percutaneous fixation with screw can be achieved by fluoroscopic-based computerized navigation system and stability can be achieved immediately after operation with few complications. Early mobilization and partial weightbearing can be permitted postoperatively. We believe fluoroscopic-based computerized navigation can produce excellent results in selected patients with mildly displaced acetabular fracture and will become an important part of the orthopedic surgeons’ tools for the treatment of certain acetabular fractures in the future, especially for elder patients who cannot tolerate either extensive surgical procedures or long-term bed rest with conservative treatment.
References
Crowl AC, Kahler DM (2002) Closed reduction and percutaneous fixation of anterior column acetabular fractures. Comput Aided Surg 7:169–178
Gay SB, Sistrom C, Wang GJ, Kahler DA, Boman T, McHugh N, Goitz HT (1992) Percutaneous screw fixation of acetabular fractures with CT guidance: preliminary results of a new technique. AJR Am J Roentgenol 158:819–822
Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res 81–106
Matta JM (1998) Percutaneous fixation of acetabular fractures. J Orthop Trauma 5:370
Matta JM, Merritt PO (1988) Displaced acetabular fractures. Clin Orthop Relat Res 83–97
Mosheiff R, Khoury A, Weil Y, Liebergall M (2004) First generation computerized fluoroscopic navigation in percutaneous pelvic surgery. J Orthop Trauma 18:106–111
Mouhsine E, Garofalo R, Borens O, Wettstein M, Blanc CH, Fischer JF, Moretti B, Leyvraz PF (2005) Percutaneous retrograde screwing for stabilisation of acetabular fractures. Injury 36:1330–1336
Norris BL, Hahn DH, Bosse MJ, Kellam JF, Sims SH (1999) Intraoperative fluoroscopy to evaluate fracture reduction and hardware placement during acetabular surgery. J Orthop Trauma 13:414–417
Parker PJ, Copeland C (1997) Percutaneous fluoroscopic screw fixation of acetabular fractures. Injury 28:597–600
Routt ML Jr., Simonian PT, Grujic L (1995) The retrograde medullary superior pubic ramus screw for the treatment of anterior pelvic ring disruptions: a new technique. J Orthop Trauma 9:35–44
Starr AJ, Jones AL, Reinert CM, Borer DS (2001) Preliminary results and complications following limited open reduction and percutaneous screw fixation of displaced fractures of the acetabulum. Injury 32 Suppl 1:SA45–SA50
Starr AJ, Reinert CM, Jones AL (1998) Percutaneous fixation of the columns of the acetabulum: a new technique. J Orthop Trauma 12:51–58
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors declare that no funding or any other kind of financial support was got for this study.
Rights and permissions
About this article
Cite this article
Lin, YC., Chen, CH., Huang, HT. et al. Percutaneous antegrade screwing for anterior column fracture of acetabulum with fluoroscopic-based computerized navigation. Arch Orthop Trauma Surg 128, 223–226 (2008). https://doi.org/10.1007/s00402-007-0369-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-007-0369-9