Abstract
CAG repeat diseases are hereditary neurodegenerative disorders caused by expansion of a polyglutamine tract in each respective disease protein. They include at least nine disorders, including Huntington’s disease (HD), dentatorubral pallidoluysian atrophy (DRPLA), spinal and bulbar muscular atrophy (SBMA), and the spinocerebellar ataxias SCA1, SCA2, SCA3 (also known as Machado-Joseph disease), SCA6, SCA7, and SCA17. It is thought that a gain of toxic function resulting from the protein mutation plays important and common roles in the pathogenesis of these diseases. Recent studies have disclosed that, in addition to the presence of clinical phenotypes and conventional neuropathology in each disease, human brains affected by CAG repeat diseases share several polyglutamine-related changes in their neuronal nuclei and cytoplasm including the formation of intranuclear inclusions. Although these novel pathologic changes also show a distribution pattern characteristic to each disease, they are generally present beyond the lesion distribution of neuronal loss, suggesting that neurons are affected much more widely than has been recognized previously. Various mouse models of CAG repeat diseases have revealed that CAG repeat lengths, which are responsible for polyglutamine diseases in humans, are not sufficient for creating the conditions characteristic of each disease in mice. Although high expression of mutant proteins in mice results in the successful generation of polyglutamine-related changes in the brain, there are still some differences from human pathology in the lesion distribution or cell types that are affected. In addition, no model has yet successfully reproduced the specific neuronal loss observed in humans. Although there are no models that fully represent the neuropathologic changes present in humans, the data obtained have provided evidence that clinical onset is not clearly associated with neuronal cell death, but depends on intranuclear accumulation of mutant proteins in neurons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
CAG repeat diseases are a group of hereditary neurodegenerative disorders caused by expansion of a CAG repeat that encodes polyglutamine in each respective disease gene. At least nine such disorders are known, including Huntington’s disease (HD), dentatorubral-pallidoluysian atrophy (DRPLA), spinal and bulbar muscular atrophy (SBMA), and spinocerebellar ataxias (SCAs) types 1, 2, 3 (also known as Machado-Joseph disease), 6, 7, and 17 [98]. Although each of these CAG repeat disorders has characteristic clinical symptoms and neuropathology, studies of affected humans and animal models suggest that a gain of toxic function resulting from the mutation plays a pivotal and common role in the pathogenesis. Therefore, most of the available animal models of these disorders are transgenic mice, which express mutant proteins with expanded polyglutamine stretches. The formation of neuronal intranuclear inclusions (NIIs) in transgenic mice expressing exon 1 of the HD gene with 113–156 CAG repeats [10] triggered the discovery of similar inclusions in the brains of humans with CAG repeat diseases. Because NIIs have been shown to possess antigenicity for expanded polyglutamine stretches as well as the causative gene products of each disease, NII formation has now become a pathologic hallmark common to all CAG repeat diseases. Although NIIs were initially thought to be toxic structures responsible for neuronal cell death in affected brain regions, subsequent investigations raised the possibility that NII formation itself might be a cellular reaction designed to reduce the acute toxic effect of the mutant proteins [9, 38, 69]. Detailed neuropathologic studies of human brains have revealed the presence of NIIs in various brain regions far beyond the lesions characterized by neuronal loss, and also other pathologic changes related to the expression or accumulation of mutant proteins with expanded polyglutamine stretches. To elucidate the molecular mechanisms underlying polyglutamine pathogenesis, various animal models of CAG repeat diseases have been generated. Although some of these models have provided valuable insights into the molecular basis of polyglutamine neurodegeneration, their pathology does not completely fit that in the human brain. In this review, we summarize the clinicopathologic features of CAG repeat diseases (SCA1, 2, 3, and 7, DRPLA and SBMA), and highlight the similarities and differences of neuropathology between human and animal models (Table 1). Because no mouse models have been generated on SCA6 and 17, we include only their neuropathologic findings of human brains in Table 1. We also include spinocerebellar ataxia type 8 in this review.
Spinocerebellar ataxia type 1
SCA1 is a dominantly inherited form of spinocerebellar degeneration caused by expansion of a CAG repeat in the SCA1 gene localized to chromosome 6p23 [97]. The numbers of CAG repeat units in patients with SCA1 range from 40 to 81, and correlate inversely with the age at onset and disease severity. The clinical features in the early stages of SCA1 are characterized by progressive ataxia, pyramidal impairment and oculomotor palsy, followed in the later stages by amyotrophy and sensory disturbance. Cognitive functions typically remain intact. Neuropathologic studies have revealed atrophy of the brainstem and spinal cord, which are more marked in patients with juvenile onset. The cerebellum may be atrophic, but the cerebrum typically appears normal. The brain weight mostly ranges from 1,100 to 1,200 g [36]. In the cerebellum, Purkinje cells are mildly to moderately depleted, but in some patients the cerebellar cortex appears almost normal. Torpedoes are occasionally observed in the granular layer. The cerebellar dentate nucleus also shows mild to moderate neuronal loss, associated with grumose degeneration, which is characterized by accumulation of numerous eosinophilic and argyrophilic granular materials around the somata and dendrites of dentate neurons. In the brainstem, neuronal loss is observed in the pontine nuclei and inferior olivary nucleus, although this is relatively mild in comparison with that found in SCA2. The substantia nigra, red nucleus and cranial nerve nuclei including the vestibular and oculomotor nuclei are often affected. The spinal cord shows apparent neuronal loss in the anterior horn and Clarke’s column with degeneration of the spinocerebellar tracts. The posterior column shows various degrees of degeneration. In the cerebrum, no apparent change is evident in the cortex, white matter, striatum or thalamus, although mild to moderate degeneration is often observed in the outer segment of the globus pallidus. The inner segment of the globus pallidus may be involved in some patients [83].
NIIs are observed in broad areas of the brain [15], such as the cerebral cortex, striatum, globus pallidus, substantia nigra, pontine nuclei, reticular formation, inferior olive, dentate nucleus and spinal anterior horn, with the highest incidence in the pontine nuclei (Fig. 1a). They are eosinophilic and spherical, and present singly or occasionally in pairs in a nucleus. Their sizes may vary even in the same patient, ranging from ∼1 to 3 μm in diameter. NIIs are inconspicuous using hematoxylin-eosin staining, but easily detectable by immunohistochemistry for ubiquitin, ataxin-1 (a protein construct of the SCA1 gene), and expanded polyglutamine stretches (using a monoclonal antibody 1C2 [80]). It should be noted that no inclusion has been found in Purkinje cells, which are an essential cell type involved in SCA1 pathogenesis. As observed in the other CAG repeat diseases including SCA2, Machado-Joseph disease and DRPLA [24, 42], Purkinje cells in the human brain are unique neuronal population that do not show prominent NII formation, even though mutant proteins accumulate in their nuclei. In addition to NIIs, immunohistochemistry using 1C2 antibody discloses granular labeling in the neuronal cytoplasm in some brain regions such as the reticular formation and oculomotor nucleus. Diffuse nuclear labeling of neurons, which is also detected in the brains of patients with Huntington’s disease and DRPLA, is observed in brain regions showing NII formation. No inclusions have been reported in glial cells.
Neuronal intranuclear inclusions in the pontine nuclei of patients with spinocerebellar ataxia type 1 (a) and Machado-Joseph disease (b–e). Round inclusions are present in the neuronal nuclei in a single (b, e) or doublet (a, c, d) form. d Fine granular labeling is also seen in the cytoplasm and nucleoplasm. e An intranuclear inclusion is non-membrane bound, and contains a mixture of granular and filamentous structures, the latter being approximately ∼12–15 nm in diameter and organized in random but sometimes parallel arrays. Arrows in b and e indicate intranuclear inclusions. a, d Immunohistochemistry for expanded polyglutamine stretches with 1C2 antibody; b hematoxylin-eosin stain; c immunohistochemistry for ubiquitin; e electron micrograph. Scale bars: a–d, 10 μm; e 1 μm
In order to study Purkinje cell pathology, SCA1 transgenic mice have been generated showing expression of full-length human SCA1 cDNAs with 82 (Q82) CAG repeats using a Purkinje cell-specific promoter, L7 [5, 8, 73]. The Q82 heterozygous mice (B05 line), however, develop progressive neurological abnormalities and ataxia commencing at ∼12 weeks of age. The Purkinje cells show several neuropathologic changes such as cytoplasmic vacuolation, progressive dendritic atrophy and ectopic location of the cell bodies within the molecular layer. NII formation has been detected in Purkinje cells, and the incidence increases with age from 25% at 6 weeks to 90% at 12 weeks. Purkinje cell loss becomes significant (∼32% decrease) at 24 weeks. Torpedoes are not observed in the cerebellar cortex, and mice usually have a normal life span. These results suggest that the development of ataxia results not from neuronal death, but from cellular dysfunction and morphological alterations that precede it. Although this mouse model provides some insight into the disease mechanism in Purkinje cells caused by the expression of mutant ataxin-1 with expanded polyglutamine stretches, the Purkinje cells show morphological changes somewhat different from those in the human SCA1 brain with respect to cytoplasmic vacuolation, ectopic location, and inclusion formation. These differences may be related to the fact that the B05 transgenic line expresses around 50–100 times the endogenous level of the mutant protein in Purkinje cells.
To provide a more accurate genetic model of SCA1, “knockin” mice have been generated by introducing the human mutation into the corresponding mouse gene. The mouse model carrying 78 CAG repeats in the mouse Sca1 locus expresses expanded ataxin-1 at endogenous levels in a proper spatial and temporal pattern; however, the mice show only mild behavioral changes late in life [48]. A neuropathologic study has revealed no neuronal loss or inclusion formation in the brain in this model. These results suggest that the mutant ataxin-1 protein with 78 glutamine residues, which is expressed at endogenous levels, is not sufficient to cause pathologic changes during the short life span of the mouse. In contrast, a knockin mouse model carrying 154 CAG repeats developed neurological abnormalities commencing at around 9 weeks of age, which progressed to neurological phenotypes including ataxia, wasting, and cognitive deficits. Most of the mice died by 45 weeks of age, accompanied by age-related hippocampal synaptic dysfunction [86]. The brain showed uniform atrophy with dilatation of all the ventricles. Purkinje cell loss with dendritic degeneration was noticeable by 34 weeks of age, and this reached 23% by 40 weeks. Hippocampal pyramidal neurons did not show significant depletion. NII formation was first observed in the cerebral cortex, hippocampal CA1 region and thalamus at 6 weeks of age, and thereafter expanded to multiple brain regions such as the caudate, putamen, brainstem and spinal cord. At 20 weeks of age, NIIs were detected in more than 80% of neurons in the cerebral cortex and hippocampus. In contrast, Purkinje cells showed a paucity of inclusion formation. No NII was detected in the hypothalamus or cerebellar granule neurons. Immunohistochemically, NIIs were positive for ataxin-1, ubiquitin and several transcription factors. The neuropathology of this mouse model resembles that of SCA1 patients in that the brain shows generalized atrophy, selective Purkinje cell loss, and widespread NII formation with a relatively low frequency in Purkinje cells. Further studies will be required to clarify whether other brain regions such as the pontine nuclei and inferior olive, which are known to be regions typically affected in SCA1 patients, show neuronal depletion. Although the distribution pattern of NIIs in the mouse model is reminiscent of that seen in SCA1 patients, the frequency of NII formation in each brain region differs somewhat between the mouse model and human. The reason for this difference is unknown, but may be due to differences in metabolic or degradation activity on accumulated mutant proteins. These phenomena in the mouse model clearly indicate that the appearance of clinical phenotypes depends on the localization of mutant ataxin-1 to neuronal nuclei, and not on the occurrence of neuronal loss.
Spinocerebellar ataxia type 2
SCA2 is a dominantly inherited neurodegenerative disease caused by expansion of a CAG repeat in the SCA2 gene localized to chromosome 12q24.1 [33, 57, 62, 66]. The numbers of CAG repeat units in patients with SCA2 range from 35 to 64. The clinical features in the early stages of SCA2 are characterized by progressive ataxia, diminished tendon reflexes and slow eye movement, followed in the later stages by amyotrophy, sensory disturbance, involuntary movements and mental deterioration. Neuropathologic studies have revealed atrophy of the cerebellum and pontine base. The substantia nigra is depigmented. The brain weight mostly ranges from 690 to 1,265 g [14, 36, 57]. In the cerebellum, Purkinje cells and granule cells are moderately to severely depleted, but the dentate nucleus is typically spared. In the brainstem, the pontine nuclei, inferior olive and substantia nigra are severely affected. Moderate degeneration is also detected in the red nucleus. The involvement of the spinal anterior horn and dorsal column is variable. Mild degeneration may be encountered in the basal ganglia, thalamus and cerebral cortex in some patients.
Ataxin-2 has a cytoplasmic localization in normal brain, and the SCA2 gene is expressed in Purkinje cells and some specific groups of brainstem and cortical neurons [28]. Purkinje cells in SAC2 patients also possess many cytoplasmic granules immunopositive for ataxin-2 and expanded polyglutamine stretches [29]. These intracytoplasmic granules are negative for ubiquitin. In contrast to the other CAG repeat diseases, NII formation is not prominent in SCA2. Ubiquitinated NIIs have been found only in 1–2% of pontine neurons. They are also detectable in the other affected regions such as the substantia nigra, inferior olive, globus pallidus and cerebral cortex, but not in Purkinje cells [41].
SCA2 transgenic mice have been generated by expressing full-length human SCA2 cDNAs with 58 (Q58) CAG repeats under the control of the Purkinje-cell-specific PcP2/L7 promoter [29]. The Q58 mice display progressive functional deficits, such as the impaired motor performance, accompanied by loss of the Purkinje cell dendritic arbor and finally loss of Purkinje cells. Although the 1C2 and ataxin-2 immunostaining is located throughout the Purkinje cell cytoplasm with some granular vesicles, no inclusion is detected in the neuronal nuclei. Recently, Aguiar et al. [3] have generated transgenic mice expressing full-length ataxin-2 with 75 glutamines using the human SCA2 promoter. The mice display impaired motor performance, and exhibit Purkinje cell degeneration. It will be necessary to study the polyglutamine-related pathology in these mice, for elucidating molecular mechanisms underlying the SCA2 pathogenesis.
Machado-Joseph disease/spinocerebellar ataxia type 3
Machado-Joseph disease (MJD) is a dominantly inherited multisystem neurodegenerative disorder characterized by variable combinations of cerebellar ataxia, pyramidal signs, dystonic extrapyramidal symptoms, peripheral neuropathy with amyotrophy, nystagmus, eyelid retraction, external ophthalmoplegia, and facial fasciculation [63, 76]. Dystonia is often prominent in younger patients. The disorder is linked to an unstable CAG repeat on chromosome 14q32.1. The numbers of CAG repeat units in patients with MJD range from 56 to 84. The brain weight of affected patients mostly ranges from 1,000 to 1,300 g. In most cases, there is obvious atrophy of the brainstem and spinal cord, and the substantia nigra is depigmented. The cerebellum may also be atrophic due to loss of white matter volume. Atrophy with brownish discoloration is occasionally evident in the globus pallidus and subthalamic nucleus. The main lesions in MJD are located in the spinocerebellar system and cerebellar dentate nucleus [36, 93]. In the spinal cord, Clarke’s column generally shows severe neuronal loss with marked degeneration of the spinocerebellar tracts. Severe degeneration is also detected in the anterior horn, with consequent degeneration of the anterior spinal roots and skeletal muscles of the extremities. The involvement of the spinal posterior horn and dorsal column is variable and usually mild. In most cases, no apparent abnormality is detected in the corticospinal tract. In the brainstem, mild to moderate neuronal loss is detectable in the pontine nuclei, with accentuation in the caudal region. Neuronal depletion is also evident in the substantia nigra, reticular formation, accessory cuneate nucleus, and cranial nerve nuclei including the nuclei of the external ocular muscles, and hypoglossal and vestibular nuclei. Although variable degrees of degeneration may be present in the red and dorsal column nuclei, the inferior olive is typically spared. The cerebellar cortical neurons are preserved in most cases, but minimal loss of Purkinje cells and occasional torpedoes are encountered in some patients. The cerebellar white matter is atrophic and shows myelin pallor due to degeneration of the pontocerebellar and spinocerebellar fibers. The dentate nucleus shows moderate to severe loss of neurons with grumose degeneration. In the globus pallidus, the internal segment is more severely affected. Severe neuronal loss is also detectable in the subthalamic nucleus. The thalamus may display mild degeneration, especially in the centromedian nucleus; however, no significant degeneration is detected in the striatum or cerebral cortex.
NII formation is found in the affected brain regions, and shows a relatively high incidence among the CAG repeat diseases [61, 71]. In addition, as in other polyglutamine disorders, NIIs are detectable in unaffected regions including the cerebral cortex, thalamus (especially the intralaminar nucleus), striatum, lateral geniculate body, inferior olive, and dorsal root and sympathetic ganglia [88, 93]. The distribution is generally wider in patients with a longer expansion of the CAG repeat. No inclusion has been observed in Purkinje cells [42, 93]. NIIs are spherical and eosinophilic, and vary in size from ∼1 to 4 μm (Fig. 1b). They are present in the nucleus as a single structure or frequently as doublets. Immunohistochemistry reveals that NIIs are positive for ubiquitin (Fig. 1c), ataxin-3, expanded polyglutamine stretches (Fig. 1d) and several transcription factors. Ultrastructurally, NIIs are non-membrane bound, and contain a mixture of granular and filamentous structures, the latter being approximately ∼12–15 nm in diameter and organized in random but sometimes parallel arrays (Fig. 1e). There is a relationship between NIIs and nuclear structures such as promyelocytic leukemia protein nuclear bodies and coiled bodies [90]. The widespread occurrence of NIIs suggests that neurons are affected in the polyglutamine pathogenesis of MJD to a much greater extent than has been recognized by conventional neuropathologic studies. A neuropathologic study of a MJD patient, who was suspected to have died at an early stage of the disease, indicated that extensive formation of NIIs may be an early pathologic change, and that NII formation is related to phenotypic expression in the disease [93]. In contrast to the frequent formation of NIIs, diffuse nuclear immunolabeling for expanded polyglutamine stretches is a rare finding in MJD brains. In addition to NIIs, affected neurons possess many cytoplasmic granules immunolabeled with 1C2. Electron microscopy has shown that the granules are a subset of lysosomes [91]. The appearance of this cytoplasmic pathology involves many brain regions with a distribution pattern generally similar to that of NII, suggesting that mutant proteins in the MJD brain are involved in both the ubiquitin/proteasome and endosomal/lysosomal pathways for protein degradation in different intraneuronal compartments. The cytoplasmic pathology is also observed in Purkinje cells of SCA6 (Fig. 2a), but absent in SCA17 (Fig. 2b). No pathologic changes related to polyglutamine pathology have been reported in glial cells or visceral organs.
Polyglutamine-related pathology in Purkinje cells of patients with spinocerebellar ataxia type 6 (a) and spinocerebellar ataxia type 17 (b), as well as in the cerebellar dentate (c, d) and pontine nuclei (e) neurons of patients with dentatorubral-pallidoluysian atrophy. a Fine granular immunolabeling is evident in the cytoplasm and nucleus (arrow). b Diffuse immunolabeling is evident in the nucleus. c Immunolabeling is seen in an intranuclear inclusion (arrow) as well as in the nucleoplasm in a diffuse pattern. d Skein-like inclusions are present in the neuronal cytoplasm. e An intranuclear inclusion is non-membrane bound, and composed of granular materials with occasional filamentous structures. a–d Immunohistochemistry for expanded polyglutamine stretches with 1C2 antibody; e electron micrograph of a neuronal intranuclear inclusion. Scale bars: a–d, 10 μm; e 1 μm
To clarify the pathogenesis of MJD, different transgenic mouse models have been generated. To determine whether the full-length mutant protein or merely the expanded glutamine repeat induces polyglutamine diseases, Ikeda et al. [31] generated SCA3 transgenic mice using a L7 promoter, which express the full-length or a truncated form of ataxin-3 with 79 glutamines in Purkinje cells. The mice carrying truncated ataxin-3 became ataxic and showed degeneration of all three layers of the cerebellum. Although it is noteworthy that this mouse model showed sufficient expansion of the polyglutamine tract to cause neuronal death, this is not a genetic model of SCA3 because of the selected targeting of Purkinje cells for neurodegeneration, which is a neuronal type scarcely affected in human MJD. In the second model, Cemal et al. [7] used a yeast artificial chromosome (YAC) to generate transgenic mice carrying the entire human MJD1 gene with its own promoter. The mice carrying a single or multiple transgene copies with expanded alleles (Q64–84) showed neurological phenotypes including ataxia, hypotonia, and motor and sensory loss, and exhibited neuronal loss in the pontine and dentate nuclei. In the cerebellar cortex, Purkinje cell loss increased with CAG-repeat length and increasing transgene copy number. The mice also showed degeneration of peripheral nerves and dorsal root ganglia. NII formation was detected in the affected brain regions and cranial nerve nuclei, with relatively low frequency in Purkinje cells. In contrast to the features of the mouse model created by Ikeda et al. no cleavage fragments of mutant ataxin-3 were detected. This mouse model is expected to reveal some aspects of the neurodegenerative processes underlying MJD pathogenesis, although the neuropathologic changes differ slightly from those of human MJD brains in terms of lesion distribution. The difference may partly depend on the expression levels of mutant ataxin-3 in each brain region. The third mouse model was generated to express human mutant (Q71) ataxin-3 mjd1a, a mutant ataxin-3 isoform resulting from alternative splicing, under control of the mouse prion promoter [20]. The high level of transgene expression indicated enrichment of ataxin-3 and its putative cleavage fragment in the nuclear fraction of brain homogenates from ataxic mice. Q71 mice expressing mutant proteins above a critical level developed phenotypes including progressive postural instability, gait and limb ataxia, weight loss and premature death. Although no neuronal loss was detected in the brain, prominent NII formation was observed in several brain regions including the olfactory bulb, deep cerebellar nuclei, pontine nuclei and spinal anterior horn. This mouse model is an example showing high expression of mutant ataxin-3 throughout the brain, and the results indicate that phenotypic expression does not depend on neuronal depletion but probably on neuronal dysfunction due to intranuclear accumulation of mutant proteins. The growth and persistence of NIIs suggests that the inclusions themselves are not directly cytotoxic to neurons. More recently, Bichelmeier et al. [4] generated SCA3 transgenic mice expressing full-length ataxin-3 with 70 or 148 glutamines under control of the mouse prion promoter. The Q70 mice developed neurological phenotypes that included tremor, behavioral deficits, strongly reduced motor and exploratory activity, and premature death. Ataxin-3- and ubiquitin-positive NIIs were detected in almost every examined brain regions except Purkinje cell layer. Although no significant Purkinje cell loss was detected, the cell bodies showed a striking shrinkage. The Q148 mice developed an even more pronounced phenotype with more inclusions and earlier death. The mice transgenic with the same construct but attached to a nuclear export signal developed a miler phenotype with less inclusions, suggesting that nuclear localization of mutant ataxin-3 is required for the manifestation of symptoms in SCA3. In all of these transgenic mouse models, no pathologic changes have been reported in the cytoplasm of neurons.
Spinocerebellar ataxia type 7
SCA7 is a dominantly inherited spinocerebellar degeneration characterized by retinal-cerebellar atrophy, and caused by expansion of a CAG repeat in the SCA7 gene localized to chromosome 3p12-13 [16, 21, 22, 26, 50, 55]. The SCA7 repeat is one of the most unstable CAG repeats known, and the number of repeats in patients ranges from 38 to 460 [85]. There is a marked variability in age at onset and severity of the symptoms. The main clinical features include a decrease of visual acuity, progressive cerebellar ataxia, dysarthria, and dysphagia. Typically, no dementia or epilepsy is noted. Patients with extremely long CAG repeat stretches show juvenile or infantile onset, more rapid disease progression, and a broader spectrum of phenotypes than those with the adult onset form. Although the SCA7 gene products are expressed throughout the brain and retina, neurodegeneration is restricted in some regions. Grossly, the brains of SCA7 patients show atrophy of the optic pathways and cerebellum. Histologically, the retinas exhibit severe degeneration of the pigmented epithelium and loss of photoreceptors, bipolar cells and ganglion cells, with consecutive degeneration from the optic nerves to optic radiations including the lateral geniculate bodies. In the cerebellum, degeneration is observed in the cortex (Purkinje cell dominant), spinocerebellar and olivocerebellar tracts, and dentate nucleus. Although the inferior olive is generally involved, the degeneration of the ponto-cerebellipetal system is variable. The pyramidal pathways and motor neurons in the brainstem and spinal cord are also affected. Degeneration may be evident in the subthalamic nucleus, globus pallidus and substantia nigra in some patients. The cerebral cortex and thalamus are typically free from degeneration.
NIIs are detected in the affected brain regions with a relatively high incidence in the inferior olive [27]. Interestingly, NIIs are also observed in areas of the cerebral cortex such as the supramarginal gyrus and insula. In addition to NIIs, 1C2 immunostaining reveals cytoplasmic granular staining in neurons in some brain regions including the supramarginal gyrus, hippocampus, thalamus, geniculate body and pontine nuclei, and is not always dependent on NII formation. No pathologic changes are detectable in glial cells. In spite of the severe phenotype, infantile-onset SCA7 patients show relatively limited neuronal degeneration in the cerebellum and retina [6, 12, 65, 79].
La Spada et al. [43] and Garden et al. [19] have generated transgenic mice expressing full-length ataxin-7 with 92 glutamines using the murine prion protein promoter. Overexpression of the mutant proteins caused a cone-rod dystrophy type of retinal degeneration and visual impairment in the mice. Intranuclear inclusions were formed in all three nuclear layers of the retina. The mice also showed progressive ataxia and premature death. Histologically, the brains disclosed no obvious neuronal loss; however, NII formation was detected in many brain regions such as the cerebellar granule cells, hippocampus, pontine nuclei and inferior olivary nucleus. Interestingly, Purkinje cells showed progressive atrophy of their soma and dendritic arbors, despite a lack of mutant protein expression, suggesting the occurrence of trans-synaptic degeneration of Purkinje cells in an anterograde or retrograde manner through involvement of the adjacent, synaptically communicating neurons in polyglutamine pathogenesis. Trans-synaptic neuronal degeneration was also observed in the other transgenic murine models of SCA7 [95]. To produce an authentic model of SCA7, Yoo et al. [94] generated knockin mice carrying 266 CAG repeats that cause infantile onset SCA7 in humans. These mice exhibited clinical features that included ataxia, visual impairment and premature death, and showed functional abnormalities such as retinal dysfunction and impaired short-term synaptic plasticity. Although no significant Purkinje cell loss was detected, the cell bodies became significantly smaller than those of wild-type Purkinje cells. The retina of the mutant mice showed progressive atrophy and loss of photoreceptors. Importantly, the retinal dysfunction occurred prior to photoreceptor loss. Although mutant ataxin-7 accumulated in multiple brain regions, neurons of the retina and cerebellum showed earlier accumulation of the proteins than other areas of the brain. Intranuclear inclusions in neurons of the cerebellum, hippocampus and retina appeared at relatively later stages of the disease course. Interestingly, in the other brain regions, nuclear inclusions appeared more rapidly, but were localized in glial cells. Although the distribution pattern of nuclear inclusions should be further compared between mice and humans, the possible expression of mutant ataxin-7 at endogenous levels with a proper spatio-temporal pattern in the mice may contribute to the development of a lesion distribution that is relatively similar to that in patients with infantile-onset SCA7. The pathology seen in adult SCA7 patients has not yet been fully represented by animal models.
Dentatorubral-pallidoluysian atrophy
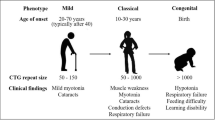
DRPLA is an autosomal dominant neurodegenerative disorder caused by an expansion of the CAG repeat in the DRPLA gene located on chromosome 12p13.31. The number of CAG repeat units in DRPLA patients ranges from 49 to 84. Intergenerational instability is more pronounced in paternal transmission. DRPLA patients show various symptoms, such as myoclonus, epilepsy, ataxia, choreoathetosis and dementia, and the combinations of these symptoms depend on the age at onset [53]. Patients with earlier onset (generally below the age of 20 years) show progressive myoclonus, epilepsy and mental retardation (juvenile type, as classified by Naito). Patients showing late disease onset (over the age of 40 years) predominantly show cerebellar ataxia and dementia (late-adult type). Patients in whom the disease appears between the third and fifth decades belong to an intermediate type, and usually show ataxia and choreoathetosis (early-adult type). There is a reverse correlation between the age at onset and CAG repeat length. In contrast to the considerable heterogeneity in clinical presentation, the neuropathology of the DRPLA brain shows a relatively uniform pattern of lesion distribution, with combined degeneration of the dentatorubral and pallidoluysian systems. The globus pallidus and subthalamic nucleus (Luys body) show consistent loss of neurons with astrocytic gliosis. In the globus pallidus, neuronal depletion is more severe in the lateral segment than in the medial segment. The dentate nucleus also shows loss of neurons, and the remaining atrophic neurons frequently exhibit grumose degeneration. Degeneration of the red nucleus is typically mild. In general, pallidoluysian degeneration is more marked than that of the dentatorubral systems in the juvenile type, and the reverse situation is observed in the late adult type. Mild degeneration may be seen in the cerebral cortex, especially in patients showing juvenile onset. In the case of infantile onset with 80 CAG repeats, neuronal depletion occurs in multiple brain regions including the cerebral cortex, striatum, inferior olive and cerebellar cortex [56]. Diffuse myelin pallor of the cerebral and cerebellar white matter is often reported in aged patients. Morphometric analysis has revealed a decreased number of glial cells in the affected white matter [92]. Despite the restricted nature of the brain lesions, it is characteristic that the amount of central nervous system (CNS) tissue is significantly reduced throughout the brain and spinal cord. Brain weights of DRPLA patients often become less than 1,000 g [52]. Most of the brain regions lacking obvious neuronal loss show an increase of neuronal density due to atrophy of the neuropil. Thickening of the cranium is often observed in patients with juvenile onset.
NII formation in the DRPLA brain is not restricted to the dentatorubral and pallidoluysian systems, but involves multiple regions including the cerebral cortex, substantia nigra and pontine nuclei. Although the distribution is widespread, the incidence of neurons with inclusions is relatively low, and ranges from ∼1 to 3% even in the dentate nucleus. NIIs in DRPLA are immunohistochemically positive for atrophin-1, expanded polyglutamine stretches (Fig. 2c), ubiquitin and transcription factors [89, 90]. Intranuclear inclusions are also detectable in glial cells [24, 92], as well as in non-neural tissues such as the kidney and pancreas [89]. Immunohistochemistry with 1C2 antibody shows that diffuse accumulation of mutant atrophin-1 in neuronal nuclei (Fig. 2c) is the predominant pathologic condition, rather than NII formation, and involves a wide range of CNS regions including the dentatorubral and pallidoluysian systems [89]. The extent and frequency of neurons showing the diffuse nuclear pathology changes markedly and strikingly depending on the CAG repeat length, suggesting that neuronal dysfunction caused by mutant protein accumulation, rather than neuronal depletion, is responsible for the development of various clinical features in DRPLA. Neuronal nuclei with accumulation of mutant atrophin-1 show deformity with marked nuclear membrane indentations [77]. Immunohistochemistry with 1C2 antibody also reveals the presence of granular staining in the neuronal cytoplasm, with a distribution pattern resembling that of diffuse nuclear staining [93]. In addition to NII formation, filamentous inclusions are also observed exclusively in the cytoplasm of dentate nucleus neurons [87]. The morphology of these structures is indistinguishable from the skein-like inclusions observed in motor neurons in amyotrophic lateral sclerosis; however, they are immunohistochemically positive for atrophin-1, expanded polyglutamine stretches (Fig. 2d) and ubiquitin, but negative for TDP-43, the TAR DNA-binding protein 43. Light and electron microscopic features (Fig. 2e) of NIIs in DRPLA are essentially similar to those of MJD.
To elucidate the molecular mechanisms of neurodegeneration, Schilling et al. [70] generated DRPLA transgenic mice expressing full-length human atrophin-1 with 65 glutamines under transcriptional control of the mouse prion protein promoter, which is expressed at a high level in neurons throughout the brain. These mice exhibited progressive ataxia, tremors, abnormal movements, seizures and premature death. No neuronal loss was detected in the mouse brains, but diffuse nuclear accumulation of mutant atrophin-1 was observed in variable numbers of neurons throughout the brain. Intranuclear inclusions were occasionally detected in some brain regions such as the dentate nucleus, although these were immunohistochemically negative for ubiquitin. Sato et al. generated mouse models of DRPLA harboring a single copy of a full-length human mutant DRPLA gene with 76 or 129 CAG repeats [67, 68, 90]. The hemizygous transgenic offspring with Q129 exhibited progressive neurological manifestations similar to those of patients with juvenile-type DRPLA, such as myoclonus, generalized seizure, ataxia, and premature death. The brains of transgenic mice showed progressive atrophy, but no apparent neuronal loss until death. Diffuse accumulation of mutant protein occurred in neuronal nuclei at postnatal day 4, and thereafter the nuclear pathology expanded to a wide range of CNS regions (Fig. 3a, b), as seen in the human DRPLA brain. Ubiquitinated NII formation was detectable at 9 weeks of age in selected brain regions such as the dentate nucleus and cerebral cortex, and then expanded to multiple brain regions (Fig. 3c, d). The NIIs were spherical, solitary, and composed mainly of fibrous structures, which were straight or curved, ∼9–12 nm in diameter, and organized in random arrays (Fig. 3e). Although no PML protein was detected on or around the NIIs, coiled bodies were present in contact with them. Thus, there are some differences in the ultrastructure of NIIs between humans and model mice. This may be partly due to the amount of time a neuron is exposed to the mutant protein. Neuronal cytoplasmic granular immunostaining with 1C2 antibody was detected in some brain regions such as the brainstem tegmentum and nuclei (Fig. 3b). Intraneuronal inclusions were also found in glial cell in a homozygous mouse [92]. The results obtained in Q129 mice indicate that the appearance of clinical symptoms is not caused by neuronal death, but depends on the diffuse accumulation of mutant proteins in neuronal nuclei. Q76 mice show no obvious phenotypes or NII formation, and have a normal life span; however, intranuclear accumulation of mutant protein is observed in CNS neurons, being milder and slower than that in Q129 mice. These results suggest that a CAG repeat length of 76, which is responsible for juvenile-type DRPLA in humans, is not sufficient for creating the disease condition of DRPLA in mice, and that accumulation of a certain level of mutant protein is needed for the development of polyglutamine pathogenesis.
Polyglutamine-related pathology in neurons of a transgenic mouse model for dentatorubral-pallidoluysian atrophy with 129 CAG repeats. a Neurons in the cerebellar deep nuclei show intense immunolabeling in an intranuclear inclusion (arrow) as well as in the nucleoplasm in a diffuse pattern. b Fine granular immunolabeling (arrowheads) in the cytoplasm of brainstem neurons. c Intense immunolabeling is evident in intranuclear inclusions as well as in the nucleoplasm of cerebral cortical neurons. d Intranuclear inclusions in the cerebral cortical neurons are also positive for ubiquitin. e An intranuclear inclusion (arrow) is non-membrane bound, and composed mainly of filamentous structures, which were straight or curved, ∼9–12 nm in diameter, and organized in random arrays. a–c Immunohistochemistry for expanded polyglutamine stretches with 1C2 antibody; d immunohistochemistry for ubiquitin; e electron micrograph of the nucleus of a cerebral cortical neuron. Scale bars: a–d, 10 μm; e 1 μm
Spinal and bulbar muscular atrophy
SBMA, also known as Kennedy’s disease, is an X-linked, slowly progressive motor neuronopathy caused by an expansion of the CAG repeat in the first exon of the androgen receptor (AR) gene located on chromosome Xq13–21. The number of CAG repeat units in SBMA patients ranges from 40 to 62. This disease affects males, and female carriers are usually asymptomatic. Patients show proximal muscle and bulbar muscle weakness, atrophy and fasciculation, and also frequently present with endocrine abnormalities including gynecomastia and testicular atrophy. SBMA patients can have hand tremor, muscle cramps, and distally accentuated sensory axonopathy in the peripheral nervous system. Postmortem examinations reveal a severely reduced number of motor neurons in the spinal anterior horns, and facial and hypoglossal nuclei [23, 59, 74]. The remaining motor neurons are atrophic. There may be loss of neurons in the dorsal root ganglia [45]. Skeletal muscle biopsies show generally neurogenic changes. Intranuclear inclusions containing the mutant AR with expanded polyglutamine stretches are detected in the remaining motor neurons of the brainstem and spinal cord as well as in the skin, testis and some other visceral organs [46, 47]. Ultrastructurally, these inclusions consist of granular dense aggregates of AR-positive materials without a limiting membrane or filamentous structures [47]. No polyglutamine-related pathology has been reported in glial cells.
A transgenic mouse model expressing 239 expanded pure CAG repeats under the control of a human AR promoter exhibited a small body size, weakness, poor truncal and limb coordination, reduced activity and a short lifespan [2]. NIIs were formed in the cerebrum, cerebellum, brainstem and spinal cord, with a wider distribution pattern than that of human SBMA. Intranuclear inclusions were also observed in glial cells. The ultrastructure of the inclusions was similar to that observed in SBMA patients. There was no evidence of neuronal or muscle degeneration in the model mice. A SBMA mouse model expressing truncated human AR with 112 CAG repeats under control of the neurofilament light chain promoter exhibited motor impairment, accompanied by upper motor deficits [1]. The neuronal expression of mutant proteins in selected brain regions such as the spinal cord anterior horn, brainstem, cerebral cortex and dorsal root ganglia might account for the phenotypic expression and formation of NIIs in the restricted regions. Neither neuronal loss nor neurogenic muscle atrophy was observed in this model. These two mouse models showed no marked phenotypic difference with gender, because the transgenes used did not contain the ligand-binding domain located in the C-terminus of AR. Katsuno et al. [37] generated transgenic mice expressing the full-length human AR containing 97 CAG repeats under control of the cytomegalovirus enhancer and the chicken β-actin promoter. The mice showed a small body size, muscle atrophy, weakness, reduced activity and a short lifespan, all of which were markedly pronounced in the male mice. In the brains of these mice, immunohistochemistry for expanded polyglutamine stretches revealed the presence of diffuse nuclear staining and less frequent NIIs in neurons of the spinal cord, cerebrum, cerebellum, brainstem and dorsal root ganglia as well as non-neuronal tissues such as heart, muscle and pancreas. The expanded distribution of polyglutamine-related pathology in this model may be caused by extensive expression of mutant proteins in the brain. Muscle histology showed significant grouped atrophy and small angulated fibers. Although neuronal cell loss was not evident in any part of the brain and spinal cord, morphologic studies revealed axonal atrophy of the spinal anterior nerve roots as well as shrinkage of the spinal motor neurons. Interestingly, castration of affected male mice significantly improved the symptoms, pathologic findings, and nuclear localization of mutant proteins. To develop a truly representative model of SBMA, Sopher et al. [75] generated a YAC transgenic mouse model expressing the human AR gene with 100 CAG repeats. The mice showed a late disease onset, gradually progressive neuromuscular phenotype and early mortality, dying at 15–24 months of age. Histopathology at 16 months revealed a reduced number of motor neurons in the lumbar spinal cord, and denervation atrophy of the quadriceps muscle. Although mutant AR proteins with expanded polyglutamine stretches accumulate diffusely in the nuclei of affected spinal cord and brainstem neurons in SBMA patients, no NIIs were detected in these regions in the transgenic mice at 14 months of age. In contrast, punctate nuclear aggregates of mutant proteins were observed in the dorsal lateral hypothalamus and tectum. Interestingly, punctate staining was also demonstrated in spinal cord astrocytes. Although the mice showed pathological changes in the spinal cord and skeletal muscles that resembled to those in human SBMA patients, the lack of nuclear inclusions in motor neurons or their presence in glial cells may be a fundamental problem in this disease model.
Spinocerebellar ataxia type 8
SCA8 is a hereditary neurodegenerative disorder caused by expansion of a CTG repeat in the 3′ untranslated region of a gene localized to chromosome 13q21 [40]. Affected individuals show progressive gait and limb ataxia, dysarthria and nystagmus, with variable ages at onset [11, 30]. Neuropathologic studies have revealed relatively pure atrophy of the cerebellum [35]. Histologically, severe loss of Purkinje cells is the most prominent finding. The remaining Purkinje cells are atrophic and occasionally show somatic sprouts. Neuronal loss is also detectable in the inferior olive and substantia nigra. Although SCA8 is not a CAG repeat disease, it is interesting that 1C2-positive intranuclear inclusions and pan-nuclear staining are found in Purkinje, medullary and dentate neurons from human SCA8 brains [51]. These inclusions are also positive for ubiquitin. 1C2-positive granular structures are detected in the cytoplasm of Purkinje cells [35]. Glial cell involvement is not seen.
Moseley et al. [51] generated a transgenic mouse model in which the full-length human SCA8 mutation was transcribed using its endogenous promoter. The (CTG)116 expansion lines exhibited motor deficits, generalized wasting and premature death. Although histological analysis of the brain did not show any obvious neurodegenerative changes, 1C2- and ubiquitin-positive intranuclear inclusions were found in a subset of Purkinje cells and pontine neurons. The pathologic findings in brains of human SCA8 and the transgenic mice suggest that, in SCA8, there is translation of a polyglutamine protein, encoded on a previously unidentified antiparallel transcript spanning the repeat in the CAG direction. The expression of noncoding (CUG) n expansion transcripts and the presence of intranuclear polyglutamine inclusions suggests that SCA8 pathogenesis involves toxic gain-of-function mechanisms at both the protein and RNA levels.
Conclusion
It is now evident that the brains of humans with CAG repeat diseases share several polyglutamine-related changes in their neuronal nuclei and cytoplasm, in addition to the conventional pathology characterized by neuronal depletion. Although NIIs are the pathologic hallmark common to these disorders, they are frequently present beyond the regions of distribution of neuronal loss. These features suggest that neurons are affected by polyglutamine pathogenesis much more widely than has been recognized previously. The diffuse nuclear immunostaining with 1C2 antibody indicates that mutant proteins also accumulate diffusely throughout the nucleoplasm of neurons. As suggested by the data obtained from studies of DRPLA, it is likely that this pathologic change is more closely related to the development of clinical phenotypes in DRPLA than NII formation. In MJD, however, NII formation is a predominant form of pathologic change, and seems to be critical for phenotypic expression. Thus, the significance of these two nuclear changes may differ in the disease process of each CAG repeat disorder. The presence of neuronal cytoplasmic granular labeling for expanded polyglutamine in brains of patients with several CAG repeat diseases suggests that, in addition to the ubiquitin/proteasome pathways, the endosomal/lysosomal pathway may be a relatively common route for degradation of proteins with the mutation. This processing mechanism may serve as a target for new forms of therapy for these disorders.
The mouse models described above indicate that the CAG repeat lengths, which are responsible for polyglutamine diseases in humans, are not sufficient for creating equivalent disease conditions in mice. The short lifespan of mice, or possibly high levels of metabolic activity directed against the mutant proteins, may partly explain the results obtained. The models also support the notion that, although expanded polyglutamine tracts themselves are toxic, residues outside the tract in each causative gene product have important roles in defining the disease process and lesion distribution. Various mouse models have been generated using methods such as the induction of highly expanded polyglutamine tracts, an increase of transgene copy number, and the use of specific promoters. However, there is no model that fully represents the neuropathologic changes observed in humans. Most of these mouse models have been partly successful in generation of polyglutamine-related changes such as NII formation and diffuse nuclear labeling, but there are still some differences in lesion distribution or affected cell types in comparison with human pathology. It has also been generally difficult to induce neuronal loss in these models. In order to mimic selective neuronal degeneration of CAG repeat diseases in mice, it may be necessary to express a much higher level of mutant protein with a proper spatio-temporal pattern in the brain. Although the currently available murine models of CAG repeat diseases do not completely represent the neuropathology seen in humans, they have provided many insights into the disease processes underlying polyglutamine pathogenesis. The most fundamental and commonly accepted knowledge provided by these models is that clinical onset is not clearly associated with neuronal cell death, but depends on intranuclear accumulation of mutant proteins in neurons. This is in good harmony with the disease process of CAG repeat disorders that has been suggested from neuropathologic studies of human brains. The models have also shown the age-dependent intranuclear accumulation of mutant proteins, and the necessity of a certain level of protein accumulation for the development of polyglutamine pathogenesis. Recent studies have provided evidences that affected neurons suffer from functional dysregulation including transcriptional abnormalities [17, 44, 49, 64, 72, 82]. In HD, it is suggested that intracellular vesicle trafficking is impaired, and lack of proper uptake of neurotrophic factors may be an important pathological trigger leading to striatal cell death [13, 18, 81, 82]. These pathomechanisms may account for the general late-onset clinical phenotypes in patients with CAG repeat diseases. Because NIIs contain ubiquitin and proteasome subunits, it has been proposed that an impairment of the ubiquitin–proteasome system (UPS) might underlie the pathogenesis of polyglutamine disorders. However, since the initial discovery, the UPS impairment hypothesis has remained controversial. While studies on cell models and on postmortem tissue support this working hypothesis, in vitro studies in mouse models fail to do so [84]. Although it is important to determine whether proteasome inhibition may be elicited by direct interaction with ubiquitylated forms of aggregated or monomeric mutant proteins [84], much therapeutic effort will be directed at enhancement of cellular protective measures that include the use of chaperones as a strategy in preventing many versions of polyglutamine diseases [25, 58, 60].
References
Abel A, Walcott J, Woods J, Duda J, Merry DE (2001) Expression of expanded repeat androgen receptor produces neurologic disease in transgenic mice. Hum Mol Genet 10:107–116
Adachi H, Kume A, Li M, Nakagomi Y, Niwa H, Do J, Sang C, Kobayashi Y, Doyu M, Sobue G (2001) Transgenic mice with an expanded CAG repeat controlled by the human AR promoter show polyglutamine nuclear inclusions and neuronal dysfunction without neuronal cell death. Hum Mol Genet 10:1039–1048
Aguiar J, Fernández J, Aguilar A, Mendoza Y, Vázquez M, Suárez J, Berlanga J, Cruz S, Guillén G, Herrera L, Velázquez L, Santos N, Merino N (2006) Ubiquitous expression of human SCA2 gene under the regulation of the SCA2 self promoter cause specific Purkinje cell degeneration in transgenic mice. Neurosci Lett 392:202–206
Bichelmeier U, Schmidt T, Hübener J, Boy J, Rüttiger L, Häbig K, Poths S, Bonin M, Knipper M, Schmidt WJ, Wilbertz J, Wolburg H, Laccone F, Riess O (2007) Nuclear localization of ataxin-3 is required for the manifestation of symptoms in SCA3: in vivo evidence. J Neurosci 27:7418–7428
Burright EN, Clark HB, Servadio A, Matilla T, Feddersen RM, Yunis WS, Duvick LA, Zoghbi HY, Orr HT (1995) SCA1 transgenic mice: a model for neurodegeneration caused by an expanded CAG trinucleotide repeat. Cell 82:937–948
Carpenter S, Schumacher GA (1966) Familial infantile cerebellar atrophy associated with retinal degeneration. Arch Neurol 14:82–94
Cemal CK, Carroll CJ, Lawrence L, Lowrie MB, Ruddle P, Al-Mahdawi S, King RHM, Pook MA, Huxley C, Chamberlain S (2002) YAC transgenic mice carrying pathological alleles of the MJD1 locus exhibit a mild and slowly progressive cerebellar deficit. Hum Mol Genet 11:1075–1094
Clark HB, Burright EN, Yunis WS, Larson S, Wilcox C, Hartman B, Matilla A, Zoghbi HY, Orr HT (1997) Purkinje cell expression of a mutant allele of SCA1 in transgenic mice leads to disparate effects on motor behaviors, followed by a progressive cerebellar dysfunction and histological alterations. J Neurosci 17:7385–7395
Cummings CJ, Reinstein E, Sun Y, Antalffy B, Jiang Y, Ciechanover A, Orr HT, Beaudet AL, Zoghbi HY (1999) Mutation of the E6-AP ubiquitin ligase reduces nuclear inclusion frequency while accelerating polyglutamine-induced pathology in SCA1 mice. Neuron 24:879–892
Davies SW, Turmaine M, Cozens BA, DiFiglia M, Sharp AH, Ross CA, Scherzinger E, Wanker EE, Mangiarini L, Bates GP (1997) Formation of neuronal intranuclear inclusions underlies the neurological dysfunction in mice transgenic for the HD mutation. Cell 90:537–548
Day JW, Schut LJ, Moseley ML, Durand AC, Ranum LP (2000) Spinocerebellar ataxia type 8: clinical features in a large family. Neurology 55:649–657
de Jong PT, de Jong JG, de Jong-Ten Doeschate JM, Delleman JW (1980) Olivopontocerebellar atrophy with visual disturbances. An ophthalmologic investigation into four generations. Ophthalmology 87:793–804
del Toro D, Canals JM, Gines S, Kojima M, Egea G, Alberch J (2006) Mutant huntingtin impairs the post-Golgi trafficking of brain-derived neurotrophic factor but not its Val66Met polymorphism. J Neurosci 26:12748–12757
Dürr A, Smadja D, Cancel G, Lezin A, Stevanin G, Mikol J, Bellance R, Buisson GG, Chneiweiss H, Dellanave J, Agid Y, Brice A, Vernant JC (1995) Autosomal dominant cerebellar ataxia type I in Martinique (French West Indies). Clinical and neuropathological analysis of 53 patients from three unrelated SCA2 families. Brain 118 (Pt 6):1573–1581
Duyckaerts C, Dürr A, Cancel G, Brice A (1999) Nuclear inclusions in spinocerebellar ataxia type 1. Acta Neuropathol 97:201–207
Enevoldson TP, Sanders MD, Harding AE (1994) Autosomal dominant cerebellar ataxia with pigmentary macular dystrophy. A clinical and genetic study of eight families. Brain 117:445–460
Everett CM, Wood NW (2004) Trinucleotide repeats and neurodegenerative disease. Brain 127:2385–2405
Fan MM, Fernandes HB, Zhang LY, Hayden MR, Raymond LA (2007) Altered NMDA receptor trafficking in a yeast artificial chromosome transgenic mouse model of Huntington’s disease. J Neurosci 27:3768–3779
Garden GA, Libby RT, Fu YH, Kinoshita Y, Huang J, Possin DE, Smith AC, Martinez RA, Fine GC, Grote SK, Ware CB, Einum DD, Morrison RS, Ptacek LJ, Sopher BL, La Spada AR (2002) Polyglutamine-expanded ataxin-7 promotes non-cell-autonomous purkinje cell degeneration and displays proteolytic cleavage in ataxic transgenic mice. J Neurosci 22:4897–4905
Goti D, Katzen SM, Mez J, Kurtis N, Kiluk J, Ben-Haïm L, Jenkins NA, Copeland NG, Kakizuka A, Sharp AH, Ross CA, Mouton PR, Colomer V (2004) A mutant ataxin-3 putative-cleavage fragment in brains of Machado-Joseph disease patients and transgenic mice is cytotoxic above a critical concentration. J Neurosci 24:10266–10279
Gouw LG, Digre KB, Harris CP, Haines JH, Ptacek LJ (1994) Autosomal dominant cerebellar ataxia with retinal degeneration: clinical, neuropathologic, and genetic analysis of a large kindred. Neurology 44:1441–1447
Gouw LG, Kaplan CD, Haines JH, Digre KB, Rutledge SL, Matilla A, Leppert M, Zoghbi HY, Ptacek LJ (1995) Retinal degeneration characterizes a spinocerebellar ataxia mapping to chromosome 3p. Nat Genet 10:89–93
Harding AE, Thomas PK, Baraitser M, Bradbury PG, Morgan-Hughes JA, Ponsford JR (1982) X-linked recessive bulbospinal neuronopathy: a report of ten cases. J Neurol Neurosurg Psychiatry 45:1012–1019
Hayashi Y, Kakita A, Yamada M, Koide R, Igarashi S, Takano H, Ikeuchi T, Wakabayashi K, Egawa S, Tsuji S, Takahashi H (1998) Hereditary dentatorubral-pallidoluysian atrophy: detection of widespread ubiquitinated neuronal and glial intranuclear inclusions in the brain. Acta Neuropathol 96:547–552
Herbst M, Wanker EE (2006) Therapeutic approaches to polyglutamine diseases: combating protein misfolding and aggregation. Curr Pharm Des 12:2543–2555
Holmberg M, Johansson J, Forsgren L, Heijbel J, Sandgren O, Holmgren G (1995) Localization of autosomal dominant cerebellar ataxia associated with retinal degeneration and anticipation to chromosome 3p12-p21.1. Hum Mol Genet 4:1441–1445
Holmberg M, Duyckaerts C, Dürr A, Cancel G, Gourfinkel-An I, Damier P, Faucheux B, Trottier Y, Hirsch EC, Agid Y, Brice A (1998) Spinocerebellar ataxia type 7 (SCA7): a neurodegenerative disorder with neuronal intranuclear inclusions. Hum Mol Genet 7:913–918
Huynh DP, Del Bigio MR, Ho DH, Pulst SM (1999) Expression of ataxin-2 in brains from normal individuals and patients with Alzheimer’s disease and spinocerebellar ataxia 2. Ann Neurol 45:232–241
Huynh DP, Figueroa K, Hoang N, Pulst SM (2000) Nuclear localization or inclusion body formation of ataxin-2 are not necessary for SCA2 pathogenesis in mouse or human. Nat Genet 26:44–50
Ikeda Y, Shizuka M, Watanabe M, Okamoto K, Shoji M (2000) Molecular and clinical analyses of spinocerebellar ataxia type 8 in Japan. Neurology 54:950–955
Ikeda H, Yamaguchi M, Sugai S, Aze Y, Narumiya S, Kakizuka A (1996) Expanded polyglutamine in the Machado-Joseph disease protein induces cell death in vitro and in vivo. Nat Genet 13:196–202
Ikeuchi T, Takano H, Koide R, Horikawa Y, Honma Y, Onishi Y, Igarashi S, Tanaka H, Nakao N, Sahashi K, Tsukagoshi H, Inoue K, Takahashi H, Tsuji S (1997) Spinocerebellar ataxia type 6: CAG repeat expansion in alpha1A voltage-dependent calcium channel gene and clinical variations in Japanese population. Ann Neurol 42:879–884
Imbert G, Saudou F, Yvert G, Devys D, Trottier Y, Garnier JM, Weber C, Mandel JL, Cancel G, Abbas N, Dürr A, Didierjean O, Stevanin G, Agid Y, Brice A (1996) Cloning of the gene for spinocerebellar ataxia 2 reveals a locus with high sensitivity to expanded CAG/glutamine repeats. Nat Genet 14:285–291
Ishikawa K, Owada K, Ishida K, Fujigasaki H, Shun Li M, Tsunemi T, Ohkoshi N, Toru S, Mizutani T, Hayashi M, Arai N, Hasegawa K, Kawanami T, Kato T, Makifuchi T, Shoji S, Tanabe T, Mizusawa H (2001) Cytoplasmic and nuclear polyglutamine aggregates in SCA6 Purkinje cells. Neurology 56:1753–1756
Ito H, Kawakami H, Wate R, Matsumoto S, Imai T, Hirano A, Kusaka H (2006) Clinicopathologic investigation of a family with expanded SCA8 CTA/CTG repeats. Neurology 67:1479–1481
Iwabuchi K, Tsuchiya K, Uchihara T, Yagishita S (1999) Autosomal dominant spinocerebellar degenerations. Rev Neurol (Paris) 155:255–270
Katsuno M, Adachi H, Kume A, Li M, Nakagomi Y, Niwa H, Sang C, Kobayashi Y, Doyu M, Sobue G (2002) Testosterone reduction prevents phenotypic expression in a transgenic mouse model of spinal and bulbar muscular atrophy. Neuron 35:843–854
Klement IA, Skinner PJ, Kaytor MD, Yi H, Hersch SM, Clark HB, Zoghbi HY, Orr HT (1998) Ataxin-1 nuclear localization and aggregation: role in polyglutamine-induced disease in SCA1 transgenic mice. Cell 95:41–53
Koide R, Kobayashi S, Shimohata T, Ikeuchi T, Maruyama M, Saito M, Yamada M, Takahashi H, Tsuji S (1999) A neurological disease caused by an expanded CAG trinucleotide repeat in the TATA-binding protein gene: a new polyglutamine disease? Hum Mol Genet 8:2047–2053
Koob MD, Moseley ML, Schut LJ, Benzow KA, Bird TD, Day JW, Ranum LP (1999) An untranslated CTG expansion causes a novel form of spinocerebellar ataxia (SCA8). Nat Genet 21:379–384
Koyano S, Uchihara T, Fujigasaki H, Nakamura A, Yagishita S, Iwabuchi K (1999) Neuronal intranuclear inclusions in spinocerebellar ataxia type 2: triple-labeling immunofluorescent study. Neurosci Lett 273:117–120
Koyano S, Iwabuchi K, Yagishita S, Kuroiwa Y, Uchihara T (2002) Paradoxical absence of nuclear inclusion in cerebellar Purkinje cells of hereditary ataxias linked to CAG expansion. J Neurol Neurosurg Psychiatry 73:450–452
La Spada AR, Fu YH, Sopher BL, Libby RT, Wang X, Li LY, Einum DD, Huang J, Possin DE, Smith AC, Martinez RA, Koszdin KL, Treuting PM, Ware CB, Hurley JB, Ptacek LJ, Chen S (2001) Polyglutamine-expanded ataxin-7 antagonizes CRX function and induces cone-rod dystrophy in a mouse model of SCA7. Neuron 31:913–927
Lam YC, Bowman AB, Jafar-Nejad P, Lim J, Richman R, Fryer JD, Hyun ED, Duvick LA, Orr HT, Botas J, Zoghbi HY (2006) ATAXIN-1 interacts with the repressor Capicua in its native complex to cause SCA1 neuropathology. Cell 127:1335–1347
Li M, Sobue G, Doyu M, Mukai E, Hashizume Y, Mitsuma T (1995) Primary sensory neurons in X-linked recessive bulbospinal neuropathy: histopathology and androgen receptor gene expression. Muscle Nerve 18:301–308
Li M, Miwa S, Kobayashi Y, Merry DE, Yamamoto M, Tanaka F, Doyu M, Hashizume Y, Fischbeck KH, Sobue G (1998) Nuclear inclusions of the androgen receptor protein in spinal and bulbar muscular atrophy. Ann Neurol 44:249–254
Li M, Nakagomi Y, Kobayashi Y, Merry DE, Tanaka F, Doyu M, Mitsuma T, Hashizume Y, Fischbeck KH, Sobue G (1998) Nonneural nuclear inclusions of androgen receptor protein in spinal and bulbar muscular atrophy. Am J Pathol 153:695–701
Lorenzetti D, Watase K, Xu B, Matzuk MM, Orr HT, Zoghbi HY (2000) Repeat instability and motor incoordination in mice with a targeted expanded CAG repeat in the Sca1 locus. Hum Mol Genet 9:779–785
Luthi-Carter R, Strand AD, Hanson SA, Kooperberg C, Schilling G, La Spada AR, Merry DE, Young AB, Ross CA, Borchelt DR, Olson JM (2002) Polyglutamine and transcription: gene expression changes shared by DRPLA and Huntington’s disease mouse models reveal context-independent effects. Hum Mol Genet 11:1927–1937
Martin JJ, Van Regemorter N, Krols L, Brucher JM, de Barsy T, Szliwowski H, Evrard P, Ceuterick C, Tassignon MJ, Smet-Dieleman H, Hayez-Delatte F, Willems PJ, Van Broeckhoven C (1994) On an autosomal dominant form of retinal-cerebellar degeneration: an autopsy study of five patients in one family. Acta Neuropathol (Berl) 88:277–286
Moseley ML, Zu T, Ikeda Y, Gao W, Mosemiller AK, Daughters RS, Chen G, Weatherspoon MR, Clark HB, Ebner TJ, Day JW, Ranum LP (2006) Bidirectional expression of CUG and CAG expansion transcripts and intranuclear polyglutamine inclusions in spinocerebellar ataxia type 8. Nat Genet 38:758–769
Naito H, Oyanagi S (1982) Familial myoclonus epilepsy and choreoathetosis: hereditary dentatorubral-pallidoluysian atrophy. Neurology 32:798–807
Naito H (1990) The clinical picture and classification of dentatorubral-pallidoluysian atrophy (DRPLA). Shinkeinaika 32:450–456 (in Japanese)
Nakamura K, Jeong SY, Uchihara T, Anno M, Nagashima K, Nagashima T, Ikeda S, Tsuji S, Kanazawa I (2001) SCA17, a novel autosomal dominant cerebellar ataxia caused by an expanded polyglutamine in TATA-binding protein. Hum Mol Genet 10:1441–1448
Neetens A, Martin JJ, Libert J, Van den Ende P (1990) Autosomal dominant cone dystrophy-cerebellar atrophy (ADCoCA) (modified ADCA Harding II). Neuroophthalmology 10:261–275
Ohama E, Shimoda Y, Shimomura T, Katou S, Kimura M (1995) Dentatorubral-pallidoluysian atrophy: a neuropathological study of father and son in a family. Neuropathology 15(suppl):147 (in Japanese)
Orozco G, Estrada R, Perry TL, Araña J, Fernandez R, Gonzalez-Quevedo A, Galarraga J, Hansen S (1989) Dominantly inherited olivopontocerebellar atrophy from eastern Cuba. Clinical, neuropathological, and biochemical findings. J Neurol Sci 93:37–50
Orr HT (2001) Beyond the Qs in the polyglutamine diseases. Gene Dev 15:925–932
Oyanagi K, Aoki K, Morita T, Igarashi S, Inuzuka T, Horikawa Y (1996) Disaggregation of polyribosomes in the spinal anterior horn cells in a patient with X-linked spinal and bulbar muscular atrophy. Acta Neuropathol 91:444–447
Paul S (2007) Polyglutamine-mediated neurodegeneration: use of chaperones as prevention strategy. Biochemistry (Mosc) 72:359–366
Paulson HL, Perez MK, Trottier Y, Trojanowski JQ, Subramony SH, Das SS, Vig P, Mandel JL, Fischbeck KH, Pittman RN (1997) Intranuclear inclusions of expanded polyglutamine protein in spinocerebellar ataxia type 3. Neuron 19:333–344
Pulst SM, Nechiporuk A, Nechiporuk T, Gispert S, Chen XN, Lopes-Cendes I, Pearlman S, Starkman S, Orozco-Diaz G, Lunkes A, DeJong P, Rouleau GA, Auburger G, Korenberg JR, Figueroa C, Sahba S (1996) Moderate expansion of a normally biallelic trinucleotide repeat in spinocerebellar ataxia type 2. Nat Genet 14:269–276
Rosenberg RN (1992) Machado-Joseph disease: an autosomal dominant motor system degeneration. Mov Disord 7:193–203
Ross CA (2002) Polyglutamine pathogenesis: emergence of unifying mechanisms for Huntington’s disease and related disorders. Neuron 35:819–822
Ryan SJ Jr, Knox DL, Green WR, Konigsmark BW (1975) Olivopontocerebellar degeneration. Clinicopathologic correlation of the associated retinopathy. Arch Ophthalmol 93:169–172
Sanpei K, Takano H, Igarashi S, Sato T, Oyake M, Sasaki H, Wakisaka A, Tashiro K, Ishida Y, Ikeuchi T, Koide R, Saito M, Sato A, Tanaka T, Hanyu S, Takiyama Y, Nishizawa M, Shimizu N, Nomura Y, Segawa M, Iwabuchi K, Eguchi I, Tanaka H, Takahashi H, Tsuji S (1996) Identification of the spinocerebellar ataxia type 2 gene using a direct identification of repeat expansion and cloning technique, DIRECT. Nat Genet 14:277–284
Sato T, Oyake M, Nakamura K, Nakao K, Fukusima Y, Onodera O, Igarashi S, Takano H, Kikugawa K, Ishida Y, Shimohata T, Koide R, Ikeuchi T, Tanaka H, Futamura N, Matsumura R, Takayanagi T, Tanaka F, Sobue G, Komure O, Takahashi M, Sano A, Ichikawa Y, Goto J, Kanazawa I, Katsuki M, Tsuji S (1999) Transgenic mice harboring a full-length human mutant DRPLA gene exhibit age-dependent intergenerational and somatic instabilities of CAG repeats comparable with those in DRPLA patients. Hum Mol Genet 8:99–106
Sato T, Yamada M, Oyake M, Nakao K, Nakamura K, Katsuki M, Takahashi H, Tsuji S (1999) Transgenic mice harboring a full-length human DRPLA gene with highly expanded CAG repeats exhibit severe disease phenotype. Am J Hum Genet 65(suppl):A30
Saudou F, Finkbeiner S, Devys D, Greenberg ME (1998) Huntingtin acts in the nucleus to induce apoptosis but death does not correlate with the formation of intranuclear inclusions. Cell 95:55–66
Schilling G, Wood JD, Duan K, Slunt HH, Gonzales V, Yamada M, Cooper JK, Margolis RL, Jenkins NA, Copeland NG, Takahashi H, Tsuji S, Price DL, Borchelt DR, Ross CA (1999) Nuclear accumulation of truncated atrophin-1 fragments in a transgenic mouse model of DRPLA. Neuron 24:275–286
Schmidt T, Landwehrmeyer GB, Schmitt I, Trottier Y, Auburger G, Laccone F, Klockgether T, Völpel M, Epplen JT, Schöl L, Riess O (1998) An isoform of ataxin-3 accumulates in the nucleus of neuronal cells in affected brain regions of SCA3 patients. Brain Pathol 8:669–679
Shimohata T, Nakajima T, Yamada M, Uchida C, Onodera O, Naruse S, Kimura T, Koide R, Nozaki K, Sano Y, Ishiguro H, Sakoe K, Ooshima T, Sato A, Ikeuchi T, Oyake M, Sato T, Aoyagi Y, Hozumi I, Nagatsu T, Takiyama Y, Nishizawa M, Goto J, Kanazawa I, Davidson I, Tanese N, Takahashi H, Tsuji S (2000) Expanded polyglutamine stretches interact with TAFII130, interfering with CREB-dependent transcription. Nat Genet 26:29–36
Skinner PJ, Koshy BT, Cummings CJ, Klement IA, Helin K, Servadio A, Zoghbi HY, Orr HT (1997) Ataxin-1 with an expanded glutamine tract alters nuclear matrix-associated structures. Nature 389:971–974
Sobue G, Hashizume Y, Mukai E, Hirayama M, Mitsuma T, Takahashi A (1989) X-linked recessive bulbospinal neuronopathy. A clinicopathological study. Brain 112:209–232
Sopher BL, Thomas PS Jr, LaFevre-Bernt MA, Holm IE, Wilke SA, Ware CB, Jin LW, Libby RT, Ellerby LM, La Spada AR (2004) Androgen receptor YAC transgenic mice recapitulate SBMA motor neuronopathy and implicate VEGF164 in the motor neuron degeneration. Neuron 41:687–699
Sudarsky L, Coutinho P (1995) Machado-Joseph disease. Clin Neurosci 3:17–22
Takahashi H, Egawa S, Piao YS, Hayashi S, Yamada M, Shimohata T, Oyanagi K, Tsuji S (2001) Neuronal nuclear alterations in dentatorubral-pallidoluysian atrophy: ultrastructural and morphometric studies of the cerebellar granule cells. Brain Res 919:12–9
Toyoshima Y, Yamada M, Onodera O, Shimohata M, Inenaga C, Fujita N, Morita M, Tsuji S, Takahashi H (2004) SCA17 homozygote showing Huntington’s disease-like phenotype. Ann Neurol 55:281–286
Traboulsi EI, Maumenee IH, Green WR, Freimer ML, Moser H (1988) Olivopontocerebellar atrophy with retinal degeneration. A clinical and ocular histopathologic study. Arch Ophthalmol 106:801–806
Trottier Y, Lutz Y, Stevanin G, Imbert G, Devys D, Cancel G, Saudou F, Weber C, David G, Tora L, Agid Y, Brice A, Mandel JL (1995) Polyglutamine expansion as a pathological epitope in Huntington’s disease and four dominant cerebellar ataxias. Nature 378:403–406
Truant R, Atwal R, Burtnik A (2006) Hypothesis: Huntingtin may function in membrane association and vesicular trafficking. Biochem Cell Biol 84:912–917
Truant R, Atwal RS, Burtnik A (2007) Nucleocytoplasmic trafficking and transcription effects of huntingtin in Huntington’s disease. Prog Neurobiol [Epub ahead of print]
Uchihara T, Takeda Y, Kobayashi T, Kasuga T, Ishikawa K, Kirei K, Mizusawa H, Endo T, Hirokawa K, Kuroiwa T (2006) Unexpected clinicopathological phenotype linked to small elongation of CAG repeat in SCA1 gene. J Neurol 253:396–398
Valera AG, Diáz-Hernández M, Hernández F, Lucas JJ (2007) Testing the possible inhibition of proteasome by direct interaction with ubiquitylated and aggregated huntingtin. Brain Res Bull 72:121–123
van de Warrenburg BP, Frenken CW, Ausems MG, Kleefstra T, Sinke RJ, Knoers NV, Kremer HP (2001) Striking anticipation in spinocerebellar ataxia type 7: the infantile phenotype. J Neurol 248:911–914
Watase K, Weeber EJ, Xu B, Antalffy B, Yuva-Paylor L, Hashimoto K, Kano M, Atkinson R, Sun Y, Armstrong DL, Sweatt JD, Orr HT, Paylor R, Zoghbi HY (2002) A long CAG repeat in the mouse Sca1 locus replicates SCA1 features and reveals the impact of protein solubility on selective neurodegeneration. Neuron 34:905–919
Yamada M, Piao YS, Toyoshima Y, Tsuji S, Takahashi H (2000) Ubiquitinated filamentous inclusions in cerebellar dentate nucleus neurons in dentatorubral-pallidoluysian atrophy contain expanded polyglutamine stretches. Acta Neuropathol (Berl) 99:615–618
Yamada M, Hayashi S, Tsuji S, Takahashi H (2001) Involvement of the cerebral cortex and autonomic ganglia in Machado-Joseph disease. Acta Neuropathol (Berl) 101:140–144
Yamada M, Wood JD, Shimohata T, Hayashi S, Tsuji S, Ross CA, Takahashi H (2001) Widespread occurrence of intranuclear atrophin-1 accumulation in the central nervous system neurons of patients with dentatorubral-pallidoluysian atrophy. Ann Neurol 49:14–23
Yamada M, Sato T, Shimohata T, Hayashi S, Igarashi S, Tsuji S, Takahashi H (2001) Interaction between neuronal intranuclear inclusions and promyelocytic leukemia protein nuclear and coiled bodies in CAG repeat diseases. Am J Pathol 159:1785–1795
Yamada M, Tsuji S, Takahashi H (2002) Involvement of lysosomes in the pathogenesis of CAG repeat diseases. Ann Neurol 52:498–503
Yamada M, Sato T, Tsuji S, Takahashi H (2002) Oligodendrocytic polyglutamine pathology in dentatorubral-pallidoluysian atrophy. Ann Neurol 52:670–674
Yamada M, Tan CF, Inenaga C, Tsuji S, Takahashi H (2004) Sharing of polyglutamine localization by the neuronal nucleus and cytoplasm in CAG-repeat diseases. Neuropathol Appl Neurobiol 30:665–675
Yoo SY, Pennesi ME, Weeber EJ, Xu B, Atkinson R, Chen S, Armstrong DL, Wu SM, Sweatt JD, Zoghbi HY (2003) SCA7 knockin mice model human SCA7 and reveal gradual accumulation of mutant ataxin-7 in neurons and abnormalities in short-term plasticity. Neuron 37:383–401
Yvert G, Lindenberg KS, Picaud S, Landwehrmeyer GB, Sahel JA, Mandel JL (2000) Expanded polyglutamines induce neurodegeneration and trans-neuronal alterations in cerebellum and retina of SCA7 transgenic mice. Hum Mol Genet 9:2491–2506
Zhuchenko O, Bailey J, Bonnen P, Ashizawa T, Stockton DW, Amos C, Dobyns WB, Subramony SH, Zoghbi HY, Lee CC (1997) Autosomal dominant cerebellar ataxia (SCA6) associated with small polyglutamine expansions in the alpha 1A-voltage-dependent calcium channel. Nat Genet 15:62–69
Zoghbi HY, Orr HT (1995) Spinocerebellar ataxia type 1. Semin Cell Biol 6:29–35
Zoghbi HY, Orr HT (2000) Glutamine repeats and neurodegeneration. Ann Rev Neurosci 23:217–247
Acknowledgments
We thank S. Egawa, Y. Ohta, C. Tanada, J. Takasaki, N. Kaneko, T. Tanabe and Y. Itou for their technical assistance, and M. Machida and Y. Ueda for their secretarial assistance. This research was supported by a grant from the Research Committee for Ataxic Diseases, the Ministry of Health, Labor and Welfare, Japan, a Grant-in-Aid for Scientific Research (17300109), and a Grant-in-Aid for Scientific Research on Priority Areas-Advanced Brain Project (15016044) from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamada, M., Sato, T., Tsuji, S. et al. CAG repeat disorder models and human neuropathology: similarities and differences. Acta Neuropathol 115, 71–86 (2008). https://doi.org/10.1007/s00401-007-0287-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-007-0287-5