Abstract
Remote ischemic conditioning (RIC) is acutely cardioprotective in ischemia–reperfusion injury. We aimed to evaluate the effect of RIC on septic cardiomyopathy and associated multi-organ failure in a lipopolysaccharide (LPS)-induced sepsis mouse model. Balb/c mice were divided into sham, LPS, and LPS + RIC groups. LPS 10 mg/kg or saline control was injected intraperitoneally. RIC was performed by four cycles of 5 min ischemia and 5 min reperfusion of the left lower limb just before the LPS injection. Cardiac function on echocardiography, circulating mediators, blood biochemistry, and MAPK signalling was assessed. Survival 7 days after LPS injection was evaluated in sham-treated, RIC, and daily repeated RIC groups. An LPS-induced decrease in cardiac output was ameliorated by RIC with preserved left ventricular systolic function. LPS-induced increases in TNF-α, IL-1β, IL-6, and high-mobility group box 1 protein (HMGB1) were significantly suppressed by RIC. RIC also suppressed increases in plasma cardiac troponin I, aspartate transaminase, alanine transaminase, blood urea nitrogen, and creatinine with suppressed ERK and JNK phosphorylation in heart, liver, and kidney tissue. RIC significantly improved survival rate (p = 0.0037). Survival rate in the daily repeated RIC group was 100%, and it was higher than that in the RIC group (p = 0.0088). In summary, RIC reduced circulating and myocardial inflammatory mediators associated with septic cardiomyopathy, and led to improved ventricular function, cardiac output, and survival. Our data also revealed that chronic RIC has additional benefit in terms of mortality in sepsis. While further studies are required, RIC may be a clinically useful tool to ameliorate sepsis-induced cardiomyopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Remote ischemic conditioning (RIC) is a highly cardioprotective phenomenon induced by repeated transient ischemia of a remote organ or tissue. The use of the technique has been widely reported since its conceptual description by Przyklenk et al in 1993 [26]. While early rodent studies showed that RIC can be induced by transient of, e.g., the kidney or mesentery, Kharbanda et al. first reported that transient limb ischemia can reduce myocardial infarction size by 50% [14].
RIC has been shown to be effective in multiple preclinical, and proof-of-principle clinical trials [3, 31], and is subsequently undergoing phase-3 clinical trials in patients undergoing emergency percutaneous coronary intervention for myocardial infarction [20]. The effects of RIC are now known to go beyond immediate cardioprotection via modification of acute ischemia–reperfusion injury. For example, Wei et al. subsequently showed that daily RIC delivered for 28 days provided additional benefit by reducing myocardial inflammatory responses and mitigating adverse ventricular remodeling in a myocardial infarction model [34].
The underlying mechanisms of RIC have been extensively investigated, and reviewed [4, 9, 18, 30], and result from a complex neuro-humoral response to the initial episodes of transient remote ischemia. In addition to cycles of ischemia reperfusion, electrical stimulation, chemical stimulation, and mechanical trauma can all trigger RIC [16]. The role of neural pathways in cardioprotection has recently been reviewed extensively [7]. The involvement of vagus nerve in RIC is particularly important [8, 19], and it has been reported that visceral organs innervated by the vagus nerve are a source of humoral factor(s) such as glucagon-like peptide-1 (GLP-1) that have cardioprotectant activity [1]. The release of cardioprotective factor(s) can also occur through vago-splenic axis in RIC [8, 19]. Other mediators, such as autacoids, hormones, cytokines/chemokines, neuro-peptides, amino acids, nitric oxide/nitrite, RNAs, and micro RNAs, are also reported to be the possible humoral factor(s) [6, 16]. At the target level, it is uncertain whether the increase in acetylcholine concentration in the myocardium mediates the cardioprotective effects of RIC [1]. Pathways such as endothelial nitric oxide synthase/ protein kinase G (eNOS/PKG), reperfusion injury salvage kinases (RISK), and survivor activating factor enhancement (SAFE) pathways, have all been reported as potentially important intracellular signal transduction at the target organ following RIC [16]. Although the precise mechanisms of the cytoprotective effects remain to be fully elucidated, what is clear is that these effects involve mitigation of the inflammatory response both in circulating leukocytes [29, 33, 37], and in the ischemic tissue [27, 33, 37]. This ‘anti-inflammatory’ effect of RIC has led to its study in other model systems, not involving classical ischemia–reperfusion pathways. Indeed, several studies have shown that RIC improved mortality in lipopolysaccharide (LPS)-induced sepsis [12, 15]. Another study showed that RIC preserved function in the microcirculation, improved organ function, and prolonged survival in sepsis induced by injecting autologous feces [22].
In the present study, we evaluated the effect of limb RIC on ventricular function using echocardiography in an LPS-induced sepsis mouse model. In addition, we assessed circulating inflammatory mediators and local cytokine responses in the target organs to investigate the mechanisms of RIC’s effect in sepsis. In addition, we subsequently evaluated the effect of RIC on prognosis in sepsis. Importantly, we not only assessed the effect of RIC, but also assessed the effect of additional daily RIC on mortality in our sepsis model.
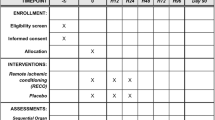
Methods
Animals
Male BALB/c mice (8–10 weeks) were obtained from Charles River Laboratories (Ashland, OH). The experimental protocol was approved by the Animal Care and Use Committee of Cincinnati Children’s Research Foundation.
RIC
RIC was induced by 4 cycles of 5 min ischemia (left hindlimb ischemia using a tourniquet around the upper thigh) and subsequent 5 min reperfusion without anesthesia in accordance with the previous reports [14, 34].
Effect of RIC on hemodynamics cardiac function
Sham (n = 9), LPS (n = 14), and LPS + RIC (n = 16) groups were prepared as mentioned above. The mice received 10 mg/kg LPS intraperitoneal injection, and echocardiography was performed 16 h later. Anesthesia was induced with inhaled isoflurane, chest hair removed with a depilatory agent, and the mouse secured with tape to the warmed imaging platform. Echocardiography was performed using a Vevo2100 imaging system equipped with a 40 MHz high-frequency transducer (VisualSonics Inc. Toronto, Canada) in accordance with the American Society of Echocardiography standard views. All images were analyzed by registered cardiovascular sonographers specializing in animal’s sonography using the VisualSonics software package. To minimize bias, the studies were randomly presented to the measuring sonographer and date/time stamps obscured. All measurements were in triplicate on three consecutive cardiac cycles and reported as an averaged value. Left ventricular ejection fraction and fractional shortening were measured using M-mode. Cardiac output, stroke volume, left ventricular end-diastolic, and systolic volume were measured using two-dimensional echo. Longitudinal, radial, and circumferential strain was measured using speckle-tracking echocardiography.
Effect of RIC on early and late inflammatory mediators
Sham, LPS, and LPS + RIC groups were prepared (n = 4 mice/each group). Saline or LPS (O111:B4, Sigma-Aldrich) 10 mg/kg was injected intraperitoneally. In the LPS + RIC group, RIC was performed just before LPS injection. The mice were euthanized with pentobarbital 1, 2, 4, and 16 h after the injection, and blood was drawn from inferior vena cava. The blood samples were collected and centrifuged at 3000 rpm for 15 min, and plasma samples were collected as the resulting supernatant. Tumor necrosis factor-alfa (TNF-α), interleukin 1 beta (IL-1β) and IL-6 were measured using enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems, Inc. Minneapolis, MN). These ELISA kits were used according to the manufacturer’s instructions.
To evaluate plasma HMGB1 level, mice were divided into sham, LPS and LPS + RIC groups (n = 8 mice/each group), and the mice were sacrificed 16 h after saline or LPS injection. We measured plasma high-mobility group box 1 protein (HMGB1) using western blot as previously reported [10, 23, 32]. Briefly, an Amicon Ultra-0.5 centrifugal filter device (MilliporeSigma, Burlington, MA) was used to remove proteins larger than 100 kDa molecular weight. The filtrated plasma was loaded on Bolt Bis–Tris gels (Thermo Fisher Scientific Co., Waltham, MA), and the gels were run at 100 V constant using MOPS SDS running buffer (Thermo Fisher Scientific Co.). Proteins were transferred to the membrane, and the membrane was incubated with anti-HMGB1 antibody (ab18256) (Abcam, Cambridge, MA) overnight at 4 °C. The membranes were incubated with anti-rabbit antibody (Thermo Fisher Scientific Co.) for 90 min. Developing reagents (Thermo Fisher Scientific Inc.) was used for developing membrane. The band intensity was measured using Image J.
Effect of RIC on systemic organs in LPS-induced experimental endotoxemia
The mice were divided into sham (n = 6), LPS (n = 7), and LPS + RIC (n = 8) groups, and sacrificed 16 h after 10 mg/kg LPS intraperitoneal injection. Blood, heart, liver, and kidney samples were collected. Blood was centrifuged, and plasma samples were stored. Tissue samples were stored at – 80 °C until the tissues were subsequently homogenized with radioimmunoprecipitation assay buffer for western blotting. Plasma cardiac troponin I (cTnI), aspartate transaminase (AST), alanine transaminase (ALT), blood urea nitrogen (BUN), and creatinine (Cr) were measured using the plasma samples. TnI ELISA kit from Life Diagnostics, Inc. (West Chester, PA), AST and ALT kits from BioLegend (San Diego, CA), and BUN kit from Thermo Fisher Scientific Co. were used for their measurements. Every assay kit was used according to the manufacturers’ instructions.
We also assessed mitogen-activated protein kinases signaling by performing western blot using homogenized tissue samples from heart, liver, and kidney. Anti-extracellular signal-regulated kinase (ERK) (#9102), phospho-ERK (#9101), c-Jun N-terminal kinase (JNK) (#9252), and phospho-JNK (#4668) antibodies (cell-signaling technology) were used as the first antibodies. Anti-rabbit antibody (Thermo Fisher Scientific Co.) was used as the second antibody.
Survival experiment
Non-treated, RIC, and daily repeated RIC groups were prepared (n = 20 mice/each group). In RIC group, RIC was performed just before LPS injection. In daily repeated RIC group, RIC was repeated every day for 5 days in addition to the first RIC. Daily repeated RIC consisted of 4 cycles of 5 min ischemia (left hindlimb ischemia using a tourniquet around the upper thigh) and subsequent 5 min reperfusion, the same protocol used for the first RIC procedure performed just before LPS injection. The mice were assessed every 12 h for 7 days.
Statistical analysis
All data were expressed as mean ± SEM. Student’s t test was used to compare mean values between two groups. Differences between three groups were determined by ANOVA. When significant differences were detected by ANOVA, Bonferroni test was used for post hoc comparisons. Gehan–Breslow–Wilcoxon test was used for survival analysis. A value of p < 0.05 was regarded as a significant difference. Statistical analyses were performed using the Prism 6 (GraphPad Software, CA).
Results
RIC improved ventricular function
Ejection fraction was decreased in LPS group compared with sham group, and it was preserved in LPS + RIC group (47.8 ± 2.5, 32.2 ± 4.2, and 46.9 ± 3.7% in sham, LPS, and LPS + RIC group, respectively, p = 0.01). Fractional shortening was also decreased in LPS group, and it was preserved in LPS + RIC group (23.7 ± 1.5, 15.5 ± 2.4, and 23.7 ± 1.5% in sham, LPS, and LPS + RIC group, respectively, p = 0.02) (Fig. 1a–c). Strain analysis showed that longitudinal strain was worsened in LPS group, and it was significantly improved by RIC. The same trend was observed in circumferential and radial strain (Fig. 1d–f).
RIC improved ventricular function and hemodynamics. Balb/c mice were divided into sham (n = 9), LPS (n = 14), and LPS + RIC (n = 16) groups. Echocardiography was performed 16 h after saline or LPS intraperitoneal injection. Ejection fraction and fractional shortening were decreased in LPS group compared with sham group, and it was preserved in LPS + RIC group (a–c). Longitudinal, circumferential, and radial strain were worsened in LPS group, and RIC significantly improved this parameter (d–f). Cardiac output and stroke volume were decreased in LPS group, and they were preserved in LPS + RIC group (g, h). There was no difference in left ventricular end-diastolic volume; whereas, left ventricular end-systolic volume was significantly smaller in LPS + RIC group compared with LPS group (i, j). LPS injection significantly reduced heart rate, and RIC tended to increase it although there was no statistically significant difference (k). LPS lipopolysaccharide, RIC remote ischemic conditioning. Data are mean ± SEM. *p < 0.05; †p < 0.01; ‡p < 0.001; §p < 0.0001; vs. LPS group as tested by ANOVA
RIC improved hemodynamics
Two-dimensional echo showed that cardiac output was decreased in LPS group and that it was preserved in LPS + RIC group (6.0 ± 0.9, 2.8 ± 0.2, and 5.4 ± 0.9 ml/min, in sham, LPS, and LPS + RIC group, respectively, p < 0.01) (Fig. 1g). Stroke volume was also decreased in LPS group, and RIC improved it (16.0 ± 2.1, 9.6 ± 0.7, and 15.2 ± 1.3 μl, in sham, LPS, and LPS + RIC group, respectively, p < 0.01) (Fig. 1h). There was no difference in left ventricular end-diastolic volume, whereas left ventricular end-systolic volume was significantly smaller in LPS + RIC group compared with LPS group (Fig. 1i, j). LPS injection significantly reduced HR, and RIC tended to increase it, although there was no statistically significant difference (Fig. 1k).
RIC negatively regulated early and late inflammatory mediators
RIC reduced the LPS-induced increase of plasma TNF-α at 1 h (819 ± 92 vs. 2184 ± 89 pg/ml, p < 0.0001) and 2 h (598 ± 25 vs. 2360 ± 167 pg/ml, p < 0.0001) after LPS injection (Fig. 2a). RIC also inhibited spleen TNF-α increase 1 h (194 ± 24 vs. 301 ± 22 ng/g protein, p < 0.01) and 2 h (122 ± 21 vs. 217 ± 38 ng/g protein, p < 0.01) after LPS injection (Fig. 2b). Plasma IL-1β and IL-6 levels peaked 16 h after LPS injection. In the LPS + RIC group, peak plasma IL-1β and IL-6 were significantly lower compared with LPS group (43 ± 5 vs. 516 ± 137 pg/ml, p < 0.05; 2.0 ± 0.9 vs. 145.7 ± 41.0 ng/ml, p < 0.0001) (Fig. 2c, d). Plasma HMGB1 was almost 6 times lower in LPS + RIC group compared with LPS group (p < 0.05) 16 h after LPS injection (Fig. 2e).
RIC negatively regulated early and late inflammatory mediators. Balb/c mice were divided into sham, LPS, and LPS + RIC groups were prepared (n = 4 mice/each group). Saline or LPS (O111:B4) 10 mg/kg was injected intraperitoneally, and RIC was performed just before LPS injection. Plasma TNF-α, IL-1β, and IL-6 were measured using ELISA 1, 2, 4, and 16 h after the injection. RIC reduced the LPS-induced increase of plasma and spleen TNF-α at 1 h and 2 h after LPS injection (a, b). In the RIC group, peak plasma IL-1β and IL-6 were significantly lower compared with LPS group. c, d Sham, LPS and LPS + RIC groups (n = 8 mice/each group) mice were prepared, and plasma HMGB1 was measured using western blot 16 h after saline or LPS injection. Plasma HMGB1 was 5.9 times lower in LPS + RIC group compared with LPS group (e). HMGB1 high-mobility group box 1 protein, IL-1β interleukin 1 beta, IL-6 interleukin 6, LPS lipopolysaccharide, RIC remote ischemic conditioning, TNF-α tumor necrosis factor-alfa. Data are mean ± SEM of 6–8 mice per group. *p < 0.05; †p < 0.01; ‡p < 0.001; §p < 0.0001; vs. LPS group as tested by Student’s test
RIC protected systemic organs
Plasma cTnI level was higher in LPS group compared with control group, and RIC attenuated the LPS-induced cTnI increase (0.0 ± 0.0, 0.39 ± 0.16, and 0.03 ± 0.03 ng/ml in sham, LPS, and LPS + RIC group, respectively, p < 0.05) (Fig. 3a). In terms of liver function, LPS injection increased AST, and RIC significantly suppressed its increase (5.5 ± 0.9, 42.5 ± 4.1, and 29.2 ± 2.3 IU/l in sham, LPS, and LPS + RIC group, respectively, p < 0.0001) (Fig. 3b). ALT was also increased by LPS injection, and it was suppressed by RIC (4.9 ± 0.5, 78.8 ± 18.7, and 12.1 ± 1.7 IU/l in sham, LPS, and LPS + RIC group, respectively, p = 0.0002) (Fig. 3c). Regarding renal function, LPS injection increased BUN, and RIC significantly suppressed its increase (20.4 ± 1.4, 72.9 ± 4.6, and 54.6 ± 6.6 mg/dl in sham, LPS, and LPS + RIC group, respectively, p < 0.0001) (Fig. 3d). Cr was also increased by LPS injection, and its increase was inhibited by RIC (0.16 ± 0.03, 0.26 ± 0.02, and 0.18 ± 0.02 mg/dl in sham, LPS, and LPS + RIC group, respectively, p < 0.01) (Fig. 3e).
RIC protected heart, liver, and kidney. Balb/c mice were divided into sham (n = 6), LPS (n = 7), and LPS + RIC (n = 8) groups, and sacrificed 16 h after LPS intraperitoneal injection. Blood samples were collected, and plasma cTnI, AST, ALT, BUN, and Cr were measured using each assay kit. Compared with control group, cTnI, AST. ALT, BUN, and Cr were higher in LPS group, and RIC attenuated the LPS-induced their increases (a–e). AST aspartate transaminase, ALT alanine transaminase, BUN blood urea nitrogen, Cr creatinine, cTnI cardiac troponin I, LPS lipopolysaccharide, RIC remote ischemic conditioning. Data are mean ± SEM. *p < 0.05; †p < 0.01; ‡p < 0.001; §p < 0.0001; vs. LPS group as tested by ANOVA
LPS-induced ERK-signaling activation was inhibited by RIC in heart, liver, and kidney (Fig. 4a–c). LPS-induced JNK signaling activation was also inhibited by RIC in heart, liver, and kidney (Fig. 4d–f).
RIC suppressed MAPK signal activation in systemic organs. Balb/c mice were divided into sham (n = 6), LPS (n = 7), and LPS + RIC (n = 8) groups. The mice were sacrificed, and heart, liver, kidney samples were collected 16 h after LPS intraperitoneal injection, and homogenized. Using the homogenized tissue, MAPK signaling was assessed by performing western blot. LPS-induced ERK-signaling activation was inhibited by RIC in heart, liver, and kidney (a–c). LPS-induced JNK signaling activation was also inhibited by RIC in heart, liver, and kidney (d–f). ERK extracellular signal-regulated kinase, JNK c-Jun N-terminal kinase, LPS lipopolysaccharide, MAPK mitogen-activated protein kinase. Data are mean ± SEM. *p < 0.05; †p < 0.01; ‡p < 0.001; §p < 0.0001; vs. LPS group as tested by ANOVA
RIC improved survival rate in LPS-induced experimental endotoxemia
In the non-treated group, the first death was observed within 12 h after LPS injection, and the 7-day survival rate was 35%. In the RIC group, the first death was observed 24 h after LPS injection, and the 7-day survival rate was 70%, which was significantly higher than that in non-treated group (p = 0.0037) (Fig. 5). Remarkably, all the mice in the daily repeated RIC group survived, which was significantly higher than those in RIC group (p = 0.0088).
Acute and chronic RIC improved mortality in LPS-induced sepsis. Non-treated, RIC, and daily repeated RIC groups were prepared (n = 20/each group). In RIC group, RIC was performed just before LPS injection. In daily repeated RIC group, RIC was repeated every day for 5 days in addition to the initial RIC. The mice were assessed every 12 h for 7 days. In the non-treated group, the 7-day survival rate was 35%. In the RIC group, the 7-day survival rate was 70%, which was significantly higher than that in non-treated group (p = 0.0037). Remarkably, all the mice in the daily repeated RIC group survived. The survival rate in this group was significantly higher than that in RIC group (p = 0.0088). LPS lipopolysaccharide, RIC remote ischemic conditioning. Gehan–Breslow–Wilcoxon test was used for statistical analysis
Discussion
The cardioprotective effect of RIC after myocardial infarction has been reported in many previous preclinical and clinical studies [3, 14, 20, 26, 31]. The potentially beneficial effects of RIC extend beyond acute cardioprotection, however. RIC has also been shown to protect other organs, such as liver, kidney, and brain, from ischemia–reperfusion injury [9]. Although the mechanism of RIC has not been fully elucidated, there is extensive evidence that the effects of RIC go beyond induction of classic cytoprotective signaling pathways. Several groups have shown an important anti-inflammatory effect of RIC. Konstantinov et al. showed that RIC negatively regulates inflammatory gene expression [17], and Shimizu et al. subsequently demonstrated that RIC suppresses human neutrophil adhesion and phagocytosis [29]. While this ‘anti-inflammatory’ effect of RIC may contribute to the reduction in post-MI remodeling [34], there may be other beneficial effects. Indeed, Orbegozo Cortés et al. recently reported that RIC, induced by balloon occlusion of the aortic bifurcation, improved hemodynamics, preserved tissue perfusion, and leads to better survival in bacteria-induced septic sheep [22]. Furthermore, Kim et al. also reported that RIC improved inflammatory responses and survival in the LPS-induced sepsis mouse model [15], but myocardial effects were not examined.
We used a similar LPS-induced sepsis model to evaluate the effect of RIC on ventricular function and hemodynamics using echocardiography. As expected, LPS injection decreased EF and FS consistent with previous reports [21, 35]. Longitudinal, radial, and circumferential strain were also reduced by LPS, which supports the notion that LPS-induced sepsis reduces ventricular systolic function (septic cardiomyopathy). The impact of RIC on these adverse effects, or their hemodynamic consequences, has not been examined in detail; however, all of the adversely affected echocardiographic parameters were improved by RIC. Furthermore, by two-dimensional echo, stroke volume and cardiac output were decreased by LPS administration and improved by RIC.
Sepsis is a systemic inflammatory response syndrome caused by infection and can be a life-threatening pathophysiological condition. Septic cardiomyopathy is transient or fatal myocardial dysfunction caused by inflammatory cytokines such as TNF-α, IL-1β, and IL-6 released by inflammatory cells in sepsis [13]. HMGB1, which is one of the damage-associated molecular patterns (DAMPs), is known as a late mediator of lethality in sepsis [32] and is also a trigger of septic cardiomyopathy [13]. Sepsis-induced myocardial dysfunction decreases systemic organ blood perfusion, further increases the release of DAMPs, accelerates systemic inflammation in systemic organs, and consequently leads to MOF [13]. Therapeutic intervention to reduce sepsis-induced inflammatory cytokines and the subsequent myocardial dysfunction they induce may, therefore, improve the incidence of multiple organ failure (MOF) and mortality in sepsis. We hypothesized that RIC suppresses inflammatory cytokines and HMGB1, attenuates septic cardiomyopathy, protects systemic organs, and improves mortality in sepsis.
The peak plasma TNF-α level in our animals was significantly suppressed by RIC, compatible with the previous report by Kim et al. [15]. The spleen is an important source of TNF-α production [11], and it was recently reported that the activation of a vago-splenic axis may be causally associated with RIC’s cardioprotective effect [8, 19]. In addition, TNF-α production in spleen is reportedly reduced by vagus nerve stimulation via cholinergic anti-inflammatory pathway [2]. Our results demonstrated that the increase of splenic TNF-α was also suppressed by RIC, indicating the possibility that spleen plays an important role in RIC’s anti-inflammatory effect in this sepsis model. RIC also suppressed the release of other circulating inflammatory cytokines such as IL-1β and IL-6 in LPS-induced sepsis, suggesting a broad anti-inflammatory effect of this strategy. This reduction in the systemic inflammatory response was associated with improved myocardial function.
We subsequently investigated the effect of RIC on LPS-induced myocardial tissue damage and inflammatory cell-signaling activation. RIC significantly reduced the LPS-induced increase in cTnI, suggesting that RIC suppresses myocardial tissue damage and protects the heart. At the cellular level, LPS itself acts on pattern recognition receptors such as toll-like receptors and stimulates intracellular inflammatory signaling including ERK and JNK [5]. TNF-α, IL-1β, IL-6, and HMGB1 are known to act on toll-like receptors to stimulate these inflammatory signaling [28, 35]. The results of the current studies showed that ERK and JNK were activated by LPS administration and that RIC dramatically suppressed the activation of ERK, JNK accompanied with decreased TNF-α, IL-1β, IL-6, and HMGB1. HMGB1 is a mediator that has been shown to influence significantly the prognosis in sepsis [32]. In animal sepsis models, plasma HMGB1 levels peak 16–24 h after the onset, and, several studies have reported the efficacy of HMGB1 antibody on sepsis [32, 36]. Moreover, HMGB1 has a direct cardio-suppressant effect function [13, 35]. Our novel finding of an almost sixfold reduction in plasma HMGB1 levels is possibly one of the more important effects RIC, in terms of preservation of cardiac function and improving prognosis in sepsis.
That said, it was clear that RIC also mitigated LPS-induced MOF. Blood chemistry tests revealed that AST, ALT, BUN, and Cr were all worsened by administration of LPS, and RIC significantly improved circulating levels. This might be via direct, cytoprotective, pathways or via secondary effects resulting from improved myocardial performance. Maintenance of cardiac output by RIC may clearly contribute to the protection of liver and kidney, but we also demonstrated that intracellular inflammatory signaling such as ERK and JNK was significantly suppressed in the liver and kidney by RIC. Therefore, inhibiting the increases of circulating inflammatory mediators and suppressing subsequent intracellular inflammatory signaling may also contribute to the protection of liver and kidney by RIC in LPS-induced sepsis.
We also examined the effect of a single administration of RIC on mortality in our LPS-induced sepsis model. In the RIC group, the survival rate was significantly higher than that of LPS group, which is compatible with that of previous reports [12, 15]. Unlike prior studies, we also examined the effect of repeated episodes of RIC on outcome. Reports on the effect of chronically repeated RIC have recently increased. Wei et al. were the first to report that the RIC performed daily for a month after myocardial infarction reduced the peri-infarct inflammatory reaction, inhibited myocardial fibrosis, and leads to improved cardiac functional recovery and survival [34]. More recently, Pryds et al. reported that daily RIC reduced plasma NT-pro BNP and promoted fibrinolysis in chronic ischemic heart failure patients [24, 25]. Consistent with these therapeutic effects of daily RIC, remarkably all mice survived when subjected to daily repeated RIC, indicating that chronic RIC has a potentially important additional effect in terms of mortality in sepsis. However, it is worth noting that we did not evaluate the effect of additional repeated RIC on inflammatory mediators or systemic organs damage in this proof-of-principle experiment. The mechanisms of daily repeated RIC’s therapeutic remain unsolved both in the previous reports and our study, and therefore, future study is needed to determine the mechanisms of this additional benefit.
Limitations
The LPS-induced sepsis model is clearly different from clinical sepsis in that there is no infectious source; however, the LPS model has the advantage of having been extensively used for preclinical testing of potential clinical therapies. Nonetheless, although RIC exerted an anti-inflammatory effect in this experiment, and prior studies have demonstrated direct effects on neutrophil activity in humans, these effects may ultimately be adverse by suppressing appropriate responses to bacterial infection. Consequently, prior to clinical application, it will be necessary to verify our findings with a sepsis model using live bacteria. Finally, in clinical practice, it is obviously impossible to perform RIC on patients prior to the development of clinical sepsis (unless administered prior to a procedure associated with a risk of systemic sepsis). Our data, however, support the performance of future studies, in which the effect of RIC initiated after the onset of sepsis on sepsis-induced cardiomyopathy, MOF, and mortality should be evaluated.
Conclusion
In conclusion, RIC reduced circulating inflammatory mediators associated with septic cardiomyopathy, suppressed inflammatory signaling pathways in heart tissue, reduced cardiac damage, and consequently preserved ventricular function in LPS-induced septic cardiomyopathy. RIC also preserved hepatic and renal function, and improved mortality in our LPS-induced sepsis mouse model. Although additional repeated RIC further improved mortality in sepsis, further studies are needed to fully understand the mechanisms of its benefit.
References
Basalay MV, Davidson SM, Gourine AV, Yellon DM (2018) Neural mechanisms in remote ischaemic conditioning in the heart and brain: mechanistic and translational aspects. Basic Res Cardiol 113:25. https://doi.org/10.1007/s00395-018-0684-z
Borovikova LV, Ivanova S, Zhang M, Yang H, Botchkina GI, Watkins LR, Wang H, Abumrad N, Eaton JW, Tracey KJ (2000) Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 405:458–462 https://doi.org/10.1038/35013070
Bøtker HE, Kharbanda R, Schmidt MR, Bøttcher M, Kaltoft AK, Terkelsen CJ, Munk K, Andersen NH, Hansen TM, Trautner S, Lassen JF, Christiansen EH, Krusell LR, Kristensen SD, Thuesen L, Nielsen SS, Rehling M, Sørensen HT, Redington AN, Nielsen TT (2010) Remote ischaemic conditioning before hospital admission, as a complement to angioplasty, and effect on myocardial salvage in patients with acute myocardial infarction: a randomised trial. Lancet 375:727–734. https://doi.org/10.1016/S0140-6736(09)62001-8
Donato M, Buchholz B, Rodriguez M, Pérez V, Inserte J, García-Dorado D, Gelpi RJ (2013) Role of the parasympathetic nervous system in cardioprotection by remote hindlimb ischaemic preconditioning. Exp Physiol 98:425–434. https://doi.org/10.1113/expphysiol.2012.066217
Dumitru CD, Ceci JD, Tsatsanis C, Kontoyiannis D, Stamatakis K, Lin JH, Patriotis C, Jenkins NA, Copeland NG, Kollias G, Tsichlis PN (2000) TNF-α induction by LPS is regulated posttranscriptionally via a Tpl2/ERK-dependent pathway. Cell 103:1071–1083. https://doi.org/10.1016/S0092-8674(00)00210-5
Gedik N, Kottenberg E, Thielmann M, Frey UH, Jakob H, Peters J, Heusch G, Kleinbongard P (2017) Potential humoral mediators of remote ischemic preconditioning in patients undergoing surgical coronary revascularization. Sci Rep 7:12660 https://doi.org/10.1038/s41598-017-12833-2
Hausenloy DJ, Bøtker HE, Ferdinandy P, Heusch G, Ng GA, Redington A, Garcia-Dorado D (2019) Cardiac innervation in acute myocardial ischaemia/reperfusion injury and cardioprotection. Cardiovasc Res (in press). https://doi.org/10.1093/cvr/cvz053
Heusch G (2019) The spleen in myocardial infarction. Circ Res 124:26–28. https://doi.org/10.1161/CIRCRESAHA.118.314331
Heusch G, Bøtker HE, Przyklenk Redington A, Yellon D (2015) Remote ischemic conditioning. J Am Coll Cardiol 65:177–195. https://doi.org/10.1016/j.jacc.2014.10.031
Huston JM, Gallowitsch-Puerta M, Ochani M, Ochani K, Yuan R, Rosas-Ballina M, Ashok M, Goldstein RS, Chavan S, Pavlov VA, Metz CN, Yang H, Czura CJ, Wang H, Tracey KJ (2007) Transcutaneous vagus nerve stimulation reduces serum high mobility group box 1 levels and improves survival in murine sepsis. Crit Care Med 35:2762–2768. https://doi.org/10.1097/01.CCM.0000288102.15975.BA
Huston JM, Ochani M, Rosas-Ballina M, Liao H, Ochani K, Pavlov VA, Gallowitsch-Puerta M, Ashok M, Czura CJ, Foxwell B, Tracey KJ, Ulloa L (2006) Splenectomy inactivates the cholinergic antiinflammatory pathway during lethal endotoxemia and polymicrobial sepsis. J Exp Med 203:1623–1628. https://doi.org/10.1084/jem.20052362
Joseph B, Khalil M, Hashmi A, Hecker L, Kulvatunyou N, Tang A, Friese RS, Rhee P (2017) Survival benefits of remote ischemic conditioning in sepsis. J Surg Res 213:131–137. https://doi.org/10.1016/j.jss.2016.01.033
Kakihana Y, Ito T, Nakahara M, Yamaguchi K, Yasuda T (2016) Sepsis-induced myocardial dysfunction: pathophysiology and management. J Intensive Care 4:22. https://doi.org/10.1186/s40560-016-0148-1
Kharbanda RK, Mortensen UM, White PA, Kristiansen SB, Schmidt MR, Hoschtitzky JA, Vogel M, Sorensen K, Redington AN, MacAllister R (2002) Transient limb ischemia induces remote ischemic preconditioning in vivo. Circulation 106:2881–2883. https://doi.org/10.1161/01.CIR.87.3.893
Kim YH, Yoon DW, Kim JH, Lee JH, Lim CH (2014) Effect of remote ischemic post-conditioning on systemic inflammatory response and survival rate in lipopolysaccharide-induced systemic inflammation model. J Inflamm (Lond) 11:16. https://doi.org/10.1186/1476-9255-11-16
Kleinbongard P, Skyschally A, Heusch G (2016) Cardioprotection by remote ischemic conditioning and its signal transduction. Pflugers Arch 469:159–181. https://doi.org/10.1007/s00424-016-1922-6
Konstantinov IE, Arab S, Kharbanda RK, Li J, Cheung MM, Cherepanov V, Downey GP, Liu PP, Cukerman E, Coles JG, Redington AN (2004) The remote ischemic preconditioning stimulus modifies inflammatory gene expression in humans. Physiol Genomics 19:143–150. https://doi.org/10.1152/physiolgenomics.00046.2004
Li J, Rohailla S, Gelber N, Rutka J, Sabah N, Gladstone RA, Wei C, Hu P, Kharbanda RK, Redington AN (2014) MicroRNA-144 is a circulating effector of remote ischemic preconditioning. Basic Res Cardiol 109:423. https://doi.org/10.1007/s00395-014-0423-z
Lieder HR, Kleinbongard P, Skyschally A, Hagelschuer H, Chilian WM, Heusch G (2018) Vago-splenic axis in signal transduction of remote ischemic preconditioning in pigs and rats. Circ Res 123:1152–1163. https://doi.org/10.1161/CIRCRESAHA.118.313859
McLeod SL, Iansavichene A, Cheskes S (2017) Remote ischemic perconditioning to reduce reperfusion injury during acute ST-segment-elevation myocardial infarction: A systematic review and meta-analysis. J Am Heart Assoc 17:6. https://doi.org/10.1161/JAHA.117.005522
Niu J, Azfer A, Kolattukudy PE (2008) Protection against lipopolysacharide-induced myocardial dysfunction in mice by cardiac-specific expression of soluble Fas. J Mol Cell Cardiol 44:160–169. https://doi.org/10.1016/j.yjmcc.2007.09.016
Orbegozo Cortés D, Su F, Santacruz C, Hosokawa K, Donadello K, Creteur J, De Backer D, Vincent JL (2016) Ischemic conditioning protects the microcirculation, preserves organ function, and prolongs survival in sepsis. Shock 45:419–427. https://doi.org/10.1097/SHK.0000000000000526
Pavlov VA, Ochani M, Yang LH, Gallowitsch-Puerta M, Ochani K, Lin X, Levi J, Parrish WR, Rosas-Ballina M, Czura CJ, Larosa GJ, Miller EJ, Tracey KJ, Al-Abed Y (2007) Selective α7-nicotinic acetylcholine receptor agonist GTS-21 improves survival in murine endotoxemia and severe sepsis. Crit Care Med 35:1139–1144. https://doi.org/10.1097/01.CCM.0000259381.56526.96
Pryds K, Kristiansen J, Neergaard-Petersen S, Nielsen RR, Schmidt MR, Refsgaard J, Kristensen SD, Bøtker HE, Hvas AM, Grove EL (2017) Effect of long-term remote ischaemic conditioning on platelet function and fibrinolysis in patients with chronic ischaemic heart failure. Thromb Res 153:40–46. https://doi.org/10.1016/j.thromres.2017.03.008
Pryds K, Nielsen RR, Jorsal A, Hansen MS, Ringgaard S, Refsgaard J, Kim WY, Petersen AK, Bøtker HE, Schmidt MR (2017) Effect of long-term remote ischemic conditioning in patients with chronic ischemic heart failure. Basic Res Cardiol 112:67. https://doi.org/10.1007/s00395-017-0658-6
Przyklenk K, Bauer B, Ovize M, Kloner RA, Whittaker P (1993) Regional ischemic ‘preconditioning’ protects remote virgin myocardium from subsequent sustained coronary occlusion. Circulation 87:893–899. https://doi.org/10.1161/01.CIR.87.3.893
Rohailla S, Clarizia N, Sourour M, Sourour W, Gelber N, Wei C, Li J, Redington AN (2014) Acute, delayed and chronic remote ischemic conditioning is associated with downregulation of mTOR and enhanced autophagy signaling. PLoS ONE 9:e111291. (https://doi.org/10.1371/journal.pone.0111291)
Sabio G, Davis RJ (2014) TNF and MAP kinase signaling pathways. Semin Immunol 26:237–245. https://doi.org/10.1016/j.smim.2014.02.009
Shimizu M, Saxena P, Konstantinov IE, Cherepanov V, Cheung MM, Wearden P, Zhangdong H, Schmidt M, Downey GP, Redington AN (2010) Remote ischemic preconditioning decreases adhesion and selectively modifies functional responses of human neutrophils. J Surg Res 158:155–161. https://doi.org/10.1016/j.jss.2008.08.010
Shimizu M, Tropak M, Diaz RJ, Suto F, Surendra H, Kuzmin E, Li J, Gross G, Wilson GJ, Callahan J, Redington AN (2009) Transient limb ischaemia remotely preconditions through a humoral mechanism acting directly on the myocardium: evidence suggesting cross-species protection. Clin Sci (Lond) 117:191–200. https://doi.org/10.1042/CS20080523
Thielmann M, Kottenberg E, Kleinbongard P, Wendt D, Gedik N, Pasa S, Price V, Tsagakis K, Neuhäuser M, Peters J, Jakob H, Heusch G (2013) Cardioprotective and prognostic effects of remote ischaemic preconditioning in patients undergoing coronary artery bypass surgery: a single-centre randomised, double-blind, controlled trial. Lancet 382:597–604. https://doi.org/10.1016/S0140-6736(13)61450-6
Wang H, Bloom O, Zhang M, Vishnubhakat JM, Ombrellino M, Che J, Frazier A, Yang H, Ivanova S, Borovikova L, Manogue KR, Faist E, Abraham E, Andersson J, Andersson U, Molina PE, Abumrad NN, Sama A, Tracey KJ (1999) HMG-1 as a late mediator of endotoxin lethality in mice. Science 285:248–251. https://doi.org/10.1126/science.285.5425.248
Wang Q, Liu GP, Xue FS, Wang SY, Cui XL, Li RP, Yang GZ, Sun C, Liao X (2015) Combined vagal stimulation and limb remote ischemic perconditioning enhances cardioprotection via an anti-inflammatory pathway. Inflammation 38:1748–1760. https://doi.org/10.1007/s10753-015-0152-y
Wei M, Xin P, Li S, Tao J, Li Y, Li J, Liu M, Li J, Zhu W, Redington AN (2011) Repeated remote ischemic postconditioning protects against adverse left ventricular remodeling and improves survival in a rat model of myocardial infarction. Circ Res 108:1220–1225. https://doi.org/10.1161/CIRCRESAHA.110.236190
Xu H, Su Z, Wu J, Yang M, Penninger JM, Martin CM, Kvietys PR, Rui T (2010) The alarmin cytokine, high mobility group box 1, is produced by viable cardiomyocytes and mediates the lipopolysaccharide-induced myocardial dysfunction via a TLR4/phosphatidylinositol 3-kinase γ pathway. J Immunol 184:1492–1498. https://doi.org/10.4049/jimmunol.0902660
Yang H, Ochani M, Li J, Qiang X, Tanovic M, Harris HE, Susarla SM, Ulloa L, Wang H, DiRaimo R, Czura CJ, Wang H, Roth J, Warren HS, Fink MP, Fenton MJ, Andersson U, Tracey KJ (2004) Reversing established sepsis with antagonists of endogenous high-mobility group box 1. Proc Natl Acad Sci USA 101:296–301. https://doi.org/10.1073/pnas.2434651100
Zhang J, Zhang J, Yu P, Chen M, Peng Q, Wang Z, Dong N (2017) Remote ischaemic preconditioning and sevoflurane postconditioning synergistically protect rats from myocardial injury induced by ischemia and reperfusion partly via inhibition TLR4/MyD88/NF-κB signaling pathway. Cell Physiol Biochem 41:22–32. https://doi.org/10.1159/000455815
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interests to report.
Rights and permissions
About this article
Cite this article
Honda, T., He, Q., Wang, F. et al. Acute and chronic remote ischemic conditioning attenuate septic cardiomyopathy, improve cardiac output, protect systemic organs, and improve mortality in a lipopolysaccharide-induced sepsis model. Basic Res Cardiol 114, 15 (2019). https://doi.org/10.1007/s00395-019-0724-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00395-019-0724-3