Abstract
Urotensin II (UTII) and its seven trans-membrane receptor (UTR) are up-regulated in the heart under pathological conditions. Previous in vitro studies have shown that UTII trans-activates the epidermal growth factor receptor (EGFR), however, the role of such novel signalling pathway stimulated by UTII is currently unknown. In this study, we hypothesized that EGFR trans-activation by UTII might exert a protective effect in the overloaded heart. To test this hypothesis, we induced cardiac hypertrophy by transverse aortic constriction (TAC) in wild-type mice, and tested the effects of the UTII antagonist Urantide (UR) on cardiac function, structure, and EGFR trans-activation. After 7 days of pressure overload, UR treatment induced a rapid and significant impairment of cardiac function compared to vehicle. In UR-treated TAC mice, cardiac dysfunction was associated with reduced phosphorylation levels of the EGFR and extracellular-regulated kinase (ERK), increased apoptotic cell death and fibrosis. In vitro UTR stimulation induced membrane translocation of β-arrestin 1/2, EGFR phosphorylation/internalization, and ERK activation in HEK293 cells. Furthermore, UTII administration lowered apoptotic cell death induced by serum deprivation, as shown by reduced TUNEL/Annexin V staining and caspase 3 activation. Interestingly, UTII-mediated EGFR trans-activation could be prevented by UR treatment or knockdown of β-arrestin 1/2. Our data show, for the first time in vivo, a new UTR signalling pathway which is mediated by EGFR trans-activation, dependent by β-arrestin 1/2, promoting cell survival and cardioprotection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Seven-transmembrane receptors (7TMRs) belong to the largest family of membrane receptors, regulating multiple functions in the cardiovascular system [41, 47], and accounting for a large number of prescriptions for heart failure (HF) [17, 25]. Despite optimal therapy, HF remains a relentless, progressive disease with poor prognosis, and thus novel treatments are needed to ameliorate cardiac dysfunction and prolong survival in these patients.
Urotensin II (UTII) is a conserved cyclic neuropeptide expressed in the cardiovascular, neuronal and urogenital systems [5, 11, 29] interacting with a specific 7TMR (UTR) activating Gq and phospholipase C to generate inositol triphosphate and diacylglycerol, and thereby increasing intracellular calcium and activating protein kinase C [1, 14, 28]. UTII and UTR are up-regulated under pathological conditions, including congestive heart failure, essential hypertension, coronary artery disease and type II diabetes [36, 50]. UTII exogenous administration promotes hypertrophy of rat neonatal cardiomyocytes [27], and potentiates isoproterenol-induced cardiac growth [33, 49]. Thus, UTII might be an important determinant of cardiac dysfunction, inducing G-protein-mediated intracellular effects similar to those described for angiotensin II or endothelin-1 [4, 8, 10, 31, 32].
For a number of years, it has been known that 7TMRs activate G-protein signalling and, to limit unrestrained stimulation, G-protein-coupled receptor kinases (GRKs), leading to β-arrestins binding, which sterically interdict further G-protein signalling and scaffold receptors to the internalization machinery [43]. However, it has been recently appreciated that β-arrestins not only terminate G-protein signalling, but also function as adaptor molecules, allowing for the assembly of multiprotein signalling complexes, and promoting novel signalling pathways [24]. Among these, β-arrestins can link 7TMR stimulation to the trans-activation of epidermal growth factor receptor (EGFR) [34] through a number of undefined steps, including metalloproteinases (MMP)-mediated cleavage and extracellular shedding of heparin-binding EGF, resulting in EGFR activation [9, 16, 39, 42]. Very little is known regarding the pathophysiological effects that such novel mechanisms of signal transduction exert in the heart.
Recent studies have suggested that EGFR trans-activation plays a critical role in UTII hypertrophic signal transduction in rat cardiomyocytes [27]. The role(s) of such novel signalling pathways stimulated by UTII in the overloaded heart are currently unknown. Since β-arrestin-mediated β1-adrenergic receptor (β1AR) signalling to the EGFR has been recently shown to be beneficial in mice undergoing chronic sympathetic stimulation [28], in this study we hypothesized that UTII might exert a protective effect in the heart by trans-activating the EGFR. To test this hypothesis, we analyzed the effects of the UTR antagonist Urantide (UR) in a cellular system and in a mouse model of heart failure induced by pressure overload. Both in vivo and in vitro, UR inhibited UTR-mediated EGFR trans-activation and promoted cell death. In response to pressure overload, UR rapidly induced cardiac dysfunction, demonstrating the protective role of this signalling pathway in pathological cardiac remodelling.
Methods
Animal studies
All experiments involving animals were conformed to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85–23, revised 1996) and were approved by the animal welfare regulation of University Federico II of Naples, Italy. Animals were maintained under equal conditions of temperature (21 ± 1°C), humidity (60 ± 5%) and light/dark cycle, and had free access to normal rodent chow.
Mouse model of pressure overload
Wild-type C57BL/6 male mice (8-week-old; n = 30) were anesthetized with an intramuscular injection of ketamine 100 mg/kg and xylazine 5 mg/kg (Sigma). Chronic pressure overload was induced by transverse aortic constriction (TAC) in 10 mice as previously described [12, 38, 45]. Additional mice underwent (the same day of the TAC procedure) the implant of mini-osmotic pumps (Alzet Model 2002; DURECT) as previously described [18] to systemically deliver UTII (TAC + UTII, 12 μmol/kg/day, n = 13), the UTII antagonist Urantide (TAC + UR, 2 μmol/kg/day, n = 12) or the EGFR inhibitor AG1478 (TAC + AG1478, 12 mg/kg/day, n = 6). Another group of animals underwent a left thoracotomy without aortic constriction (SHAM, n = 8). Mice from all the groups were killed 7 days after surgery to perform molecular or histological analyses. During killing, after body weight (BW) calculation, mice were anesthetized as described above, and the efficacy of the pressure overload was invasively tested by measuring the arterial pressures in the right carotid artery (proximal to the suture) and the left right carotid artery (distal to the suture). Only TAC animals with systolic pressure gradients >40 mmHg were included in the study. Next, the hearts were removed and cardiac chambers dissected to assess the left ventricular weight.
Transthoracic echocardiography
Cardiac function was not invasively monitored by transthoracic echocardiography using the Vevo 770 high resolution imaging system (VisualSonics, Toronto, Canada) before the surgery and right before termination. Briefly, the mice were anesthetized as previously described, and echocardiograms were performed with a 30-MHz RMV-707B scanning head and analyzed as previously reported [37].
Cell culture
Human embryonic kidney (HEK) 293 cells and smooth muscle-derived A10 cells (SMCs) were obtained from American Type Culture Collection (ATCC) and maintained in Dulbecco’s modified Eagle’s medium supplemented with 10% FBS, 200 mg/ml l-glutamine, 100 units/ml penicillin, and 100 μg/ml streptomycin. HEK 293 cells were transfected with 1 µg of cDNA encoding EGFR-FLAG, EGFR-GFP, β-arrestin-GFP and UTR with FuGENE6 reagent according to the manufacturer’s instructions (Roche Applied Science). Transfected cells were incubated overnight in serum-free medium supplemented with 0.1% BSA, 10 mM HEPES (pH 7.4), and 1% penicillin prior to stimulation. Under serum starvation conditions, cells were pre-incubated with different UTR antagonists: UR (30 nM), BIM23127 (3 μM), UFP-803 (100 nM), [ORN5] URP (3 μM) and SB657510 (200 nM) or with the EGFR inhibitor AG1478 (1 μM; Calbiochem) for 30 min, followed by stimulation with UTII (100 nM; Sigma-Aldrich), EGF (10 ng/ml; Upstate Biotechnology) for 15 or 5 min (immunoblotting), and 30 min (confocal microscopy).
Confocal microscopy
Following stimulation, HEK293 cells were rinsed with ice-cold PBS and fixed with 3.7% formaldehyde in PBS for 30 min. EGFR internalization and β-arrestin recruitment was visualized by green fluorescence using a single sequential line of excitation filters. The fluorescent data sets were visualized with a Zeiss 510 confocal laser scanning microscope and analyzed by LSM 510 software.
Protein extraction and immunoblot analysis
Cultured cells and left ventricular samples were lysed in a buffer containing 150 mM NaCl, 50 mM Tris pH 8.5 mM EDTA, 1% v/v NP-40, 0.5% w/v deoxycholate, 10 mM NaF, 10 mM Na2 pyrophosphate, 2 mM PMSF, 2 μg/ml leupeptin, 2 μg/ml aprotinin; pH 7.4. Lysates were incubated on ice for 15 min and then centrifuged at 38,000×g for 30 min at 4°C. Protein concentrations in all lysates were measured using a dye-binding protein assay kit (Bio-Rad) and a spectrophotometer reader (Bio Rad) at a wavelength of 595 nm. Immunoblotting and immunoprecipitation were performed using commercially available antibodies (see below) as previously described [19]. Bands were visualized by enhanced chemiluminescence (ECL; Amersham Life Sciences Inc.) according to the manufacturer’s instructions, and were quantified using densitometry (Chemidoc, Biorad, USA). Each experiment and densitometric quantification was separately repeated at least three times.
Antibodies
In the present study, we used commercially available primary antibodies anti-UTR (polyclonal, Sigma-Aldrich), anti-UTII (monoclonal, Phoenix Pharmaceuticals), anti-GAPDH (monoclonal, Santa Cruz), anti-Tubulin (monoclonal, Sants Cruz), anti-GRK2 (monoclonal, Santa Cruz), anti-pERK (monoclonal, Santa Cruz), anti-ERK (monoclonal, Santa Cruz), anti-FLAG (monoclonal, Sigma-Aldrich), anti-EGFR (polyclonal, Santa Cruz), anti-pEGFR Tyr845 (polyclonal, Upstate Biotechnology), anti-phosphotyrosine PY20 (polyclonal, Santa Cruz) and anti-cleaved caspase-3 (monoclonal, Cell signalling), anti-β-arrestin 1/2 (polyclonal, Santa Cruz). Secondary antibodies were purchased from Amersham Life Sciences Inc.
Histology
Left ventricular specimens were fixed in 4% formaldehyde and embedded in paraffin. After de-paraffinization and re-hydratation, 4 μm-thick sections were prepared, mounted on glass slides and stained with Masson trichrome for quantitative analysis of the infarct size as previously described [7] or with 1% Sirius red in picric acid (Carlo Erba Laboratories, Italy) to detect interstitial fibrosis. The fibrotic area (red) was measured in at least 3 hearts/group (2 sections/sample, 6–10 images/section), using a computer-assisted image analysis system (Image J, USA), and was expressed as a percentage of total area. To determine capillary density, sections were incubated with a biotinilated lectin from Bandeiraea simplicifolia (Sigma) and amplified by a Tyramide Signal Amplification (TSA) Biotin System kit (Perkin Elmer Life Sciences, MA). Staining was developed using DAB + substrate chromogen (DAKO, CA) and counterstained with Mayer’s Hematoxylin. Capillary density was quantified by counting the lectin positive capillary numbers, normalized to the tissue area, in 30 randomly-chosen, high-power (200×) fields. All the sections were examined with a microscope (Leitz, DIAPLAN) and images were acquired with a digital camera (Digital JVC, TK-C1380).
TUNEL staining
Terminal deoxynucleotidyl transferase-mediated dUTP nick-end labelling (TUNEL) was performed on fixed paraffin-embedded left ventricular sections (4 μm) using an ApopTag Peroxidase In Situ Apoptosis Detection Kit (Chemicon, UK), according to the manufacturer’s instructions. TUNEL staining was visualized with 3,3’-diaminobenzidine (DAB, Vector), which stained brown the positive nuclei. Cardiac sections were then counterstained with methyl green (Carlo Erba). For cultured cells and AG1478-treated mice, the DNA nicks were determined with the use of an ApopTag Fluorescein Direct In Situ Apoptosis Detection kit (Chemicon, UK) according to the manufacturer’s instructions. TUNEL staining was visualized by specific green fluorescence and nuclei by 4’-6-diamidino-2-phenylindole (DAPI) (nuclear counterstain). All the sections were examined with a microscope (Leitz, DIAPLAN) and images were acquired with a digital camera (Digital JVC, TK-C1380).
Annexin V staining
Adherent A10 cells were treated for 24 h with UTII (100 nM) and UR (30 nM), harvested by trypsinization and combined with floating cells. Next, cells were stained with Annexin V Cy3 (MBL, Japan), and the percentage of apoptosis was analyzed by flow cytometry. All flow cytometric analyses were performed on a flow cytometer equipped with a 25-mW argon ion laser for excitation at 570 nm (FACSCalibur, Becton & Dickinson), and the data were analyzed with the Cell Quest software (Becton & Dickinson). All analyses were repeated 3–4 times with different preparations of cells. Gating was set to exclude debris and cellular aggregates, and 10,000 or more events were counted for each analysis.
β-Arrestin 1/2 knockdown
30–50% confluent HEK293 cells were transfected with 100 pmol siRNA for β-arrestin 1–2 (Stealth siRNA, INVITROGEN), or Stealth RNAi negative control (INVITROGEN) and 1 µg of cDNA encoding for UTR and EGFR-GFP using Lipofectamine 2000 reagent (INVITROGEN) according to the manufacturer’s protocols. All assays were performed 48 h after siRNA transfection. Cells were serum-starved for 12 h, and then stimulated with UTII (100 nM) or EGF (10 ng/ml) for 15 or 5 min (immunoblotting), and 30 min (confocal microscopy).
Statistical analysis
Data are expressed as mean ± SE. Multi-group comparisons were made with a one-way ANOVA with a Tukey’s finishing test. For all analyses, a minimum value of p < 0.05 was considered significant; when present, a p value < 0.001 was specified.
Results
UTR antagonism reduces EGFR trans-activation and promotes cardiac dysfunction in response to pressure overload
In order to study the role of UTII signalling in pathological cardiac remodelling, we induced cardiac hypertrophy by transverse aortic constriction (TAC) in wild-type C67BL/6 mice [13]. This surgical procedure rapidly determines cardiac hypertrophy as shown by cardiac chambers morphometry and echocardiography (Table 1). Following TAC, two additional groups of mice underwent the chronic infusion of the UTR antagonist Urantide (UR) or vehicle by micro-osmotic pumps. In additional experiments, UR circulating levels were evaluated in mice by high performance liquid chromatography–mass spectrometry (HPLC), confirming its bioavailability up to 15 days following micropump implantation (data not shown).
Seven days after the surgery, TAC mice exhibited a significant increase in the expression levels of the UTR (Fig. 1a) and UTII (Fig. 1b) compared to the SHAM, while UR treatment had no effects on UTR or UTII levels. As expected, TAC mice also exhibited an increase in the left ventricle weight to body weight ratio (LVW/BW) compared to SHAM, and UR treatment did not affect cardiac hypertrophy development (LVW/BW, mg/g: SHAM = 4.51 ± 0.6; TAC = 6.04 ± 0.5; TAC + UR = 5.83 ± 0.5 not significant, Fig. 2a; Table 1). Interestingly, TAC + UR mice displayed a rapid impairment of cardiac function as shown by reduced % fractional shortening (% fractional shortening: SHAM = 61.01 ± 1.3, TAC = 51 ± 1.5, TAC + UR = 45 ± 1.5, p < 0.05; Fig. 2b).
Pressure overload induces endogenous UTR signalling. a Representative immunoblots (upper panels) and densitometric analysis (lower panel) of multiple independent experiments to evaluate UTR levels in left ventricular samples from mice undergoing the sham procedure (SHAM), transverse aortic constriction (TAC) or TAC with chronic infusion of the UTR antagonist Urantide (TAC + UR). Tubulin protein levels did not significantly change among the samples (*p < 0.05 vs. SHAM, n = 10 hearts/group). b Left panels representative UTII immuno-staining of cardiac sections of mouse hearts from the different groups (×40). Right panel cumulative data of multiple independent experiments (*p < 0.05 vs. SHAM, n = 10 hearts/group)
UTR antagonism promotes cardiac dysfunction, increases apoptotic cell death and reduces EGFR trans-activation in response to pressure overload. a Bar graphs showing left ventricle weight/body weight (LVW/BW) ratios in SHAM, TAC, and TAC + UR mice (*p < 0.05 vs. SHAM, n = 10 hearts/group). b Left panels representative serial M-mode echocardiographic tracings from SHAM, TAC and TAC + UR mice. Right panel % fractional shortening of SHAM, TAC and TAC + UR mice (*p < 0.05 vs. SHAM; **p < 0.05 vs. SHAM and TAC, n = 10 hearts/group). c Left panels representative TUNEL staining of cardiac sections of mouse hearts from the different groups counterstained with methyl green. Positive nuclei appear brown (arrows; ×600). Right panel cumulative data of multiple independent experiments (*p < 0.05 vs. SHAM; ** p < 0.05 vs. SHAM and TAC, n = 8 hearts/group). d Left panels representative Sirius red staining of cardiac sections of mouse hearts from the different groups (×600). Right panel cumulative data of multiple independent experiments (*p < 0.05 vs. SHAM; ** p < 0.05 vs. SHAM and TAC, n = 8 hearts/group). e Representative immunoblots (upper panels) and densitometric analysis (lower panel) of multiple independent experiments to evaluate pEGFR and EGFR levels in SHAM, TAC and TAC + UR hearts. Total EGFR levels did not significantly change among the groups as shown by similar tubulin staining among the samples (*p < 0.05 vs. SHAM, n = 8 hearts/group). f Representative immunoblots (upper panels) and densitometric analysis (lower panel) of different repeated experiments analyzing pERK protein levels in SHAM, TAC and TAC + UR hearts. Total ERK2 or tubulin levels did not significantly change among the groups as shown by similar tubulin staining among the samples (*p < 0.001 vs. SHAM, n = 8 hearts/group)
Next, to assess the effects of UTR antagonism on cell survival, TUNEL staining was performed in cardiac sections from SHAM, TAC and TAC + UR mice. UR administration significantly increased apoptotic cell death in response to pressure overload, as shown by increased TUNEL-positive nuclei (% apoptotic nuclei: SHAM = 0.031 ± 0.02, TAC = 1.4 ± 0.3, TAC + UR = 2.2 ± 0.2, p < 0.05; Fig. 2c). Furthermore, the increased apoptotic cell death in UR-treated mice was accompanied by a greater extent of interstitial fibrosis in TAC + UR mice (% fibrosis: SHAM = 0.52 ± 0.87, TAC = 8.9 ± 0.83, TAC + UR = 14.3 ± 1.32, p < 0.05; Fig. 2d). Interestingly, UR treatment did not affect capillary density, that was similarly reduced in TAC and TAC + UR compared to SHAM mice (capillary density, % of SHAM: TAC = 74% ± 10.4, TAC + UR = 68% ± 13.3, not significant).
It has been previously shown that EGFR trans-activation plays a critical role in UTII signal transduction in vitro [35]. In order to determine whether UR inhibited UTR-mediated EGFR trans-activation in vivo, EGFR phosphorylation levels were analyzed in cardiac samples from SHAM, TAC and TAC + UR mice. While pressure overload induced a significant increase in EGFR phosphorylation, this activation was completely abolished by the chronic infusion of UR (Fig. 2e). Consistent with these results, ERK activation was significantly induced by TAC, and this was inhibited by UR treatment (Fig. 2f).
EGFR antagonism promotes apoptotic cell death and cardiac dysfunction in response to pressure overload
Since the role of 7TMR-mediated EGFR trans-activation in the heart is controversial, we next tested the effects of the selective EGFR blocker AG1478 in pressure overload-induced cardiac hypertrophy. As expected, AG1478 treatment reduced EGFR and ERK phosphorylation in TAC mice (Fig. 3a, b). Interestingly, AG1478 treatment did not affect cardiac hypertrophy development, but significantly reduced cardiac function, promoted apoptosis and increased fibrosis after 7 days of pressure overload (Fig. 3c–f), suggesting that EGFR signalling is protective under conditions of pressure overload.
EGFR antagonism promotes cardiac dysfunction and apoptotic cell death in response to pressure overload. a Representative immunoblots (upper panels) and densitometric analysis (lower panel) of multiple independent experiments to evaluate pEGFR and EGFR levels in SHAM, TAC and TAC + AG1478 hearts. Total EGFR levels did not significantly change among the groups, as shown by similar GAPDH staining among the samples (*p < 0.05 vs. SHAM, n = 6 hearts/group). b Representative immunoblots (upper panel) and densitometric analysis (lower panel) of different repeated experiments analyzing pERK protein levels in the hearts of SHAM, TAC and TAC + AG1478 mice. Total ERK2 levels did not significantly change among the groups as shown by similar GAPDH staining among the samples (*p < 0.001 vs. SHAM, n = 6 hearts/group). c Bar graphs showing left ventricle weight/body weight (LVW/BW) ratios in SHAM, TAC, and TAC + AG1478 mice (*p < 0.05 vs. SHAM, n = 6 hearts/group). d Left panels representative serial M-mode echocardiographic tracings from SHAM, TAC and TAC + AG1478 mice. Right panel % fractional shortening of SHAM, TAC and TAC + AG1478 mice (*p < 0.05 vs. SHAM; ** p < 0.05 vs. SHAM and TAC, n = 6 hearts/group). e Left panels representative DAPI (right) and TUNEL (left) staining of cardiac sections of mouse hearts from the different groups. Positive nuclei appear green (arrows; ×400). Right panel cumulative data of multiple independent experiments (*p < 0.05 vs. SHAM; **p < 0.05 vs. SHAM and TAC, n = 6 hearts/group). f Left panels representative Sirius red staining of cardiac sections of mouse hearts from the different groups (×600). Right panel cumulative data of multiple independent experiments (*p < 0.05 vs. SHAM; ** p < 0.05 vs. SHAM and TAC, n = 6 hearts/group)
β-Arrestin 1 and β-arrestin 2 are required for UTR trans-activation of EGFR
To better assess the mechanisms by which UTII stimulation could mediate EGFR signalling and induce the activation of downstream signalling pathways, HEK293 cells were transiently transfected with FLAG-EGFR and UTR, and stimulated with UTII with or without UR, or EGF. UTII stimulation resulted in a significant increase in phosphorylation of the EGFR (Fig. 4a, b) along with activation of ERK (Fig. 4a, c). Importantly, these effects could be inhibited by the knockdown of β-arrestin 1/2 (Fig. 4a–c). To determine whether UTR antagonism by molecules different from UR would affect EGFR transactivation, we tested other four different commercially available UTR antagonists on EGFR signalling and internalization (supplementary online Figure S1). Even if with different potency, all tested UTR antagonists (BIM23127, UFP-803, [ORN5] URP, and SB657510) reduced EGFR and ERK phosphorylation, and EGFR internalization (supplementary online Figure S1).
UTR-mediated EGFR trans-activation is β-arrestin-dependent. a Representative immunoblots of multiple independent experiments to evaluate EGFR, pEGFR, ERK2, pERK, β-arrestin1/2 and tubulin levels in HEK 293 cells transfected with EGFR-FLAG and UTR, and then incubated with control siRNA or β-arrestin1/2 siRNA. Cells were unstimulated (CN) or stimulated with UTII, UTII + UR, UR alone or EGF. b Bar graphs showing cumulative data of multiple independent experiments to evaluate EGFR activation in HEK 293 cells; total EGFR levels did not significantly change among the groups (*p < 0.05 vs. CN). c Bar graphs showing cumulative data of multiple independent experiments to evaluate ERK activity in HEK 293 cells, total ERK2 levels did not significantly change among the groups (*p < 0.05 vs. CN). d Panels 1–5 representative β-arrestin-GFP immunofluorescence images in HEK293 cells overexpressing EGFR-FLAG, UTR and β-arrestin-GFP. Panels 6–15 representative EGFR immunofluorescence images in HEK293 cells overexpressing EGFR-GFP and UTR, and transfected with either control siRNA (panels 6–10) or β-arrestin 1/2 siRNA (panels 11–15). Cells were stimulated with UTII, EGFR, UR alone or UTII + UR. Each experiment was independently repeated 3–4 times. Scale bar 10 µm
To better determine the role of β-arrestin in EGFR trans-activation by the UTR, HEK293 cells transfected with EGFR-FLAG, UTR and β-arrestin-GFP were stimulated with UTII, EGF, UTII + UR or UR alone (Fig. 4d, panels 1–5). As expected, robust membrane translocation of β-arrestin-GFP was seen in cells stimulated with UTII (Fig. 4d, panel 2), while it was absent in cells treated with EGF, UTII + UR, or UR alone (Fig. 4d, panels 3–5). Next, HEK293 cells were transiently transfected with EGFR-GFP and UTR, and stimulated with UTII, with or without UR, or EGF. In the absence of agonist, EGFR had a uniform membrane distribution (Fig. 4d, panel 6). In contrast, UTII stimulation resulted in EGFR internalization as visualized by marked redistribution into cellular aggregates (Fig. 4d, panel 7). UTII-induced EGFR internalization was qualitatively similar to that evoked by EGF treatment (Fig. 4d, panel 8). UR treatment inhibited UTII-mediated EGFR internalization, while UR alone did not exert any effects on EGFR localization (Fig. 4d, panels 9–10). Importantly, siRNA knockdown of β-arrestin 1/2 completely blocked EGFR internalization induced by UTII, but not EGF (Fig. 4d, panels 11–15).
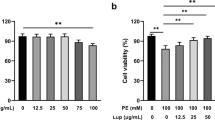
UTII or EGF reduce apoptotic cell death in vitro
Since β-arrestin–mediated signalling has been linked to the activation of protective signalling pathways [24], we next tested whether UTR-mediated GFR trans-activation would confer protection from apoptosis in smooth muscle-derived A10 cells (SMCs). In SMCs, UTII or EGF treatment significantly reduced apoptotic cell death induced by 24 h serum deprivation, as shown by TUNEL staining (Fig. 5a). In contrast, either UTR blockade by UR or EGFR inhibition by AG1478 abolished this protective effect. These results were confirmed also by Annexin V and propidium iodide double staining (Fig. 5b), and by the evaluation of caspase 3 activation (Fig. 5c). Taken together, these findings suggest that EGFR trans-activation by UTR may induce activation of cytoprotective pathways that are independent of classic G-protein-dependent signalling.
UTII reduces apoptotic cell death induced by serum deprivation. a Upper panels representative DAPI (top) and TUNEL (bottom) stainings of smooth muscle cells (SMCs) serum-starved for 24 h, then incubated with UR (30nM) or the EGFR inhibitor AG1478 (1μM) for 30 min, and next stimulated with UTII (100 nM) or EGF (10 ng/ml). After TUNEL staining, positive nuclei appear green (scale bar 100 µm). Bottom panel cumulative data of multiple independent experiments (*p < 0.05 vs. column 1; **p < 0.05 vs. columns 2, 4, 5, 7, 8). b Bar graphs showing % staining of Annexin V of serum-starved SMCs incubated with UR for 30 min, and next stimulated with UTII or EGF (*p < 0.05 vs. column 1; **p < 0.05 vs. columns 2, 4). c representative immunoblots (upper panels) and densitometric analysis (bottom panel) of multiple independent experiments to evaluate caspase 3 cleavage/activation in serum-starved SMCs incubated with UR for 30 min, and next stimulated with UTII or EGF alone (*p < 0.05 vs. column 1; **p < 0.05 vs. columns 2, 4). Tubulin levels did not significantly change among the samples
Discussion
This study shows that UTR-mediated signalling can exert beneficial effects in vitro, and confer cardioprotection in a model of cardiac pathological remodelling induced by pressure overload. In vivo trans-activation of the EGFR could be responsible for such protective effects, reducing apoptotic cell death and fibrosis induced by pressure overload.
UTII has been involved in several physiological and pathological processes, such as the regulation of vascular tone, cardiac contractility and rhythm [26]. The effects of UTII/UTR signalling on cardiac remodelling and function are currently controversial. Since patients with significantly elevated plasma UTII levels displayed improved outcomes post-myocardial infarction, it has been suggested that UTII may play a cardio-protective role in cardiac remodelling [20]. Consistent with these results, UTII has been shown to dilate coronary arteries, to reduce post-ischaemia creatin kinase and atrial natriuretic peptide release [22, 40], and to exert beneficial effects on diastolic function [15]. However, UTR blockade by SB-611812 has been previously reported to attenuate cardiac dysfunction in a rat model of coronary artery ligation, and to reduce the interstitial fibrosis within the non-infarcted zone of the left ventricle [3]. These contradictory results could be explained, at least in part, by the partial agonism of some antagonists, or by differences among the different antagonists in the ability to block EGFR trans-activation as previously shown for βAR blockers [21].
UTII administration has been shown to promote hypertrophy of rat neonatal cardiomyocytes [27], and potentiate cardiac hypertrophy induced by isoproterenol in vivo [49]. Interestingly, these effects seem to be mediated, at least in vitro, by EGFR trans-activation [27]. However, in this study UTII in vivo administration under conditions of pressure overload did not exert any additional effects on cardiac mass, function, structure or apoptosis (supplementary online Figure S2). Since pressure overload markedly induced endogenous UTII levels and UTR signalling (Fig. 1), it is not surprising that further exogenous UTII administration might not exert any additional effects. Moreover, UTR antagonism by UR did not reduce cardiac hypertrophy as recently reported by in a different model with a different UTR antagonist [23]. It is possible to speculate that inhibition of UTR signalling might not be sufficient to contrast the development of cardiac hypertrophy under conditions of pressure overload.
In this study, we show for the first time the important role of UTII signalling in EGFR trans-activation and cell fate in vivo. Currently, controversy exists as to the physiological role that 7TMR-mediated EGFR trans-activation plays in the heart. While there is evidence that angiotensin II–stimulated EGFR trans-activation can contribute to pathological hypertrophy [2, 44, 48], it is also known that the EGFR family member HER2 plays a protective role in the development of dilated cardiomyopathy [6]. Here we show that UTR–mediated signalling can exert beneficial effects in vitro, and confer cardio-protection in a mouse model of cardiac pathological remodelling induced by pressure overload. Trans-activation of the EGFR could be responsible for such protective effects during heart injury, as recently demonstrated for the β1AR [34]. Future studies will be needed to better define the precise molecular mechanisms by which the EGFR signals might positively influence cardiomyocyte function. Even if we did not directly assess βAR levels or signalling after UR treatment, UR did not affect cardiac levels of the β1AR kinase GRK2 (supplementary online Figure S3), suggesting that GRK2-dependent β1AR desensitization might not be involved in these processes.
Multiple mechanisms have been shown to connect 7TMRs and EGFR, including Src-mediated autocrine release of EGFR ligands such as HB-EGF [39], and the formation of 7TMR-EGFR signalling complexes [30]. Interestingly, EGFR trans-activation by UTR requires both β-arrestin 1 and 2, since elimination of either isoform in cells by siRNA prevented EGFR activation by UTII stimulation. This dual requirement might reflect distinct roles in the process played by each isoform, or perhaps the need for heterodimerization of β-arrestin 1 and 2, as previously demonstrated [43].
Our study has important therapeutic implications for the development of novel drugs for patients with heart failure, since all currently used drugs have been developed using assays only testing G-protein-dependent signals. Thus, while G-protein-mediated intracellular effects of UTII might be similar to those described for angiotensin II or endothelin-1 and detrimental [4, 8, 10, 31, 32], our present study shows that G-protein- independent signals triggered by UTII are protective under conditions of pressure overload. Indeed, it is now becoming increasingly clear that distinct conformations of activated 7TMRs are responsible for G-protein-dependent and β-arrestin-dependent signalling pathways [44, 46]. Based on these data, it is conceivable that new generation drugs might differentially or even exclusively activate or block one or another signalling mechanism by inducing specific conformations of a wild-type receptor, resulting in improved cardiac function and prognosis in heart failure.
In conclusion this study shows, for the first time in vivo, a new UTR signalling pathway which is mediated by EGFR trans-activation and that promotes cell survival and cardioprotection. These findings provide a mechanism for the role of UTII in cardiovascular responses to injury, and might identify novel therapeutic strategies in heart failure.
References
Ames RS, Sarau HM, Chambers JK, Willette RN, Aiyar NV, Romanic AM, Louden CS, Foley JJ, Sauermelch CF, Coatney RW, Ao Z, Disa J, Holmes SD, Stadel JM, Martin JD, Liu WS, Glover GI, Wilson S, McNulty DE, Ellis CE, Elshourbagy NA, Shabon U, Trill JJ, Hay DW, Ohlstein EH, Bergsma DJ, Douglas SA (1999) Human urotensin-II is a potent vasoconstrictor and agonist for the orphan receptor GPR14. Nature 401:282–286. doi:10.1038/45809
Asakura M, Kitakaze M, Takashima S, Liao Y, Ishikura F, Yoshinaka T, Ohmoto H, Node K, Yoshino K, Ishiguro H, Asanuma H, Sanada S, Matsumura Y, Takeda H, Beppu S, Tada M, Hori M, Higashiyama S (2002) Cardiac hypertrophy is inhibited by antagonism of ADAM12 processing of HB-EGF: metalloproteinase inhibitors as a new therapy. Nat Med 8:35–40. doi:10.1038/nm0102-35
Bousette N, Hu F, Ohlstein EH, Dhanak D, Douglas SA, Giaid A (2006) Urotensin-II blockade with SB-611812 attenuates cardiac dysfunction in a rat model of coronary artery ligation. J Mol Cell Cardiol 41:285–295. doi:10.1016/j.yjmcc.2006.05.008
Carneiro-Ramos MS, Diniz GP, Nadu AP, Almeida J, Vieira RL, Santos RA, Barreto-Chaves ML (2010) Blockage of angiotensin II type 2 receptor prevents thyroxine-mediated cardiac hypertrophy by blocking Akt activation. Basic Res Cardiol 105:325–335. doi:10.1007/s00395-010-0089-0
Chartrel N, Leprince J, Dujardin C, Chatenet D, Tollemer H, Baroncini M, Balment RJ, Beauvillain JC, Vaudry H (2004) Biochemical characterization and immunohistochemical localization of urotensin II in the human brainstem and spinal cord. J Neurochem 91:110–118. doi:10.1111/j.1471-4159.2004.02698.x
Crone SA, Zhao YY, Fan L, Gu Y, Minamisawa S, Liu Y, Peterson KL, Chen J, Kahn R, Condorelli G, Ross J Jr, Chien KR, Lee KF (2002) ErbB2 is essential in the prevention of dilated cardiomyopathy. Nat Med 8:459–465. doi:10.1038/nm0502-459
Curcio A, Noma T, Naga Prasad SV, Wolf MJ, Lemaire A, Perrino C, Mao L, Rockman HA (2006) Competitive displacement of phosphoinositide 3-kinase from beta-adrenergic receptor kinase-1 improves postinfarction adverse myocardial remodeling. Am J Physiol Heart Circ Physiol 291:H1754–H1760. doi:10.1152/ajpheart.01199.2005
d’Uscio LV, Moreau P, Shaw S, Takase H, Barton M, Luscher TF (1997) Effects of chronic ETA-receptor blockade in angiotensin II-induced hypertension. Hypertension 29:435–441
Daub H, Weiss FU, Wallasch C, Ullrich A (1996) Role of transactivation of the EGF receptor in signalling by G-protein-coupled receptors. Nature 379:557–560. doi:10.1038/379557a0
Diniz GP, Carneiro-Ramos MS, Barreto-Chaves ML (2009) Angiotensin type 1 receptor mediates thyroid hormone-induced cardiomyocyte hypertrophy through the Akt/GSK-3beta/mTOR signaling pathway. Basic Res Cardiol 104:653–667. doi:10.1007/s00395-009-0043-1
Dun SL, Brailoiu GC, Yang J, Chang JK, Dun NJ (2001) Urotensin II-immunoreactivity in the brainstem and spinal cord of the rat. Neurosci Lett 305:9–12. doi:10.1016/S0304-3940(01)01804-3
Esposito G, Perrino C, Ozaki T, Takaoka H, Defer N, Petretta MP, De Angelis MC, Mao L, Hanoune J, Rockman HA, Chiariello M (2008) Increased myocardial contractility and enhanced exercise function in transgenic mice overexpressing either adenylyl cyclase 5 or 8. Basic Res Cardiol 103:22–30. doi:10.1007/s00395-007-0688-6
Esposito G, Perrino C, Schiattarella GG, Belardo L, di Pietro E, Franzone A, Capretti G, Gargiulo G, Pironti G, Cannavo A, Sannino A, Izzo R, Chiariello M (2010) Induction of mitogen-activated protein kinases is proportional to the amount of pressure overload. Hypertension 55:137–143. doi:10.1161/HYPERTENSIONAHA.109.135467
Esposito G, Prasad SV, Rapacciuolo A, Mao L, Koch WJ, Rockman HA (2001) Cardiac overexpression of a G(q) inhibitor blocks induction of extracellular signal-regulated kinase and c-Jun NH(2)-terminal kinase activity in in vivo pressure overload. Circulation 103:1453–1458
Fontes-Sousa AP, Bras-Silva C, Pires AL, Monteiro-Sousa D, Leite-Moreira AF (2007) Urotensin II acutely increases myocardial length and distensibility: potential implications for diastolic function and ventricular remodeling. Naunyn Schmiedebergs Arch Pharmacol 376:107–115. doi:10.1007/s00210-007-0180-8
Hammoud L, Lu X, Lei M, Feng Q (2011) Deficiency in TIMP-3 increases cardiac rupture and mortality post-myocardial infarction via EGFR signaling: beneficial effects of cetuximab. Basic Res Cardiol doi:10.1007/s00395-010-0147-7
Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B (2005) ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation 112:e154–e235. doi:10.1161/CIRCULATIONAHA.105.167586
Iaccarino G, Tomhave ED, Lefkowitz RJ, Koch WJ (1998) Reciprocal in vivo regulation of myocardial G protein-coupled receptor kinase expression by beta-adrenergic receptor stimulation and blockade. Circulation 98:1783–1789
Indolfi C, Di Lorenzo E, Perrino C, Stingone AM, Curcio A, Torella D, Cittadini A, Cardone L, Coppola C, Cavuto L, Arcucci O, Sacca L, Avvedimento EV, Chiariello M (2002) Hydroxymethylglutaryl coenzyme A reductase inhibitor simvastatin prevents cardiac hypertrophy induced by pressure overload and inhibits p21ras activation. Circulation 106:2118–2124. doi:10.1161/01.CIR.0000034047.70205.97
Khan SQ, Bhandari SS, Quinn P, Davies JE, Ng LL (2007) Urotensin II is raised in acute myocardial infarction and low levels predict risk of adverse clinical outcome in humans. Int J Cardiol 117:323–328. doi:10.1016/j.ijcard.2006.05.016
Kim IM, Tilley DG, Chen J, Salazar NC, Whalen EJ, Violin JD, Rockman HA (2008) Beta-blockers alprenolol and carvedilol stimulate beta-arrestin-mediated EGFR transactivation. Proc Natl Acad Sci USA 105:14555–14560. doi:10.1073/pnas.0804745105
Klaiber M, Kruse M, Volker K, Schroter J, Feil R, Freichel M, Gerling A, Feil S, Dietrich A, Londono JE, Baba HA, Abramowitz J, Birnbaumer L, Penninger JM, Pongs O, Kuhn M (2010) Novel insights into the mechanisms mediating the local antihypertrophic effects of cardiac atrial natriuretic peptide: role of cGMP-dependent protein kinase and RGS2. Basic Res Cardiol 105:583–595. doi:10.1007/s00395-010-0098-z
Kompa AR, Wang BH, Phrommintikul A, Ho PY, Kelly DJ, Behm DJ, Douglas SA, Krum H (2010) Chronic urotensin II receptor antagonist treatment does not alter hypertrophy or fibrosis in a rat model of pressure-overload hypertrophy. Peptides 31:1523–1530. doi:10.1016/j.peptides.2010.04.026
Lefkowitz RJ, Shenoy SK (2005) Transduction of receptor signals by beta-arrestins. Science 308:512–517. doi:10.1126/science.1109237
Leineweber K, Bohm M, Heusch G (2006) Cyclic adenosine monophosphate in acute myocardial infarction with heart failure: slayer or savior? Circulation 114:365–367. doi:10.1161/CIRCULATIONAHA.106.642132
Lim M, Honisett S, Sparkes CD, Komesaroff P, Kompa A, Krum H (2004) Differential effect of urotensin II on vascular tone in normal subjects and patients with chronic heart failure. Circulation 109:1212–1214. doi:10.1161/01.CIR.0000121326.69153.98
Liu JC, Chen CH, Chen JJ, Cheng TH (2009) Urotensin II induces rat cardiomyocyte hypertrophy via the transient oxidization of Src homology 2-containing tyrosine phosphatase and transactivation of epidermal growth factor receptor. Mol Pharmacol 76:1186–1195. doi:10.1124/mol.109.05829
Liu Y, Yang XM, Iliodromitis EK, Kremastinos DT, Dost T, Cohen MV, Downey JM (2008) Redox signaling at reperfusion is required for protection from ischemic preconditioning but not from a direct PKC activator. Basic Res Cardiol 103:54–59. doi:10.1007/s00395-007-0683-y
Matsushita M, Shichiri M, Imai T, Iwashina M, Tanaka H, Takasu N, Hirata Y (2001) Co-expression of urotensin II and its receptor (GPR14) in human cardiovascular and renal tissues. J Hypertens 19:2185–2190. doi:10.1097/00004872-200112000-00011
Maudsley S, Pierce KL, Zamah AM, Miller WE, Ahn S, Daaka Y, Lefkowitz RJ, Luttrell LM (2000) The beta(2)-adrenergic receptor mediates extracellular signal-regulated kinase activation via assembly of a multi-receptor complex with the epidermal growth factor receptor. J Biol Chem 275:9572–9580. doi:10.1074/jbc.275.13.9572
Mederos y Schnitzler M, Storch U, Meibers S, Nurwakagari P, Breit A, Essin K, Gollasch M, Gudermann T (2008) Gq-coupled receptors as mechanosensors mediating myogenic vasoconstriction. EMBO J 27:3092–3103. doi:10.1038/emboj.2008.233
Morris GE, Nelson CP, Standen NB, Challiss RA, Willets JM (2010) Endothelin signalling in arterial smooth muscle is tightly regulated by G protein-coupled receptor kinase 2. Cardiovasc Res 85:424–433. doi:10.1093/cvr/cvp310
Mozaffari MS, Baban B, Liu JY, Abebe W, Sullivan JC, El-Marakby (2011) A Mitochondrial complex I and NAD(P)H oxidase are major sources of exacerbated oxidative stress in pressure-overloaded ischemic-reperfused hearts. Basic Res Cardiol doi:10.1007/s00395-011-0150-7
Noma T, Lemaire A, Naga Prasad SV, Barki-Harrington L, Tilley DG, Chen J, Le Corvoisier P, Violin JD, Wei H, Lefkowitz RJ, Rockman HA (2007) Beta-arrestin-mediated beta1-adrenergic receptor transactivation of the EGFR confers cardioprotection. J Clin Invest 117:2445–2458. doi:10.1172/JCI31901
Onan D, Pipolo L, Yang E, Hannan RD, Thomas WG (2004) Urotensin II promotes hypertrophy of cardiac myocytes via mitogen-activated protein kinases. Mol Endocrinol 18:2344–2354. doi:10.1210/me.2003-0309
Penna C, Tullio F, Perrelli MG, Moro F, Abbadessa G, Piccione F, Carriero V, Racca S, Pagliaro P (2010) Ischemia/reperfusion injury is increased and cardioprotection by a postconditioning protocol is lost as cardiac hypertrophy develops in nandrolone treated rats. Basic Res Cardiol doi:10.1007/s00395-010-0143-y
Perrino C, Naga Prasad SV, Mao L, Noma T, Yan Z, Kim HS, Smithies O, Rockman HA (2006) Intermittent pressure overload triggers hypertrophy-independent cardiac dysfunction and vascular rarefaction. J Clin Invest 116:1547–1560. doi:10.1172/JCI25397
Perrino C, Naga Prasad SV, Schroder JN, Hata JA, Milano C, Rockman HA (2005) Restoration of beta-adrenergic receptor signaling and contractile function in heart failure by disruption of the betaARK1/phosphoinositide 3-kinase complex. Circulation 111:2579–2587. doi:10.1161/CIRCULATIONAHA.104.508796
Prenzel N, Zwick E, Daub H, Leserer M, Abraham R, Wallasch C, Ullrich A (1999) EGF receptor transactivation by G-protein-coupled receptors requires metalloproteinase cleavage of proHB-EGF. Nature 402:884–888. doi:10.1038/47260
Prosser HC, Forster ME, Richards AM, Pemberton CJ (2008) Urotensin II and urotensin II-related peptide (URP) in cardiac ischemia-reperfusion injury. Peptides 29:770–777. doi:10.1016/j.peptides.2007.08.013
Rockman HA, Koch WJ, Lefkowitz RJ (2002) Seven-transmembrane-spanning receptors and heart function. Nature 415:206–212. doi:10.1038/415206a
Shah BH, Catt KJ (2004) Matrix metalloproteinase-dependent EGF receptor activation in hypertension and left ventricular hypertrophy. Trends Endocrinol Metab 15:241–243. doi:10.1016/j.tem.2004.06.011
Storez H, Scott MG, Issafras H, Burtey A, Benmerah A, Muntaner O, Piolot T, Tramier M, Coppey-Moisan M, Bouvier M, Labbe-Jullie C, Marullo S (2005) Homo- and hetero-oligomerization of beta-arrestins in living cells. J Biol Chem 280:40210–40215. doi:10.1074/jbc.M50800120
Thomas WG, Brandenburger Y, Autelitano DJ, Pham T, Qian H, Hannan RD (2002) Adenoviral-directed expression of the type 1A angiotensin receptor promotes cardiomyocyte hypertrophy via transactivation of the epidermal growth factor receptor. Circ Res 90:135–142. doi:10.1161/hh0202.104109
Tuxworth WJ, Jr, Shiraishi H, Moschella PC, Yamane K, McDermott PJ, Kuppuswamy D (2008) Translational activation of 5’-TOP mRNA in pressure overload myocardium. Basic Res Cardiol 103:41–53. doi:10.1007/s00395-007-0682-z
Violin JD, Lefkowitz RJ (2007) Beta-arrestin-biased ligands at seven-transmembrane receptors. Trends Pharmacol Sci 28:416–422. doi:10.1016/j.tips.2007.06.006
Wenzel S, Henning K, Habbig A, Forst S, Schreckenberg R, Heger J, Maxeiner H, Schluter KD (2010) TGF-beta1 improves cardiac performance via up-regulation of laminin receptor 37/67 in adult ventricular cardiomyocytes. Basic Res Cardiol 105:621–629. doi:10.1007/s00395-010-0108-1
Yoshioka J, Prince RN, Huang H, Perkins SB, Cruz FU, MacGillivray C, Lauffenburger DA, Lee RT (2005) Cardiomyocyte hypertrophy and degradation of connexin43 through spatially restricted autocrine/paracrine heparin-binding EGF. Proc Natl Acad Sci USA 102:10622–10627. doi:10.1073/pnas.0501198102
Zhang YG, Li YG, Liu BG, Wei RH, Wang DM, Tan XR, Bu DF, Pang YZ, Tang CS (2007) Urotensin II accelerates cardiac fibrosis and hypertrophy of rats induced by isoproterenol. Acta Pharmacol Sin 28:36–43. doi:10.1111/j.1745-7254.2007.00485.x
Zhu YC, Zhu YZ, Moore PK (2006) The role of urotensin II in cardiovascular and renal physiology and diseases. Br J Pharmacol 148:884–901. doi:10.1038/sj.bjp.070680
Acknowlegements
This work has been supported by the grant PRIN 2007 (No. 2007WS3JL3) from the Ministero dell’Università e della Ricerca Scientifica to M.C.; Cinzia Perrino MD PhD has been supported, in part, by a Grant “L’Oreal—Italia—For women in Science 2008”. The authors kindly thank Dr. Howard A. Rockman (Duke University, Durham NC) for supplying the EGFR-FLAG, EGFR-GFP, β-arrestin-GFP plasmids. This paper is dedicated to the memory of Professor Massimo Chiariello MD, passed away on March 23rd 2010.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
G. Esposito and C. Perrino equally contributed to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Esposito, G., Perrino, C., Cannavo, A. et al. EGFR trans-activation by urotensin II receptor is mediated by β-arrestin recruitment and confers cardioprotection in pressure overload-induced cardiac hypertrophy. Basic Res Cardiol 106, 577–589 (2011). https://doi.org/10.1007/s00395-011-0163-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00395-011-0163-2