Abstract
Redox signaling prior to a lethal ischemic insult is an important step in triggering the protected state in ischemic preconditioning. When the preconditioned heart is reperfused a second sequence of signal transduction events, the mediator pathway, occurs which is believed to inhibit mitochondrial permeability transition pore formation that normally destroys mitochondria in much of the reperfused tissue. Prominent among the mediator pathway’s events is activation of phosphatidylinositol 3-kinase and extracellular signal-regulated kinase. Recently it was found that both activation of PKC and generation of reactive oxygen species (ROS) at the time of reperfusion are required for protection in preconditioned hearts. To establish their relative order we tested whether ROS formation at reperfusion is required in hearts protected by direct activation of PKC at reperfusion. Isolated rabbit hearts were exposed to 30 min of regional ischemia and 2 h of reperfusion. Preconditioned hearts received 5 min of global ischemia and 10 min of reperfusion prior to the index ischemia. Another group of preconditioned hearts was exposed to 300 µM of the ROS scavenger N-(2-mercaptopropionyl) glycine (MPG) for 20 min starting 5 min prior to reperfusion. Infarct size was measured by triphenyltetrazolium staining. Preconditioning reduced infarct size from 36% ± 2% of the ischemic zone in control hearts to only 18 ± 2%. MPG during early reperfusion completely blocked preconditioning’s protection (33 ± 3% infarction). MPG given in the same dose and schedule to non-preconditioned hearts had no effect on infarct size. In the last group phorbol 12-myristate 13-acetate (PMA) (0.05 nM) was given to non-preconditioned hearts from 1 min before to 5 min after reperfusion in addition to MPG administered as in the other groups. MPG did not block protection from an infusion of PMA as infarct size was only 9 ± 2% of the risk zone. We conclude that while redox signaling during the first few minutes of reperfusion is an essential component of preconditioning’s protective mechanism, this step occurs upstream of PKC activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In 1997 we [2] as well as Tritto et al. [25] reported that reactive oxygen species (ROS) were involved in the triggering of ischemic preconditioning (IPC). Later it was found that ROS were generated as a result of opening of mitochondrial ATP-sensitive potassium channels (mKATP) and acted as second messengers in a pathway ending in activation of PKC, which triggered the preconditioned state [21]. In those studies ROS were recognized as part of the trigger pathway that preconditions the heart prior to the onset of the index ischemia. Several years ago it was discovered that IPC actually exerts its protective effect in the first minutes of reperfusion [9] presumably by inhibiting the formation of mitochondrial permeability transition pores (mPTP) [11]. Then it was found that redox signaling is part of the pathway that mediates IPC’s protection at the time of reperfusion as well. Penna et al. [22] reported that ROS generation was required for ischemic postconditioning to be protective. The finding that ROS could carry a protective signal at the same time that ROS were thought to be inducing reperfusion injury was very surprising [7]. But then Hausenloy et al. [10] reported that a ROS scavenger given immediately following the index ischemia also blocked IPC’s protection. These observations again illustrated similarities of the mechanisms of protection of IPC and postconditioning.
It is unknown how redox signaling acts to mediate protection at reperfusion. A number of signal transduction components have been identified in IPC’s mediator pathway including phosphatidylinositol (PI) 3-kinase and extracellular signal-regulated kinase (ERK) [9]. Additionally PKC must be activated at reperfusion [10, 16, 22] and adenosine A2b receptors must be occupied [16]. Hausenloy and colleagues [10] have speculated that the order of these components was first PKC activation followed in order by occupancy of adenosine receptors, activation of the survival kinases PI3-kinase and ERK, opening of mKATP, and generation of ROS and finally ending with inhibition of mPTP formation. In the present study we tested that order by directly activating PKC with phorbol 12-myristate 13-acetate (PMA), which we have previously shown mimics IPC when given at reperfusion [16] in a PKC-dependent fashion [23]. If redox signaling is downstream of PKC as Hausenloy et al. [10] have proposed, then a ROS scavenger should block protection resulting from PKC activation.
2 Methods
2.1 Surgical preparation
All animal care satisfied published guidelines [20] and procedures were approved by institutional committees. Briefly, New Zealand White rabbits were anesthetized with pentobarbital sodium (30 mg/kg i.v.) and ventilated with 100% oxygen. The heart was exposed and a suture was passed around a coronary arterial branch. The heart was excised and perfused on a Langendorff apparatus with Krebs-Henseleit bicarbonate buffer bubbled with 95% O2/5% CO2 to a pH of 7.35–7.45 at 38°C. A fluid-filled latex balloon measured pressure in the left ventricle.
2.2 Experimental protocol
Hearts of 6 experimental groups underwent 30-min coronary branch occlusion/2-h reperfusion. Control hearts had no other intervention. IPC hearts were preconditioned with 5-min global ischemia/10-min reperfusion prior to the index ischemia. In group 3 IPC hearts received N-(2-mercaptopropionyl) glycine (MPG, 300 µM) for 20 min starting 5 min before reperfusion. In the fourth group MPG was given in the same dose and schedule to non-preconditioned hearts. In the fifth group PMA (0.05 nM) was given from 1 min before to 5 min after reperfusion, and in group 6 PMA was similarly administered in addition to MPG as in groups 3 and 4. The dose of PMA was selected empirically as one that was known to confer protection [18]; and because that protection could be blocked by chelerythrine [16] the dependence of PMA’s protective effect on PKC was assured. It should be noted that group 4, a control group of MPG alone, was not contemporary but rather was from a previous study in our laboratory [5].
2.3 Measurement of risk zone and infarct size
At the end of the experiments the coronary artery was reoccluded, and 2–9 µm fluorescent microspheres (Microgenics Corp., Freemont, CA) were infused to demarcate the non-fluorescent risk zone. The heart was cut into 2-mm-thick slices that were incubated in 1% triphenyltetrazolium chloride to stain noninfarcted tissue. Areas of infarct and risk zone were determined by planimetry of each slice and volumes calculated. Infarction is expressed as a percentage of the region at risk.
2.4 Statistics
Infarct sizes were compared with one-way ANOVA, and post hoc pairwise comparisons done with Student–Newman–Keuls test. P < 0.05 was considered to be significant.
3 Results
Hemodynamics are presented in Table 1. There were no significant baseline group differences. Coronary occlusion caused significant decreases in left ventricular developed pressure and coronary flow in all groups. There was partial recovery following reperfusion.
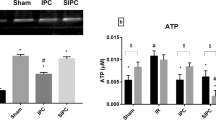
Infarct size data appear in Fig. 1. Thirty minutes of regional ischemia and 2 h of reperfusion resulted in 17.6 ± 1.7% infarction of the risk zone in IPC hearts, which was significantly smaller than 36.4 ± 1.7% infarction seen in non-preconditioned hearts (P < 0.001). When IPC hearts were reperfused in the presence of MPG, infarct size increased to 32.6 ± 3.4% of the risk zone indicating that IPC’s protection had been blocked. MPG in a non-preconditioned heart had no effect on infarct size (37.0 ± 2.3% infarction). The pulse of PMA fully protected the hearts (6.8 ± 1.0% infarction) and MPG did not block PMA’s protection as infarct size was only 9.2 ± 1.5% of the risk zone. Interestingly infarct size in the two PMA groups was significantly smaller than that in the IPC group (P < 0.002).
4 Discussion
We were able to confirm the observation of Hausenloy et al. [10] that ROS production early in reperfusion is required for IPC’s protection in our rabbit model. Our data also indicate that the protection from a direct PKC activator is independent of ROS production suggesting that the ROS step occurs upstream of the PKC step. Through the use of inhibitors PKC activity early in reperfusion has been shown to be required for protection against infarction from both IPC [10, 16] and postconditioning [22, 23]. Furthermore, the direct PKC activator PMA given at reperfusion mimics IPC’s protection [16, 23] and this protection is blocked by chelerythrine verifying that PMA protected in a PKC-dependent manner [23].
Our previous data indicate that the adenosine A2b receptor resides downstream of PKC in the mediator pathway because at reperfusion an A2b receptor antagonist blocks protection from PMA but the PKC blocker chelerythrine does not block protection from an A2b agonist [16, 23]. We found that PKC activity lowers the threshold for A2b agonists to activate the survival kinases suggesting that in the IPC heart the increased sensitivity allows endogenous adenosine to activate protective signaling through the normally low-affinity A2b receptors [16]. Accordingly we were able to demonstrate that PI3-kinase and ERK activity is dependent on population of adenosine receptors since receptor inhibition at reperfusion blocked survival kinase activation in IPC hearts [24]. Also, protection from PMA at reperfusion could be blocked by the PI3-kinase blocker wortmannin [23]. Taken together this information now allows us to propose a revised arrangement for the sequence of signal transduction elements for the mediator pathway. In our new order we start with ROS followed in sequence by PKC, A2b receptors, and survival kinases leading to inhibition of mPTP (Fig. 2).
Costa et al. [6] found that mKATP openers protected isolated mitochondria from Ca++-induced mPTP formation. That protection was both ROS- and PKC-sensitive. Furthermore they could show that ROS protected by activation of PKC. Because these were isolated mitochondria they concluded that once the mKATP opened all of the signal transduction elements required to inhibit mPTP formation were present within the mitochondria. The present findings are in agreement with some of the observations made by Costa et al. [6] Protection from PMA does not require ROS and is therefore downstream of the ROS signal. However, PMA’s protection requires both adenosine receptor occupancy as well as PI3-kinase activation [23] indicating that in a whole heart protection from a direct PKC activator still requires signals that arise from outside the mitochondria. We have no explanation for this apparent discrepancy.
The protection from PMA was significantly more potent than that from IPC. While IPC is thought to selectively activate a single isoform of PKC (perhaps ɛ), PMA is not selective for any isoform and may have activated additional isoforms to provide more protection. Alternatively the single IPC protocol we used may not have fully preconditioned our hearts. PMA also reduced coronary flow and contractility. The reduced coronary flow could have ischemically preconditioned the hearts, but if that were the case MPG should have blocked it. Although PMA was present in the perfusate for about a minute before reperfusion it would not have appreciably entered the ischemic tissue until the artery was reperfused because of sparse collateralization in the rabbit heart.
Our data do not provide information about the location of the mKATP channel in the signaling cascade. In a recent study Gross et al. [8] gave the mKATP opener BMS-191095 just prior to reperfusion in open-chest rats and were able to mimic IPC’s anti-infarct effect. Moreover they could block BMS-191095’s protection with the PI3-kinase inhibitor wortmannin thus putting mKATP ahead of PI3-kinase. The most likely place for mKATP to reside would be ahead of the ROS step. IPC’s trigger pathway has been extensively studied and in that pathway we [15, 21] and others [1] have found that potassium entry from mKATP opening results in ROS production by the mitochondria. Thus the mediator pathway could simply look like IPC’s trigger pathway with mKATP opening resulting in ROS production. This suggestion does not fit all of the data, however. In a cardiomyocyte model Lebuffe et al. [17] found that they could protect cells against simulated ischemia with either PMA or hydrogen peroxide and that the mKATP blocker 5-hydroxydecanoate blocked protection from both. That would put the mKATP channel downstream of ROS and PKC. Juhaszova et al. [13] also were confronted with discrepant data about the location of mKATP in their flowchart and decided that the data warranted a dual location, one upstream of the ROS step and another downstream near mPTP, and we have also done that in Fig 2.
How do we explain the apparent coexistence of a protective free radical signal and the very injurious free radical burst that is supposed to occur in the reperfused heart [3]? Most observers have noted that IPC does not increase but actually reduces overall ROS production in reperfused hearts [26]. The most likely explanation is that the ROS signal is carried by one specific radical species and/or in one intracellular compartment. MPG obviously is able to scavenge the radical species that signals the protection. MPG is a very selective scavenger for hydroxyl radical and peroxynitrite and does not affect superoxide or hydrogen peroxide [4]. We also have unpublished measurements showing that MPG does not scavenge nitric oxide. In addition MPG reportedly concentrates 500-fold in mitochondria making it highly effective against mitochondria-generated ROS [19]. Protection from preconditioning with a ROS generator is known to be PKC-dependent [2, 25], and indeed Korichneva et al. [14] found that ROS could directly activate PKC in vitro by reacting with its thiol groups. Thus hydroxyl radical made by mitochondria could directly activate local PKC independent of the other injurious ROS species generated during reperfusion. The simplest explanation for our observation is that hydroxyl radical made by the IPC heart’s mitochondria early in reperfusion protects by activating PKC. It is currently unknown why that activation fails to occur in the non-IPC heart.
References
Andrukhiv A, Costa AD, West IC, Garlid KD (2006) Opening mitoKATP increases superoxide generation from complex I of the electron transport chain. Am J Physiol 291:H2067–H2074
Baines CP, Goto M, Downey JM (1997) Oxygen radicals released during ischemic preconditioning contribute to cardioprotection in the rabbit myocardium. J Mol Cell Cardiol 29:207–216
Bolli R (1990) Mechanism of myocardial “stunning”. Circulation 82:723–738
Bolli R, Jeroudi MO, Patel BS, Aruoma OI, Halliwell B, Lai EK, McCay PB (1989) Marked reduction of free radical generation and contractile dysfunction by antioxidant therapy begun at the time of reperfusion: evidence that myocardial “stunning” is a manifestation of reperfusion injury. Circ Res 65:607–622
Cohen MV, Yang X-M, Downey JM (2007) The pH hypothesis of postconditioning: staccato reperfusion reintroduces oxygen and perpetuates myocardial acidosis. Circulation 115:1895–1903
Costa ADT, Jakob R, Costa CL, Andrukhiv K, West IC, Garlid KD (2006) The mechanism by which the mitochondrial ATP-sensitive K+ channel opening and H2O2 inhibit the mitochondrial permeability transition. J Biol Chem 281:20801–20808
Downey JM, Cohen MV (2006) A really radical observation: a comment on Penna et al. in Basic Res Cardiol (2006) 101:180–189. Basic Res Cardiol 101:190–191
Gross ER, Hsu AK, Gross GJ (2007) GSK3β inhibition and KATP channel opening mediate acute opioid-induced cardioprotection at reperfusion. Basic Res Cardiol 102:341–349
Hausenloy DJ, Tsang A, Mocanu MM, Yellon DM (2005) Ischemic preconditioning protects by activating prosurvival kinases at reperfusion. Am J Physiol 288:H971–H976
Hausenloy DJ, Wynne AM, Yellon DM (2007) Ischemic preconditioning targets the reperfusion phase. Basic Res Cardiol 102:445–452
Hausenloy DJ, Yellon DM, Mani-Babu S, Duchen MR (2004) Preconditioning protects by inhibiting the mitochondrial permeability transition. Am J Physiol 287:H841–H849
Iliodromitis EK, Liu Y, Kremastinos DT, Cohen MV, Downey JM (2007) Redox signaling at reperfusion is required for ischemic preconditioning’s protection. Eur Heart J 28(Abst Suppl):360
Juhaszova M, Zorov DB, Kim S-H, Pepe S, Fu Q, Fishbein KW, Ziman BD, Wang S, Ytrehus K, Antos CL, Olson EN, Sollott SJ (2004) Glycogen synthase kinase-3β mediates convergence of protection signaling to inhibit the mitochondrial permeability transition pore. J Clin Invest 113:1535–1549
Korichneva I, Hoyos B, Chua R, Levi E, Hammerling U (2002) Zinc release from protein kinase C as the common event during activation by lipid second messenger or reactive oxygen. J Biol Chem 277:44327–44331
Krenz M, Oldenburg O, Wimpee H, Cohen MV, Garlid KD, Critz SD, Downey JM, Benoit JN (2002) Opening of ATP-sensitive potassium channels causes generation of free radicals in vascular smooth muscle cells. Basic Res Cardiol 97:365–373
Kuno A, Critz SD, Cui L, Solodushko V, Yang X-M, Krahn T, Albrecht B, Philipp S, Cohen MV, Downey JM (2007) Protein kinase C protects preconditioned rabbit hearts by increasing sensitivity of adenosine A2b-dependent signaling during early reperfusion. J Mol Cell Cardiol 43:262–271
Lebuffe G, Schumacker PT, Shao Z-H, Anderson T, Iwase H, Vanden Hoek TL (2003) ROS and NO trigger early preconditioning:relationship to mitochondrial KATP channel. Am J Physiol 284:H299–H308
Liu Y, Ytrehus K, Downey JM (1994) Evidence that translocation of protein kinase C is a key event during ischemic preconditioning of rabbit myocardium. J Mol Cell Cardiol 26:661–668
Nadtochiy SM, Burwell LS, Brookes PS (2007) Cardioprotection and mitochondrial S-nitrosation: effects of S-nitroso-2-mercaptopropionyl glycine (SNO-MPG) in cardiac ischemia-reperfusion injury. J Mol Cell Cardiol 42:812–825
National Research Council (1996) Guide for the care and use of laboratory animals, 7th edn. National Academy Press, Washington
Pain T, Yang X-M, Critz SD, Yue Y, Nakano A, Liu GS, Heusch G, Cohen MV, Downey JM (2000) Opening of mitochondrial KATP channels triggers the preconditioned state by generating free radicals. Circ Res 87:460–466
Penna C, Rastaldo R, Mancardi D, Raimondo S, Cappello S, Gattullo D, Losano G, Pagliaro P (2006) Post-conditioning induced cardioprotection requires signaling through a redox-sensitive mechanism, mitochondrial ATP-sensitive K+ channel and protein kinase C activation. Basic Res Cardiol 101:180–189
Philipp S, Yang X-M, Cui L, Davis AM, Downey JM, Cohen MV (2006) Postconditioning protects rabbit hearts through a protein kinase C-adenosine A2b receptor cascade. Cardiovasc Res 70:308–314
Solenkova NV, Solodushko V, Cohen MV, Downey JM (2006) Endogenous adenosine protects preconditioned heart during early minutes of reperfusion by activating Akt. Am J Physiol 290:H441–H449
Tritto I, D’Andrea D, Eramo N, Scognamiglio A, De Simone C, Violante A, Esposito A, Chiariello M, Ambrosio G (1997) Oxygen radicals can induce preconditioning in rabbit hearts. Circ Res 80:743–748
Vanden Hoek TL, Becker LB, Shao Z-H, Li C-Q, Schumacker PT (2000) Preconditioning in cardiomyocytes protects by attenuating oxidant stress at reperfusion. Circ Res 86:541–548
Acknowledgments
This work was supported in part by grants HL-20468 and HL-50688 from the Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Dost is supported by a grant from the Turkish Scientific and Technical Research Council (TUBITAK). A preliminary report of these data was presented as an abstract at the 2007 European Society of Cardiology meeting in Vienna [12].
Author information
Authors and Affiliations
Corresponding author
Additional information
Returned for 1. revision: 29 August 20071. Revision received: 19 September 2007
Rights and permissions
About this article
Cite this article
Liu, Y., Yang, XM., Iliodromitis, E.K. et al. Redox signaling at reperfusion is required for protection from ischemic preconditioning but not from a direct PKC activator. Basic Res Cardiol 103, 54–59 (2008). https://doi.org/10.1007/s00395-007-0683-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00395-007-0683-y