Abstract
Objective
To evaluate the regulation of matrix metalloproteinase (MMP)-2 in diabetic cardiomyopathy.
Methods
Left ventricle (LV) function was determined by a micro-tip catheter in streptozotocin (STZ)-induced diabetic rats, 2 or 6 weeks (w) after STZ-application. LV total collagen, collagen type I and III content were immunohistologically analyzed and quantified by digital image analysis. LV collagen type I, III and MMP-2 mRNA expression was quantified by real-time RT-PCR. LV pro- and active MMP-2 levels were analyzed by zymography; Smad 7, membrane type (MT)1-MMP and tissue inhibitor metalloproteinase (TIMP)-2 protein levels by Western Blot.
Results
STZ-induced diabetes was associated with a time-dependent impairment of LV diastolic and systolic function. This was paralleled by a time-dependent increase in LV total collagen content, despite reduced LV collagen type I and III mRNA levels, indicating a role of post-transcriptional/post-translational changes of extracellular matrix regulation. Six weeks (w) after STZ-injection, MMP-2 mRNA expression and pro-MMP-2 levels were 2.7-fold (P < 0.005) and 1.3-fold (P < 0.05) reduced versus controls, respectively, whereas active MMP-2 was decreased to undetectable levels 6 w post-STZ. Concomitantly, Smad 7 and TIMP-2 protein levels were 1.3-fold (P < 0.05) and 10-fold (P < 0.005) increased in diabetics versus controls, respectively, whereas the 45 kDa form of MT1-MMP was undetectable in diabetics.
Conclusion
Under STZ-diabetic conditions, cardiac fibrosis is associated with a dysregulation in extracellular matrix degradation. This condition is featured by reduced MMP-2 activity, concomitant with increased Smad 7 and TIMP-2 and decreased MT1-MMP protein expression, which differs from mechanisms involved in dilated and ischemic heart disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Several studies have shown that dysregulation in the degradation of the extracellular matrix (ECM) by matrix metalloproteinases (MMPs), specifically MMP-2 and MMP-9, is involved in the pathogenesis of a wide spectrum of cardiovascular disorders, including atherosclerosis, restenosis, congestive heart failure, myocardial infarction and cardiomyopathy [1, 11, 15, 21]. Diabetic cardiomyopathy is a multifactorial condition associated with a change of myocardial extracellular matrix (interstitial and perivascular fibrosis), interstitial inflammation, an activated cardiac renin-angiotensin-system, oxidative stress, impaired Ca2+-homeostasis and endothelial dysfunction, leading to impaired cardiac ventricular function [34, 37, 38, 44]. In diabetic cardiomyopathy, cardiac fibrosis [39] has recently been shown to be associated with a decrease in MMP-2 expression/activity [8, 43], whereas MMP-9 expression was found to be unchanged [8] or increased [43]. Glucose and angiotensin II, 2 factors associated with diabetic cardiomyopathy, reduce MMP activity in cultured fibroblasts [4].
The decrease in MMP-2 activity in the diabetic heart, which might contribute to the increased accumulation of collagen in the diabetic heart, triggered us to further investigate its regulation. Besides others, MMP-2 digests type I, II, and III collagen [2], important for left ventricular diastolic and systolic performance. Moreover, MMP-2 has recently been shown to be a direct mediator of ventricular remodelling and systolic dysfunction [6]. Similar to other members of the metalloproteinase family, MMP-2 is secreted in a latent form (pro-MMP-2) requiring proteolytic processing in order to become catalytically active [11]. The main activation of pro-MMP-2 takes place on the cell surface and is mediated by membrane type (MT)-MMPs, including MT1-MMP (MMP-14) [27], whereas the proteolytic activity of MMP-2 can be inhibited by binding of tissue inhibitor metalloproteinase (TIMP)-2 to the active catalytic domain of MMP-2. Moreover, the expression of MMP-2 is known to be increased by TGF-β1 signaling [16], of which Smad 7 is an intracellular antagonist [45].
However, the regulation of MMP-2 in different cardiac disorders is less well understood. We further characterized MMP-2 regulation under experimental diabetic conditions to investigate the hypothesis whether MMP-2 dysregulation may be among the mechanisms involved in the development of fibrosis in diabetic cardiomyopathy.
2 Materials and methods
2.1 Animals
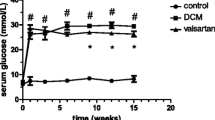
Eight weeks old male Sprague Dawley (SD) rats (300–330 g, Charles River) were maintained on a 12 h light/dark cycle and fed with a standard chow ad libitum (n = 8/group). Diabetes mellitus (DM) was induced by a single injection of streptozotocin (STZ; 70 mg/kg; i.p.) prepared in 0.1 M sodium citrate buffer, pH 4.5 (Sigma, Munich, Germany) as described in detail previously [39]. The STZ-model using 70 mg/kg i.p. is a well established model to study diabetic cardiomyopathy [7, 37–39]. Insulin supplementation in animals injected with this dose of STZ leads to an improvement of left ventricle (LV) function, indicating the role of hyperglycemia in cardiac dysfunction in this model [28]. Only rats with blood glucose levels ≥300 mg/dl 5 days after STZ injection were used in the study. Age-matched non-diabetic SD rats were injected with sodium citrate buffer and used as controls. Rats were sacrificed 2 weeks (w) and 6 w after STZ-injection. Non-diabetic control rats were sacrificed 6 w after sodium citrate buffer injection. The investigation conforms with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85–23, revised 1996) and is approved by the Ethical Committee for the Use of Experimental Animals of the Charité, Berlin (Germany).
2.2 Hemodynamic characterization
The animals were anesthetized with sodium pentobarbital (60 mg/kg; ip), intubated and artificially ventilated. A 2F micro pressure Tip-catheter (Millar Instruments Inc., Houston, Texas, USA) was positioned in the LV via the right carotid artery as previously described [39]. Indices of systolic and diastolic cardiac performance were derived from LV pressure-data. LV systolic function was quantified by the end-systolic pressure (LVP) and the peak rate of rise in left ventricular pressure (dP/dt max). LV diastolic function was measured by end-diastolic pressure (LVEDP), peak dP/dt min and the time constant of isovolumic pressure relaxation (tau). Furthermore, the heart rate (HR) was determined by customized software.
2.3 Tissue preparation
After hemodynamic characterization, the hearts were excised, and circa 2 mm thick transverse sections of the hearts were rapidly frozen in liquid nitrogen and stored at -80°C for immunohistology and molecular biology purposes. A further section was paraffin embedded for Sirius Red staining.
2.4 Sirius Red staining
Total collagen content of the Sirius Red (Polyscience, Inc, Warrington, PA) stained sections was measured under circularly polarized light according to previously published methods [21] and quantified by digital image analysis (DIA) as described in detail elsewhere [39]. Perivascular fibrosis was not analyzed. All available fields (>30 fields) were measured, including the septum, the right and the left ventricle.
2.5 Immunohistology
Immunohistological staining was carried out with rabbit anti-collagen subtype I and III- and anti-pan-specific TGF-ß antibodies and quantified by DIA as described in detail elsewhere [39]. All available fields (>30 fields) were measured, including the septum, the right and the left ventricles. Data are represented as area fraction.
2.6 Real-time RT-PCR
Quantitative real-time reverse transcriptase (RT)-PCR (ABI PRISM® 7000 Sequence Detection System software version 1.0., Perkin Elmer) was performed to quantify LV rat collagen (Col) I, Col III, MMP-2 and MMP-9 cDNA levels, which were normalized relative towards the L32 housekeeping gene and multiplied by 10. Overview of the forward and reverse primers used is shown in Table 1. As DNA standards, the products of the conventional PCR for rat Col I, Col III, MMP-2, MMP-9 and L32 with the use of the primers designed for real-time PCR, were cloned into pGEM-T Easy vector (Promega).
2.7 Gelatin zymography
Frozen adult rat myocardial tissue samples were homogenized in 5 x volumes of extraction buffer containing: 10 mmol/l cacodylic acid, pH 5.0, 0.15 mol/l NaCl, 1 µmol/l ZnCl2, 20 mmol/l CaCl2, 1.5 mmol/l NaN3, and 0.01% (v/v) Triton X-100 at 4°C overnight. Protein samples (50 µg) were mixed with loading buffer lacking reducing agents (10% w/v SDS, 4% w/v sucrose, 0.1% w/v bromophenol blue) and applied without boiling to 10% SDS/polyacrylamide gel containing 1 mg/ml of gelatin B and separated by gelelectrophoresis. Supernatant of HT 1080 (10 µl), human fibrosarcoma cells, served as positive control. Gelatinolytic activity was visualized as clear areas of lysis in the gel. Each sample lane was scanned and presented as percent of latent MMP-2 HT1080-standard. Quantification was performed by the size-fractionated banding pattern densitometrically.
2.8 Western Blot
LV samples were homogenized in lysis buffer containing proteinase inhibitors. An equal amount of protein (10–50 µg) was loaded into a 10% SDS-polyacrylamide gel. Smad 7 (Santa Cruz Biotechnology, Santa Cruz, CA, USA), MT1-MMP/MMP-14 (Sigma, Munich, Germany), TIMP-2 (IM 56L, Calbiochem, Bad Soden, Germany), β tubulin (Santa Cruz) and calsequestrin (PA1–913; Dianova, Hamburg, Germany) were detected with each specific antibody. β tubulin or calsequestrin were used to confirm equal protein loading. Data were expressed as the ratio of the band intensity of the protein of interest (Smad 7, MT1-MMP/MMP-14 or TIMP-2) versus β tubulin or calsequestrin and represented as the percentage of the non-diabetic control group SD-Co 6w. The blots were visualized with chemiluminescene (ECL) system (Amersham Bioscience, Buckinghamshire, UK). Quantitative analysis of the intensity of the bands was performed with Lab Works.
2.9 Statistical analysis
Statistical analysis was performed using JMP Statistical Discovery Software Version 4.05 (SAS Institute, Cary, NC, USA). Non-parametric tests were used for hemodynamic measurements, collagen and TGF-β data analysis, since normal distribution was excluded regarding all parameters. Quantitative and qualitative data were compared, by conducting the Wilcoxon-Kruskal-Wallis test on rank sums. The significant difference for multiple comparisons of all pairs was calculated by the Tukey-Kramer posthoc analysis. Paired and unpaired Student’s t tests were employed for zymography, Western Blot and real-time RT-PCR data analysis. Data are presented as mean ± SEM, except for collagen data which are presented as medians and interquartile ranges (25%–75%th percentile). Differences were considered significant at P ≤ 0.05 in all tests performed.
3 Results
3.1 Hemodynamic data
STZ-induced diabetes was associated with a time-dependent impairment of diastolic function, as indicated by increased dP/dt min and elongated Tau. LVEDP increased by 30%, 6 weeks after STZ-injection, but failed to reach significance. In addition, systolic function was decreased over time, illustrated by reduced LVP and dP/dt max (Table 2). HR was significantly reduced by SD-STZ 2w and SD-STZ 6w compared to SD-Co 6w, which is a characteristic of diabetes-associated dysfunctional cardiac autonomic neuropathy [40].
3.2 Effect of streptozotocin-induced diabetes mellitus on cardiac collagen and TGF-ß
Total collagen deposition increased moderately in the first 2w after STZ application, leading to a 2.1-fold (P < 0.05) higher total collagen content 6w post STZ-injection compared to non-diabetic controls (Fig. 1a, b). The increase in total collagen content 6w after STZ-application, was reflected in a 4.2-fold (P < 0.05) and 3.5-fold (P < 0.05) rise in collagen type I and type III-positive immunostainings, respectively (Fig. 1b). In contrast, mRNA expression of LV collagen type I and type III decreased time-dependently, leading to 8.8-fold (P < 0.005) and 9.3-fold (P < 0.0001) lower expression in SD-STZ 6w vs. SD-Co 6w LVs, respectively (Fig. 1c). TGF-ß positive staining was 54-fold (P < 0.05) increased in SD-STZ 6w compared to SD-Co 6w (Fig. 2).
Time-dependent effect of streptozotocin-induced diabetes mellitus on cardiac total collagen, type I and type III content and mRNA expression. a Cardiac total collagen deposition, expressed as area fraction (AF) %, in non-diabetic SD-Co 6w rats, in rats 2w (SD-STZ 2w) and 6w (SD-STZ 6w) after STZ injection. Data are represented as medians and interquartile ranges (25%–75%th percentile) (n = 6); * P < 0.05 vs. SD-Co 6w. b Representative pictures of total collagen deposition by Sirius Red staining (original magnification ×200) and of collagen type I and type III content visualized by immunostaining (original magnification ×200). Left panel baseline total collagen, collagen type I and III expression in a non-diabetic SD-Co 6w rat heart. Right panel total collagen, collagen type I and III abundance in a SD-STZ 6w rat heart. c LV collagen type I (black bar) and III (white bar) mRNA expression in non-diabetic SD-Co 6w, SD-STZ 2w and SD-STZ 6w rats, normalized to ribosomal L32, multiplied by 10 (n = 4–6). Data are represented as mean ± SEM; § P < 0.05 vs. SD-Co 6w and SD-STZ 6w, * P < 0.05 vs. SD-Co 6w and SD-STZ 2w
Effect of streptozotocin-induced diabetes mellitus on cardiac TGF-ß expression. a Representative picture of TGF-ß staining (original magnification ×200). Left panel baseline TGF-ß expression in a non-diabetic SD-Co 6w rat heart. Right panel increased TGF-ß expression in a SD-STZ 6w rat heart. b Cardiac TGF-ß expression, depicted as area fraction (AF) %, in non-diabetic SD-Co 6w rats and in rats 6w after STZ injection (SD-STZ 6w). Data are represented as medians and interquartile ranges (25%–75%th percentile) (n = 6); * P < 0.05 vs. SD-Co 6w
3.3 Effect of streptozotocin-induced diabetes mellitus on cardiac MMP-9 mRNA, MMP-2 mRNA expression and latent and active MMP-2 levels
LV MMP-9 mRNA tended to be higher in SD-STZ 6w versus SD-Co 6w (SD-Co 6w: 0.0017 ± 0.00051 vs. SD-STZ 6w: 0.0065 ± 0.0020; P = 0.06). LV MMP-2 mRNA expression in SD-STZ 2w and SD-STZ 6w was 2.7-fold (P < 0.005) lower compared to SD-Co 6w (Fig. 3a). In agreement, densitometric analysis of zymographic bands demonstrated that pro-MMP-2 at 72 kDa was 1.3-fold (P < 0.05) reduced in SD-STZ 6w compared to SD-Co 6w heart specimens (Fig. 3b). In addition, MMP-2 activity detected at 66 kDa in SD-Co 6w hearts (0.023 ± 0.0036), was undetectable in SD-STZ 6w hearts (Fig. 3b).
Effect of streptozotocin-induced diabetes mellitus on cardiac MMP-2 mRNA expression and pro-(latent) and active MMP-2 levels. a LV MMP-2 mRNA expression in non-diabetic SD-Co 6w, SD-STZ 2w and SD-STZ 6w rats, normalized to ribosomal L32, multiplied with 10 (n = 4–6). b Upper panel representative inverse picture of zymography of SD-Co 6w and SD-STZ 6w rat hearts, illustrating pro-(latent) and active MMP-2 bands. Lower panel bar graph representing the intensity of latent (black bar) and active (white bar) MMP-2 bands of SD-Co 6w and SD-STZ 6w rat hearts (n = 6). a, b Data are represented as mean ± SEM; * P < 0.05 vs. SD-Co 6w. B.D.: below detection limit
3.4 Effect of streptozotocin-induced diabetes mellitus on cardiac Smad 7 protein levels
Smad 7 was found to be 1.3-fold (P < 0.05) higher expressed in SD-STZ 6w compared to SD-Co 6w (Fig. 4).
Effect of streptozotocin-induced diabetes mellitus on cardiac Smad 7 levels. Upper panel representative Western Blot of SD-Co 6w and SD-STZ 6w rat hearts, illustrating Smad 7 and β tubulin bands. Lower panel bar graphs of relative densitometric means, represented as the percentage of the non-diabetic control group SD-Co 6w of Smad 7 to β tubulin (n = 4). Data are represented as mean ± SEM; * P < 0.05 vs. SD-Co 6w
3.5 Effect of streptozotocin-induced diabetes mellitus on cardiac MT1-MMP and TIMP-2 protein levels
Under non-diabetic conditions, the 45 kDa form of MT1-MMP was more extensively expressed as the 60 kDa form. Both forms were undetectable in SD-STZ 6w hearts (Fig. 5a), whereas TIMP-2 protein expression was 10-fold (P < 0.005) increased in SD-STZ 6w compared to SD-Co 6w hearts (Fig. 5b).
Effect of streptozotocin-induced diabetes mellitus on cardiac MT1-MMP and TIMP-2 levels. a Upper panel representative Western Blot of SD-Co 6w and SD-STZ 6w rat hearts, illustrating MT1-MMP and calsequestrin bands. Lower panel bar graphs of relative densitometric means, represented as the percentage of the non-diabetic control group SD-Co 6w of MT1-MMP towards calsequestrin (n = 6). b Upper panel Western Blot of SD-Co 6w and SD-STZ 6w rat hearts, illustrating TIMP-2 and calsequestrin bands. Lower panel bar graphs of relative densitometric means, represented as the percentage of the non-diabetic control group SD-Co 6w of MT1-MMP to calsequestrin. (n = 5). a, b Data are represented as mean ± SEM; * P < 0.005 vs. SD-Co 6w. B.D.: below detection limit
4 Discussion
The salient finding of the present study is that dysregulation of ECM degradation contributes to the development of cardiac fibrosis in experimental Type I diabetic cardiomyopathy. Thereby, we show that decreased MMP-2 activity concomitant with increased Smad 7 protein levels, decreased MT1-MMP and increased TIMP-2 protein expression, are involved in this condition, which differs from mechanisms involved in dilated and ischemic heart disease.
Evidence from human [5, 31] and experimental models of diabetic cardiomyopathy [13, 25, 39] indicate cardiac fibrosis as pathological substrate of diabetic cardiomyopathy. Cardiac fibrosis leads to increased LV stiffness and decreased ventricular wall compliance, resulting in systolic and in particular diastolic dysfunction. Besides micro-ischemia and inflammation, induction of transforming growth factor (TGF)-β has been indicated to contribute to cardiac fibrosis, leading to the expectation that collagen type I and type III mRNA levels might be increased, at least in early phases of the development of cardiac fibrosis.
Cardiac total collagen deposition, collagen type I and type III content and TGF-ß protein expression were increased in STZ-induced Type I diabetic rats compared to non-diabetic controls. Moreover, the time-dependent increase in cardiac total collagen content was associated with an impairment of early diastolic and systolic function over-time. However, unexpectedly, LV collagen type I and type III mRNA expression declined time-dependently after STZ-injection. This suggests that the increase in collagen type I and type III abundance found in STZ-diabetic rats might lead to suppression of collagen type I and type III mRNA expression as a negative feedback mechanism. On the other hand it also suggests that this accumulation in collagen type I and type III might be due to post-transcriptional/post-translational changes including alterations in ECM regulation, which is mainly controlled by the MMP/TIMP system.
Among others, MMP-2 digests type I, II, and III collagen [2] and is secreted as an inactive pro-enzyme, which is mainly activated by a membrane-linked process involving MT1-MMP, whereas an excess of TIMP-2 inhibits MMP-2 activation by binding all MT1-MMP molecules [9]. In the present study, we demonstrated that MMP-2 mRNA expression declined already after 2w of STZ injection and that MMP-2 mRNA and pro-MMP-2 expression were reduced in STZ-diabetic rat hearts, 6w after STZ-injection compared to non-diabetic controls. Moreover, we could demonstrate that cardiac Smad 7 expression is increased under diabetic conditions. Smad proteins have recently been identified as important components of the TGF-β1 signaling pathway of which Smad 7 is an intracellular antagonist [18, 45]. The role of Smad 7 in MMP-2 regulation is still a matter of discussion: whereas Wang et al. [42] reported that ectopic over-expression of Smad 7 in primary cardiac myofibroblasts was associated with increased MMP-2 activity in the presence and absence of TGF-β1, others found that Smad 7 can suppress TGF-β1-induced MMP-2 production [16, 22], which is independent from its phosphorylation status [23]. The latter is in agreement with our findings under diabetic conditions. We suggest that the reduced MMP-2 mRNA expression and pro-MMP-2 expression found under diabetic conditions can be partly explained by increased Smad 7 protein expression, despite induced TGF-β1 (Fig. 6).
Hypothetical scheme illustrating the proposed cardiac signaling pathway contributing to cardiac fibrosis in streptozotocin-induced diabetes mellitus. The reduction in MMP-2 mRNA expression and latent MMP-2 protein levels under diabetic conditions can be explained by the increase of cardiac Smad 7 expression, which suppresses TGF-β1-induced MMP-2 production, whereas the suppression of MT1-MMP expression together with the increased TIMP-2 expression, leading to an excess of TIMP-2 in the presence of MMP-2 and MT1-MMP, are responsible for the decreased MMP-2 activation in experimental diabetic cardiomyopathy. These mechanisms leading to decreased MMP-2 activity contribute to cardiac fibrosis in streptozotocin-induced diabetes mellitus
Besides a decrease in MMP-2 mRNA expression and latent MMP-2, also the active form of MMP-2 was significantly decreased under diabetic conditions. These results are comparable with observations in diabetes mellitus type 1 [12] and type 2 [17] experimental models of diabetic nephropathy and in cell culture [32, 35], illustrating that impaired matrix degradation is associated with reduced MMP-2 activity. However, this regulation seems to be specific for diabetic conditions since chronic pressure overload in MMP-2 knock out [19] mice is associated with less interstitial fibrosis, and MMP-2 transgenic [6] mice have been reported to be associated with fibrosis.
Moreover, we could demonstrate that MT1-MMP protein expression was reduced and TIMP-2 protein expression increased under diabetic conditions. This suggests that the decreased MMP-2 activity in experimental diabetic cardiomyopathy is due to (1) the reduction in MMP-2 mRNA expression and latent MMP-2, (2) the suppression of MT1-MMP expression and (3) the increase in TIMP-2 expression (Fig. 6). These findings are in line with in vitro studies on collagen lattices where glycation is associated with reduced MMP-2 activity and with decreased MT1-MMP expression [14, 24]. Moreover, we found that in non-diabetic rat hearts, especially the 45 kDa form of MT1-MMP was expressed. Since the activation of pro-MMP-2 is concomitant with an increase in the processing of MT1-MMP from the 60 kDa to the 45 kDa form [33], this finding underscores the activation of pro-MMP-2 under non-diabetic conditions. Interestingly, MT1-MMP also has collagenolytic activity on type I, II, and III collagen [20], implying that down-regulation of MT1-MMP leads to reduced proteolysis of collagen type I, II, III, directly via reduction of its own expression and indirectly via reduced MMP-2 activity.
In conclusion, we describe a mechanism contributing to cardiac fibrosis, which differs from mechanisms involved in dilated or ischemic cardiomyopathy. The latter are characterized by myocardial fibrosis associated with increased collagen type I and type III mRNA expression [21] and MMP activity [10, 26, 36], including MMP-2 [29, 30], and reduced Smad 7 expression [41]. In contrast, under STZ-diabetic conditions, in the absence of LV dilatation [3], cardiac fibrosis is associated with decreased collagen type I and type III mRNA expression, decreased MMP-2 activity and increased Smad 7 expression.
Although the role of other MMPs still has to be investigated, we suggest that the control of matrix regulation differs under certain pathological conditions, which may imply the need for differential therapeutic strategies to prevent the development of cardiac fibrosis under diabetic conditions.
References
Ahmed SH, Clark LL, Pennington WR, Webb CS, Bonnema DD, Leonardi AH, McClure CD, Spinale FG, Zile MR (2006) Matrix metalloproteinases/tissue inhibitors of metalloproteinases: relationship between changes in proteolytic determinants of matrix composition and structural, functional, and clinical manifestations of hypertensive heart disease. Circulation 113:2089–2096
Aimes RT, Quigley JP (1995) Matrix metalloproteinase-2 is an interstitial collagenase. Inhibitor-free enzyme catalyzes the cleavage of collagen fibrils and soluble native type I collagen generating the specific 3/4- and 1/4-length fragments. J Biol Chem 270:5872–5876
Akula A, Kota MK, Gopisetty SG, Chitrapu RV, Kalagara M, Kalagara S, Veeravalli KK, Gomedhikam JP (2003) Biochemical, histological and echocardiographic changes during experimental cardiomyopathy in STZ-induced diabetic rats. Pharmacol Res 48:429–435
Asbun J, Manso AM, Villarreal FJ (2005) Profibrotic influence of high glucose concentration on cardiac fibroblast functions: effects of losartan and vitamin E. Am J Physiol Heart Circ Physiol 288:H227–H234
Bell DS (1995) Diabetic cardiomyopathy. A unique entity or a complication of coronary artery disease? Diabetes Care 18:708–714
Berman M, Teerlink J, Li L, Mahimkar R, Zhu BQ, Nguyen A, Dahi S, Karliner J, Lovett DH (2006) Cardiac matrix metalloproteinase-2 expression independently induces marked ventricular remodeling and systolic dysfunction. Am J Physiol Heart Circ Physiol 292:H1847–H1860
Bidasee KR, Zhang Y, Shao CH, Wang M, Patel KP, Dincer UD, Besch HR Jr. (2004) Diabetes increases formation of advanced glycation end products on Sarco(endo)plasmic reticulum Ca2+-ATPase. Diabetes 53:463–473
Bollano E, Omerovic E, Svensson H, Waagstein F, Fu M (2006) Cardiac remodeling rather than disturbed myocardial energy metabolism is associated with cardiac dysfunction in diabetic rats. Int J Cardiol [Epub ahead of print]
Butler GS, Butler MJ, Atkinson SJ, Will H, Tamura T, Schade van Westrum S, Crabbe T, Clements J, d’Ortho MP, Murphy G (1998) The TIMP2 membrane type 1 metalloproteinase “receptor” regulates the concentration and efficient activation of progelatinase A. A kinetic study. J Biol Chem 273:871–880
Coker ML, Zellner JL, Crumbley AJ, Spinale FG (1999) Defects in matrix metalloproteinase inhibitory stoichiometry and selective MMP induction in patients with nonischemic or ischemic dilated cardiomyopathy. Ann N Y Acad Sci 878:559–562
Dollery CM, McEwan JR, Henney AM (1995) Matrix metalloproteinases and cardiovascular disease. Circ Res 77:863–868
Han SY, Jee YH, Han KH, Kang YS, Kim HK, Han JY, Kim YS, Cha DR (2006) An imbalance between matrix metalloproteinase-2 and tissue inhibitor of matrix metalloproteinase-2 contributes to the development of early diabetic nephropathy. Nephrol Dial Transplant 21:2406–2416
Hayashi T, Sohmiya K, Ukimura A, Endoh S, Mori T, Shimomura H, Okabe M, Terasaki F, Kitaura Y (2003) Angiotensin II receptor blockade prevents microangiopathy and preserves diastolic function in the diabetic rat heart. Heart 89:1236–1242
Kuzuya M, Asai T, Kanda S, Maeda K, Cheng XW, Iguchi A (2001) Glycation cross-links inhibit matrix metalloproteinase-2 activation in vascular smooth muscle cells cultured on collagen lattice. Diabetologia 44:433–436
Kuzuya M, Nakamura K, Sasaki T, Cheng XW, Itohara S, Iguchi A (2006) Effect of MMP-2 deficiency on atherosclerotic lesion formation in apoE-deficient mice. Arterioscler Thromb Vasc Biol 26:1120–1125
Lee EO, Kang JL, Chong YH (2005) The amyloid-beta peptide suppresses transforming growth factor-beta1-induced matrix metalloproteinase-2 production via Smad7 expression in human monocytic THP-1 cells. J Biol Chem 280:7845–7853
Lupia E, Elliot SJ, Lenz O, Zheng F, Hattori M, Striker GE, Striker LJ (1999) IGF-1 decreases collagen degradation in diabetic NOD mesangial cells: implications for diabetic nephropathy. Diabetes 48:1638–1644
Massague J (2000) How cells read TGF-beta signals. Nat Rev Mol Cell Biol 1:169–178
Matsusaka H, Ide T, Matsushima S, Ikeuchi M, Kubota T, Sunagawa K, Kinugawa S, Tsutsui H (2006) Targeted deletion of matrix metalloproteinase 2 ameliorates myocardial remodeling in mice with chronic pressure overload. Hypertension 47:711–717
Ohuchi E, Imai K, Fujii Y, Sato H, Seiki M, Okada Y (1997) Membrane type 1 matrix metalloproteinase digests interstitial collagens and other extracellular matrix macromolecules. J Biol Chem 272:2446–2451
Pauschinger M, Knopf D, Petschauer S, Doerner A, Poller W, Schwimmbeck PL, Kuhl U, Schultheiss HP (1999) Dilated cardiomyopathy is associated with significant changes in collagen type I/III ratio. Circulation 99:2750–2756
Phanish MK, Wahab NA, Colville-Nash P, Hendry BM, Dockrell ME (2006) The differential role of Smad2 and Smad3 in the regulation of pro-fibrotic TGFbeta1 responses in human proximal-tubule epithelial cells. Biochem J 393:601–607
Pulaski L, Landstrom M, Heldin CH, Souchelnytskyi S (2001) Phosphorylation of Smad7 at Ser-249 does not interfere with its inhibitory role in transforming growth factor-beta-dependent signaling but affects Smad7-dependent transcriptional activation. J Biol Chem 276:14344–14349
Rittie L, Berton A, Monboisse JC, Hornebeck W, Gillery P (1999) Decreased contraction of glycated collagen lattices coincides with impaired matrix metalloproteinase production. Biochem Biophys Res Commun 264:488–492
Riva E, Andreoni G, Bianchi R, Latini R, Luvara G, Jeremic G, Traquandi C, Tuccinardi L (1998) Changes in diastolic function and collagen content in normotensive and hypertensive rats with long-term streptozotocin-induced diabetes. Pharmacol Res 37:233–240
Rutschow S, Li J, Schultheiss HP, Pauschinger M (2006) Myocardial proteases and matrix remodeling in inflammatory heart disease. Cardiovasc Res 69:646–656
Sato H, Takino T, Okada Y, Cao J, Shinagawa A, Yamamoto E, Seiki M (1994) A matrix metalloproteinase expressed on the surface of invasive tumour cells. Nature 370:61–65
Schaible TF, Malhotra A, Bauman WA, Scheuer J (1983) Left ventricular function after chronic insulin treatment in diabetic and normal rats. J Mol Cell Cardiol 15:445–458
Seeland U, Kouchi I, Zolk O, Itter G, Linz W, Bohm M (2002) Effect of ramipril and furosemide treatment on interstitial remodeling in post-infarction heart failure rat hearts. J Mol Cell Cardiol 34:151–163
Seeland U, Selejan S, Engelhardt S, Muller P, Lohse MJ, Bohm M (2007) Interstitial remodeling in beta1-adrenergic receptor transgenic mice. Basic Res Cardiol 102:183–193
Shehadeh A, Regan TJ (1995) Cardiac consequences of diabetes mellitus. Clin Cardiol 18:301–305
Singh R, Song RH, Alavi N, Pegoraro AA, Singh AK, Leehey DJ (2001) High glucose decreases matrix metalloproteinase-2 activity in rat mesangial cells via transforming growth factor-beta1. Exp Nephrol 9:249–257
Stanton H, Gavrilovic J, Atkinson SJ, d’Ortho MP, Yamada KM, Zardi L, Murphy G (1998) The activation of ProMMP-2 (gelatinase A) by HT1080 fibrosarcoma cells is promoted by culture on a fibronectin substrate and is concomitant with an increase in processing of MT1-MMP (MMP-14) to a 45 kDa form. J Cell Sci 111(Pt 18):2789–2798
Stilli D, Lagrasta C, Berni R, Bocchi L, Savi M, Delucchi F, Graiani G, Monica M, Maestri R, Baruffi S, Rossi S, Macchi E, Musso E, Quaini F (2007) Preservation of ventricular performance at early stages of diabetic cardiomyopathy involves changes in myocyte size, number and intercellular coupling. Basic Res Cardiol 102:488–499
Tack I, Elliot SJ, Potier M, Rivera A, Striker GE, Striker LJ (2002) Autocrine activation of the IGF-I signaling pathway in mesangial cells isolated from diabetic NOD mice. Diabetes 51:182–188
Thomas CV, Coker ML, Zellner JL, Handy JR, Crumbley AJ 3rd, Spinale FG (1998) Increased matrix metalloproteinase activity and selective upregulation in LV myocardium from patients with end-stage dilated cardiomyopathy. Circulation 97:1708–1715
Tschope C, Spillmann F, Rehfeld U, Koch M, Westermann D, Altmann C, Dendorfer A, Walther T, Bader M, Paul M, Schultheiss HP, Vetter R (2004) Improvement of defective sarcoplasmic reticulum Ca2+ transport in diabetic heart of transgenic rats expressing the human kallikrein-1 gene. Faseb J 18:1967–1969
Tschope C, Walther T, Escher F, Spillmann F, Du J, Altmann C, Schimke I, Bader M, Sanchez-Ferrer CF, Schultheiss HP, Noutsias M (2005) Transgenic activation of the kallikrein-kinin system inhibits intramyocardial inflammation, endothelial dysfunction and oxidative stress in experimental diabetic cardiomyopathy. Faseb J 19:2057–2059
Tschope C, Walther T, Koniger J, Spillmann F, Westermann D, Escher F, Pauschinger M, Pesquero JB, Bader M, Schultheiss HP, Noutsias M (2004) Prevention of cardiac fibrosis and left ventricular dysfunction in diabetic cardiomyopathy in rats by transgenic expression of the human tissue kallikrein gene. Faseb J 18:828–835
Vinik AI, Ziegler D (2007) Diabetic cardiovascular autonomic neuropathy. Circulation 115:387–397
Wang B, Hao J, Jones SC, Yee MS, Roth JC, Dixon IM (2002) Decreased Smad 7 expression contributes to cardiac fibrosis in the infarcted rat heart. Am J Physiol Heart Circ Physiol 282:H1685–H1696
Wang B, Omar A, Angelovska T, Drobic V, Rattan SG, Jones SC, Dixon IM (2007) Regulation of collagen synthesis by inhibitory Smad7 in cardiac myofibroblasts. Am J Physiol Heart Circ Physiol 293:H1282–H1290
Westermann D, Rutschow S, Jager S, Linderer A, Anker S, Riad A, Unger T, Schultheiss HP, Pauschinger M, Tschope C (2007) Contributions of inflammation and cardiac matrix metalloproteinase activity to cardiac failure in diabetic cardiomyopathy: the role of angiotensin type 1 receptor antagonism. Diabetes 56:641–646
Westermann D, Van Linthout S, Dhayat S, Dhayat N, Schmidt A, Noutsias M, Song XY, Spillmann F, Riad A, Schultheiss HP, Tschope C (2007) Tumor necrosis factor-alpha antagonism protects from myocardial inflammation and fibrosis in experimental diabetic cardiomyopathy. Basic Res Cardiol 102:500–507
Wrana JL (2000) Regulation of Smad activity. Cell 100:189–192
Acknowledgments
This study was supported by the DFG (TR SFB19 B5, A21) to CT and MP and by the Bundesministerium für Bildung und Forschung (Competence Network of Heart Failure) to MB; US.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sophie Van Linthout and Ute Seeland contributed equally.
Returned for 1. Revision: 24 October 2007 1. Revision received: 21 December 2007
Returned for 2. Revision: 7 January 2008 2. Revision received: 17 January 2008
Rights and permissions
About this article
Cite this article
Van Linthout, S., Seeland, U., Riad, A. et al. Reduced MMP-2 activity contributes to cardiac fibrosis in experimental diabetic cardiomyopathy. Basic Res Cardiol 103, 319–327 (2008). https://doi.org/10.1007/s00395-008-0715-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00395-008-0715-2