Abstract
CB1 antagonism is associated with reduced doxorubicin-induced cardiotoxicity and decreased cerebrocortical infarction. Rimonabant, a selective CB1 receptor antagonist, was, before it was withdrawn, proposed as a treatment for obesity and reported to reduce cardiovascular risk by improving glucose and lipid profiles and raising adiponectin levels. The cardioprotective actions of rimonabant in 6-week-old C57BL/6J mice fed either high-fat (HFD) or standard diets (STD) for 8 weeks were investigated. At 14 weeks, mice received rimonabant (10 mg/kg/day, i.p.) or vehicle for 1 week and were then subjected to an in vivo acute myocardial infarction. The influence of rimonabant on infarct size (IS) in CB1 knockout (CB1−/−) and wild-type (CB1+/+) mice was also examined. C57BL/6J mice that had been maintained on STD or HFD exhibited 4.3 and 21.4% reductions in body weight following 7 days rimonabant treatment. Rimonabant reduced IS in both STD (29.6 ± 3.5% vs. 49.8 ± 6.9% in control, P < 0.05) and HFD (26.9 ± 1.5% vs. 48.7 ± 7% in control, P < 0.05) mice. In CB1−/− mice rimonabant failed to reduce body weight or IS (51.0 ± 5.3% vs. 49.7 ± 4.7% in control, P > 0.05), although significant reductions were seen in CB1+/+ mice (IS, 48.9 ± 4.6% control vs. 30.5 ± 3.1% rimonabant, P < 0.05). To exclude the possibility that weight loss alone induced cardioprotection, HFD mice were switched to STD for 7 days (HFD–STD), resulting in an 11.3 ± 1.0% decrease in body weight compared to control (+2.1 ± 1.1% in HFD). This, however, was not associated with IS reduction (39.1 ± 3.9% HFD–STD vs. 40.0 ± 5.3% HFD, P > 0.05). Serum and cardiac adiponectin levels were unaltered by rimonabant treatment. HL-1 cell death was not prevented by 1 or 7 days treatment with rimonabant. We conclude that rimonabant-induced infarct limitation may involve the CB1 receptor, although not necessarily cardiac CB1 receptors, and is unrelated to weight loss or altered adiponectin synthesis.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
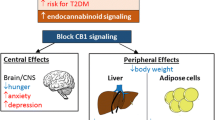
Acute myocardial infarction is the leading cause of mortality globally. Various procedures, such as mechanical manipulation [20, 21, 41] and the administration of many, chemically diverse substances [4, 18, 39, 57], including endogenous factors [5, 8, 16, 25, 40], have been shown to be beneficial with respect to infarct size reduction. White adipose tissue produces a plethora of bioactive peptides, including the adipocytokines, which play vital roles in satiety and energy balance, and have been implicated in obesity, metabolic disease and cardiovascular disease [27]. Recently, the adipocytokines leptin [22, 55], apelin [54] and visfatin [32], apart from inducing metabolic effects, have been shown to protect against myocardial ischaemia–reperfusion (I/R) injury. Another peptide, which probably represents a key adipocytokine with respect to metabolic control, namely adiponectin, has also attracted considerable attention with respect to cardiovascular disease and myocardial protection [24, 49, 50, 58].
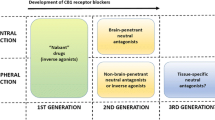
The cannabinoid receptor represents a potential therapeutic target, particularly in the context of metabolic regulation, craving and pain control [34], and drugs acting as both agonists and antagonists of cannabinoid receptors have been identified. The best known of these drugs are the CB1 antagonists which have been proposed as treatments for obesity and drug dependency [34]. In this regard, the CB1 antagonist rimonabant has had a particularly high profile, and was proposed as not only a treatment in obesity but also as adjunct therapy in diabetes, improving both lipid and glucose profiles [10, 28]. Recently, however, on the recommendation of the United States Food and Drug Administration, and the European Medicines Agency, rimonabant has been withdrawn because a proportion of patients developed undesirable psychological side effects. This is unfortunate because pharmacological studies revealed that rimonabant was a highly potent and selective CB1 receptor antagonist [10], and evidence was obtained that its effectiveness in the treatment of obesity, metabolic syndrome and lipid dysfunction relied on its CB1 receptor blocking activity [13]. In addition to its CB1 blocking action, rimonabant was reported to increase adiponectin levels in both humans and animals [2, 13, 17, 45]. This observation is significant given that (1) plasma adiponectin has been reported to be inversely related to cardiovascular risk [1, 37, 44], (2) although produced predominantly by adipocytes, adiponectin is also synthesised by cardiomyocytes, raising the possibility that adiponectin released by the heart may feed back onto the cardiomyocyte to exert autocrine/paracrine effects [24, 58] and (3) as outlined above, adiponectin has been shown to reduce infarct size in an animal model of I/R injury [49]. Therefore, it is feasible that any cardioprotective actions exerted by rimonabant might involve increases in adiponectin expression.
The myocardium expresses CB1 receptors [6], and CB1 antagonists, including rimonabant, have been shown to reduce doxorubicin-induced cardiotoxicity [36] and decrease cerebrocortical infarct size [3]. These observations, coupled with reports that rimonabant is effective in reducing the levels of cardiovascular risk factors [28], led us to hypothesise that rimonabant might prove to be cardioprotective. So, despite the fact that it has been withdrawn, we felt that it was important to establish if a selective and potent CB1 antagonist like rimonabant reduces myocardial I/R injury in vivo, given the possibility that similar but safer drugs may eventually come online. Normal and obese mice were employed in the bulk of these studies which focused primarily on the influence exerted by rimonabant on myocardial infarct size. Some attempt, however, was made to investigate mechanisms that may underly the actions of rimonabant. Thus, the possibility that rimonabant influences myocardial integrity through the agency of the cardioprotective adipocytokine, adiponectin, was considered. In addition, the involvement of the CB1 receptor in its potential actions was investigated using whole body CB1 knockout animals.
Materials and methods
Animals and materials
Experiments using animals were conducted in accordance with the Animals (Scientific Procedures) Act 1986 published by the UK Home Office and the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996). Six-week-old C57BL/6J male mice, purchased from Harlan UK Limited (Oxon, UK), were fed either a high-fat diet (HFD) of 5.2 kcal/g energy density (TestDiet, Richmond, USA; 58Y1: 24% protein, 35% fat, 26% carbohydrates, 60% energy from fat) or a standard rodent diet (STD) of 3.4 kcal/g energy density (Harlan Teklad, Oxon, UK; 2018: 18% protein, 5% fat, 57% carbohydrates) for 8 weeks. CB1+/+ and CB1−/− mice were obtained from Sanofi-Aventis (Montpellier, France) and were generated as described previously [48]. All chemicals were purchased from Sigma-Aldrich (Dorset, UK), unless otherwise stated. Rimonabant was a gift from Sanofi-Aventis (Montpellier, France) and was dissolved in a 1% Cremophor EL/ethanol-94% mixture diluted with normal saline for in vivo studies, and in a 0.1% Cremophor EL/ethanol-94% mixture diluted with Claycomb medium for in vitro studies.
Rimonabant treatment
Six-week-old C57BL/6J male mice were given HFD or STD for 8 weeks before commencing drug treatment with either vehicle (1% Cremophor EL/ethanol-94% mixture) or rimonabant (10 mg/kg/day) for 7 days intraperitoneally: rimonabant was administered for 7 days because pilot studies in HFD mice revealed that this treatment regime resulted in a 20–25% reduction in body weight, a similar decrease to that recorded by Bensaid et al. [2]. Following treatment, animals underwent an ischaemia–reperfusion protocol (see details below). A cohort of vehicle-treated mice were subjected to an ischaemic preconditioning (IPC) protocol in which the coronary artery was occluded for 5 min followed by 5 min of reperfusion prior to the index ischaemia, and served as a positive control group for this experimental model. In addition, a series of experiments were carried out in which the acute effects of rimonabant on myocardial I/R injury were examined in STD-fed C57BL/6J male mice (14 weeks old) that had been given a single bolus dose of vehicle or rimonabant (10 mg/kg/day) intravenously, 10 min prior to ischaemia. As for C57BL/6J mice, STD-fed CB1+/+ and CB1−/− male mice (14 weeks old) were treated with either vehicle or rimonabant for 7 days prior to myocardial I/R injury. The dose of rimonabant used in our experiments (i.e. 10 mg/kg/day) was the same as that employed previously [2, 45].
Weight loss and acute myocardial I/R injury
Six-week-old C57BL/6J male mice were randomised to three diet regimes: (1) HFD: mice were fed on HFD for 9 weeks, (2) STD: mice were fed on STD for 9 weeks or (3) HFD–STD: mice were fed on HFD for 8 weeks followed by a switch to STD for 1 week. At the end of the different diet regimes, mice were subjected to acute myocardial I/R injury.
In vivo model of ischaemia–reperfusion injury
In brief, mice were anaesthetised by intraperitoneal injection with a combination of ketamine, xylazine and atropine (0.01 ml/g, final concentrations of ketamine, xylazine and atropine 10 mg/ml, 2 mg/ml and 0.06 mg/ml, respectively) and body temperature was maintained at 37 ± 0.5°C. The external jugular vein and carotid artery were cannulated for drug administration and mean arterial blood pressure (MABP) measurement, respectively. A tracheotomy was performed for artificial respiration at 120 strokes/min (200 μl stroke volume supplemented with oxygen) and a limb lead 1 electrocardiogram was recorded. A left anterior thoracotomy was performed and the left anterior descending (LAD) coronary artery was ligated with a 8/0 prolene monofilament polypropylene suture placed approximately 2 mm below the tip of the left atrial. The heart was allowed to stabilise for 15 min prior to ligation of the LAD for 30 min to induce ischaemia: successful LAD coronary artery occlusion was confirmed by the presence of ST elevation and decreased arterial blood pressure. At the end of the ischaemic period the ligature was released and a 120 min period of reperfusion followed. Following reperfusion, the heart was isolated and the aortic root cannulated so that 2,3,5-triphenyltetrazolium chloride (5 ml of 1%) could be injected to demarcate the infarcted tissue. The LAD was then re-ligated and Evan’s blue dye (2 ml of 0.5%) perfused to delineate the risk zone. The heart was frozen and sectioned into 1–2 mm transverse sections from apex to occlusion site (5 slices/heart). The slices were then fixed in 10% neutral buffer formalin and photographed with a digital Eskape-fixed camera (Eskape Labs, NY, USA). The risk zone and infarct size were determined by computerised planimetry using the NIH Image J 1.63 software. Risk zone was expressed as a percentage of the left ventricle and infarct size expressed as a percentage of the risk zone [32].
Western blot analysis
Six-week-old C57BL/6J male mice received HFD or STD for 8 weeks before commencing drug treatment with vehicle (1% of Cremophor EL and ethanol-94% mixture) or rimonabant (10 mg/kg/day) for 7 days intraperitoneally. Mouse hearts were then excised, snap-frozen and stored at −80°C. Proteins were extracted by sonication on ice followed by high-speed centrifugation. Proteins were then separated by sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to Hybond ECL nitrocellulose membranes (Amersham Biosciences, Buckinghamshire, UK). The membranes were blocked with TBST (20 mM Tris–HCl, 137 mM NaCl, 0.1% Tween 20 and pH 7.6) containing 5% non-fat dried milk for 1 h, followed by three washes in TBST and then incubated for 2 h with rabbit monoclonal Acrp30 (adiponectin) antibody (C45B10; Cell Signaling Technology, Massachusetts, USA) or rabbit polyclonal CB1 antibody (ab23703; Abcam Plc, Cambridge, UK). After three washes of 5 min in TBST, membranes were then incubated for 1 h with horseradish peroxidase-conjugated anti-rabbit polyclonal antibody (Cell Signaling Technology, Massachusetts, USA). Membranes were then washed three times for 15 min in TBST and enhanced chemiluminescence (ECL) Western blotting reagent (Amersham Biosciences, Buckinghamshire, UK) was used to detect the endogenous levels of total adiponectin and CB1 protein. The membranes were then exposed to photographic films which were scanned and protein band intensity, expressed as arbitrary units, determined by computerised densitometry (NIH ImageJ 1.4 g). The relative changes for the proteins of interest were calculated correcting for differences in protein loading as established by probing for β-actin (Abcam Plc, Cambridge, UK) [15, 53].
ELISA assay
Blood (taken from the chest cavity on removal of the heart) was collected and centrifuged (2,500×g) to yield serum which was frozen at −80°C until the time of analysis. Adiponectin was measured by enzyme-linked immunosorbent assay (ELISA) using 96-well microplates (B-Bridge International, Inc., Mountain View, CA, USA) and a microplate reader (BMG LABTECH Ltd, Aylesbury, Bucks, UK).
HL-1 cells
HL-1 cells (murine atrial cardiomyocytes) [11] were maintained in Claycomb medium (SAFC Bioscience, Kansas, USA) containing 100 μM norepinephrine, 2 mM l-glutamine, 10% fetal bovine serum and 1% penicillin/streptomycin. Cells were seeded at 3 × 104 cells per well in 6-well plates containing Claycomb medium and maintained at 37°C. Cells were subjected to 6 h of hypoxia followed by 18 h of reoxygenation to simulate ischaemia–reperfusion injury. Hypoxia was induced in a custom-made airtight hypoxic chamber, using a buffer simulating the conditions of ischaemia [in mmol/l: 1.0 KH2PO4, 10.0 NaHCO3, 1.2 MgCl2·6H20, 25.0 Na(4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES), 74.0 NaCl, 16.0 KCl, 1.2 CaCl2 and 20.0 Na lactate, pH 6.2], bubbled with 95% nitrogen/5% CO2. Reoxygenation was achieved by replacing the buffer with Claycomb medium. Cells were randomised to the following six treatment groups (Fig. 1).
Experimental protocols for in vitro hypoxia-reoxygenation studies. HL-1 cells were subjected to 6 h hypoxia followed by 18 h reoxygenation and cell death was assessed using the fluorescent probe propidium iodide. HL-1 cells were treated with vehicle (control) or rimonabant (100 nM) for 1 day or 7 days prior to hypoxia. In addition, insulin (300 mU/ml) was added at reoxygenation as a positive control
-
1.
Acute control: cells were treated with vehicle (0.1% Cremophor EL/ethanol-94% mixture) for 1 day.
-
2.
Acute control + insulin: cells were treated with vehicle for 1 day and 300 mU/ml of insulin added at reoxygenation: insulin was used as a positive control as it is known to markedly reduce cell death.
-
3.
Acute rimonabant: cells were treated with rimonabant (final concentration 100 nM) for 1 day.
-
4.
Chronic control: cells were treated with vehicle for 7 days.
-
5.
Chronic control + insulin: cells were treated with vehicle for 7 days and 300 mU/ml of insulin (used as a positive control) added at reoxygenation.
-
6.
Chronic rimonabant: cells were treated with 100 nM rimonabant for 7 days.
At the end of the reoxygenation period, 5 μl of propidium iodide (PI, 1 μg/ml) was added to the cells for 5 min. The percentage of dead cells (as indicated by red fluorescence, PI positive) was calculated by fluorescence microscopy and expressed as a percentage of the total number of cells (PI positive and PI negative) (n > 1,000 cells from 4 to 7 different experiments).
Statistical analysis
All values are expressed as mean ± SEM. Data were analyzed by unpaired t test or one-way ANOVA followed by a Dunnett’s multiple comparison post hoc test where appropriate. A P < 0.05 was considered statistically significant.
Results
Rimonabant reduced body weight in C57BL/6J and CB1+/+ mice but not in CB1−/− mice
C57BL/6J mice fed on STD or HFD and treated over 7 days with rimonabant exhibited 4.3% (P < 0.05) and 21.4% (P < 0.05) reductions in body weight, respectively, compared with mice that received vehicle (Fig. 2). At the start of treatment with rimonabant, the mean body weight of CB1−/− mice was 25.8 ± 0.4 g, which was significantly lower than that of CB1+/+ mice (29.2 ± 0.6 g; P < 0.05; Fig. 3). It has been reported previously that CB1−/− mice have a lower body weight despite the fact that their relative energy intake is comparable to that of WT mice [46]. As shown in Fig. 3, treatment with rimonabant reduced body weight in CB1+/+ mice but had no effect on CB1−/− mice.
Body weight (a) and percentage change in body weight (b) during a 7-day treatment with vehicle (control) or rimonabant (10 mg/kg/day) in STD-fed (n = 17 control, filled square; n = 14 rimonabant, filled circle) and HFD-fed (n = 21 control, open square; n = 14 rimonabant, open circle) C57BL/6J mice. Rimonabant reduced body weight in both STD-fed and HFD-fed mice.*P < 0.05
Body weight (a) and percentage change in body weight (b) during a 7-day treatment with vehicle (control) or rimonabant (10 mg/kg/day) in STD-fed CB1+/+ (filled square control and filled circle rimonabant) and CB1−/− mice (open square control and open circle rimonabant) (n = 8 in each group). Rimonabant was shown to reduce body weight in CB1+/+ but not in CB1−/− mice.*P < 0.05
Chronic treatment with rimonabant reduced infarct size in C57BL/6J mice
Treatment with rimonabant produced no significant changes in MABP or heart rate (Table 1). The risk zones for myocardial infarcts were comparable between the treatment groups; 48.5 ± 2.7%, 49.9 ± 4.8%, 46.5 ± 7.9%, 47.3 ± 5.3%, 60.7 ± 4.9% and 54.5 ± 5.0% in STD-control, STD-rimonabant, STD-IPC, HFD-control, HFD-rimonabant and HFD-IPC, respectively (P > 0.05). Rimonabant, when given for 7 days, significantly reduced infarct size in both STD mice (29.6 ± 3.5% vs. 49.8 ± 6.9% in STD-control; P < 0.05; Fig. 4a) and HFD mice (26.9 ± 1.5% vs. 48.7 ± 7% in HFD-control, P < 0.05; Fig. 4b). The infarct-limiting effect of rimonabant was comparable to IPC (26.8 ± 3.6% in STD and 22.9 ± 3.5% in HFD; P < 0.05 vs. control). However, rimonabant, when given acutely 10 min before prolonged ischaemia, did not modify infarct size (37.7 ± 2.5% in control vs. 41.7 ± 4.7% in rimonabant; n = 7; P > 0.05) or haemodynamic parameters (Table 1).
Effect of rimonabant on infarct size, expressed as a percentage of the risk zone, in STD-fed (a) and HFD-fed (b) C57BL/6J mice pre-treated with vehicle (control) or rimonabant (10 mg/kg/day) for 7 days. IPC was performed on vehicle-treated mice as a positive control. Rimonabant and IPC reduced myocardial infarct size significantly in both STD-fed and HFD-fed C57BL/6J mice. Numbers in parentheses indicate n numbers.*P < 0.05
Rimonabant did not induce cardioprotection in CB1−/− mice
Seven days treatment with rimonabant significantly reduced infarct size in the CB1+/+ mice from 48.9 ± 4.6% in the control group to 30.5 ± 3.1% in the rimonabant-treated group (P < 0.05). However, this infarct-reducing effect of rimonabant was abolished in CB1−/− mice (49.7 ± 4.7%, control vs. 51.0 ± 5.3%, rimonabant; P > 0.05) (Fig. 5). The size of the risk zones was similar in all treatment groups (57.4 ± 6.0% in CB1+/+ control, 56.8 ± 4.3% in CB1+/+ rimonabant, 59.5 ± 5.7% in CB1−/− control and 49.8 ± 5.5% in CB1−/− rimonabant; 1 > 0.05), as were the haemodynamic parameters (Table 1).
Effect of rimonabant on infarct size, expressed as a percentage of the risk zone, in STD-fed CB1+/+ and CB1−/− mice pre-treated with vehicle (control) or rimonabant (10 mg/kg/day) for 7 days. Rimonabant reduced myocardial infarct size significantly in CB1+/+ but not in CB1−/− mice. Numbers in parentheses indicate n numbers.*P < 0.05
Weight loss did not confer cardioprotection
Since rimonabant reduced weight in all treated mice (except CB1−/− mice), we wished to exclude the possibility that weight loss alone conferred cardioprotection in this model. To this end, we returned HFD-fed C57BL/6J mice to STD for 7 days (HFD–STD group) and the body weight decreased by 11.3%, whereas mice that remained on HFD did not exhibit any changes (Fig. 6). The weight loss in these mice was not as marked as that observed in HFD mice treated with rimonabant (21.4%) but was greater than that seen in STD mice treated with rimonabant (4.3%) (Fig. 2). Histological analysis revealed that mean infarct size after I/R in HFD–STD mice (39.1 ± 3.9%, n = 8) was similar to that in HFD (40.0 ± 5.3%; n = 8; P > 0.05) and STD mice (42.1 ± 2.9%; n = 8; P > 0.05). The myocardial risk zones were comparable between the groups (46.6 ± 6.2% in HFD–STD vs. 48.8 ± 4.1% in HFD and 61.2 ± 7.4% in STD; P > 0.05).
Rimonabant did not modify serum or cardiac adiponectin levels
In order to determine whether rimonabant protects the heart by augmenting adiponectin synthesis, we measured plasma and cardiac adiponectin levels. HFD mice were found to have higher adiponectin levels in both blood serum and cardiac tissue compared to STD mice. However, as shown in Fig. 7, chronic treatment with rimonabant did not significantly modify serum adiponectin levels in STD (10.4 ± 2.9 μg/ml vs. 8.9 ± 1.4 μg/ml in control, P > 0.05) or HFD mice (22.9 ± 1.7 μg/ml vs. 26.5 ± 1.2 μg/ml in control; P > 0.05) (Fig. 7a). Similarly, adiponectin expression in cardiac tissue was unaffected by 7 days treatment with rimonabant (Fig. 7b).
Serum adiponectin levels (a) and cardiac adiponectin levels (b) in STD-fed and HFD-fed C57BL/6J mice. Mice were pre-treated with vehicle (control) or rimonabant (10 mg/kg/day) for 7 days (n = 6 in each group). Serum and cardiac adiponectin levels were found to be higher in HFD-fed mice than in STD-fed mice but were not affected by 7 days treatment with rimonabant
Chronic treatment with rimonabant did not improve HL-1 cell viability
Because chronic, but not acute, treatment with rimonabant conferred cardioprotection in mice, this suggested that rimonabant might be having an indirect effect on the heart. To investigate this, we performed an in vitro study using a cardiac cell line. Cell death in HL-1 cells treated with vehicle for 24 h and subjected to hypoxia-reoxygenation was 34.5 ± 4.8% (Fig. 8b). The administration of insulin (used as a positive control) at reoxygenation reduced cell death significantly as compared with control (9.5 ± 3.6% vs. 34.5 ± 4.8% in control; P < 0.05; Fig. 8b). By contrast, rimonabant (100 nM) failed to inhibit cell death (30.4 ± 6.9%; P > 0.05). Similar results were obtained when HL-1 cells were treated with rimonabant for 7 days (43.7 ± 7.7% in control vs. 38.1 ± 5.0% in rimonabant; P > 0.05; Fig. 8b), whilst insulin remained protective against hypoxia-reoxygenation-induced cell death over this period. Western blotting confirmed that CB1 receptors were present on HL-1 cells (see Fig. 8a).
a A representative Western blot showing the presence of a 60 kDa band corresponding to the CB1 receptors in extracts from a mouse heart and HL-1 cells. b Cell viability following 6 h of hypoxia and 18 h of reoxygenation in HL-1 cells treated with rimonabant (100 nM) for 1 day or 7 days. Rimonabant did not affect the % cell death elicited by hypoxia-reoxygenation injury, whilst insulin (300 mU/ml) added at reoxygenation to vehicle-treated cells significantly reduced the % cell death.*P < 0.05
Discussion
The present study demonstrates for the first time that chronic treatment with the selective CB1 receptor antagonist rimonabant reduces myocardial infarct size in a clinically relevant in vivo model. These cardioprotective effects appeared to centre on the CB1 receptor, as evidenced by data obtained with CB1−/− mice, and were evidently independent of rimonabant’s ability to induce weight loss. In addition, rimonabant-induced protection appeared not to involve altered adiponectin synthesis, as reflected by the lack of changes in serum and cardiac adiponectin levels. Interestingly, the findings in HL-1 cells suggested that rimonabant may not have a direct cytoprotective effect on cardiomyocytes.
The role of the CB1 receptor in myocardial I/R injury has yet to be fully elucidated. Thus, whilst CB1 receptors have been reported to mediate the preconditioning effects triggered by a brief period of ischaemia [6] or the nitric oxide donor nitroglycerin [62], the effects induced by lipopolysaccharide [29] and heat stress did not [26]. Studies focusing on the protection exerted by endocannabinoids against myocardial I/R injury have also yielded equivocal results with respect to the CB receptor subtypes involved [38]. In our study, the CB1 receptor antagonist rimonabant exerted an infarct-limiting effect in an in vivo murine model of acute myocardial I/R injury when mice were pre-treated for 7 days with drug, but not when rimonabant was administered 10 min prior to ischaemia. The lack of an acute cardioprotective effect of rimonabant coincides with the results of previous studies carried out with CB1 antagonists in vivo [19, 30] and ex vivo [26]. Nevertheless, CB1 receptor antagonists have been shown to reduce cardiac dysfunction and prevent apoptosis in a doxorubicin-induced acute heart failure model, when administered up to 5 days [36]. Apart from the heart, CB1 receptor antagonists have been shown to protect neurons, e.g. the administration of rimonabant was found to reduce infarct size in a rat stroke model [3].
Although rimonabant has been reported to be a highly selective CB1 receptor antagonist, as evidenced by K i values for CB1 and CB2 of 1.8–11.8 nM and 515–13,200 nM, respectively [42], studies in the brain indicated that rimonabant may possess additional tissue preserving properties, including partial agonist activity [56]. In the current study we attempted to clarify this situation further and were aided in this task using the CB1−/− mouse. Consequently, we obtained data indicating that the infarct-reducing effect of rimonabant did, indeed, involve a CB1 receptor-mediated mechanism.
CB1 receptors are known to play major roles in appetite regulation and energy balance through actions in the hypothalamus [14]. Meanwhile, the weight-reducing effects of rimonabant are well established and the drug was originally proposed as a treatment in obesity [2, 12, 45, 46]. Rimonabant-induced weight loss has been attributed to a reduction in food intake during the early phase of treatment followed by sustained increases in metabolic rate and energy expenditure [2, 33, 46]. In the present study, the degree of weight loss induced by rimonabant appeared to be dependent on the initial body weight of animals. Thus, the extent of weight loss observed in HFD mice (~36 g body weight) was found to exceed that seen in STD mice (~29 g body weight). In agreement with previous studies [46, 47], the weight-reducing effects of rimonabant were found to be absent in CB1−/− mice, providing further evidence that the actions of rimonabant are mediated through a CB1 receptor-mediated mechanism. It was reported by Shinmura et al. [51] that weight loss induced by short-term (4 weeks) caloric restriction (CR), in both young and old rats, led to improved myocardial ischaemic tolerance in vitro. Subsequently, the same workers demonstrated that short-term (2 weeks) CR in mice resulted in cardioprotective effects that were mediated by adiponectin via activation of AMPK [52]. In the light of these findings we, therefore, considered the possibility that the cardioprotective effects exerted by rimonabant in our in vivo murine model might be related to its weight-reducing action. To answer this question we carried out an investigation into the influence of diet-induced weight loss on myocardial I/R injury. Weight loss was achieved by dietary switch from HFD to STD for 7 days (the same period of time used for rimonabant treatment). Interestingly, infarct size in these mice was subsequently found to be similar to that in mice maintained on HFD, even though a 11.3% reduction in body weight was recorded. These data therefore suggest that weight loss probably does not contribute to the infarct-limiting effect of rimonabant.
Adiponectin has been implicated in cardioprotection [49] and is being increasingly recognised as a potential biomarker for the metabolic syndrome and cardiovascular disease [23]. Interestingly, it has been demonstrated that adiponectin synthesis is not restricted to adipose tissue but also occurs in tissues such as bone-forming cells, hepatocytes and cardiomyocytes [43]. Its physiological actions are mediated via specific receptors, AdipoR1 and AdipoR2, which are expressed in cardiac tissue [43]. Studies performed in whole animals and cultured 3T3F442A preadipocytes have shown that rimonabant increases adiponectin mRNA and protein expression via a CB1 receptor-mediated mechanism [2, 17, 45]. For this reason we investigated whether the cardioprotective actions of rimonabant observed in the present study involved increases in adiponectin synthesis. We found, however, that the adiponectin levels in blood serum and heart tissue harvested from mice, pre-treated with rimonabant, were similar to those in mice pre-treated with vehicle, suggesting that increased adiponectin synthesis may not underlie the cardioprotective actions of rimonabant. Our findings are at variance with the results of a previous study which showed that rimonabant treatment in HFD mice was associated with a significant, but modest (18%), increase in serum adiponectin [45]. This study, however, involved treating large numbers of mice for 10 weeks with rimonabant [45], whereas in our study mice were treated for only 1 week. Clearly, therefore, the differences in dosing regimens may have influenced the outcome as regards adiponectin levels. Studies utilising adiponectin-deficient mice should resolve the issue as to whether rimonabant-induced elevations in adiponectin levels influence CB1 receptor antagonist-mediated cardioprotection. Finally, as regards the serum adiponectin results obtained with HFD animals, at first sight these appear to be at variance with previously published data [1, 37, 44], i.e. increases, rather than decreases, were observed. However, it has been reported previously that serum adiponectin increases in mice maintained on a HFD for 10 weeks to greater extents than in animals fed normal chow, before declining to levels below baseline [9].
Despite the fact that rimonabant did not alter serum adiponectin levels, our results still suggested that rimonabant was having an indirect effect on the heart, because cardioprotection was only observed after chronic and not acute treatment. To try and confirm that rimonabant confers cardioprotection indirectly (i.e. does not protect cardiomyocytes directly) we performed in vitro studies using a cardiomyocyte cell line. In view of the fact that the phenotype of isolated primary adult myocytes changes over the period of time in culture used in the present study (i.e. up to 7 days), we chose to use the HL-1 cardiomyocyte cell line, which retains many of the characteristics of primary myocytes, including contractile activity [11]. Interestingly, we found that both acute and chronic treatment with rimonabant failed to protect HL-1 cells against hypoxia-reoxygenation injury, perhaps indicating that rimonabant-induced protection observed in our murine in vivo I/R model was not occurring as a result of a direct action on cardiomyocytes. Subsequently, we confirmed, by Western blot analysis, that HL-1 cells express CB1 receptors, an observation that has not, to our knowledge, been reported previously. These data provide further evidence that rimonabant does not produce its cardioprotective actions via a direct action on the cardiomyocyte or, indeed, an influence on cardiomyocyte-borne CB1 receptors. Interestingly, CB1 antagonists have been shown to directly protect H9c2 myocardial cells against doxorubicin-induced cytotoxity, suggesting that various protective pathways may be involved in preventing tissue damage, the particular pathway mobilised being dependent upon the type of insult that cells/tissues are exposed to [36].
Clearly, the mechanism(s) whereby the CB1 receptor antagonist, rimonabant, exerts its cardioprotective effects remain to be fully elucidated. One possibility that might be considered is that the endocannabinoid system plays a role. We speculate that rimonabant may cause elevations in endocannabinoid levels, thereby compensating for reduced CB1 activity as a consequence of chronic CB1 inhibition. Another possibility that might be explored concerns cross-talk between CB1 and CB2 receptors with CB2 expression being increased as a result of CB1 inhibition. Both scenarios could lead to increased CB2 activation, which is known to be cardioprotective [6, 19, 26, 29, 31, 38], although it has been reported that whilst CB1 expression is evident in the heart [7, 60, 61], CB2 expression is absent [7]. In order to investigate these hypotheses measurements of circulating endocannabinoid levels would need to be carried out, including in samples derived from experiments involving cannabinoid receptor-deficient mice and the administration of CB2 receptor antagonists. Wagner and coworkers [59], for example, reported that changes in endogenous cannabinoids contributed to hypotension in acute myocardial infarction, and that CB1 blockade with rimonabant restored mean arterial pressure but, paradoxially, increased rat mortality. However, as alluded to in the second paragraph of “Discussion” and discussed by Mendizábal and Adler-Graschinsky [35] in their review on cannabinoid therapy in cardiovascular disease, the field of cannabinoid research is highly complex necessitating extreme caution when it comes to the interpretation of experimental data.
To conclude, the principal finding of this study was that chronic treatment with the selective CB1 receptor antagonist, rimonabant, reduced myocardial injury, as indicated by decreased infarct size. An attempt was made to investigate mechanisms that may underly rimonabant-induced cardioprotection. Thus, data were obtained suggesting that rimonabant-induced cardioprotection may be mediated through CB1 receptors, although their precise location has yet to be established, and actions independent of effects on body weight or adiponectin synthesis.
References
Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, Hotta K, Shimomura I, Nakamura T, Miyaoka K, Kuriyama H, Nishida M, Yamashita S, Okubo K, Matsubara K, Muraguchi M, Ohmoto Y, Funahashi T, Matsuzawa Y (1999) Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun 257:79–83
Bensaid M, Gary-Bobo M, Esclangon A, Maffrand JP, Le Fur G, Oury-Donat F, Soubrie P (2003) The cannabinoid CB1 receptor antagonist SR141716 increases Acrp30 mRNA expression in adipose tissue of obese fa/fa rats and in cultured adipocyte cells. Mol Pharmacol 63:908–914
Berger C, Schmid PC, Schabitz WR, Wolf M, Schwab S, Schmid HH (2004) Massive accumulation of N-acylethanolamines after stroke. Cell signalling in acute cerebral ischemia? J Neurochem 88:1159–1167
Bhamra GS, Hausenloy DJ, Davidson SM, Carr RD, Paiva M, Wynne AM, Mocanu MM, Yellon DM (2008) Metformin protects the ischemic heart by the Akt-mediated inhibition of mitochondrial permeability transition pore opening. Basic Res Cardiol 103:274–284
Bose AK, Mocanu MM, Carr RD, Brand CL, Yellon DM (2005) Glucagon-like peptide 1 can directly protect the heart against ischemia/reperfusion injury. Diabetes 54:146–151
Bouchard JF, Lepicier P, Lamontagne D (2003) Contribution of endocannabinoids in the endothelial protection afforded by ischemic preconditioning in the isolated rat heart. Life Sci 72:1859–1870
Brown SM, Wager-Miller J, Mackie K (2002) Cloning and molecular characterization of the rat CB2 receptor. Biochim Biophys Acta 1576:255–264
Bullard AJ, Govewalla P, Yellon DM (2005) Erythropoietin protects the myocardium against reperfusion injury in vitro and in vivo. Basic Res Cardiol 100:397–403
Bullen JW, Bluher S, Kelesidis T, Mantzoros CS (2007) Regulation of aiponectin and its receptors in response to development of diet-induced obesity in mice. Am J Physiol Endocrinol Metab 292:E1079–E1086
Carai MA, Colombo G, Gessa GL (2005) Rimonabant: the first therapeutically relevant cannabinoid antagonist. Life Sci 77:2339–2350
Claycomb WC, Lanson NA Jr, Stallworth BS, Egeland DB, Delcarpio JB, Bahinski A, Izzo NJ Jr (1998) HL-1 cells: a cardiac muscle cell line that contracts and retains phenotypic characteristics of the adult cardiomyocyte. Proc Natl Acad Sci USA 95:2979–2984
Colombo G, Agabio R, Diaz G, Lobina C, Reali R, Gessa GL (1998) Appetite suppression and weight loss after the cannabinoid antagonist SR 141716. Life Sci 63:L113–L117
Despres JP, Golay A, Sjostrom L (2005) Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med 353:2121–2134
Di Marzo V, Goparaju SK, Wang L, Liu J, Batkai S, Jarai Z, Fezza F, Miura GI, Palmiter RD, Sugiura T, Kunos G (2001) Leptin-regulated endocannabinoids are involved in maintaining food intake. Nature 410:822–825
Efthymiou CA, Mocanu MM, Yellon DM (2005) Atorvastatin and myocardial reperfusion injury: new pleiotropic effect implicating multiple prosurvival signaling. J Cardiovasc Pharmacol 45:247–252
Fuglesteg BN, Suleman N, Tiron C, Kanhema T, Lacerda L, Andreasen TV, Sack MN, Jonassen AK, Mjøs OD, Opie LH, Lecour S (2008) Signal transducer and activator of the transcription-3 is involved in the cardioprotective signalling pathway activated by insulin therapy at reperfusion. Basic Res Cardiol 103:444–453
Gary-Bobo M, Elachouri G, Scatton B, Le Fur G, Oury-Donat F, Bensaid M (2006) The cannabinoid CB1 receptor antagonist rimonabant (SR141716) inhibits cell proliferation and increases markers of adipocyte maturation in cultured mouse 3T3 F442A preadipocytes. Mol Pharmacol 69:471–478
Gross ER, Hsu AK, Gross GJ (2007) GSK3β inhibition and KATP channel opening mediate acute opioid-induced cardioprotection at reperfusion. Basic Res Cardiol 102:341–349
Hajrasouliha AR, Tavakoli S, Ghasemi M, Jabehdar-Maralani P, Sadeghipour H, Ebrahimi F, Dehpour AR (2008) Endogenous cannabinoids contribute to remote ischemic preconditioning via cannabinoid CB2 receptors in the rat heart. Eur J Pharmacol 579:246–252
Hausenloy DJ, Yellon DM (2008) Clinical translation of cardioprotective strategies. Basic Res Cardiol 103:493–500
Hausenloy DJ, Ong S-B, Yellon DM (2009) The mitochondrial permeability transition pore as a target for preconditioning and postconditioning. Basic Res Cardiol 104:189–202
Heusch G (2006) Obesity - a rik factor or a RISK factor for myocardial infarction? Br J Pharmacol 149:1–3
Hug C, Lodish HF (2005) The role of the adipocyte hormone adiponectin in cardiovascular disease. Curr Opin Pharmacol 5:129–134
Ishikawa Y, Akasaka Y, Ishii T, Yoda-Murakami M, Choi-Miura NH, Tomita M, Ito K, Zhang L, Akishima Y, Ishihara M, Muramatsu M, Taniyama M (2003) Changes in the distribution pattern of gelatin-binding protein of 28 kDa (adiponectin) in myocardial remodelling after ischaemic injury. Histopathology 42:43–52
Jonassen AK, Sack MN, Mjos OD, Yellon DM (2001) Myocardial protection by insulin at reperfusion requires early administration and is mediated via Akt and p70s6 kinase cell-survival signaling. Circ Res 89:1191–1198
Joyeux M, Arnaud C, Godin-Ribuot D, Demenge P, Lamontagne D, Ribuot C (2002) Endocannabinoids are implicated in the infarct size-reducing effect conferred by heat stress preconditioning in isolated rat hearts. Cardiovasc Res 55:619–625
Kershaw EE, Flier JS (2004) Adipose tissue as an endocrine organ. J Clin Endocrinol Metab 89:2548–2556
Lafontan M, Piazza PV, Girard J (2007) Effects of CB1 antagonist on the control of metabolic functions in obese type 2 diabetic patients. Diabetes Metab 33:85–95
Lagneux C, Lamontagne D (2001) Involvement of cannabinoids in the cardioprotection induced by lipopolysaccharide. Br J Pharmacol 132:793–796
Lasukova OV, Maslov LN, Ermakov SI, Crawford D, Barth F, Krylatov AV, Hanus LO (2008) Role of cannabinoid receptors in regulation of cardiac tolerance to ischemia and reperfusion. Izv Akad Nauk Ser Biol 47:1–478
Lepicier P, Bouchard JF, Lagneux C, Lamontagne D (2003) Endocannabinoids protect the rat isolated heart against ischaemia. Br J Pharmacol 139:805–815
Lim SY, Davidson SM, Paramanathan AJ, Smith CC, Yellon DM, Hausenloy DJ (2008) The novel adipocytokine visfatin exerts direct cardioprotective effects. J Cell Mol Med 12:1395–1403
Liu YL, Connoley IP, Wilson CA, Stock MJ (2005) Effects of the cannabinoid CB1 receptor antagonist SR141716 on oxygen consumption and soleus muscle glucose uptake in Lep(ob)/Lep(ob) mice. Int J Obes (Lond) 29:183–187
Mackie K (2006) Cannabinoid receptors as therapeutic targets. Annu Rev Pharmacol Toxicol 46:101–122
Mendizábal VE, Adler-Graschinsky E (2007) Cannabinoids as therapeutic agents in cardiovascular disease: a tale of passions and illusions. Br J Pharmaol 151:427–440
Mukhopadhyay P, Batkai S, Rajesh M, Czifra N, Harvey-White J, Hasko G, Zsengeller Z, Gerard NP, Liaudet L, Kunos G, Pacher P (2007) Pharmacological inhibition of CB1 cannabinoid receptor protects against doxorubicin-induced cardiotoxicity. J Am Coll Cardiol 50:528–536
Ouchi N, Kihara S, Funahashi T, Matsuzawa Y, Walsh K (2003) Obesity, adiponectin and vascular inflammatory disease. Curr Opin Lipidol 14:561–566
Pacher P, Hasko G (2008) Endocannabinoids and cannabinoid receptors in ischaemia-reperfusion injury and preconditioning. Br J Pharmacol 153:252–262
Peart JN, Gross ER, Reichelt ME, Hsu A, Headrick JP, Gross J (2008) Activation of kappa-opioid receptors at reperfusion affords cardioprotection in both rat and mouse hearts. Basic Res Cardiol 103:454–463
Penna C, Mancardi D, Tullio F, Pagliaro P (2008) Postconditioning and intermittent bradykinin induced cardioprotection require cyclooxygenase activation and prostacyclin release during reperfusion. Basic Res Cardiol 103:368–377
Penna C, Tullio F, Merlino A, Moro F, Raimondo S, Rastaldo R, Perrelli M-G, Mancardi D, Pagliaro P (2008) Postconditioning cardioprotection against infarct size and post-ischemic systolic dysfunction is influenced by gender. Basic Res Cardiol. doi:10.1007s00395-008-0762-8 [Epub ahead of print]
Pertwee RG (2005) Pharmacological actions of cannabinoids. Handb Exp Pharmacol 168:1–51
Pineiro R, Iglesias MJ, Gallego R, Raghay K, Eiras S, Rubio J, Dieguez C, Gualillo O, Gonzalez-Juanatey JR, Lago F (2005) Adiponectin is synthesized and secreted by human and murine cardiomyocytes. FEBS Lett 579:5163–5169
Pischon T, Girman CJ, Hotamisligil GS, Rifai N, Hu FB, Rimm EB (2004) Plasma adiponectin levels and risk of myocardial infarction in men. JAMA 291:1730–1737
Poirier B, Bidouard JP, Cadrouvele C, Marniquet X, Staels B, O’Connor SE, Janiak P, Herbert JM (2005) The anti-obesity effect of rimonabant is associated with an improved serum lipid profile. Diabetes Obes Metab 7:65–72
Ravinet TC, Arnone M, Delgorge C, Gonalons N, Keane P, Maffrand JP, Soubrie P (2003) Anti-obesity effect of SR141716, a CB1 receptor antagonist, in diet-induced obese mice. Am J Physiol Regul Integr Comp Physiol 284:R345–R353
Ravinet TC, Delgorge C, Menet C, Arnone M, Soubrie P (2004) CB1 cannabinoid receptor knockout in mice leads to leanness, resistance to diet-induced obesity and enhanced leptin sensitivity. Int J Obes Relat Metab Disord 28:640–648
Robbe D, Kopf M, Remaury A, Bockaert J, Manzoni OJ (2002) Endogenous cannabinoids mediate long-term synaptic depression in the nucleus accumbens. Proc Natl Acad Sci USA 99:8384–8388
Shibata R, Sato K, Pimentel DR, Takemura Y, Kihara S, Ohashi K, Funahashi T, Ouchi N, Walsh K (2005) Adiponectin protects against myocardial ischemia-reperfusion injury through AMPK- and COX-2 dependent mechanisms. Nat Med 11:1096–1103
Shimada K, Miyazaki T, Daida H (2004) Adiponectin and atherosclerotic disease. Clin Chim Acta 344:1–12
Shinmura K, Tamaki K, Bolli R (2005) Short-term caloric restriction improves ischemic tolerance independent of opening of ATP-sensitive K+ channels in both young and aged hearts. J Mol Cell Cardiol 39:285–296
Shinmura (2007) Cardioprotective effects of short-term caloric restriction are mediated by adiponectin via activation of AMP-activated protein kinase. Circulation 116:2809–2817
Siddall HK, Warrell CE, Yellon DM, Mocanu MM (2008) Ischemia-reperfusion injury and cardioprotection: investigating PTEN, the phosphatase that negatively regulates PI3 K, using a congenital model of PTEN haploinsufficiency. Basic Res Cardiol 103:560–568
Simpkin JC, Yellon DM, Davidson SM, Lim SY, Wynne AM, Smith CC (2007) Apelin-13 and apelin-36 exhibit direct cardioprotective activity against ischemiareperfusion injury. Basic Res Cardiol 102:518–528
Smith CC, Mocanu MM, Davidson SM, Wynne AM, Simpkin JC, Yellon DM (2006) Leptin, the obesity-associated hormone, exhibits direct cardioprotective effects. Br J Pharmacol 149:5–13
Sommer C, Schomacher M, Berger C, Kuhnert K, Muller HD, Schwab S, Schabitz WR (2006) Neuroprotective cannabinoid receptor antagonist SR141716A prevents downregulation of excitotoxic NMDA receptors in the ischemic penumbra. Acta Neuropathol 112:277–286
Strande JL, Hsu A, Su J, Fu X, Gross GJ, Baker JE (2007) SCH 79797, a selective PAR1 antagonist, limits myocardial ischemia/reperfusion injury in rat hearts. Basic Res Cardiol 102:350–358
Takahashi T, Saegusa S, Sumino H, Nakahashi T, Iwai K, Morimoto S, Nojima T, Kanda T (2005) Adiponectin, T-cadherin and tumour necrosis factor-alpha in damaged cardiomyocytes from autopsy specimens. J Int Med Res 33:236–244
Wagner JA, Bauersachs J, Karcher J, Wiesler M, Goparaju SK, Kunos G, Ertl G (2001) Endogenous cannabinoids mediate hypotension after experimental myocardial infarction. J Am Coll Cardiol 38:2048–2054
Wagner JA, Hu K, Karcher J, Bauersachs J, Schäfer A, Laser M, Han H, Ertl G (2003) CB1 cannabinoid receptor antagonism promotes remodeling and cannabinoid treatment prevents endothelial dysfunction and hypertension in rats with myocardial infarction. Br J Pharmacol 138:1251–1258
Wagner JA, Abesser M, Karcher J, Laser M, Kunos G (2005) Coronary vasodilator effects of endogenous cannabinoids in vasopressin-preconstricted unpaced rat isolated hearts. J Cardiovasc Pharmacol 46:348–355
Wagner JA, Abesser M, Harvey-White J, Ertl G (2006) 2-Arachidonylglycerol acting on CB1 cannabinoid receptors mediates delayed cardioprotection induced by nitric oxide in rat isolated hearts. J Cardiovasc Pharmacol 47:650–655
Acknowledgments
This project was supported by Sanofi Aventis and the British Heart Foundation. SY Lim is funded by the Wellcome Trust.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, S.Y., Davidson, S.M., Yellon, D.M. et al. The cannabinoid CB1 receptor antagonist, rimonabant, protects against acute myocardial infarction. Basic Res Cardiol 104, 781–792 (2009). https://doi.org/10.1007/s00395-009-0034-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00395-009-0034-2