Abstract
Whether cannabinoids act as neuroprotectants or, on the contrary, even worsen neuronal damage after cerebral ischemia is currently under discussion. We have previously shown that treatment with the cannabinoid (CB1) receptor antagonist SR141716A reduces infarct volume by ∼40% after experimental stroke. Since it is suggested that SR141716A may exert neuroprotection besides its cannabinoid receptor-blocking effect, we addressed the question whether SR141716A may act via modulation of postischemic ligand binding to excitatory NMDA and/or α-amino-3-hydroxy-5-methyl-4-isoxazole-proprionic acid (AMPA) receptors. For this purpose, rats (n = 12) were treated with either intravenous saline (control) or CB1 receptor antagonist SR141716A (1 mg/kg) 30 min after permanent middle cerebral artery occlusion. Five hours after ischemia, quantitative receptor autoradiography was performed using [3H]CP 55,940, [3H]MK-801, and [3H]AMPA for labeling of CB1, NMDA, and AMPA receptors, respectively. Ligand binding was analyzed within the infarct core, cortical penumbra, and corresponding areas of the contralateral hemisphere and compared to that of sham-operated rats (n = 5). Both in ischemic controls and SR141716A-treated rats [3H]CP 55,940 ligand binding was not specifically regulated in the cortical penumbra or contralateral cortex. Importantly, reduced infarct volumes in SR141716A-treated rats were associated with maintained [3H]MK-801 binding to excitotoxic NMDA receptors in the penumbra, compared to a decrease in the control group. In summary, our data suggest that SR141716A may possess additional intrinsic neuroprotective properties independent of receptor-coupled pathways or due to action as a partial agonist.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Cloning of a central cannabinoid (CB1) receptor from both rat and man [12, 26] triggered the search for endogenous ligands. A few years later, two main substances based on fatty acids were identified and collectively termed endocannabinoids: anandamide and 2-arachidonoylglycerol (2-AG) (for review see [8]). This discovery of an endogenous cannabinoid system immediately focused research activities on its therapeutic potential for a variety of neurological diseases including in vivo models of excitotoxic brain damage. While several studies could demonstrate a neuroprotective effect of endocannabinoids in the animal models of ischemic stroke [18, 20, 31], there was increasing evidence that at least part of the endocannabinoid effect was not mediated by cannabinoid receptors since selective pharmacological blockade or knockout of CB1 receptors failed to completely neutralize the cannabinoid effect [9, 25, 28, 45]. Recently, we could demonstrate that, after permanent cerebral ischemia in rats, anandamide is slightly but significantly increased in the ischemic hemisphere compared to other N-acylethanolamines (NAEs), which are inactive at cannabinoid receptors [4]. Since treatment with the selective CB1 receptor antagonist SR141716A caused a significant reduction of the infarct volume by about 40% compared to ischemic control animals [4], activation of cannabinoid CB1 receptors during the acute postischemic phase seems to be deleterious rather than neuroprotective.
Since the endocannabinoid system modulates NMDA and α-amino-3-hydroxy-5-methyl-4-isoxazole-proprionic acid (AMPA) receptor expression as well as function [2, 21, 43], the aim of this study has been to further check for a possible interplay between cannabinoid and glutamate receptors. Therefore, cannabinoid receptors were pharmacologically blocked by the selective CB1 receptor antagonist SR141716A. Analysis of ligand binding was performed shortly after the ischemic stroke. At this time point, since cerebral ischemia is still in its dynamic phase, periinfarct tissue, the so-called penumbra, is at risk and restoration of the cerebral blood flow critically determines the final lesion size.
Materials and methods
Animal experiments
Animal protocols were approved by the Ethics Committee of the University of Heidelberg according to EU regulations. Experiments were performed on adult male Wistar rats (270–320 g body weight), as previously described by [4]. Material from these animals was used for our present study.
In brief, before surgery, animals were randomly assigned to one of two experimental groups: control group (n = 6) treated with intravenous saline or SR141716A group (n = 3–6) treated with intravenous cannabinoid receptor antagonist SR141716A (1 mg/kg) (N-(piperidin-1-yl)-5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide-hydrochloride) dissolved in 0.1% dimethylsulfoxide (DMSO). At this very low concentration, no effects of DMSO on brain receptor or membrane function have, so far, been described in the literature. Protective effects of DMSO have been reported to occur only from a minimum concentration of 0.5% in vitro [13], while an in vivo study using the same model of permanent focal ischemia in the rat detected neuroprotective effects at concentrations of at least 10% [39]. Concentration of SR141716A (a generous gift from Sanofi Synthelabo in Berlin, Germany) was chosen according to a previous study by Hansen et al. [15]. In both groups, therapy commenced 30 min after the initiation of permanent middle cerebral artery occlusion (pMCAO), which was achieved by applying the endovascular filament method [22]. The PMCAO of the right middle cerebral artery was maintained until the end of the experiment. An additional sham group (n = 5) was subjected to all surgical procedures but without pMCAO. In order to rule out the potential alterations of [3H]CP55,940 binding by the antagonist SR141716A itself, two groups of control rats, treated either with 1 mg/kg SR141716A (n = 4) or 0.1% DMSO (n = 5), were investigated too.
Rats were anesthetized with 350 μl of a 7:1 solution of 10% ketamin (Ketanest™) and 2% xylazinhydrochloride (Rompun™) intraperitoneally. Anesthesia was maintained by re-injection of 150 μl of the solution after 2 h. The left femoral artery and vein were exposed via an incision and cannulated with PE-50 polyethylene tubing. The arterial catheter served for continuous blood pressure recording and blood gas analysis (AVL 990, AVL, Bad Homburg, Germany). The venous catheter was used to administer either vehicle or treatment solution. Core temperature was maintained at 37°C throughout the experiment by a heating pad connected to a rectal probe. Two hours prior to pMCAO, two microdialysis probes were placed bilaterally into the striatum for analysis of microdialysate [4].
Dissection and histology
For examination of receptor regulation during the hyperacute phase of stroke, animals were decapitated 5 h after pMCAO. The brain was removed and sliced into five coronal sections starting at +2.2 mm anterior of the bregma to -5.8 mm dorsal of the bregma. From these sections, two small corresponding areas of each hemisphere were removed for neurochemical analysis [4]. The remaining sections were immediately frozen in liquid nitrogen at −70°C and stored deep-frozen in parafilm wrapping. The infarct lesion volume was evaluated using coronal cryosections of 20 μm thickness according to a silver impregnation method as previously described [46]. In compensation for the effect of brain edema, the corrected infarct volume was calculated as described more detailed by Swanson et al. [44]. Here, in brief, corrected volume of infarct area equals left hemisphere area minus (right hemisphere area minus infarct area). For receptor autoradiography, coronal cryostat sections of 12 μm thickness were serially cut at −20°C at the level of the dorsal hippocampus and mounted on triethoxysilylpropylamine-coated slides.
Receptor autoradiography
Quantitative in vitro receptor autoradiography studies were performed using [3H]CP 55,940, [3H]MK-801, and [3H]AMPA as ligands for CB1, NMDA, and AMPA receptors, respectively [16, 36, 42]. Ligands were purchased from NEN™ Life Science Products Inc (Boston, MA, USA). Labeling and incubation procedures for NMDA and AMPA receptors were performed according to the protocols of Zilles et al. [47] as previously described [40]. Labeling of CB1 receptors was performed according to the protocol of Herkenham et al. [17]. In brief, CB1 receptors were incubated with 10 nM [3H]CP 55,940 (specific activity 158.0 Ci/mmol; 50 mM Tris–HCl buffer, pH 7.4, containing 5% BSA) for 90 min at 22°C. Incubation was terminated by washing for 4 h in ice-cold buffer containing 1% bovine serum albumin. Incubation with [3H]MK-801 and [3H]AMPA was always preceded by a preincubation period with the respective buffer to remove endogenous ligands. In order to demonstrate the maximum binding of [3H]MK-801 to NMDA receptors, the binding assay was performed in a magnesium- and zinc-free solution (50 mM Tris–HCl buffer, pH 7.2) and in the presence of 30 μM glycine and 50 μM spermidine with 5 nM [3H]MK-801 (specific activity 21.7 Ci/mmol) at 22°C for 60 min. Incubation was terminated by washing in cold buffer (2 × 5 min) and in H2O (2 s). AMPA receptors were labeled with 10 nM [3H]AMPA (specific activity 42.2 Ci/mmol) in 50 mM Tris–acetate buffer (pH 7.2, containing 100 mM KSCN) for 45 min at 4°C. Incubation was terminated by rinsing (3 × 4 s) with cold buffer and fixation rinsing (2 × 2 s) with acetone/glutaraldehyde solution. Unspecific binding was determined by co-incubation of alternating sections with labeled ligands and excess of an appropriate unlabeled competitor. Subsequent to the final rinsing procedure, slides were carefully dried in either a stream of cool air ([3H]MK-801) or hot air ([3H]AMPA and [3H]CP 55,940). Air-dried, tritium-labeled sections were co-exposed with [3H]plastic standards (Microscales®; Amersham, Freiburg, Germany) and brain-paste standards to a [3H]-sensitive film (Kodak™ BioMax™ MR-1; Amersham, Braunschweig, Germany) for 7–8 weeks ([3H]MK-801 and [3H]CP 55,940), respectively. Autoradiographies were scanned in equal light conditions by means of a DMC video camera (Polaroid, Offenbach, Germany) and digitized with the AIS image analysis system (Imaging Research Inc., St. Catharines, ON, Canada). Gray value images of the co-exposed plastic standards were used to compute a nonlinear calibration curve, which defined a relationship between gray values in the autoradiographs and concentrations of radioactivity. Plastic standards were calibrated to tissue standards with known concentrations of radioactivity. Final values were normalized to sham control levels (mean ± SEM), as described by Hansen et al. [14]. For analysis of ligand binding in different brain areas, Nissl-stained cryostat sections were scanned with a DMC video camera (Polaroid) and the infarct areas marked on the monitor. Then, images were superimposed on the autoradiographies. Quantitative analysis of radioactivity was performed separately in all six cortical layers within the infarct center (‘core’) and adjacent to the infarct (‘penumbra’) as well as in a corresponding area of the hemisphere contralateral to the infarct. In untreated sham controls, analysis was performed in just one hemisphere within areas corresponding to those in ischemic animals. Analysis of potential alteration of [3H]CP 55,940 binding by SR141716A was performed in control rats in corresponding areas of the cortical infarct and periinfarct region in both hemispheres. Regions of interest were marked on the monitor and the gray values were automatically assessed by the imaging software. In all cases, nonspecific binding was just above background labeling or completely invisible. Therefore, the degree of background density could be used as an estimate of unspecific binding and subtracted from the total binding.
Statistical analysis
Ligand binding was analyzed by calculating mean concentration values for each ligand and region. Significant group effects were confirmed by analysis of variance (ANOVA) and least significant difference (LSD) error protection. A P value < 0.05 was considered statistically significant. Analysis was performed using the general statistics module of Analyse-it™ for Microsoft Excel (Analyse-it Software, Ltd., Leeds, UK).
Results
Quantitative receptor autoradiography
Treatment with SR141716A did not significantly alter [3H]CP 55,940 binding in two cortical areas corresponding to the ischemic core and the penumbra of ischemic rats (Table 1).
CB1 receptor ([3H]CP 55,940 binding)
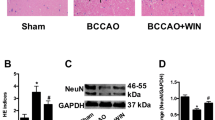
[3H]CP 55,940 ligand binding in all cortical layers of the ischemic core did not differ significantly in the ischemic group from that in sham controls. However, a dramatic reduction was seen in the SR141716A group, reaching significance in layer I (Fig. 1). This effect was neither present in the ischemic penumbra (ip) nor in the corresponding cortical areas of the contralateral hemisphere with binding levels remaining largely unchanged within the two experimental groups (Fig. 1).
Postischemic [3H]CP 55,940 binding. No specific postischemic regulation of [3H]CP 55,940 binding was detectable in ischemic controls. Pharmacologically blocking CB1 receptors by SR141716A inhibited [3H]CP 55,940 binding only in the infarct core whereas in the ip and contralateral cortex the binding values did not differ from controls. Values are means ± SEM (n = 4–5) presented as % of sham-operated controls (asterisks: significant difference compared to sham, P < 0.05; ANOVA and LSD protection)
NMDA receptor ([3H]MK-801 binding)
[3H]MK-801 ligand binding density within the ischemic core was significantly reduced in cortical layers I–IV and VI in the ischemic group and in cortical layers I–IV in the SR141716A-treated group (Figs. 2, 3). In the ip [3H]MK-801 ligand binding values of ischemic controls were reduced in all layers reaching significance in layers II and III (Figs. 2, 3). No significant alterations of [3H]MK-801 cortical ligand binding were detectable in the SR141716A group (Figs. 2, 3). Similar to the ip, there was a trend to reduced [3H]MK-801 ligand binding values in the contralateral cortex in ischemic controls whereas binding densities in the SR141716A group remained largely unchanged (Figs. 2, 3).
Postischemic [3H]MK-801 binding. Compared to sham, binding values were decreased within the infarct core in all experimental groups. Treatment with the CB1 antagonist SR141716A maintained [3H]MK-801 ligand binding to excitotoxic NMDA receptors in the ip, possibly indicating the high intrinsic neuroprotective efficacy of SR141716A. Values are means ± SEM (n = 3–6) presented as % of sham-operated controls (asterisks: significant difference compared to sham, P < 0.05; ANOVA and LSD protection)
Representative autoradiograms of [3H]MK-801 ligand binding in the various experimental groups. In contrast to untreated ischemic controls (b) the [3H]MK-801 binding to potentially excitotoxic NMDA receptors in the ischemic penumbra (ip) of SR141716A-treated rats is largely maintained (c) compared to sham control (a), suggesting high intrinsic neuroprotective properties of the cannabinoid receptor antagonist SR141716A. Abbreviations: I infarct area, marked in yellow, cl contralateral, ip ischemic penumbra, core infarct core, asterisks: area for measurement of unspecific binding
α-amino-3-hydroxy-5-methyl-4-isoxazole-proprionic acid receptor ([3H]AMPA binding)
Within the infarct core, [3H]AMPA ligand binding density was significantly decreased to about 30% of sham controls in all cortical layers in ischemic controls and SR141716A-treated rats, respectively (Fig. 4). In the ip, reduction of [3H]AMPA ligand binding was not as pronounced as in the ischemic core but, nevertheless, reached significance in all layers in the ischemic group and in layers I–IV and VI in the SR141716A group (Fig. 4). Within the corresponding cortex of the contralateral hemisphere [3H]AMPA binding was widely maintained in ischemic controls. In the SR141716A group, there was a trend to reduced values. This, however, did not reach any significance (Fig. 4).
Postischemic [3H]AMPA binding [3H]AMPA binding was reduced in both experimental groups throughout all layers in the infarct core and the ip. In the contralateral cortex, no significant changes are detectable in ischemic controls and SR141716A treated rats. Values are means ± SEM (n = 4–6) presented as % of sham-operated controls (asterisks: significant difference compared to sham, P < 0.05; ANOVA and LSD protection)
Absolute binding values (fmol/mg) for all three ligands used are presented in Table 2.
Discussion
The neuroprotective action of endocannabinoids and exogenously applicated cannabinoids against brain damage after cerebral ischemia is controversially discussed [7, 11, 15, 20, 23, 24, 28, 30, 32, 37, 38, 45]. There is growing body of evidence that at least part of the cannabinoid effect is not mediated by cannabinoid receptors since selective pharmacological blockade or knockout of CB1 receptors fails to completely neutralize the cannabinoid effect [9, 25, 28, 45]. Surprisingly, by use of the CB1 receptor antagonist SR141716A, we could recently demonstrate a significant reduction of infarct volume in a model of permanent cerebral ischemia by about 40% [4]. Whether SR141716A exerts its neuroprotective effects by blocking CB1 receptors or whether it is, in fact, neuroprotective, independent of CB1 receptor pathways, remains so far unclear. In our present study we checked whether SR141716A may exert its neuroprotective effects by modulating ligand binding to excitatory glutamate receptors in the ip.
Most surprisingly, [3H]MK-801 ligand binding to excitatory NMDA receptors in the ischemic penumbra was maintained compared to a significant reduction in ischemic controls (Figs. 2, 3) while binding to AMPA receptors in this region was downregulated both in controls and SR141716A-treated rats. Since a multitude of studies could convincingly demonstrate that NMDA receptors are mediators of excitotoxic neuronal death resulting from over-activation of excitatory glutamate receptors (for review see [10, 29]), it could be assumed that a substance which has been shown to be more potent in postischemic neuroprotection than the NMDA receptor antagonist MK-801 [4] would not enhance the binding density of precisely this receptor in the cortical penumbra. Therefore, our finding would best fit in with the hypothesis that the CB1 receptor antagonist SR141716A possesses additional intrinsic neuroprotective properties or a partial agonist activity. Using the rat model of transient forebrain ischemia, Nagayama et al. [28] were able to show that the neuroprotective effect of WIN 55212, a cannabinoid receptor agonist, was only partially neutralized by SR141716A. In a ouabain-induced injury model in neonatal rats, it was possible to antagonize the effect of anandamide for measurements of the lesion volume at day seven which was not the case for measurements of early cytotoxic edema [45]. Moreover, application of SR141716A alone, i.e., not concomitant with anandamide, did not increase the ouabain-induced brain injury [45]. In an in vivo newborn rat model of acute severe asphyxia, SR141716A failed to modify the protective effect of WIN 55212 on early neuronal death, but abolished the WIN 55212-induced inhibition of delayed neuronal death [25]. A recent study by Hansen et al. [15] provided strong evidence for a separate neuroprotective effect of SR141716A in counteracting NMDA-induced excitotoxic injury in neonatal rats, whereas both CB1 agonists and CB2 antagonists failed to protect brain tissue against excitotoxicity. Similarly, a neuroprotective effect of SR141716A was shown in a rat model of unilateral focal ischemia-reperfusion injury whereas WIN 55212 failed to reduce the infarct volume [27]. More importantly, an in vitro study by Berdyshev et al. [3] provided strong evidence that SR141716A has its own signaling potential via extracellular signal-regulated kinase (ERK) phosphorylation and, to a lesser degree, AP-1 activation which, in turn, may exert the neuroprotective effect. Finally, SR141716A was suggested to act as a selective inverse agonist for central cannabinoid receptors [6]. Therefore, SR141716 may possibly exert its neuroprotective effect due to intrinsic properties and even despite higher levels of [3H]MK-801 binding values to NMDA receptors, compared to ischemic controls which, at early timepoints after injury, are generally thought to exert excitotoxic effects [5].
Reduction of [3H]MK-801 ligand binding in the ischemic core as early as 5 h after onset of ischemia, as seen for ischemic control rats in the present study, is well in line with data supplied by Que et al. [34]. Using a photothrombotic ischemia model, the authors demonstrated a 60% reduction already after 4 h, which became even more pronounced at later time points [19, 33, 34, 41]. In our present study, lowered levels of [3H]MK-801 binding values in the ischemic core were also seen in SR141716A-treated rats (Fig. 2), most likely reflecting progression and irreversibility of the injury in this area.
Until now, little is known about the postischemic regulation of central cannabinoid receptors. To the best of our knowledge, there is only one single study analyzing the density of cannabinoid receptors after focal cerebral ischemia by immunohistochemistry and Western blotting [18]. The authors demonstrated an upregulation of CB1 receptors in neurons of the peri-infarct area in rats as early as 2 h after the onset of ischemia. On the basis of these findings, a crucial role for the endocannabinoid system in postischemic neuroprotection was suggested. Increased abundance of the respective receptor protein, however, does not necessarily reflect enhanced ligand binding or increased receptor activation. In our present study, we could convincingly demonstrate that, 5 h after onset of permanent ischemia, there is no specific postischemic alteration of [3H]CP55,940 ligand binding density to CB1 receptors in any cortical layer of the ip or in any corresponding areas of the contralateral hemisphere (Fig. 1). Furthermore, in a model of global ischemia, we could recently demonstrate that after a short ischemic period usually used for ischemic preconditioning, survival of neurons at risk is even associated with downregulation of CB1 receptors [38], thus, suggesting a harmful mechanism of CB1 receptors for postischemic neuronal fate.
The maintenance of [3H]CP55,940 binding within the ischemic core in control rats is somewhat surprising. The most feasible explanation is that there is a stronger resistance of CB1 binding sites to degradation, associated with consecutively delayed reduction of binding values. This phenomenon is similar to the extremely delayed reduction of [3H]muscimol binding to inhibitory γ-aminobutyric acid (GABA)A receptors in irreversibly damaged brain tissue [1, 40, 41]. On the other hand, reduced [3H]CP55,940 binding in the SR141716A group is most likely due to the blocking of binding sites by the pharmacon [35], at least as far as the ischemic core with consecutively reduced wash-out is concerned.
In summary, our present data demonstrate the absence of specific postischemic regulation of central CB1 cannabinoid receptors in the ischemic core as well as in the penumbra and contralateral cortical areas. Even more important is the fact that [3H]MK-801 binding to excitotoxic NMDA receptors in the ip is maintained in the SR141716A group which is associated with a maximum reduction of the infarct volume [4]. Thus, our current data would well fit in with previous studies suggesting that the cannabinoid receptor antagonist SR141716A possesses additional intrinsic neuroprotective or partial agonist properties. Vice versa, the relevance of the endocannabinoid system for robust neuroprotection during the hyperacute postischemic phase has to be critically challenged in future studies.
References
Araki T, Kanai Y, Murakami F, Kato H, Kogure K (1993) Postischemic changes in the binding of excitatory and inhibitory neurotransmitters in the gerbil brain. Pharmacol Biochem Behav 45:945–949
Auclair N, Otani S, Soubrie P, Crepel F (2000) Cannabinoids modulate synaptic strength and plasticity at glutamatergic synapses of rat prefrontal cortex pryramidal neurons. J Neurophysiol 83:3287–3293
Berdyshev EV, Schmid PC, Krebsbach RJ, Hillard CJ, Huang C, Chen N, Dong Z, Schmid HHO (2001) Cannabinoid-receptor-independent cell signalling by N-acylethanolamines. Biochem J 360:67–75
Berger C, Schmid PC, Schäbitz WR, Wolf M, Schwab S, Schmid HHO (2004) Massive accumulation of N-acylethanolamines after stroke. Cell signalling in acute cerebral ischemia? J Neurochem 88:1159–1167
Biegon A, Fry PA, Paden CM, Alexandrovich A, Tsenter J, Shohami E (2004) Dynamic changes in N-methyl-d-aspartate receptors after closed head injury in mice: implications for treatment of neurological and cognitive deficits. Proc Natl Acad Sci USA 101:5117–5122
Bouaboula M, Perrachon S, Milligan L, Canat X, Rinaldi-Carmona M, Portier M, Barth F, Calandra B, Pecceu F, Lupker J, Maffrand JP, Le Fur G, Casellas P (1997) A selective inverse agonist for central cannabinoid receptor inhibits mitogen-activated protein kinase activation stimulated by insulin or insulin-like growth factor 1. J Biol Chem 272:22330–22339
Chan GC, Hinds TR, Impey S, Storm DR (1998) Hippocampal neurotoxicity of Δ9-tetrahydrocannabinol. J Neurosci 18:5322–5332
Di Marzo V, Melck D, Bisogno T, De Petrocellis L (1998) Endocannabinoids: endogenous receptor ligands with neuromodulatory action. Trends Neurosci 21:521–528
Di Marzo V, Breivogel CS, Tao Q, Bridgen DT, Razdan RK, Zimmer AM, Zimmer A, Martin BR (2000) Levels, metabolism and pharmacological activity of anandamide in CB1 cannabionoid receptor knockout mice: evidence for non-CB1, non-CB2 receptor-mediated actions of anandamide in mouse brain. J Neurochem 75:2434–2444
Dirnagl U, Iadecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: an integrated review. Trends Neurosci 22:391–397
Downer E, Boland B, Fogarty M, Campbell V (2001) Δ9-tetrahydrocannabinol induces the apoptotic pathway in cultured cortical neurones via activation of the CB1 receptor. Neuroreport 12:3973–3978
Gérard CM, Mollereau C, Vassart G, Parmentier M (1991) Molecular cloning of a human cannabinoid receptor which is also expressed in testis. Biochemistry 279:129–134
Greiner C, Schmidinger A, Hülsmann S, Moskopp D, Wolfer J, Köhling R, Speckmann E-J, Wassmann H (2000) Acute protective effect of nimodipine and dimethyl sulfoxide against hypoxic and ischemic brain damage in brain slices. Brain Res 887:316–322
Hansen HH, Schmid PC, Bittigau P, Lastres-Becker I, Berrendero F, Manzanares J, Ikonomidou C, Schmid HH, Fernandez-Ruiz JJ, Hansen HS (2001) Anandamide, but not 2-arachidonoylglycerol, accumulates during in vivo neurodegeneration. J Neurochem 78:1415–1427
Hansen HH, Azcoitia I, Pons S, Romero J, Garcia-Segura LM, Ramos JA, Hansen HS, Fernández-Ruiz J (2002) Blockade of cannabinoid CB(1) receptor function protects against in vivo disseminating brain damage following NMDA-induced excitotoxicity. J Neurochem 82:154–158
Herkenham M, Lynn AB, Little MD, Johnson R, Melvin LS, De Costa BR, Rice KC (1990) Cannabinoid receptor localization in brain. Proc Natl Acad Sci USA 87:1932–1936
Herkenham M, Lynn AB, Johnson MR, Melvin LS, De Costa BR, Rice KC (1991) Characterization and localization of cannabinoid receptors in rat brain: a quantitative in vitro autoradiographic study. J Neurosci 11:563–583
Jin KL, Moa XO, Goldsmith PC, Greenberg DA (2000) CB1 cannabinoid receptor induction in experimental stroke. Ann Neurol 48:257–261
Jolkkonen J, Gallagher NP, Zilles K, Sivenius J (2003) Behavioral deficits and recovery following transient focal cerebral ischemia in rats: glutamatergic and GABAergic receptor densities. Behav Brain Res 138:187–200
Landfield PW, Cadwallader LB, Vinsant S (1988) Quantitative changes in hippocampal structures following long-term exposure to delta 9-tetrahydrocannabinol: possible mediation by glucocorticoid system. Brain Res 443:47–62
Lei S, Pelkey A, Topolnik L, Congar P, Lacaille JC, McBain CJ (2003) Depolarization-induced long-term depression at hippocampal mossy fiber-CA3 pyramidal neuron synapses. J Neurosci 23:9786–9795
Longa EZ, Weinstein PR, Carlson S, Cummins R (1989) Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 20:84–91
Louw DF, Yang FW, Sutherland GR (2000) The effect of δ-9-tetrahydrocannabinol on forebrain ischemia in rat. Brain Res 857:183–187
Marsicano G, Goodenough S, Monory K, Hermann H, Eder M, Cannich A, Azad SC, Cascio MG, Gutierrez SO, van der Stelt M, Lopez-Rodrigues ML, Casanova E, Schutz G, Zieglgansberger W, Di Marzo V, Behl C, Lutz B (2003) CB1 cannabinoid receptors and on-demand defense against excitotoxicity. Science 302:84–88
Martinez-Orgado J, Fernandez-Frutos B, Gonzalez R, Romero E, Uriguen L, Romero J, Viveros MP (2003) Neuroprotection by the cannabinoid agonist WIN-55212 in an in vivo newborn rat model of acute severe asphyxia. Brain Res Mol Brain Res 1141:32–139
Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI (1990) Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346:561–564
Muthian S, Rademacher DJ, Roelke CT, Gross GJ, Hillard CJ (2004) Anandamide content is increased and CB1 cannabinoid receptor blockade is protective during transient, focal cerebral ischemia. Neuroscience 129:743–750
Nagayama T, Sinor AD, Simon RP, Chen J, Graham SH, Jin K, Greenberg DA (1999) Cannabinoids and neuroprotection in global and focal cerebral ischemia and in neuronal cultures. J Neurosci 19:2987–2995
Obrenovitch TP, Urenjak J (1997) Altered glutamatergic transmission in neurological disorders: from high extracellular glutamate to excessive synaptic efficacy. Prog Neurobiol 51:39–87
Panikashvili D, Simeonidou C, Ben-Shabat S, Hanus L, Breuer A, Mechoulam R, Shohami E (2001) An endogenous cannabinoid (2-AG) is neuroprotective after brain injury. Nature 413:527–531
Panikashvili D, Mechoulam R, Beni SM, Alexandrovich A, Shohami E (2005) CB1 cannabinoid receptors are involved in neuroprotection via NF-kappa B inhibition. J Cereb Blood Flow Metab 25:477–484
Parmentier-Batteur S, Jin K, Mao XO, Xie L, Greenberg DA (2002) Increased severity of stroke in CB1 cannabinoid receptor knock-out mice. J Neurosci 22:9771–9775
Qü M, Mittmann T, Luhmann HJ, Schleicher A, Zilles K (1998) Long-term changes of ionotropic glutamate and GABA receptors after unilateral permanent focal cerebral ischemia in the mouse brain. Neuroscience 85:29–43
Que M, Schiene K, Witte OW, Zilles K (1999) Widespread up-regulation of NMDA receptors after focal photothrombotic lesion in rat brain. Neurosci Lett 273:77–80
Rinaldi-Carmora M, Barth F, Heaulme M, Alonso R, Shire D, Congy C, Soubrie P, Breliere JC, Le Fur G (1995) Biochemical and pharmacological characterisation of SR141716A, the first potent and selective brain cannabinoid receptor antagonist. Life Sci 56:1941–1947
Sakurai SY, Cha J-HJ, Penney JB, Young AB (1991) Regional distribution and properties of [3H]MK-801 binding sites determined by quantitative autoradiography in rat brain. Neuroscience 40:533–543
Scallet AC (1991) Neurotoxicology of cannabis and THS: a review of chronic exposure studies in animals. Pharmacol Biochem Behav 40:671–676
Schomacher M, Müller HD, Sommer C (2006) Short-term ischemia usually used for ischemic preconditioning down-regulates central cannabinoid receptors in the gerbil hippocampus. Acta Neuropathol (Berl) 111:8–14
Shimizu S, Simon RP, Graham SH (1997) Dimethylsulfloxide (DMSO) treatment reduces infarction volume after permanent focal cerebral ischemia in rats. Neurosci Lett 239:125–127
Sommer C, Fahrner A, Kiessling M (2002) [3H]Muscimol binding to GABAA receptors is upregulated in CA1 neurons of the gerbil hippocampus in the ischemia tolerant state. Stroke 33:1093–1100
Sommer C, Kollmar R, Schwab S, Kiessling M, Schäbitz WR (2003) Exogenous brain-derived neurotrophic factor prevents postischemic downregulation of [3H]muscimol binding to GABAA receptors in the cortical penumbra. Mol Brain Res 111:24–30
Standley S, Tocco G, Tourigny M-F, Massicotte F, Thompson RF, Baudry M (1995) Developmental changes in a-amino-3-hydroxy-5-methyl-4-isoxazole proprionate receptor properties and expression in the rat hippocampal formation. Neuroscience 67:881–892
Suarez I, Bodega G, Fernandez-Ruiz J, Ramos JA, Rubio M, Fernandez B (2004) Down-regulation of the AMPA glutamate receptor subunits GluR1 and GluR2/3 in the rat cerebellum following pre- and perinatal delta9-tetrahydrocannabinol exposure. Cerebellum 3:66–74
Swanson RA, Morton MT, Tsao-Wu G, Savalos RA, Davidson C, Sharp FR (1990) A semiautomated method for measuring brain infarct volume. J Cereb Blood Flow Metab 10:290–293
van der Stelt M, Veldhuis WB, Van Haaften GW, Fezza F, Bisogno T, Bar PR, Veldink GA, Vliegenthart JF, Di Marzo V, Nicolay K (2001) Exogenous anandamide protects rat brain against acute neuronal injury in vivo. J Neurosci 21:8765–8771
Vogel J, Mobius C, Kuschinsky W (1999) Early delineation of ischemic tissue in rat brain cryosections by high-contrast staining. Stroke 30:1134–1141
Zilles K, Wu J, Crusio WEH, Schwegler H (2000) Water maze and radial maze learning and the density of binding sites of glutamate, GABA, and serotonin receptors in the hippocampus of inbred mouse strains. Hippocampus 10:213–225
Acknowledgments
This work was in part supported by the Bundesministerium für Bildung und Forschung. SR141716A was a generous gift from Sanofi Synthelabo, Berlin, Germany. The authors greatly acknowledge the excellent technical assistance of Stephan Hennes and Jessica Saba. Astrid Wöber kindly gave editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sommer, C., Schomacher, M., Berger, C. et al. Neuroprotective cannabinoid receptor antagonist SR141716A prevents downregulation of excitotoxic NMDA receptors in the ischemic penumbra. Acta Neuropathol 112, 277–286 (2006). https://doi.org/10.1007/s00401-006-0110-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-006-0110-8