Abstract
Purpose
The aim of this study was to investigate the effects of creatine supplementation on muscle wasting in Walker-256 tumor-bearing rats.
Methods
Wistar rats were randomly assigned into three groups (n = 10/group): control (C), tumor bearing (T), and tumor bearing supplemented with creatine (TCr). Creatine was provided in drinking water for a total of 21 days. After 11 days of supplementation, tumor cells were implanted subcutaneously into T and TCr groups. The animals’ weight, food and water intake were evaluated along the experimental protocol. After 10 days of tumor implantation (21 total), animals were euthanized for inflammatory state and skeletal muscle cross-sectional area measurements. Skeletal muscle components of ubiquitin–proteasome pathways were also evaluated using real-time PCR and immunoblotting.
Results
The results showed that creatine supplementation protected tumor-bearing rats against body weight loss and skeletal muscle atrophy. Creatine intake promoted lower levels of plasma TNF-α and IL-6 and smaller spleen morphology changes such as reduced size of white pulp and lymphoid follicle compared to tumor-bearing rats. In addition, creatine prevented increased levels of skeletal muscle Atrogin-1 and MuRF-1, key regulators of muscle atrophy.
Conclusion
Creatine supplementation prevents skeletal muscle atrophy by attenuating tumor-induced pro-inflammatory environment, a condition that minimizes Atrogin-1 and MuRF-1-dependent proteolysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Muscle wasting is the main component of cancer cachexia, leading to a progressive impairment of work capacity [1], that compromises the effectiveness of therapeutic treatment and constitutes a stronger hallmark of poor prognosis in cancer patients [2]. Currently, muscle wasting caused by cancer is used as a pointer for survival prognosis [3,4,5]. Studies suggest that muscle wasting during cancer results from an imbalance between degradation and protein synthesis, mediated specially by cytokines and reactive oxygen species (ROS) [6, 7]. The upregulation of pro-inflammatory cytokines and ROS formation may promote muscular catabolism via the ubiquitin–proteasome (Ub) system, which is considered the main mechanism responsible for the enhanced muscle protein degradation in cancer cachexia [8]. Muscle atrogenes F-Box (MAFbx)/Atrogin-1 and muscle ring-finger-1 (MuRF-1) are two muscle-specific E3 ubiquitin ligases that promote polyubiquitination of proteins to target them for proteolysis by the Ub system [3]; the skeletal muscle protein expression of Atrogin-1 and MuRF-1 are increased in skeletal muscle under atrophy-inducing different conditions, including cancer cachexia [9].
After its popularization in the sports field in the 1990s, creatine supplementation has been introduced in the medical field due to its therapeutic and prophylactic effects on diseases involving muscle loss, such as Duchenne syndrome, amyotrophic lateral sclerosis, and disuse atrophy, among others [10,11,12,13,14,15,16,17]. The proposed mechanisms for the action of creatine in these diseases are based on their interaction with cellular bioenergetics (creatine phosphate system) due to its capacity to increase the mitochondria ATP pool and energetic regulation (the pleiotropic effect of creatine supplementation is addressed by Wallimann et al. [18], while the therapeutic role of creatine is revised by Gualano et al. [11]). Recently, creatine supplementation has demonstrated antioxidant properties as well as effectiveness to counteracting elevated pro-inflammatory cytokines [16, 19,20,21,22,23]. Despite the promising results, to date only two papers effectively have studied the effects of creatine supplementation on cancer cachexia. Deminice et al. [24] and Campos-Ferraz et al. [20] demonstrated that creatine supplementation can prevent body weight loss and tumor growth, and it presents anti-inflammatory effect in tumor-bearing rats. However, the effects of creatine supplementation on cancer-induced muscle wasting and its mechanisms of action remain unknown.
Therefore, the aim of this study was to investigate the effects of creatine supplementation on muscle wasting in Walker-256 tumor-bearing rats. We hypothesized that creatine supplementation may mitigate inflammation and oxidative damage brought about by tumor growth, important trigger of proteolytic signalling via Atrogin-1 and MuRF-1.
Methods
Thirty male Wistar rats (initially weighing ~ 220 g) obtained from the Biological Sciences Center, at the State University of Londrina, were housed in collective cages on a 12 h light/dark cycle at a mean temperature of 22 °C, with free access to food and water for the entirety of the experimental protocol (Nuvilab CR1; Nuvital Nutrients Ltda., Curitiba, Brazil). All procedures were approved by the Ethics Committee for Animal Use at the same institution and were in accordance with the ethical standards of Brazilian College of Animal Experimentation as well as the Declaration of Helsinki and its later amendments. Animals were randomly assigned to three groups designated as control (C, n = 10), tumor-bearing (T, n = 10), and tumor-bearing supplemented with creatine (TCr, n = 10). The TCr group was provided 8 g/l creatine monohydrate in their drinking water (1.0 ± 0.1 g/kg/day) for a total of 21 days. After 11 days of creatine supplementation, Walker-256 carcinoma cells were injected subcutaneously into the right flank of the T and TCr animals. Creatine supplementation was maintained after inoculation and the animals were euthanized 10 days after cell implantation. 21 days of creatine supplementation was previously demonstrated to increase intramuscular creatine content [24]. 10 days of tumor growth was chosen based on previous studies demonstrating that it promoted muscle atrophy [25]. During the experiment, food/water intake was measured daily, and the animals’ body weight was measured every 2 days. Body weight gain was determined as gain of body weight in the 10 days between tumor inoculation and euthanasia.
Tumor implantation
Tumor implantation was carried out as previously described by Padilha et al. [25]. Briefly, tumor cells were obtained from ascitic intraperitoneal tumors (2.0 × 106 cells in 0.5 ml PBS) in host animals. The percentage of viable cells was determined by the trypan blue dye exclusion method (nonviable cells stained blue), using a Neubauer chamber. T and TCr groups received a Walker-256 cell suspension (7.0 × 107 cells in 0.5 ml of PBS) injected subcutaneously into the right flank of the animals. Control rats were inoculated in the same region with 0.5 ml of PBS.
Euthanasia and tissue preparation
After 10 days of tumor growth, rats were anesthetised with an intraperitoneal injection of ketamine and xylazine (90 and 10 mg/kg, respectively) and euthanized by exsanguination. Euthanasia was performed between 9 and 12 a.m. Approximately 3 ml of blood was collected from inferior vena cava into heparinized tubes; the blood was then centrifuged at 1000g for 15 min and plasma was collected and stored at − 80 °C until analysis. The soleus and extensor digitorum longus (EDL) were dissected and weighed; the sum of both was used as a gross muscle mass parameter. Half sections of soleus and EDL muscles were quickly frozen in liquid nitrogen and stored at − 80 °C for future analysis, while the remaining sections were prepared for histological analysis (for fiber cross-sectional area assessment). The spleen was also removed, weighted, and prepared for histological analysis. Epididymal and retroperitoneal fat was identified, excised, and weighed; the sum of both was used as the gross fat mass parameter.
Histological analysis
For optical microscopy analysis, one portion of soleus and EDL muscles, as well as spleen were fixed in 4% formaldehyde for 24 h, dehydrated with graded ethanol, and embedded in paraffin blocks as described by Fonseca et al. [26]. Serial sections (5 µm) were performed and stained with hematoxylin and eosin (H&E). For skeletal muscle fibers’ cross-sectional area (CSA) determination, images captured by an optical microscope at a magnification of 200× were quantified (~ 1200 fibers per group). Spleen images captured from an optical microscope at a 200× magnification were used for white spleen pulp and follicle size determination. In both cases, images were processed using ImageJ software (Wayne Rasband, National Institutes of Health, USA).
Cytokines and lipid peroxidation assay
Plasma interleukins necrosis factor-alpha (TNF-α, Ref: #88-7340-88) and interleukin 6 (IL-6, Ref: #88-7064-88) were determined using the ELISA kit Ready-SET-Go from eBioscience (San Diego, CA). The lipid peroxidation marker malonaldehyde (MDA) was measured in the EDL muscle using HPLC (Shimadzu® SPD-20 UV/VIS, Kyoto, Japan) as described by Spirlandelli et al. [27].
Gene expression
Total RNA was isolated from 100 mg of soleus muscle using a RiboPure Kit (Ambion, part number AM 1924, USA). Total RNA was quantified by spectrophometer at OD 260/280 (NanoDrop2000c, ThermoScientific, USA). Additional DNase I treatment (DNA-free Kit, Ambion, part number AM1906, USA) was employed to remove contaminating DNA. cDNA was synthesized from 1000ηg of total RNA using high-capacity cDNA Reverse Transcription Kit (Applied Byosystems, part number 4374966, USA). Quantitative real-time PCR was performed using a 7500 Fast Real-time PCR System (Applied Biosystems, USA). The following Taqman® Gene Expression Assays (Applied Biosystems, USA) were used in this study: Fbxo 32 (F-box protein 32) Rn00591730_m; mTOR (mechanistic target of rapamycin, serine/threonine kinase) Rn00571541_ml. Beta actin was used as the reference gene for the normalization of the reaction. Relative quantification was determined by the 2−ΔΔCT method.
Immunoblotting
EDL and soleus muscle pieces (50 mg) were homogenized in a buffer solution containing 50 mM HEPES, 40 mM NaCl, 2 mM EDTA, 1,5 mM Na3VO4, 50 mM NaF, 10 mM sodium pyrophosphate, 10 mM sodium betaglycerolphosphate, 1% Triton-X 100, and a protease Inhibitor Cocktail (cOmplete™, ROCHE), then centrifuged at 13,000 rpm at 4 °C. The supernatant was isolated for protein assay using QPRO-BCA kit Standard (Cyanagen Srl). After protein quantification the samples were separated on 10% acrilamide gel and transferred to PVDF membrane (Bio-Rad, Immun-Blot®), blocked with 5% non-fat milk and immunoblotted with primary rabbit antibodies FBXO32 (ab74023, Abcam, UK), MuRF-1 (ab172479, Abcam, UK), and GAPDH (G9545, Sigma-Aldrich®). The secondary antibody was Goat Anti-Rabbit IgG (Bio-Rad laboratories, USA). Band densitometries were obtained using Image J software. Membranes contained samples from all studied groups. Normalization was made by dividing the densitometry value of each band of interest by the raw densitometry value of GAPDH [28].
Statistical analyses
Data are reported as mean ± standard deviation. All data were tested for normal distribution by Shapiro–Wilk. Since CSA analysis of soleus and EDL muscles presented abnormal distributions, differences between groups were assessed with a Kruskal–Wallis’ test followed by Dunn’s post hoc. Intergroup differences for the remaining variables were tested with one-way ANOVA followed by Tukey’s post hoc. The significance level was set at P < 0.05 in all cases.
Results
After 10 days of tumor growth and compared to C, tumor-bearing rats demonstrated a significant decrease in body weight gain, which was partially attenuated by creatine supplementation (Fig. 1a). Although tumor-bearing rats demonstrated 9 and 15% reduction in relative muscle and fat mass, respectively, compared to controls, statistics demonstrated no differences in muscle or fat mass between groups (Fig. 1b, c). No differences in food (C 24.6 ± 1.4; T 23.4 ± 1.8; TCr 24.4 ± 1.6 g/day/animal) or water intake (C 41.9 ± 2.2, T 45.5 ± 3.0, TCr 43.2 ± 4.2 ml/day/animal) were observed between groups along the protocol.
Evaluation of general parameters in animals. a Body weight gain after tumor cell inoculation (10 days); b ∑ skeletal muscle weight (soleus and EDL); c ∑ fat weight (epididymal and retroperitoneal) for groups C (control), T (tumor) and TCr (tumor-creatine supplemented). Values are presented as mean ± SD. a,b,cDifferent letters represent statistical difference (P < 0.05) by one-way ANOVA followed by Tukey’s post hoc
Tumor development promoted skeletal muscle atrophy when compared to control, as evidenced by the reduction in the cross-sectional area of soleus and EDL muscles. Muscle atrophy was attenuated in both muscles by creatine supplementation (Fig. 2).
Cross-sectional area of muscle fibers stained with H&E. Scatter plot of the median cross-sectional area (left) and cross-sectional area distribution by occurrence number (right) of a the soleus muscle and bextensor digitorum longus (EDL) muscle; representative images of cross-sectional area of soleus muscle c in groups C (control), T (tumor), and TCr (tumor-creatine supplemented). a,b,cDifferent letters represent statistical difference (P < 0.05) by Kruskal–wallis and Dunn’s post hoc
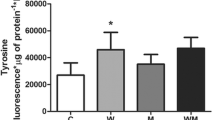
Figure 3 demonstrates that the plasmatic levels of TNF-α and IL-6 in tumor-bearing rats were 1.5 and 3.5-fold higher, respectively, when compared to C. In contrast, creatine supplementation prevented elevated TNF-α and IL-6 plasma concentration (Fig. 3a, b). Creatine supplementation also mitigated tumor-induced elevated lipid peroxidation markers MDA (Fig. 4c) Creatine supplementation also prevented increased follicle and white spleen pulp size induced by tumor growth, despite not preventing splenomegaly (Fig. 3d–g).
Systemic markers of inflammation status. a Plasmatic tumor necrosis factor-alpha (TNF-α); b interleukin 6 (IL-6) and c interleukin 10 (IL-10). d Spleen weight; e H&E-stained spleen sections for analysis of f follicle and white spleen pulp size. Representative images of spleen histology, indicates white spleen pulp and g follicle size of groups C (control), T (tumor) and TCr (tumor-creatine supplemented). Values are presented as mean ± SD. a,b,cDifferent letters represent statistical difference (P < 0.05) by one-way ANOVA followed by Tukey’s post hoc
Evaluation of protein synthesis and degradation in the analyzed skeletal muscles. a Skeletal muscle mRNA levels of mTOR and Atrogin-1. MuRF-1 and Atrogin-1 protein levels in b EDL and c soleus muscles of groups C (control), T (tumor), and TCr (tumor-creatine supplemented). Values are presented as mean ± SD. a,b,cDifferent letters represent statistical difference (P < 0.05) by one-way ANOVA followed by Tukey’s post hoc
mRNA and protein levels of key triggers of protein degradation are presented in Fig. 4. Creatine-supplemented tumor-bearing rats presented lower Atrogin-1 mRNA levels when compared to both C and T groups (Fig. 4a). Creatine supplementation also prevented tumor-induced increases in MuRF-1 and Atrogin-1 protein content in the EDL muscle (Fig. 5b). This pattern, however, was not observed in the soleus muscle (Fig. 4c).
Discussion
As loss of muscle mass and weakness are key factors for cancer cachexia and patient survival, the counteraction of muscle wasting is emerging as a therapy of choice to combat cancer cachexia. Since creatine has emerged as a therapeutic adjuvant in several muscle-wasting disorders [10,11,12,13,14,15,16,17], we propose a study to investigate the possible anti-atrophy effects of creatine supplementation against cancer-induced muscle wasting. Our results clearly demonstrated that creatine supplementation effectively prevents tumor-induced body weight loss and muscle wasting by decreasing the Atrogin-1 and MuRF-1 proteolysis signaling associated with reduced lipid peroxidation and inflammation markers (see Fig. 5, a schematic illustration of the main results obtained). All of this was more evident in EDL glycolytic compared to the skeletal muscle oxidative soleus.
Although there was no gross modification of total muscle weight as previously demonstrated [25], 10 days of Walker-256 tumor cell inoculation promoted microscopically detected muscle atrophy. Our data demonstrated a reduction of the cross-sectional area in both tumor-bearing soleus and EDL muscles, compared to control rats. This skeletal muscle atrophy was promoted by a catabolic state inherent to systemic organic response against tumor growth, as demonstrated by splenomegaly, altered spleen morphology, elevated plasma interleukins and muscle lipid peroxidation. Indeed, chronic inflammation and ROS formation are both major drivers of cachexia [3]. Nowadays, abundant evidence reveals that oxidative stress [7] and elevated inflammatory cytokines [29,30,31] activate all four proteolytic pathways (the Ub system, autophagy, calpains, and caspase-3) for skeletal muscle protein breakdown. Ub has been demonstrated as the pathway primarily responsible for muscle protein degradation in cancer cachexia [32]. Significant myotube atrophy with Atrogin-1 overexpression was observed in the C2C12 cells treated with TNF-α [33, 34]. Meanwhile, knockdown of Atrogin-1 by small interfering RNA (siRNA) protected C2C12 cells from the adverse effect of TNF-α [8]. Experiments regulating functions in tumor-bearing mice also support the requirement of IL-6 in cachexia. Increased circulating IL-6 in cachectic APCMin/+ is associated with increased Atrogin-1 levels [35]. Thus, the presence of the inflammatory mediators TNF-α and IL-6 triggers E3 ligases that mediate the breakdown of myofibrillar proteins by the Ub and promote muscle atrophy [32]. MuRF-1 and Atrogin-1 are key E3 ligases which mediate sarcomeric breakdown and inhibition of protein synthesis [36]. Thus, Atrogin-1 and MuRF-1 have been demonstrated to be highly specific markers of muscle atrophy including cancer cachexia [8]. Our study clearly demonstrated that a pro-inflammatory environment imposed by tumor growth promoted activation of the catabolic Ub system mediated by upregulation of key E3 ligases MuRF-1 and Atrogin-1.
In the past few years, studies have demonstrated that creatine supplementation prevents muscle loss and function in patients with rheumatoid arthritis [37], chronic obstructive pulmonary disease [38], Duchenne dystrophy [17], and cast immobilization [39]. The authors speculate that this improvement is based on creatine’s ability to increase water retention due to its osmotic properties [39]. This suggested that the cell’s hydration state is an important factor in the control of protein turnover, being related to the MAPK (mitogen-activated protein kinase) pathway, which plays an important role in the regulation of protein synthesis [38, 39]. Other authors believe that the effects of creatine on muscle loss protection are due to (1) its antioxidant action [23], (2) its anti-inflammatory action [40], (3) its ability to stimulate faster differentiation of myoblasts by transcription of myogenic regulatory factors [41, 42] and/or (4) the interaction in degradation pathways by attenuating the levels of p53 (protein related with muscle apoptosis) [43]. Remarkably, our data demonstrated that creatine supplementation was able to prevent overexpression of the key E3 ligases Atrogin-1 and MuRF-1, and then counteract muscle atrophy induced by cancer cachexia. These data are new and pioneering and are probably related to the action of creatine in mitigating oxidative damage and systemic inflammation. The data also agree with other studies that demonstrated the antioxidant effects of creatine [23, 44,45,46]. Lawler et al. [23] demonstrated a direct dose–response relationship of creatine concentration with anion superoxide (O2−), peroxynitrite (ONOO–), and 2,20-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS) as determined by the rate of renewal of the ABTS radical, and concluded that creatine has a significant role as an antioxidant. Studies in vivo from our laboratory confirmed the in vitro findings on the potential of creatine to remove reactive oxygen species [45, 46]. The anti-inflammatory action of creatine has also been demonstrated in rodents and humans [40, 42, 47]. Khanna and Madan [40] were the first to demonstrate creatine protection against inflammation using models of arthritis induced by carrageenan (50–500 mg kg−1), nystatin (500 mg kg−1), and formaldehyde (100–500 mg kg−1). Nomura et al. [47] demonstrated that creatine supplementation inhibited endothelial permeability, neutrophil adhesion, and adhesion molecule expression in cultured endothelial cells treated with H2O2 and TNF-α. Studies in humans demonstrated that creatine supplementation can inhibit elevated TNF-α and IL-6 induced by strenuous exercise [19, 48, 49]. More recently, Campos-Ferraz et al. [20] demonstrated that creatine supplementation reduced plasma levels of IL-6 in a 15-day model of a Walker-256 tumor. Thus, our study provides robust indicatory that the anti-atrophy effects of creatine are inherent to its antioxidant and anti-inflammatory effects that prevent key E3 ligases’ overexpression and severe muscle protein breakdown, even if in a muscle-fiber-dependent manner. This data are novel and particularly relevant since all cancer-induced muscle loss treatments are palliative. Creatine can be a safe and cheap adjuvant tool to counteract muscle loss during cancer.
It is noteworthy that, although tumor growth could promote atrophy in both the soleus and EDL muscles, Atrogin-1 and MuRF-1-dependent proteolytic pathway activation is more preeminent in the EDL muscle. It is in accordance with the previous studies demonstrating that fast-twitch glycolytic fibers such as EDL are more vulnerable than slow-twitch oxidative fibers such as soleus under a variety of atrophic conditions, including cancer cachexia [50]. Interestingly, our study demonstrated that creatine supplementation could prevent muscle atrophy in both slow-twitch soleus and fast-twitch EDL muscles. Creatine is taken up by both slow and fast-twitch muscle fibers, but fast-twitch fibers have a greater capacity for creatine storage than slow-twitch [18]. Whether fast-twitch fibers are more susceptible to creatine and phosphocreatine loss under muscle-wasting conditions such as cachexia is unknown.
In conclusion, our findings provide initial evidence that creatine supplementation mitigates skeletal muscle wasting resulting from cancer cachexia. Remarkably, creatine supplementation prevents skeletal muscle atrophy by attenuating tumor-induced oxidative damage and pro-inflammatory environment. This condition decreases the expression of important regulators of ubiquitin proteasome-mediated skeletal muscle protein breakdown such as Atrogin-1 and MuRF-1.
References
Tan BHL, Fearon KCH (2008) Cachexia: prevalence and impact in medicine. Curr Opin Clin Nutr Metab Care 11:400–407
Galvão DA, Spry NA, Taaffe DR et al (2008) Changes in muscle, fat and bone mass after 36 weeks of maximal androgen blockade for prostate cancer. BJU Int 102:44–47. https://doi.org/10.1111/j.1464-410X.2008.07539.x
Argilés JM, Busquets S, Stemmler B, López-Soriano FJ (2014) Cancer cachexia: understanding the molecular basis. Nat Rev Cancer 14:754–762
Lenk K, Schuler G, Adams V (2010) Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J Cachexia Sarcopenia Muscle 1:9–21
Penna F, Bonetto A, Muscaritoli M et al (2010) Muscle atrophy in experimental cancer cachexia: is the IGF-1 signaling pathway involved? Int J Cancer 127:1706–1717. https://doi.org/10.1002/ijc.25146
Balkwill FR, Mantovani A (2012) Cancer-related inflammation: common themes and therapeutic opportunities. Semin Cancer Biol 22:33–40
Powers SK, Morton AB, Ahn B, Smuder AJ (2016) Redox control of skeletal muscle atrophy. Free Radic Biol Med 98:208–217. https://doi.org/10.1016/j.freeradbiomed.2016.02.021
Yuan L, Han J, Meng Q et al (2015) Muscle-specific E3 ubiquitin ligases are involved in muscle atrophy of cancer cachexia: an in vitro and in vivo study. Oncol Rep 33:2261–2268. https://doi.org/10.3892/or.2015.3845
Gomes-Marcondes MCC, Tisdale MJ (2002) Induction of protein catabolism and the ubiquitin-proteasome pathway by mild oxidative stress. Cancer Lett 180:69–74. https://doi.org/10.1016/S0304-3835(02)00006-X
Johnston APW, Burke DG, MacNeil LG, Candow DG (2009) Effect of creatine supplementation during cast-induced immobilization on the preservation of muscle mass, strength, and endurance. J Strength Cond Res 23:116–120. https://doi.org/10.1519/JSC.0b013e31818efbcc
Gualano B, Artioli GG, Poortmans JR, Lancha Junior AH (2010) Exploring the therapeutic role of creatine supplementation. Amino Acids 38:31–44. https://doi.org/10.1007/s00726-009-0263-6
Gualano B, Roschel H, Lancha AH et al (2012) In sickness and in health: the widespread application of creatine supplementation. Amino Acids 43:519–529. https://doi.org/10.1007/s00726-011-1132-7
Mazzini L, Balzarini C, Colombo R et al (2001) Effects of creatine supplementation on exercise performance and muscular strength in amyotrophic lateral sclerosis: preliminary results. J Neurol Sci 191:139–144. https://doi.org/10.1016/S0022-510X(01)00611-6
Menezes LG, Sobreira C, Neder L et al (2007) Creatine supplementation attenuates corticosteroid-induced muscle wasting and impairment of exercise performance in rats. J Appl Physiol 102:698–703. https://doi.org/10.1152/japplphysiol.01188.2005
Sakkas GK, Schambelan M, Mulligan K (2009) Can the use of creatine supplementation attenuate muscle loss in cachexia and wasting? Curr Opin Clin Nutr Metab Care 12:623–627
Smith RN, Agharkar AS, Gonzales EB (2014) A review of creatine supplementation in age-related diseases: more than a supplement for athletes. F1000 Res 3:222–233. https://doi.org/10.12688/f1000research.5218.1
Tarnopolsky MA, Mahoney DJ, Vajsar J et al (2004) Creatine monohydrate enhances strength and body composition in Duchenne muscular dystrophy. Neurology 62:1771–1777. https://doi.org/10.1212/01.WNL.0000125178.18862.9D
Wallimann T, Tokarska-Schlattner M, Schlattner U (2011) The creatine kinase system and pleiotropic effects of creatine. Amino Acids 40:1271–1296. https://doi.org/10.1007/s00726-011-0877-3
Bassit RA, Curi R, Costa Rosa LFBP (2008) Creatine supplementation reduces plasma levels of pro-inflammatory cytokines and PGE2 after a half-ironman competition. Amino Acids 35:425–431. https://doi.org/10.1007/s00726-007-0582-4
Campos-Ferraz PL, Gualano B, das Neves W et al (2016) Exploratory studies of the potential anti-cancer effects of creatine. Amino Acids 48:1993–2001. https://doi.org/10.1007/s00726-016-2180-9
Fimognari C, Sestili P, Lenzi M et al (2009) Protective effect of creatine against RNA damage. Mutat Res Fundam Mol Mech Mutagen 670:59–67. https://doi.org/10.1016/j.mrfmmm.2009.07.005
Guidi C, Potenza L, Sestili P et al (2008) Differential effect of creatine on oxidatively-injured mitochondrial and nuclear DNA. Biochim Biophys Acta Gen Subj 1780:16–26. https://doi.org/10.1016/j.bbagen.2007.09.018
Lawler JM, Barnes WS, Wu G et al (2002) Direct antioxidant properties of creatine. Biochem Biophys Res Commun 290:47–52. https://doi.org/10.1006/bbrc.2001.6164
Deminice R, Cella PS, Padilha CS et al (2016) Creatine supplementation prevents hyperhomocysteinemia, oxidative stress and cancer-induced cachexia progression in Walker-256 tumor-bearing rats. Amino Acids 48:2015–2024. https://doi.org/10.1007/s00726-016-2172-9
Guarnier FA, Cecchini AL, Suzukawa AA et al (2010) Time course of skeletal muscle loss and oxidative stress in rats with walker 256 solid tumor. Muscle Nerve 42:950–958. https://doi.org/10.1002/mus.21798
Padilha CS, Borges FH, Costa Mendes da Silva LE et al (2017) Resistance exercise attenuates skeletal muscle oxidative stress, systemic pro-inflammatory state, and cachexia in Walker-256 tumor-bearing rats. Appl Physiol Nutr Metab 42:916–923. https://doi.org/10.1139/apnm-2016-0436
Fonseca H, Powers SK, Gonalves D et al (2012) Physical inactivity is a major contributor to ovariectomy-induced sarcopenia. Int J Sports Med 33:268–278. https://doi.org/10.1055/s-0031-1297953
Magdalon J, Chimin P, Belchior T et al (2016) Constitutive adipocyte mTORC1 activation enhances mitochondrial activity and reduces visceral adiposity in mice. Biochim Biophys Acta Mol Cell Biol Lipids 1861:430–438. https://doi.org/10.1016/j.bbalip.2016.02.023
Londhe P, Guttridge DC (2015) Inflammation induced loss of skeletal muscle. Bone 80:131–142. https://doi.org/10.1016/j.bone.2015.03.015
Carson JA, Baltgalvis KA (2010) Interleukin 6 as a key regulator of muscle mass during cachexia. Exerc Sport Sci Rev 38:168–176. https://doi.org/10.1097/JES.0b013e3181f44f11
Narsale AA, Carson JA (2014) Role of interleukin-6 in cachexia: therapeutic implications. Curr Opin Support Palliat Care 8:321–327. https://doi.org/10.1097/SPC.0000000000000091
Johns N, Stephens NA, Fearon KCH (2013) Muscle wasting in cancer. Int J Biochem Cell Biol 45:2215–2229. https://doi.org/10.1016/j.biocel.2013.05.032
De Larichaudy J, Zufferli A, Serra F et al (2012) TNF- α and tumor-induced skeletal muscle atrophy involves sphingolipid metabolism. Skelet Muscle 2:2–20. https://doi.org/10.1186/2044-5040-2-2
Moylan JS, Smith JD, Chambers MA et al (2008) TNF-α induction of atrogin-1/MAFbx mRNA depends on Foxo4 expression but not AKT-Foxo1/3 signaling. AJP Cell Physiol 295:C986–C993. https://doi.org/10.1152/ajpcell.00041.2008
Baltgalvis KA, Berger FG, Peña MMO et al (2009) Muscle wasting and interleukin-6-induced atrogin-I expression in the cachectic ApcMin/+mouse. Pflugers Arch Eur J Physiol 457:989–1001. https://doi.org/10.1007/s00424-008-0574-6
Glass DJ (2010) Signaling pathways perturbing muscle mass. Curr Opin Clin Nutr Metab Care 13:225–229. https://doi.org/10.1097/MCO.0b013e32833862df
Wilkinson TJ, Lemmey AB, Jones JG et al (2016) Can creatine supplementation improve body composition and objective physical function in rheumatoid arthritis patients? A Randomized Controlled Trial. Arthritis Care Res (Hoboken) 68:729–737. https://doi.org/10.1002/acr.22747
Fuld JP, Kilduff LP, Neder JA et al (2005) Creatine supplementation during pulmonary rehabilitation in chronic obstructive pulmonary disease. Thorax 60:531–537. https://doi.org/10.1136/thx.2004.030452
Aoki MS, Lima WP, Miyabara EH et al (2004) Deleteriuos effects of immobilization upon rat skeletal muscle: role of creatine supplementation. Clin Nutr 23:1176–1183. https://doi.org/10.1016/j.clnu.2004.03.004
Khanna NK, Madan BR (1978) Studies on the anti-inflammatory activity of creatine. Arch Int Pharmacodyn Thérapie 231:340–350
Sestili P, Ambrogini P, Barbieri E et al (2016) New insights into the trophic and cytoprotective effects of creatine in in vitro and in vivo models of cell maturation. Amino Acids 48:1897–1911. https://doi.org/10.1007/s00726-015-2161-4
Barbieri E, Guescini M, Calcabrini C et al (2016) Creatine prevents the structural and functional damage to mitochondria in myogenic, oxidatively stressed C2C12 cells and restores their differentiation capacity. Oxid Med Cell Longev 5152029:1–12. https://doi.org/10.1155/2016/5152029
Rahimi R, Mirzaei B, Rahmani-Nia F, Salehi Z (2015) Effects of creatine monohydrate supplementation on exercise-induced apoptosis in athletes: a randomized, double-blind, and placebo-controlled study. J Res Med Sci 20:733–738. https://doi.org/10.4103/1735-1995.168320
Sestili P, Martinelli C, Colombo E et al (2011) Creatine as an antioxidant. Amino Acids 40:1385–1396
Deminice R, Portari GV, Vannucchi H, Jordao AA (2009) Effects of creatine supplementation on homocysteine levels and lipid peroxidation in rats. Br J Nutr 102:110–116. https://doi.org/10.1017/S0007114508162985
Deminice R, da Silva RP, Lamarre SG et al (2011) Creatine supplementation prevents the accumulation of fat in the livers of rats fed a high-fat diet. J Nutr 141:1799–1804. https://doi.org/10.3945/jn.111.144857
Nomura A, Zhang M, Sakamoto T et al (2003) Anti-inflammatory activity of creatine supplementation in endothelial cells in vitro. Br J Pharmacol 139:715–720. https://doi.org/10.1038/sj.bjp.0705316
Santos RVT, Bassit RA, Caperuto EC, Costa Rosa LFBP (2004) The effect of creatine supplementation upon inflammatory and muscle soreness markers after a 30 km race. Life Sci 75:1917–1924. https://doi.org/10.1016/j.lfs.2003.11.036
Deminice R, Rosa FT, Franco GS et al (2013) Effects of creatine supplementation on oxidative stress and inflammatory markers after repeated-sprint exercise in humans. Nutrition 29:1127–1132. https://doi.org/10.1016/j.nut.2013.03.003
Wang Y, Pessin JE (2013) Mechanisms for fiber-type specificity of skeletal muscle atrophy. Curr Opin Clin Nutr Metab Care 16:243–250. https://doi.org/10.1097/MCO.0b013e328360272d
Acknowledgements
Supported by CAPES-Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, Brazil #88881.068035/2014-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that there is no potential conflict of interests regarding this article.
Rights and permissions
About this article
Cite this article
Cella, P.S., Marinello, P.C., Borges, F.H. et al. Creatine supplementation in Walker-256 tumor-bearing rats prevents skeletal muscle atrophy by attenuating systemic inflammation and protein degradation signaling. Eur J Nutr 59, 661–669 (2020). https://doi.org/10.1007/s00394-019-01933-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-019-01933-6