Abstract
Background
Mitochondria are the main cellular sites devoted to ATP production and lipid oxidation. Therefore, the mitochondrial dysfunction could be an important determinant of cellular fate of circulating lipids, that accumulate in the cytoplasm, if they are not oxidized. The ectopic fat accumulation is associated with the development of insulin resistance, and a link between mitochondrial dysfunction and insulin resistance has been proposed.
Methods
Recent data on the possible link existing between mitochondrial dysfunction in the liver and diet-induced obesity will be summarized, focusing on the three factors that affect the mitochondrial oxidation of metabolic fuels, i.e. organelle number, organelle activity, and energetic efficiency of the mitochondrial machinery in synthesizing ATP. Search in PubMed relevant articles from 2003 to 2014 was conducted, by using query “liver mitochondria and obesity” “hepatic mitochondria and obesity” “liver mitochondria and high fat diet” and “hepatic mitochondria and high fat diet” and including related articles by the same groups.
Results
Several works, by using different physiological approaches, have dealt with alteration in mitochondrial function in obesity and diabetes. Most results show that hepatic mitochondrial function is impaired in models of obesity and insulin resistance induced by high-fat or high-fructose feeding.
Conclusions
Since mitochondria are the main producers of both cellular energy and free radicals, dysfunctional mitochondria could play an important role in the development of insulin resistance and ectopic fat storage in the liver, thus supporting the emerging idea that mitochondrial dysfunction is closely related to the development of obesity, type 2 diabetes mellitus and non-alcoholic steatohepatitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
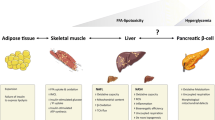
Hyperlipidic–hypercaloric diets are now frequently consumed in modern societies, coupled with low levels of physical activity. These factors contribute importantly to the development of pathological conditions, which include obesity, hypertension, insulin resistance, dyslipidemia, and liver diseases. The liver is a central player in the physiological regulation of whole-body energy homeostasis as well as in the pathogenesis of the epidemiologically relevant metabolic disorders, such as obesity and diabetes. In particular, chronic dietary overload with fructose and saturated fatty acids, typical of western societies, will enhance accumulation of lipid metabolites and oxidative stress in liver [1–3]. The ectopic fat accumulation in liver is tightly associated with the development of insulin resistance [4, 5]. In fact, hepatic accumulation of diacylglycerol (DAG) and ceramide, as well as DAG-induced activation of protein kinase C, can impair insulin signaling, most notably at the level of the insulin receptor substrates [6–9].
The rate at which fat accumulates in tissues is determined by several factors, such as the rate of lipid uptake from the circulation and the utilization of lipids within the tissues [10]. Mitochondria are the main cellular sites devoted to fatty acid oxidation. For these reasons, a role for mitochondrial dysfunction in the onset of insulin resistance has been proposed and a number of studies have dealt with possible alteration in mitochondrial function in obesity and diabetes, both in humans and animal models, using different experimental paradigms and with different approaches. In particular, it should be taken into account that the mitochondrial oxidation of metabolic fuels depends on organelle number, organelle activity, and energetic efficiency of the mitochondrial machinery in synthesizing ATP from the oxidation of fuels. Therefore, the main goal of this review was to collect and analyze the available data on liver mitochondria and diet-induced obesity with the focus on all the three above parameters. Search in PubMed of relevant articles from 2003 to 2014 was conducted, by using query “liver mitochondria and obesity” “hepatic mitochondria and obesity” “liver mitochondria and high fat diet” and “hepatic mitochondria and high fat diet” with the inclusion of related articles by the same groups. A summary of the obtained results is presented in Tables 1 and 2.
Mitochondrial functionality and insulin resistance
Mitochondria are key organelles in energy metabolism, especially in tissues with high metabolic activity, such as liver. Therefore, mitochondrial dysfunction could play an important role in the pathogenesis of the metabolic disorders.
Mitochondrial production of reactive oxygen species (ROS) is frequently reported to be increased in the physiopathology of insulin resistance and could cause damage to cellular macromolecules, thus causing damage to cellular structures, including mitochondria. Mitochondrial impairment would lead to a decreased oxidative capacity, thus favoring intracellular lipid storage that is considered a key player in the development of insulin resistance.
An alternative pathway leading to hepatic insulin resistance could involve an elevated β-oxidation [11–14], that is viewed as an adaptive mechanism, but provides large amounts of reduced equivalents (NADH, H+ and FADH2) and electrons to the respiratory chain regardless of the ATP demand. Thus, oxidative phosphorylation would be unbalanced, promoting successively increasing ROS production, mitochondrial and cellular damages, and reduction of insulin signal transduction.
Several works, by using different physiological approaches, have investigated the relationship between onset of insulin resistance and mitochondrial functioning in liver, that exerts a deep impact on glucose homeostasis. These studies have included measurements of mitochondrial mass and function and are based on assessment of mitochondrial membrane potential, proton leak kinetics, mitochondrial content by ultrastructural observations, citrate synthase activity, ratio of mitochondrial relative to nuclear DNA, polarographic determination of oxygen consumption rates, enzyme activities of mitochondrial respiratory complexes I–V, markers of oxidative stress such as lipid peroxidation products, and antioxidant capacity such as superoxide dismutase specific activity [15–22]. The results that have been obtained report either decreased, unchanged or even increased hepatic mitochondrial function and oxidative phosphorylation capacity in insulin resistant states.
Mitochondrial functionality and high-fat diet
In rats fed a high-fat diet, a loss of cristae in hepatic mitochondria has been shown, as well as swollen mitochondria and decreased matrix density [23, 24]. When considering mitochondrial respiration and ATP production, the activity assessed in isolated liver mitochondria from rats exposed to a high-fat diet has been found either decreased [19], unchanged [25] or even increased [26] when compared with controls. Several discrepancies exist regarding possible high-fat diet-induced changes in mitochondrial respiratory chain activity and respiration. Cytochrome oxidase activity has been found increased [27], unchanged [25, 28] or reduced [18, 29]. State 3 oxygen consumption in isolated liver mitochondria with different substrates was either reported as unchanged [25, 28, 30–32], increased [33, 34] or significantly reduced [18, 29, 35–37].
Mitochondria generate most of the energy used by cells, and the efficiency with which ATP is synthesized by mitochondrial oxidative phosphorylation is dependent on mitochondrial coupling. Excess in energy intake and/or high degree of mitochondrial coupling cause an increase in proton motive force to a maximum, with respiratory complexes that become highly reduced and may release electrons directly to oxygen resulting in a higher ROS production, thus altering cell functioning and leading to several pathologies. Therefore, it appears important to study the link between mitochondria and insulin resistance with a focus on the degree of mitochondrial coupling. Again, when examining the results obtained in literature, the efficiency of oxidative phosphorylation and the mitochondrial membrane potential were either increased [28] or unchanged [19, 25, 33, 38].
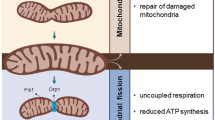
To gain more insight into this link, we have used a rat model that displays several correlates human obesity [39]. In these high-fat fed rats, the combination of slight increases in metabolisable energy intake and slight decreases in energy expenditure resulted in positive energy balance that cumulated over the 7-week study period to result in marked increases in body energy gain and lipid gain; the latter resulting in part from an increase in metabolic efficiency [39]. Other metabolic characteristics that resembles human obesity in the above rats fed a high-fat diet for 7 weeks are insulin resistance and hepatic steatosis [39], a common complication of diet-induced obesity [40]. Since mitochondria are the major cellular site involved in fatty acid metabolism and the main source of ROS, they could play a key role in ectopic fat storage and related complications. An increase in mitochondrial protein mass together with a significant decrease in State 3 respiratory capacities were found in rats fed high-fat diet [39]. These modifications of mitochondrial compartment are similar to those found in response to aging [41] and oxidative stress [42]. The results strongly suggest that high-fat feeding causes an early onset of mitochondrial decay in adult rats. An additional mechanism that can regulate mitochondrial energy production is the degree of coupling of oxidative phosphorylation, which in turn depends on mitochondrial inner membrane permeability to protons (proton leak). The significant decrease in proton leak exhibited by mitochondria from rats fed a high-fat diet suggests an increase in mitochondrial coupling in this condition. When mitochondrial coupling is higher, less substrates need to be burned to obtain a given amount of ATP, with a following decrease in liver ability to fatty acids delivered from the blood. In addition, in coupled mitochondria, an increase in the production of ROS by the respiratory chain could take place, since one of the postulated roles for mitochondrial proton leak is to maintain membrane potential below the critical threshold for ROS production [43]. The results showed an increased oxidative damage in rats fed a high-fat diet, with no compensatory increase in antioxidant by SOD activity [39], a condition that contributes to the development of insulin resistance and hepatic disease [44].
Similar alterations in hepatic mitochondrial protein mass, capacity and degree of oxidative stress were found when rats fed a high-fat diet for only 2 weeks [45, 46], at a time point when no alteration of insulin signaling could be detected [45, 46]. Accordingly, in hyperphagic obese OLETF rats it has been found that hepatic mitochondrial dysfunction precedes the development of insulin resistance and hepatic steatosis [47]. Taken together, these results suggest that the above modifications of mitochondrial compartment in liver precede and can contribute to the subsequent development of insulin resistance.
Mitochondrial functionality and fructose-rich diet
Diet-induced obesity and insulin resistance can also be elicited by fructose-rich diets. In fact, dietary fructose intake has risen considerably in the last decades due to increase in the consumption of pre-packaged foods, soft drinks and juice beverages containing sucrose or high-fructose corn syrup [48–50]. In addition, the 25 % increase in fructose consumption over the past 30 years coincides closely with the increase in the prevalence of obesity [48–50] and in the risk of diabetes, cardiometabolic disease and gout, as well as with lipid disturbances [51]. In humans it is difficult to assess the contribution of fructose intake alone to the development of the above metabolic disorders, since, in everyday life, additional factors are involved, such as hypercaloric diet rich in saturated fat and low physical activity. For these reasons, animal models could help to shed light on the role of dietary fructose on excessive lipid depots and correlated metabolic diseases. Following long-term intake of a fructose-rich low fat diet in adult, sedentary rats we have found several metabolic derangements typical of human obesity, such as increased body lipids [52], ectopic lipid deposition and altered insulin sensitivity [53]. In addition, a stimulation of whole-body and hepatic net de novo lipogenesis contributes to excess lipid accumulation in our fructose-fed rats. This latter result fits well with literature data showing an increased de novo lipogenesis in humans after long-term fructose feeding [54, 55] as well as with several animal studies reporting that hepatic de novo lipogenesis is stimulated by fructose intake, alone [56, 57] or in combination with high dietary fat [46]. On the other hand, the effect of fat feeding on hepatic de novo lipogenesis is less clear, since this metabolic pathway has been found reduced [56–60] or even increased [61–63].
Using our animal model to study the metabolic effects of fructose, we have also found alteration in hepatic mitochondrial energetics [64]. Respiratory capacities evaluated in isolated liver mitochondria were found unchanged, while ATP needed for biosynthetic pathways is obtained at a lower cost, since hepatic mitochondria display increased degree of coupling and are less responsive to the uncoupling effect of fatty acids. Higher coupling efficiency implies lower fuel burning that could partly explain the higher body lipids found in fructose-fed rats. Another unwanted consequence of the increased degree of coupling is higher ROS production, and in fact, hepatic mitochondria showed signs of oxidative damage, both in the lipid and in the protein component, together with decreased activity of SOD, one of the enzymatic component of the antioxidant system. After short-term feeding with a fructose-rich diet, at variance with the results obtained with high-fat diet [45, 46], other groups have found reduced insulin sensitivity [65], together with increased oxidative stress in liver [66], in face of unchanged mitochondrial capacity [67]. Interestingly, higher hepatic mitochondrial efficiency and oxidative damage have also been found in rats fed high-fat diet [39], indicating similar effects of fructose-rich or high-fat diet, while the two diets exhibit a different effect on mitochondrial oxidative capacity (Table 2).
Conclusions
It is clear that hepatic mitochondrial function is impaired by high-fat or high-fructose feeding. Since mitochondria are the main producers of both cellular energy and free radicals, dysfunctional mitochondria can play an important role in the development of insulin resistance and ectopic fat storage in the liver, thus supporting the emerging idea that mitochondrial dysfunction could be closely related to the development of metabolic diseases, such as obesity, type 2 diabetes mellitus and non-alcoholic steatohepatitis.
References
Roden M (2006) Mechanisms of disease: hepatic steatosis in type 2 diabetes–pathogenesis and clinical relevance. Nature Clin Pract Endocrinol Metab 2:335–448
Smith BW, Adams LA (2011) Non-alcoholic fatty liver disease. Crit Rev Clin Lab Sci 48:97–113
Rolo AP, Teodoro JS, Palmeira CM (2012) Role of oxidative stress in the pathogenesis of nonalcoholic steatohepatitis. Free Radic Biol Med 52:59–69
Szendroedi J, Roden M (2009) Ectopic lipids and organ function. Curr Opin Lipidol 20:50–56
Takamura T, Misu H, Ota T, Kaneko S (2012) Fatty liver as a consequence and cause of insulin resistance: lessons from type 2 diabetic liver. Endocr J 59:745–763
Samuel VT, Liu ZX, Qu X, Elder BD, Bilz S, Befroy D et al (2004) Mechanism of hepatic insulin resistance in non-alcoholic fatty liver disease. J Biol Chem 279:32345–32353
Kumashiro N, Erion DM, Zhang D, Kahn M, Beddow SA, Chu X et al (2011) Cellular mechanism of insulin resistance in nonalcoholic fatty liver disease. Proc Natl Acad Sci USA 108:16381–16385
Jornayvaz FR, Shulman GI (2012) Diacylglycerol activation of protein kinase Cε and hepatic insulin resistance. Cell Metab 15:574–584
Schmitz-Peiffer C, Biden TJ (2012) Protein kinase C function in muscle, liver, and beta-cells and its therapeutic implications for type 2 diabetes. Diabetes 57:1774–1783
Turner N, Heilbronn LK (2008) Is mitochondrial dysfunction a cause of insulin resistance? Trends Endocrinol Metab 19:324–330
Pessayre D, Fromenty B, Mansouri A (2004) Mitochondrial injury in steatohepatitis. Eur J Gastroenterol Hepatol 16:1095–1105
Pessayre D (2007) Role of mitochondria in non-alcoholic fatty liver disease. J Gastroenterol Hepatol 22(Suppl 1):S20–S27
Silvestri E, Cioffi F, Glinni D, Ceccarelli M, Lombardi A, de Lange P et al (2010) Pathways affected by 3,5-diiodo-l-thyronine in liver of high fat-fed rats: evidence from two-dimensional electrophoresis, blue-native PAGE, and mass spectrometry. Mol BioSyst 6(11):2256–2271
de Lange P, Cioffi F, Senese R, Moreno M, Lombardi A, Silvestri E et al (2011) Nonthyrotoxic prevention of diet-induced insulin resistance by 3,5-diiodo-l-thyronine in rats. Diabetes 60(11):2730–2739
Pérez-Carreras M, Del Hoyo P, Martín MA, Rubio JC, Martín A, Castellano G et al (2003) Defective hepatic mitochondrial respiratory chain in patients with nonalcoholic steatohepatitis. Hepatology 38:999–1007
Lockman KA, Nyirenda MJ (2010) Interrelationships between hepatic fat and insulin resistance in non-alcoholic fatty liver disease. Curr Diab Rev 6:341–347
Vial G, Dubouchaud H, Leverve XM (2010) Liver mitochondria and insulin resistance. Acta Biochim Pol 57:389–392
Vial G, Dubouchaud H, Couturier K, Cottet-Rousselle C, Taleux C, Athias A et al (2011) Effects of a high-fat diet on energy metabolism and ROS production in rat liver. J Hepatol 54:348–356
Bouderba S, Sanz MN, Sánchez-Martín C, El-Mir MY, Villanueva GR, Detaille D et al (2012) Hepatic mitochondrial alterations and increased oxidative stress in nutritional diabetes-prone Psammomys obesus model. Exp Diab Res 2012:430176
Yu L, Fink BD, Herlein JA, Oltman CL, Lamping KG, Sivitz WI (2014) Dietary fat, fatty acid saturation and mitochondrial bioenergetics. J Bioenerg Biomembr 46(1):33–44
Satapati S, Sunny NE, Kucejova B, Fu X, He TT, Méndez-Lucas A et al (2012) Elevated TCA cycle function in the pathology of diet-induced hepatic insulin resistance and fatty liver. J Lipid Res 53(6):1080–1092
Enos RT, Velázquez KT, Murphy EA (2014) Insight into the impact of dietary saturated fat on tissue-specific cellular processes underlying obesity-related diseases. J Nutr Biochem 25(6):600–612
Lieber CS, Leo MA, Mak KM, Xu Y, Cao Q, Ren C et al (2004) Model of nonalcoholic steatohepatitis. Am J Clin Nutr 79:502–509
Kathirvel E, Morgan K, French SW, Morgan TR (2013) Acetyl-l-carnitine and lipoic acid improve mitochondrial abnormalities and serum levels of liver enzymes in a mouse model of nonalcoholic fatty liver disease. Nutr Res 33(11):932–941
Flamment M, Arvier M, Gallois Y, Simard G, Malthièry Y, Ritz P et al (2008) Fatty liver and insulin resistance in obese Zucker rats: no role for mitochondrial dysfunction. Biochimie 90:1407–1413
Buchner DA, Yazbek SN, Solinas P, Burrage LC, Morgan MG, Hoppel CL et al (2011) Increased mitochondrial oxidative phosphorylation in the liver is associated with obesity and insulin resistance. Obesity 19(5):917–924
Valdecantos MP, Pérez-Matute P, González-Muniesa P, Prieto-Hontoria PL, Moreno-Aliaga MJ, Martínez JA (2012) Lipoic acid administration prevents nonalcoholic steatosis linked to long-term high-fat feeding by modulating mitochondrial function. J Nutr Biochem 23:1676–1684
Flamment M, Rieusset J, Vidal H, Simard G, Malthièry Y, Fromenty B et al (2012) Regulation of hepatic mitochondrial metabolism in response to a high fat diet: a longitudinal study in rats. J Physiol Biochem 68:335–344
Nadal-Casellas A, Amengual-Cladera E, Proenza AM, Lladó I, Gianotti M (2010) Long-term high-fat-diet feeding impairs mitochondrial biogenesis in liver of male and female rats. Cell Physiol Biochem 26:291–302
Oliveira CP, Coelho AM, Barbeiro HV, Lima VM, Soriano F, Ribeiro C et al (2006) Liver mitochondrial dysfunction and oxidative stress in the pathogenesis of experimental nonalcoholic fatty liver disease. Braz J Med Biol Res 39:189–194
Ciapaite J, Bakker SJ, Van Eikenhorst G, Wagner MJ, Teerlink T, Schalkwijk CG et al (2007) Functioning of oxidative phosphorylation in liver mitochondria of high-fat diet fed rats. Biochim Biophys Acta 1772:307–316
Franko A, von Kleist-Retzow JC, Neschen S, Wu M, Schommers P, Böse M et al (2014) Liver adapts mitochondrial function to insulin resistant and diabetic states in mice. J Hepatol 60(4):816–823
Ciapaite J, van den Broek NM, Te Brinke H, Nicolay K, Jeneson JA, Houten SM et al (2011) Differential effects of short- and long-term high-fat diet feeding on hepatic fatty acid metabolism in rats. Biochim Biophys Acta 1811:441–451
Poussin C, Ibberson M, Hall D, Ding J, Soto J, Abel ED et al (2011) Oxidative phosphorylation flexibility in the liver of mice resistant to high-fat diet-induced hepatic steatosis. Diabetes 60(9):2216–2224
Mantena SK, Vaughn DP, Andringa KK, Eccleston HB, King AL, Abrams GA et al (2009) High fat diet induces dysregulation of hepatic oxygen gradients and mitochondrial function in vivo. Biochem J 417(1):183–193
Teodoro JS, Duarte FV, Gomes AP, Varela AT, Peixoto FM, Rolo AP et al (2013) Berberine reverts hepatic mitochondrial dysfunction in high-fat fed rats: a possible role for SirT3 activation. Mitochondrion 13(6):637–646
Morris EM, Jackman MR, Meers GM, Johnson GC, Lopez JL, MacLean PS et al (2013) Reduced hepatic mitochondrial respiration following acute high-fat diet is prevented by PGC-1α overexpression. Am J Physiol 305(11):G868–G880
Lanni A, Moreno M, Lombardi A, de Lange P, Silvestri E, Ragni M et al (2005) 3,5-diiodo-l-thyronine powerfully reduces adiposity in rats by increasing the burning of fats. FASEB J 19(11):1552–1554
Crescenzo R, Bianco F, Falcone I, Prisco M, Liverini G, Iossa S (2008) Alterations in hepatic mitochondrial compartment in a model of obesity and insulin resistance. Obesity 16:958–964
Carmiel-Haggai M, Cederbaum A, Nieto N (2005) A high-fat diet leads to the progression of non-alcoholic fatty liver disease in obese rats. FASEB J 19:136–138
Navarro A, Boveris A (2007) The mitochondrial energy transduction system and the aging process. Am J Physiol 292(2):C670–C686
Lee HC, Wei YH (2005) Mitochondrial biogenesis and mitochondrial DNA maintenance of mammalian cells under oxidative stress. Int J Biochem Cell Biol 37:822–834
Korshunov SS, Skulachev VP, Starkov AA (1997) High protonic potential actuates a mechanism of production of reactive oxygen species in mitochondria. FEBS Lett 416:15–18
Houstis N, Rosen ED, Lander ES (2006) Reactive oxygen species have a casual role in multiple forms of insulin resistance. Nature 440:944–948
Iossa S, Lionetti L, Mollica MP, Crescenzo R, Botta M, Barletta A et al (2003) Effect of high-fat feeding on metabolic efficiency and mitochondrial oxidative capacity in adult rats. Br J Nutr 90:953–960
Crescenzo R, Bianco F, Coppola P, Mazzoli A, Tussellino M, Carotenuto R et al (2014) Fructose supplementation worsens the deleterious effects of short-term high-fat feeding on hepatic steatosis and lipid metabolism in adult rats. Exp Physiol 99(9):1203–1213
Rector RS, Thyfault JP, Uptergrove GM, Morris EM, Naples SP, Borengasser SJ et al (2010) Mitochondrial dysfunction precedes insulin resistance and hepatic steatosis and contributes to the natural history of non-alcoholic fatty liver disease in an obese rodent model. J Hepatol 52(5):727–736
Bray GA (2010) Soft drink consumption and obesity: it is all about fructose. Curr Opin Lipidol 21:51–57
Tappy L, Lê KA (2010) Metabolic effects of fructose and the worldwide increase in obesity. Physiol Rev 90:23–46
Samuel VT (2011) Fructose induced lipogenesis: from sugar to fat to insulin resistance. Trends Endocrinol Metab 22:60–65
Brown CM, Dulloo AG, Montani JP (2008) Sugary drinks in the pathogenesis of obesity and cardiovascular diseases. Int J Obes 32:S28–S34
Crescenzo R, Bianco F, Coppola P, Mazzoli A, Valiante S, Liverini G et al (2014) Adipose tissue remodeling in rats exhibiting fructose-induced obesity. Eur J Nutr 53:413–419
Crescenzo R, Bianco F, Coppola P, Mazzoli A, Cigliano L, Liverini G et al (2013) Increased skeletal muscle mitochondrial efficiency in rats with fructose-induced alteration in glucose tolerance. Br J Nutr 110:1996–2003
Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL et al (2009) Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest 119(5):1322–1334
Cox CL, Stanhope KL, Schwarz JM, Graham JL, Hatcher B, Griffen SC et al (2011) Consumption of fructose-sweetened beverages for 10 weeks reduces net fat oxidation and energy expenditure in overweight/obese men and women. Eur J Clin Nutr 66(2):201–208
Ren LP, Chan SM, Zeng XY, Laybutt DR, Iseli TJ, Sun RQ et al (2012) Differing endoplasmic reticulum stress response to excess lipogenesis versus lipid oversupply in relation to hepatic steatosis and insulin resistance. PLoS One 7(2):e30816. doi:10.1371/journal.pone.0030816
Ferramosca A, Conte A, Damiano F, Siculella L, Zara V (2014) Differential effects of high-carbohydrate and high-fat diets on hepatic lipogenesis in rats. Eur J Nutr 53(4):1103–1114
Duarte JA, Carvalho F, Pearson M, Horton JD, Browning JD, Jones JG et al (2014) A high-fat diet suppresses de novo lipogenesis and desaturation but not elongation and triglyceride synthesis in mice. J Lipid Res 55(12):2541–2553
Chong MF, Hodson L, Bickerton AS, Roberts R, Neville M, Karpe F et al (2008) Parallel activation of de novo lipogenesis and stearoyl-CoA desaturase activity after 3 d of high-carbohydrate feeding. Am J Clin Nutr 87(4):817–823
Feillet-Coudray C, Aoun M, Fouret G, Bonafos B, Ramos J, Casas F et al (2013) Effects of long-term administration of saturated and n-3 fatty acid-rich diets on lipid utilisation and oxidative stress in rat liver and muscle tissues. Br J Nutr 110(10):1789–1802
Morgan K, Uyuni A, Nandgiri G, Mao L, Castaneda L, Kathirvel E et al (2008) Altered expression of transcription factors and genes regulating lipogenesis in liver and adipose tissue of mice with high fat diet-induced obesity and nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol 20(9):843–854
Oosterveer MH, van Dijk TH, Tietge UJ, Boer T, Havinga R, Stellaard F et al (2009) High fat feeding induces hepatic fatty acid elongation in mice. PLoS One 4(6):e6066. doi:10.1371/journal.pone.0006066
de Meijer VE, Le HD, Meisel JA, Akhavan Sharif MR, Pan A, Nosé V et al (2010) Dietary fat intake promotes the development of hepatic steatosis independently from excess caloric consumption in a murine model. Metabolism 59(8):1092–1105
Crescenzo R, Bianco F, Falcone I, Coppola P, Liverini G, Iossa S (2013) Increased hepatic de novo lipogenesis and mitochondrial efficiency in a model of obesity induced by diets rich in fructose. Eur J Nutr 52:537–545
Castro MC, Francini F, Gagliardino JJ, Massa ML (2014) Lipoic acid prevents fructose-induced changes in liver carbohydrate metabolism: role of oxidative stress. Biochim Biophys Acta 1840:1145–1151
Castro MC, Massa ML, Shinella G, Gagliardino JJ, Francini F (2013) Lipoic acid prevents liver metabolic changes induced by administration of a fructose-rich diet. Biochim Biophys Acta 1830:2226–2232
Lambert K, Py G, Robert E, Mercier J (2003) Does high-sucrose diet alter skeletal muscle and liver mitochondrial respiration? Horm Metab Res 35:546–550
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Crescenzo, R., Bianco, F., Mazzoli, A. et al. A possible link between hepatic mitochondrial dysfunction and diet-induced insulin resistance. Eur J Nutr 55, 1–6 (2016). https://doi.org/10.1007/s00394-015-1073-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-015-1073-0