Abstract
Background
We aimed to investigate changes of incidence, outcome and related interventions of patients with acute coronary syndrome (ACS) over the past decade in Germany.
Methods
Data on the international statistical classification of diseases and procedural codes from the Federal Bureau of Statistics in Germany was used. This included all ACS cases in Germany in the years 2005–2015. Analyses were performed separately for the diagnoses of overall ACS, ST-elevation myocardial infarction (MI), non-ST-elevation MI and unstable angina pectoris. Procedures including coronary angiography and percutaneous coronary intervention and the endpoint in-hospital mortality were assessed.
Results
Between 2005 and 2015 a total of 3797,546 cases of ACS were recorded. The mean age was 69 years and 36% were females. In-hospital mortality was 6.3%, 62% underwent coronary angiography and 42% received percutaneous coronary intervention. In-hospital mortality was highest for patients with ST-elevation MI (12.0%) and lowest for patients with unstable angina pectoris (0.6%). From 2005 to 2015 the incidence rates of ACS, ST-elevation MI and unstable angina pectoris decreased, while the incidence rate of non-ST-elevation MI increased. The percentages of performed coronary angiographies and percutaneous coronary interventions increased from 52 to 70% and 34 to 50%, respectively. The adjusted incidence rate of in-hospital mortality decreased from 64.9 cases per 1000 person-years to 54.8 cases.
Conclusion
In a large dataset including more than 3.7 million cases, we report an increase in coronary procedures and a reduction of ACS incidence and related mortality in the past decade in Germany.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patients presenting with suspected acute coronary syndrome (ACS) are an important population in emergency departments worldwide and account for more than 20 million presentations to the emergency department in Europe and North America [1]. In the past decades, diagnostic and therapeutic pathways for these patients have substantially improved [2, 3]. This includes on the one hand faster and more accurate diagnostic algorithms, which are based on high-sensitivity cardiac troponin [4]. On the other hand, therapeutic options have substantially improved, as modern drug-eluting-stents, potent P2Y12 inhibitors and lipid-lowering drugs are routinely used nowadays [5, 6]. Finally, awareness for primary prevention strategies in the general population has become more available and could reduce disease burden on a large scale [7, 8].
These changes over time had an impact on outcome, as the incidence rates of acute myocardial infarction (MI), as well as related mortality decreased in developed countries [2, 9, 10]. However, there is limited data on the temporal trends of ACS diagnosis within the past decade from large contemporary datasets. Therefore, we aimed to assess incidence, outcome and related interventions of patients admitted with ACS in Germany. For this purpose, we analyzed clinical data from all cases treated for ACS in Germany between 2005 and 2015.
Methods
Study population and study design
In Germany, all clinical cases treated within a hospital have to be collected within one central database by the Federal Bureau of Statistics to enable reimbursement. Within this database, all diagnoses and performed procedures are stored. The diagnoses are coded according to the International Statistical Classification of Diseases and Related Health Problems, 10th revision, German modification (ICD-10-GM). All procedures are coded according to the German Procedure Classification (OPS). The guidelines for coding, as well as annual adaptations, allow a uniform documentation. For the present analyses, we used all cases of patients with the main diagnosis of ACS (ICD-codes I20.0, I21 or I22) from the years 2005–2015. All ICD and OPS codes, which were used for the present analyses, are provided in Table S1. The variables included age, sex, type of ACS-subgroup (ST-elevation MI (STEMI), non-ST-elevation MI (NSTEMI), and unstable Angina pectoris (UAP)), cardiovascular risk factors (hypertension, dyslipidemia, diabetes), prevalent comorbidities (peripheral artery disease, prior stroke, atrial fibrillation, chronic obstructive pulmonary disease (COPD), renal insufficiency, prior coronary-artery-bypass-grafting (CABG)) and performed procedures (coronary angiography, performed percutaneous coronary intervention (PCI), performed CABG), as well as in-hospital mortality.
The data export was performed on our behalf by the Research Data Center of the Federal Bureau of Statistics and Statistical Offices of the Federal States in Wiesbaden, Germany, and aggregated statistics were provided on the basis of R codes that we supplied to the Research Data Center. There was no commercial support for the study or the preparation of this manuscript. This study did not involve direct access by the investigators to data on individual patients, but only access to completely anonymized summary results provided by the Research Data Center. Therefore, approval by an ethics committee and informed consent were not required in accordance with German law.
Statistical analysis
Binary variables were shown as absolute numbers and percentages, whereas continuous variables were shown as mean ± standard deviation (SD). Subgroup analyses were performed for patients with STEMI, NSTEMI, UAP, according to settlement geography (urban and rural) and by month of documentation. Furthermore, age- and sex-adjusted incidence rates were calculated for overall ACS, STEMI, NSTEMI, and UAP using the age- and sex-specific distribution in Germany at the 31st of December of each year as reference. The distribution of ACS in Germany was applied as reference for incidence rates of in-hospital mortality. These were calculated in three different models: unadjusted, adjusted for age and sex, and adjusted for age, sex, diabetes, dyslipidemia, hypertension and renal failure. All statistical methods were written in R statistical software version 3.5.2 (R Foundation for Statistical Computing) and were performed at the Federal Bureau of Statistics in Germany.
Results
Characteristics of the overall population
Between 2005 and 2015 a total of 3797,546 cases of ACS were recorded (Table 1). The mean age was 68.8 years (SD 16.47) and 36.0% were females. 57.3% were diagnosed with hypertension, 43.5% with dyslipidemia, and 27.2% with diabetes. There were 1441,876 cases of UAP, 1331,514 cases of NSTEMI and 925,424 cases of STEMI in the overall dataset. Patients with NSTEMI were older compared to STEMI patients (71.7 vs. 66.2 years), were more often female and had a higher prevalence of cardiovascular risk factors.
The mean duration of the hospital stay was 7.2 days (SD 7.7) and was longer in STEMI (8.4 days, SD 8.4) and NSTEMI patients (8.6 days, SD 8.5), compared to UAP patients (5.1 days, SD 5.7). In the overall ACS population, 62.2% received a coronary angiography and 42.4% a PCI. Among STEMI patients, these rates were higher (71.6% coronary angiography and 65.3% PCI), compared to NSTEMI (60.2% and 41.0%) and UAP patients (60.8 and 30.7%). In total, 4.7% of all patients underwent coronary artery bypass grafting.
In the refining analyses according to settlement geography, no major differences in the patient characteristics were observed (Table 2). The rate of coronary angiographies was 68.5% in urban and 68.2% in rural regions. In-hospital mortality was 5.9% in urban and 6.3% in rural regions.
Temporal trends of patient characteristics, incidence and outcome from 2005 to 2015
From 2005 to 2015 we observed an increase of age (2005 mean age 68.3 years vs. 2015 69.1 years) and a decrease in female sex (37.7% vs. 34.1%) (Table 3 and S2). The presence of cardiovascular risk factors slightly increased, while the mean duration of hospital stay decreased from 7.8 days (SD 7.7) to 6.5 days (SD 6.9). Rates of coronary angiography and PCI increased from 52.4% and 33.8% to 70.5% and 50.3%, respectively. In-hospital mortality decreased from 6.4 to 5.9%. The results for each subgroup of ACS diagnosis are presented in Table S3. In subgroup analyses according to the month of documentation, the rate of ACS cases was lower in the summer months, compared to the winter months (Table S4).
The age- and sex-adjusted incidence rate of ACS decreased from 6.9 cases/1000 person-years to 5.0 cases/1000 person-years (Fig. 1a and Table S5). In subgroup analyses, the incidence rate of UAP and STEMI decreased as well, while the incidence rate of NSTEMI increased from 1.8 cases/1000 person-years to 2.5 cases/1000 person-years (Fig. 1 and Table S5).
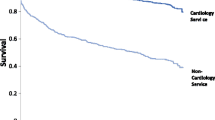
In total, 6.3% died during the in-hospital stay. The mortality rate was substantially higher in STEMI patients (12.0% vs. 6.6% in NSTEMI and 0.6% in UAP). The unadjusted incidence rates of in-hospital mortality were reduced from 64.4 cases/1000 person-years in 2005 to 59.3 cases/1000 person-years in 2015, while the age- and sex-adjusted incidence rates of in-hospital mortality was reduced from 64.9 cases/1000 person-years in 2005 to 54.8 cases/1000 person-years in 2015 (Fig. 2 and Table S6). After additional adjustment for diabetes, dyslipidemia, hypertension and renal failure the incidence rates of in-hospital mortality was reduced from 65.1 cases/1000 person-years in 2005 to 62.3 cases/1000 person-years in 2015.
Discussion
In a large population of more than 3.7 million cases, we report a decreasing incidence of acute coronary syndrome in Germany within the past decade. While the rate of performed coronary angiographies and coronary interventions increased, the in-hospital mortality and the duration of hospital stay decreased.
In this manuscript, we present novel findings. First, we were able to collect all ACS cases in Germany over the past decade, which resulted in a dataset allowing for the accurate description of ACS incidence and its changes in the last 10 years. We found a decrease in ACS and STEMI diagnosis, which is in line with earlier observations. In 2010, Yeh et al. [9] for the first time reported a strong decrease of STEMI incidence in 45,000 US patients. These changes most likely mirrored recent improvements in preventive, diagnostic, and therapeutic strategies for patients with coronary artery disease [5]. In contrast, the incidence of NSTEMI diagnosis showed an increase from 2005 to 2012 and a decrease thereafter in our study. These findings might be related to the changes in troponin assays over the past years. Troponin-testing was introduced in clinical routine at the end of the last century and was first included in the definition of MI in 2000 [11]. Since that time, troponin assays became much more widely used, but also more sensitive, allowing detection of already mild troponin elevation [12]. In Germany, high-sensitivity troponin assays became widely established after their introduction in 2009 and are today used in most hospitals [13, 14]. This may explain the continuous increase of NSTEMI diagnosis up to 2012. The fact, that NSTEMI rates did not further increase after 2012 [15] might then be a result of improved prevention strategies. In the large SWEDEHEART registry, a similar trend was observed [16]. Here, the proportion of NSTEMI diagnosis was also highest in 2012, while the rate of STEMI diagnosis showed a continuous decrease over time. This Swedish population had a similar median age and a comparable distribution of cardiovascular risk factors.
The second salient finding is, that rates of invasive procedures, such as coronary angiography and PCI, were rapidly increasing in the past decade. In addition, the duration of hospital stay was reduced by more than 1 day, and in-hospital mortality decreased. These findings confirm prior reports from the SWEDEHEART registry [2, 16]. In their cohort, the authors described a decrease of in-hospital mortality from 12.4% in 1995 to 3.7% in 2014. The authors related this improvement to the uptake of evidence-based treatments, including statins and coronary interventions in the past years. During this period, the rate of primary PCI showed a strong increase and reached up to 80% for patients diagnosed with STEMI in the year 2018, which is similar to our cohort. Furthermore, we could extend these findings about a decrease in mortality to an overall ACS patients’ cohort. Here, we observed a decline not only in NSTEMI but also in STEMI patients. Interestingly, this effect was less attenuated, when the in-hospital mortality was additionally adjusted for cardiovascular risk factors. However, there might be a reporting bias in the documentation of risk factors, as the incidence of dyslipidemia in ACS patients is unlikely to show a strong increase of more than 6% within 10 years. Therefore, adjustment for age and sex might be the most valid analysis.
More recently, a steady reduction of 30-days mortality had also been reported in a large US cohort study including more than 4 million Medicare beneficiaries with MI [10]. In contrast, results from the German Quality Assurance database, which compared the outcome of STEMI patients in Germany in 2008 and 2013, showed a slight increase of the in-hospital mortality in unadjusted analyses [17]. These differences might be explained by an increasing age, as well as an increasing risk profile. This would be supported by our analyses, as the trend of the unadjusted in-hospital mortality was less prominent.
In subgroup analyses, we found no substantial differences in patients treated in urban or rural regions. Germany is a densely populated country, with a good coverage of emergency facilities not only near the bigger cities, which might explain the lack of regional distinctions. Finally, we investigated the rate of ACS cases per month and observed a lower rate in the summer months, compared to the winter months. These results are supported by prior evidence, that cold weather might impact the incidence of cardiovascular events [18,19,20].
Our analyses have strengths, but also limitations. A major strength is, that we collected a very large dataset including all ACS cases in Germany from the past decade. Furthermore, the information on in-hospital procedures and mortality were available for all patients. A limitation is, that there might be a reporting bias for diagnoses and procedures, as these were done by each hospital locally, without a central adjudication. This could lead to an under- or over-reporting of certain diagnoses. However, due to the large sample size, this effect is unlikely to have impact on the overall results. Furthermore, there is no information on biomarkers, prescribed drugs and follow-up diagnostics in this population. Finally, due to the central organization of the Federal Bureau of Statistics, we cannot provide more detailed information about the type and volume of hospitals performing the procedures.
In conclusion, in a large dataset including 3.7 million cases from the past decade in Germany, we reported a reduction of ACS incidence and related mortality. Whether these findings are a consequence of improved primary and secondary prevention strategies or a higher usage of invasive coronary procedures needs to be shown.
References
Niska R, Bhuiya F, Xu J (2010) National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Rep 26:1–31
Szummer K, Wattentin L, Lindhagen L, Alfredsson J, Erlinge D, Held C, James S, Kellerth T, Lindahl B, Ravn-Fischer A, Rydberg E, Yndigegn T, Jernberg T (2018) Relations between implementation of new treatments and improved outcomes in patients with non-ST-elevation myocardial infarction during the last 20 years: experiences from SWEDEHEART registry 1995 to 2014. Eur Heart J 39(42):3766–3776. https://doi.org/10.1093/eurheartj/ehy554
Neumann JT, Twerenbold R, Ojeda F, Sorensen NA, Chapman AR, Shah ASV, Anand A, Boeddinghaus J, Nestelberger T, Badertscher P, Mokhtari A, Pickering JW, Troughton RW, Greenslade J, Parsonage W, Mueller-Hennessen M, Gori T, Jernberg T, Morris N, Liebetrau C, Hamm C, Katus HA, Munzel T, Landmesser U, Salomaa V, Iacoviello L, Ferrario MM, Giampaoli S, Kee F, Thorand B, Peters A, Borchini R, Jorgensen T, Soderberg S, Sans S, Tunstall-Pedoe H, Kuulasmaa K, Renne T, Lackner KJ, Worster A, Body R, Ekelund U, Kavsak PA, Keller T, Lindahl B, Wild P, Giannitsis E, Than M, Cullen LA, Mills NL, Mueller C, Zeller T, Westermann D, Blankenberg S (2019) Application of high-sensitivity troponin in suspected myocardial infarction. N Engl J Med 380(26):2529–2540. https://doi.org/10.1056/NEJMoa1803377
Twerenbold R, Neumann JT, Sorensen NA, Ojeda F, Karakas M, Boeddinghaus J, Nestelberger T, Badertscher P, Rubini Gimenez M, Puelacher C, Wildi K, Kozhuharov N, Breitenbuecher D, Biskup E, de Lavallaz JF, Flores D, Wussler D, Miro O, Martin Sanchez FJ, Morawiec B, Parenica J, Geigy N, Keller DI, Zeller T, Reichlin T, Blankenberg S, Westermann D, Mueller C (2018) Prospective validation of the 0/1-h algorithm for early diagnosis of myocardial infarction. J Am Coll Cardiol 72(6):620–632. https://doi.org/10.1016/j.jacc.2018.05.040
Nabel EG, Braunwald E (2012) A tale of coronary artery disease and myocardial infarction. New Engl J Med 366(1):54–63. https://doi.org/10.1056/NEJMra1112570
Bestehorn K, Bauer T, Fleck E, Bestehorn M, Pauletzki J, Hamm C (2015) Coronary procedures in German hospitals: a detailed analysis for specific patient clusters. Clin Res Cardiol 104(7):555–565. https://doi.org/10.1007/s00392-015-0818-3
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, Brauer M, Kutty VR, Gupta R, Wielgosz A, AlHabib KF, Dans A, Lopez-Jaramillo P, Avezum A, Lanas F, Oguz A, Kruger IM, Diaz R, Yusoff K, Mony P, Chifamba J, Yeates K, Kelishadi R, Yusufali A, Khatib R, Rahman O, Zatonska K, Iqbal R, Wei L, Bo H, Rosengren A, Kaur M, Mohan V, Lear SA, Teo KK, Leong D, O'Donnell M, McKee M, Dagenais G (2019) Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. https://doi.org/10.1016/S0140-6736(19)32008-2
Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, Bo J, Lou Q, Lu F, Liu T, Yu L, Zhang S, Mony P, Swaminathan S, Mohan V, Gupta R, Kumar R, Vijayakumar K, Lear S, Anand S, Wielgosz A, Diaz R, Avezum A, Lopez-Jaramillo P, Lanas F, Yusoff K, Ismail N, Iqbal R, Rahman O, Rosengren A, Yusufali A, Kelishadi R, Kruger A, Puoane T, Szuba A, Chifamba J, Oguz A, McQueen M, McKee M, Dagenais G, Investigators P (2014) Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med 371(9):818–827. https://doi.org/10.1056/NEJMoa1311890
Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS (2010) Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med 362(23):2155–2165. https://doi.org/10.1056/NEJMoa0908610
Krumholz HM, Normand ST, Wang Y (2019) Twenty-year trends in outcomes for older adults with acute myocardial infarction in the United States. JAMA Netw Open 2(3):e191938. https://doi.org/10.1001/jamanetworkopen.2019.1938
Alpert JS, Thygesen K, Antman E, Bassand JP (2000) Myocardial infarction redefined–a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 36(3):959–969
Westermann D, Neumann JT, Sorensen NA, Blankenberg S (2017) High-sensitivity assays for troponin in patients with cardiac disease. Nat Rev Cardiol 14(8):472–483. https://doi.org/10.1038/nrcardio.2017.48
Keller T, Zeller T, Peetz D, Tzikas S, Roth A, Czyz E, Bickel C, Baldus S, Warnholtz A, Frohlich M, Sinning CR, Eleftheriadis MS, Wild PS, Schnabel RB, Lubos E, Jachmann N, Genth-Zotz S, Post F, Nicaud V, Tiret L, Lackner KJ, Munzel TF, Blankenberg S (2009) Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med 361(9):868–877. https://doi.org/10.1056/NEJMoa0903515
Keller T, Zeller T, Ojeda F, Tzikas S, Lillpopp L, Sinning C, Wild P, Genth-Zotz S, Warnholtz A, Giannitsis E, Mockel M, Bickel C, Peetz D, Lackner K, Baldus S, Munzel T, Blankenberg S (2011) Serial changes in highly sensitive troponin I assay and early diagnosis of myocardial infarction. JAMA 306(24):2684–2693. https://doi.org/10.1001/jama.2011.1896
Anand A, Shah ASV, Beshiri A, Jaffe AS, Mills NL (2019) Global adoption of high-sensitivity cardiac troponins and the universal definition of myocardial infarction. Clin Chem 65(3):484–489. https://doi.org/10.1373/clinchem.2018.298059
Jernberg T (2019) Swedeheart Annual Report for 2018.
Bestehorn K, Bestehorn M, Fleck E, D`Ancona G, Ince H, Eggebrecht H (2019) Increase of in-hospital mortality of stemi-patients after pci? a risk adjusted analysis of German quality assurance data 2008–2013. J Cardiol Cardiovasc Ther. 13(3):555865. https://doi.org/10.19080/JOCCT.2019.13.555865
Nagarajan V, Fonarow GC, Ju C, Pencina M, Laskey WK, Maddox TM, Hernandez A, Bhatt DL (2017) Seasonal and circadian variations of acute myocardial infarction: findings from the Get With The Guidelines-Coronary Artery Disease (GWTG-CAD) program. Am Heart J 189:85–93. https://doi.org/10.1016/j.ahj.2017.04.002
Mohammad MA, Koul S, Rylance R, Frobert O, Alfredsson J, Sahlen A, Witt N, Jernberg T, Muller J, Erlinge D (2018) Association of weather with day-to-day incidence of myocardial infarction: A SWEDEHEART Nationwide Observational Study. JAMA Cardiol 3(11):1081–1089. https://doi.org/10.1001/jamacardio.2018.3466
Claeys MJ, Rajagopalan S, Nawrot TS, Brook RD (2017) Climate and environmental triggers of acute myocardial infarction. Eur Heart J 38(13):955–960. https://doi.org/10.1093/eurheartj/ehw151
Acknowledgements
J.N. was supported by a grant from the German Research Foundation, the German Heart Foundation/German Foundation of Heart Research, the Else Kröner Fresenius Stiftung and the DZHK; and is recipient of a research fellowship by the Deutsche Forschungsgemeinschaft (NE 2165/1-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JN has received honoraria from Abbott Diagnostics, Siemens and Prevencio; SB has received honoraria from Abbott Diagnostics, Siemens, Thermo Fisher, and Roche Diagnostics and is a consultant for Thermo Fisher. DW reports personal fees from Bayer, Boehringer-Ingelheim, Berlin Chemie, Astra Zeneca, Biotronik and Novartis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Neumann, J.T., Goßling, A., Sörensen, N.A. et al. Temporal trends in incidence and outcome of acute coronary syndrome. Clin Res Cardiol 109, 1186–1192 (2020). https://doi.org/10.1007/s00392-020-01612-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-020-01612-1