Abstract
Objectives
The objective of our work is to evaluate the prognostic benefit of an early invasive strategy in patients with high-risk NSTACS according to the recommendations of the 2020 clinical practice guidelines during long-term follow-up.
Methods
This retrospective observational study included 6454 consecutive NSTEACS patients. We analyze the effects of early coronary angiography (< 24 h) in patients with: (a) GRACE risk score > 140 and (b) patients with “established NSTEMI” (non ST-segment elevation myocardial infarction defined by an increase in troponins) or dynamic ST-T-segment changes with a GRACE risk score < 140.
Results
From 2003 to 2017, 6454 patients with “new high-risk NSTEACS” were admitted, and 6031 (93.45%) of these underwent coronary angiography. After inverse probability of treatment weighting, the long-term cumulative probability of being free of all-cause mortality, cardiovascular mortality and MACE differed significantly due to an early coronary intervention in patients with NSTEACS and GRACE > 140 [HR 0.62 (IC 95% 0.57–0.67), HR 0.62 (IC 95% 0.56–0.68), HR 0.57 (IC 95% 0.53–0.61), respectively]. In patients with NSTEACS and GRACE < 140 with established NSTEMI or ST/T-segment changes, the benefit of the early invasive strategy is only observed in the reduction of MACE [HR 0.62 (IC 95% 0.56–0.68)], but not for total mortality [HR 0.96 (IC 95% 0.78–1.2)] and cardiovascular mortality [HR 0.96 (IC 95% 0.75–1.24)].
Conclusions
An early invasive management is associated with reduced all-cause mortality, cardiovascular mortality and MACE in NSTEACS with high GRACE risk score. However, this benefit is less evident in the subgroup of patients with a GRACE score < 140 with established NSTEMI or ST/T-segment changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non–ST-segment elevation acute coronary syndrome (NSTEACS) is currently the most frequent manifestation of acute coronary syndromes (ACS) [1, 2]. Improvements in the pharmacological and invasive management of ACS over the last decades have demonstrated a reduction of in-hospital mortality and long-term cardiovascular events. In fact, coronary angiography plays a central role in this group of patients, allowing confirmation of diagnosis, risk stratification, and the choice of revascularization strategy and antithrombotic therapy [3, 4]. Routine coronary angiography management is well-established in NSTEACS patients, however, optimal timing of invasive strategy is less clearly defined. Recently, the new European Society of Cardiology guidelines of NSTEACS [3] recommended an early coronary angiography (within the first 24 h after hospital admission) in high-risk patients. This “new high risk” group includes patients with a GRACE risk score > 140 and patients with “established NSTEMI” (non ST-segment elevation myocardial infarction defined by an increase in troponins) or dynamic ST-T-segment changes with a GRACE risk score < 140.
The Timing of Intervention in Acute Coronary Syndromes (TIMACS) study [5] that included NSTEACS patients, showed that an early intervention was only associated with a better prognosis in patients with a GRACE risk score > 140. More recently, VERDICT trial [6] demonstrated that early invasive therapy improves long-term outcomes in high-risk patients. The EARLY Randomized Trial [7] showed that a very early invasive strategy was associated with a significant reduction in ischemic events in intermediate- and high-risk NSTEACS patients. These results were also observed in a contemporary registry and several small randomized clinical trials; although, other clinical trials have not demonstrated improvements in clinical outcomes with early invasive strategy in high-risk patients [8,9,10,11,12,13,14,15,16,17,18,19,20]. Besides, there is currently no evidence of benefit of early invasive strategy in the group of “established NSTEMI” and patients with dynamic new or presumably new contiguous ST—T-segment dynamic changes both with a GRACE score < 140 as indicated by the new recommendations of the ESC guidelines [3]. In fact, as mentioned in the guidelines text, among unselected NSTEACS patients, an early invasive strategy is not superior over a delayed invasive strategy with regard to composite clinical endpoints.
Therefore, the aim of our study is to assess the prognostic impact of an early invasive strategy (< 24 h) in all-cause mortality, cardiovascular mortality and major adverse cardiac events (MACE) in the two subgroups of patients included in “new high-risk” NSTEACS group: (a) patients with a GRACE risk score > 140 and (b) patients with a GRACE risk score < 140 and established NSTEMI or dynamic ST—T-segment changes. We have used a large contemporary real-world cohort of patients with NSTEACS from two Spanish tertiary hospitals.
Methods
The study has included all consecutive patients admitted from NSTEACS in 2 Spanish hospitals between 2003 and 2017, resulting in a sample cohort of 6454 patients. Both centers have on-site percutaneous coronary intervention capabilities without need for transfer. This retrospective analysis was performed using a prospective registry.
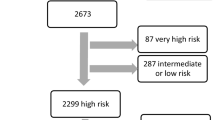
For this study, according to new ESC NSTEACS guidelines [3], high-risk NSTEACS patients were categorized into 2 groups: the first one with a GRACE risk score > 140; and another one with a GRACE score < 140 and established NSTEMI (with elevated cardiac biomarkers of necrosis) or dynamic new or presumably new contiguous ST—T-segment changes (symptomatic or silent). Early invasive coronary intervention was defined as one accomplished within the first 24 h of admission, and late invasive intervention was defined as one established after 24 h of admission. We have been excluded patients with very high risk according with the recent ESC Guidelines, and patients who died before coronary angiography.
Medical history, risk factors, biochemical and electrocardiographic findings, medication, complementary procedure tests and main diagnosis at discharge were collected by a trained medical staff. In both centers, the diagnostic and therapeutic NSTEACS protocols included blood sample determinations at arrival and the first fasting state after hospital admission. The antecedent of previous coronary heart disease was established with a previous clinical diagnosis of myocardial infarction, stable or unstable angina, or angina-driven coronary revascularization. Glomerular filtration rate was estimated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation. During the admission and after revascularization of the culprit vessel, patients with multi vessel disease underwent complete revascularization guided by an ischemia test, angina or left ventricular dysfunction.
The post-discharge follow-up of patients has a well-established protocol in each center and included phone calls and a review of electronic medical reports and institutional databases. The vital status was assured by phone calls in the absence of medical reports. All health-related processes in these health areas are based on electronic resources in both centers. Major cardiovascular adverse events (MACE) during follow-up is defined as a combination of all-cause mortality, cardiovascular mortality, myocardial infarction, heart failure hospitalization and unplanned repeat revascularization. Patient death is always typed into patients’ electronic database by the general practitioner responsible for out-of-hospital care or an in-hospital area, but the status is changed to deceased only by the department of codification of each health area; meaning that the vital status is certified by two separate processes. Trained medical staff make the collection and adjudication of clinical events in both databases. The study protocol and informed consent was approved by the ethics committee of the hospital coordination.
We compared baseline characteristics, at admission, management during hospitalization and at discharge, and clinical outcomes among these groups. Categorial variables were expressed as percentages of available data and continuous variables were expressed as the mean ± standard deviation. Continuous variables were compared using a student’s t-test, and discrete variables were compared using chi-squared or Fisher’s exact test, as necessary.
To evaluate the impact of early coronary angiography on mortality and MACE events in NSTEACS patients in this observational study, we introduced a propensity score method where the scores were created by fitting a logistic regression model to the original population of patients who underwent early invasive coronary angiography and those who did not undergo it [21]. The independent variables that appeared to be associated with the choice of the early intervention and prognosis of patients (included the components of the GRACE risk score) were clinically and statistically considered.
Before creating propensity score, missing values were imputed using multiple chained equations. We adjusted the cohorts with the inverse probability weighting of treatment approach; each individual was weighted by the inverse probability of receiving early coronary angiography, equal to 1/propensity score for the treated individuals and 1/(1 − propensity score) for the control individuals. With the methods, all samples could be utilized, which is considered to be beneficial for this observational study [22].
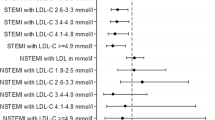
Kaplan–Meier curves with inverse probability weighting of treatment adjustment were created to compare overall and cardiovascular mortality, and MACE events, between patients who underwent early coronary angiography and those did not [22]. The log-rank test was used to confirm differences in the survival trend between the two groups. Propensity score-adjusted estimation of hazard ratio for high-risk (GRACE score > 140) and new high-risk patients (patients with a GRACE score < 140 and established NSTEMI or dynamic ST-T-segment changes), with stratification of each variable. Significance was determined as two-sided with a P value < 0.05. All statistical analyses were carried out in R version 4.0.3 using the mice, survival, forest plot, ggplot2 and survminer packages. These packages are freely available at https://cran.r-project.org.
Results
From November 2003 to November 2017, 6454 patients with “high-risk NSTEACS” were admitted, and 6031 (93.45%) of these underwent coronary angiography, with available mean follow-up of 52.2 months, IQR (interquartile range) 21.0–78.0 months for mortality outcomes. Of those invasively treated, 4819 (75.40%) patients had early invasive coronary angiography.
The baseline characteristics of the patients stratified according the risk (GRACE risk score > 140 and GRACE < 140 with established NSTEMI or dynamic ST-T-segment changes) are described in Table 1. Briefly, the mean age was 66.7 ± 13.1 years; only, 26.9% of the patients were females. Patients with a GRACE score > 140 were elderly (73.8 ± 9.8 years) compared to patients with a GRACE < 140 and established NSTEMI or dynamic ST-T-segment changes (57.8 ± 11.1 years), and were more common female (31.7% vs 20.9%, respectively). Smoker was less frequently in GRACE > 140 group (18.2% vs 42.3%), and glomerular filtration rate and hemoglobin levels were lower too (77.6 ± 28.5 vs 95.7 ± 28.7 ml/min/1.73 m2; 13.4 ± 1.9 vs 14.5 ± 1.6 mg/dL, respectively). Hypertension, diabetes mellitus, previous coronary artery disease, previous heart failure, previous stroke, chronic obstructive pulmonary disease and kidney disease were more prevalent in patients with a GRACE risk score > 140.
Cardiogenic shock during hospitalization was more common in patients with a GRACE risk score > 140 (4.0% vs 0.1%). Coronary angiography was performed more frequently in patients with a GRACE < 140 and established NSTEMI or dynamic ST-T-segment changes (96.8% vs 90.7%), with higher use of the early invasive strategy (82.0% vs 68.8%) and revascularization rates (79.0% vs 75.0%). The length of hospital stay was higher in patients with a GRACE > 140 (9.2 vs 6.1 days, respectively) and hospital mortality was higher too (7.5% vs 5.5%).
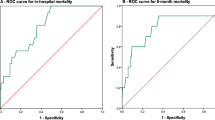
The overall mortality rate in this population of NSTEACS was 23.6%, the cardiovascular mortality rate was 16.3% and 44.9% of patients experienced at least one MACE in the long-term follow-up. After inverse probability of treatment weighting, the long-term cumulative probability of being free of all-cause mortality, cardiovascular mortality and MACE differed significantly according to early coronary intervention in patients with NSTEACS and GRACE > 140 [HR 0.62 (IC 95% 0.57–0.67), HR 0.62 (IC 95% 0.56–0.68), HR 0.57 (IC 95% 0.53–0.61), respectively] (Fig. 1). In patients with NSTEACS and GRACE < 140 with established NSTEMI or ST/T-segment changes, the benefit of the early invasive strategy is only observed in the reduction of MACE [HR 0.62 (IC 95% 0.56–0.68)], but not for total mortality [HR 0.96 (IC 95% 0.78–1.2)] and cardiovascular mortality [HR 0.96 (IC 95% 0.75–1.24)] (Fig. 2). The Fig. 3 showed the effect of early intervention among NSTEACS groups.
Discussion
In this contemporary real-world registry from two tertiary Spanish centers, early invasive management (first 24 h after hospital admission) in NSTEACS patients with a GRACE risk score > 140 was associated with lower long-term all-cause mortality, cardiovascular mortality and MACE. However, the early coronary angiography was only associated with less risk of MACE in patients with a GRACE score < 140 and established NSTEMI or dynamic ST/T-segment changes; it did not differ in preventing the all-cause mortality and cardiovascular mortality during long-term follow-up. To the best of our knowledge, this study assesses for the first time the prognostic implications of the high-risk group defined by ST/T changes and positive biomarkers [3]. According to our results the strongest benefit from an early invasive strategy was found in patients with a GRACE risk score > 140; the benefit observed in the group of patients with established NSTEMI and patients with dynamic ST/T-segment changes and a GRACE risk score < 140 was less evident. Our results may have several implications for the clinical NSTEACS management and in health system organization. First, they add information from a large, contemporary cohort of patients, and reinforce the recommendations of the ESC [3] and ACC/AHA guidelines [4] for early intervention in GRACE > 140. Second, our results suggest the importance of developing assistance networks for the adequately management of the NSTEACS, particularly in hospitals without on-site 24-h catheterization, that allow coronary angiography to be performed on weekends and during holiday season. Third, our results show the greatest long-term benefit of the early strategy in patients with high GRACE risk score. Furthermore, the prognostic benefit was observed early and are maintained throughout the long-term follow-up.
Previous studies have analyzed the optimal timing of invasive intervention in patients with NSTEACS, with conflicting results. Several studies have demonstrated that the benefit of an early invasive strategy in these patients occurs early and appears to be sustained over the long term, especially in high-risk patients. However, important differences are observed in the timing of early strategy, from immediate up to 24 h, and revascularization rates. It appears that patients with a GRACE risk score greater than 140 are well identified as high risk. However, it is not so clearly established that other patients with NSTACS should be considered high risk and, therefore, benefit from an early invasive strategy. Recently, the latest guidelines from the European Society of Cardiology [3] have included a high-risk group, the established NSTEMI diagnosis or with dynamic new or presumably new contagious ST/T-segment changes. However, its inclusion is still not fully elucidated.
TIMACS trial [5], included 2147 NSTEACS patients, demonstrated that an early invasive strategy (≤ 24 h) was better than a delayed strategy (> 36 h) in reduction of cardiovascular events (death, myocardial infarction and stroke) in patients with GRACE > 140 during a 6-month follow-up. However, this trial did not show differences between this two approaches in patients with low and intermediate risk. In the ACUITY study [8], delaying revascularization (> 24 h after hospital admission) in patients with NSTEACS was an independent predictor of early and late mortality and myocardial infarction. This prospective trial that included 7749 NSTEACS patients demonstrated that a delayed invasive management was associated with a worse prognosis in high-risk patients (TIMI 5–7). Similarly, Alvarez et al. [9] showed that early invasive intervention might be associated with reduced all-cause mortality and cardiovascular mortality in high-risk NSTEACS patients (GRACE > 140). On the other hand, Atherosclerotic Risk in Communities surveillance (ARIC) study [10] is a real-world analysis between 1987 and 2012, which showed that early percutaneous intervention was associated with a better 28-day survival both in the overall cohort and in high-risk patients; however, these differences were no longer statistically significant by 1-year of follow-up. Data from GRACE [11] and CRUSADE [12] registries did not show either an improvement in prognosis with the invasive strategy. Five-year follow-up from OPTIMA trial [13] did not observed influence of the timing of coronary intervention on patient outcomes in an intermediate to high-risk NSTEACS. There was also no benefit of an immediate invasive strategy (70 min) versus a delayed one (21 h) in a French multicenter randomized study [14]. More recently, VERDICT trial [6] shown that a very early invasive coronary intervention (< 12 h) appear to be similar compared with a delayed strategy (48–72 h) in long-term outcome. However, in patients with the highest risk (GRACE risk score > 140), a very early invasive therapy improves long-term outcome. The EARLY Randomized Trial [7] included 741 patients presenting with intermediate- or high- risk NSTEACS, that were randomized to the delayed invasive group (coronary angiography performed 12–72 h after randomization) or there very early invasive strategy (coronary angiography performed 2 h after randomization). It showed that a very early invasive strategy was associated with a significant reduction in ischemic events during 1 month of follow-up. These results are similar with our findings in patients with NSTEACS and GRACE > 140. We showed a significantly reduction of all-cause mortality, cardiovascular mortality and MACE with early coronary intervention (< 24 h after admission). This reinforces the current European [3] and American guidelines [4] recommendations of an early invasive strategy in high-risk NSTEACS group with GRACE > 140. But in the other NSTEACS groups (established NSTEMI or with ST/T-segment changes) did not show a benefit in mortality as had already been observed in previous studies. Therefore, the indication for early coronary angiography in these group of patients with “established NSTEMI” (non-ST-segment elevation myocardial infarction defined by an increase in troponins) or dynamic ST-T-segment changes with a GRACE risk score < 140 should be evaluated in randomized clinical trials.
Moreover, meta-analyses pooling published showed conflicting results regarding the optimal timing of the procedure and which groups were considered of high risk. Katritsis et al. [15], in a meta-analysis with 4013 NTEACS patients, showed that an early intervention significantly reduced the risk for recurrent ischemia and the length of hospital stay, however no significant differences have seen in terms of major events (death, myocardial infarction or stroke). In a meta-analysis published by Navarese et al. [16], it was not observed benefit of one strategy over another in the randomized nor in the observational cohort. On the other hand, a more recent meta-analysis [17] published also did not observe a reduction in mortality between the invasive versus the late strategy in patients with NSTEACS. But, four subgroups of high-risk patients showed a reduction in mortality (patients with GRACE risk score > 140, patients with elevated biomarkers, diabetic patients, patients older than 75 years). Therefore, the benefit seems to specially focus on patients with GRACE > 140, as we have observed in our study, but too patients with elevated biomarkers. Thereby, biomarkers might be of certain value to identify high-risk patients, however, this value is not well-determinate, especially because many studies use it as a binary criterion. Furthermore, most of the studies that included biomarkers did so prior to the era of high-sensitivity cardiac troponin.
Our study has several strengths. It is a real-world registry with a large number of patients and a long follow-up. We used the inverse probability of treatment weighting approach in the propensity score analysis due to the high percentage of NSTEACS patients treated with early invasive strategy, and even more important, we were interested in estimating the average treatment effect. The retrospective nature of the analysis is a potential weakness. This study was also an observational registry study, which has inherent limitations (e.g., selection bias, differences in groups concerning baseline characteristics, and unmeasured bias). These associations may be confounded by unmeasured variables. Several unmeasured confounders or details about the physician or patient decision-making might not be available in our collected data protocol and could account for some of the reported findings. Also, there may have been appropriate contraindications to adjunctive pharmacotherapy or invasive management that were not registered. Finally, long-term outcomes could have been modified by many circumstances that might not be available or controlled in the follow-up protocol. The results presented in this analysis should be considered as generating hypotheses and deserve confirmation in other registries and clinical trials.
Conclusions
In a contemporary real-world registry of NSTEACS patients, an early invasive management (first 24 h after hospital admission) is associated with reduced all-cause mortality, cardiovascular mortality and major cardiovascular adverse events in NSTACS with high (> 140) GRACE risk score during long-term follow-up. The prognostic benefit of this early intervention is less evident in the subgroup of patients with a GRACE score < 140 with markers of myocardial injury and/or electrocardiographic abnormalities also included in the new high-risk group defined by the recent ESC NSTEACS guidelines.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- ACS:
-
Acute coronary syndrome
- MACE:
-
Major adverse cardiac events
- NSTEACS:
-
Non-ST-segment elevation acute coronary syndrome
- NSTEMI:
-
Non-ST-segment elevation myocardial infarction
References
Jorgensen T, Capewell S, Prescott E et al (2013) Population-level changes to promote cardiovascular health. Eur J PrevCardiol 20:409–421. https://doi.org/10.1177/2047487312441726
Go AS, Mozaffarian D, Roger VL et al (2013) Heart disease and stroke statistics 2013 up- date: a report from the American Heart Associaton. Circulation 127:e6–e245. https://doi.org/10.1161/CIR.0b013e31828124ad
Collet J-P, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL et al (2020) ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2020:1–79. https://doi.org/10.1093/eurheartj/ehaa575
Amsterdam EA, Wenger NK, Brindis RG et al (2014) 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American college of cardiology/American heart association task force on practice guidelines. J Am CollCardiol 64:190–228. https://doi.org/10.1016/j.jacc.2014.09.017
Mehta SR, Granger CB, Boden WE, TIMACS Investigators et al (2009) Early versus delayed invasive intervention in actue coronary syndromes. N Engl J Med 360:2165–2175. https://doi.org/10.1056/NEJMoa0807986
Kofoed K, Kelbæk H, Hansen PR et al (2018) Early versus standard care invasive examination and treatment of patients with non-ST-segment elevation acute coronary syndrome: the VERDICT (Very EaRIly vs deferred invasive evaluation using computerized tomography)- randomized controlled trial. Circulation 138:2741–2750. https://doi.org/10.1161/CIRCULATIONAHA.118.037152
Lemesle G, Laine M, Pankert M et al (2020) Optimal timing of intervention in NSTE-ACS without pre-treatment: the EARLY randomized trial. JACC CardiovascInterv 13:907–917. https://doi.org/10.1016/j.jcin.2020.01.231
Sorajja P, Gersh BJ, Cox DA et al (2010) Impact of delay to angioplasty in patients with acute coronary syndromes undergoing invasive management: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) trial. J Am CollCardiol 55:1416–1424. https://doi.org/10.1016/j.jacc.2009.11.063
ÁlvarezÁlvarez B, AbouJokh Casas C, Cordero A et al (2020) Early revascularization and long-term mortality in high-risk patients with non–ST-elevation myocardial infarction. The CARDIOCHUS-HUSJ registry. Rev EspCardiol 73:35–42. https://doi.org/10.1016/j.rec.2019.02.015
Arora S, Matsushita K, Qamar A et al (2018) Early versus late percutaneous revascularization in patients hospitalized with non-ST-segment elevation myocardial infarction: the atherosclerosis risk in communities surveillance study. Catheter CardiovascInterv 91:253–259. https://doi.org/10.1002/ccd.27156
Montalescot G, Dabbous OH, Lim MJ et al (2005) Global registry of acute coronary events investigators. Am J Cardiol 95:1397–1403. https://doi.org/10.1016/j.ahj.2009.06.003
Ryan JW, Peterson ED, Chen AY, CRUSADE Investigators et al (2005) Optimal timing of intervention in non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE (Can Rapid risk stratification of Unstable angina pectoris Suppress Adverse outcomes with Early implementation of the ACC/AHA guide- lines) Registry. Circulation 11:3049–3057. https://doi.org/10.1161/CIRCULATIONAHA.105.582346
Riezebos RK, Ronner E, Bals T, OPTIMA Trial et al (2009) Immediate versus deferred coronary angioplasty in non-ST-segment elevation acute coronary syndromes. Heart 95:807–812. https://doi.org/10.1136/hrt.2008.154815
Montalescot G, Cayla G, Collet JP, ABOARD Investigators et al (2009) Immediate vs delayed intervention for acute coronary syndromes: a randomized clinical trials. JAMA 302:947–954. https://doi.org/10.1001/jama.2009.1267
Katritsis DG, Siontis GCM, Kastrati A et al (2011) Optimal timing of coronary angiography and potential intervention in non-ST-elevation acute coronary syndromes. Eur Heart J 32:32–40. https://doi.org/10.1093/eurheartj/ehq276
Navarese EP, Gurbel PA, Andreotti F et al (2013) Optimal timing of coronary invasive strategy in non-ST-segment elevation acute coronary syndromes: a systematic review and meta-analysis. Ann Intern Med 158:261–270. https://doi.org/10.7326/0003-4819-158-4-201302190-00006
Jobs A, Mehta SR, Montalescot G et al (2017) Optimal timing of an invasive strategy in patients with non-ST-elevation acute coronary syndrome: a meta-analysis of randomised trials. Lancet 390:737–746. https://doi.org/10.1016/S0140-6736(17)31490-3
Deharo P, Ducrocq G, Bode C et al (2017) Timing of angiography and outcomes in high- risk patients with non-ST-segment-elevation myocardial infarction managed invasively. Circulation 136:1895–1907. https://doi.org/10.1161/CIRCULATIONAHA.117.029779
Bonello L, Laine M, Puymirat E et al (2016) Timing of coronary invasive strategy in non- ST-segment elevation acute coronary syndromes and clinical outcomes: an updated meta-analysis. JACC CardiovascInterv 9:2267–2276. https://doi.org/10.1016/j.jcin.2016.09.017
Milosevic A, Vasiljevic-Pokrajcic Z, Milasinovic D et al (2016) Immediate versus delayed invasive intervention for non-STEMI patients: the RIDDLE-NSTEMI Study. JACC CardiovascInterv 9:541–549. https://doi.org/10.1016/j.jcin.2015.11.018
Rosenbaum PR, Rubin DB (1984) Reducing bias in observational studies using subclassification on the propensity score. Am J Stat Assoc 79:516–524. https://doi.org/10.1080/01621459.1984.10478078
Xie J, Liu C (2005) Adjusted Kaplan-Meier estimator and log-rank test with inverse probability of treatment weighting for survival data. Stat Med 24:3089–3110. https://doi.org/10.1002/sim.2174
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to this study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Rights and permissions
About this article
Cite this article
Martinón-Martínez, J., Álvarez Álvarez, B., González Ferrero, T. et al. Prognostic benefit from an early invasive strategy in patients with non-ST elevation acute coronary syndrome (NSTEACS): evaluation of the new risk stratification in the NSTEACS European guidelines. Clin Res Cardiol 110, 1464–1472 (2021). https://doi.org/10.1007/s00392-021-01829-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-021-01829-8