Abstract
Background
Long-term results after circumferential pulmonary vein isolation (CPVI) for the treatment of paroxysmal atrial fibrillation (PAF) using a robotic navigation system (RNS) have not yet been reported.
Objective
To evaluate long-term results of patients with PAF after CPVI using RNS.
Methods
In this study, 200 patients (n = 151 (75.5 %) male; median age 62.2 (54.7–67.7) years) with PAF were evaluated. In 100 patients, RNS (RN-group) was used for CPVI and compared to 100 manually ablated control patients (MN-group). Radiofrequency was used in conjunction with 3D electroanatomic mapping. Power was limited to 30 watts (W) at the posterior left atrial (LA) wall in the first 49 RNS patients (RN-group-a). After esophageal perforation occurred in one RN-group-a patient, maximum power was reduced to 20 W for the subsequent 51 patients (RN-group-b).
Results
After a median follow-up of 2 years, single (77/100 vs 77/100, p = 0.89) and multiple (90/100 vs 93/100, p = 0.29) procedure success rates were comparable between RN-group and MN-group. Single procedure success rate was significantly lower in RN-group-a as compared to RN-group-b (65.3 vs 88.2 %, p = 0.047). In RN-group-a patients, procedural times [200 (170–230) vs 152 (132–200) minutes, p < 0.01] and fluoroscopy times [16.6 (12.9–21.6) minutes vs 13.7 (9.5–19) minutes, p = 0.043] were significantly longer compared to RN-group-b patients.
Conclusion
Long-term success rate after CPVI using RNS was comparable to manual ablation. Despite a lower power limit of 20 W at the posterior LA wall, single procedure success rate was higher in RN-group-b as compared to RN-group-a. Procedure time and fluoroscopy time decreased, whilst success rate increased with increasing experience in the RN-group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia, affecting approximately 2.5 % of the middle-aged German population [1]. Catheter ablation for drug-refractory AF has been established as a treatment option over the last few years [2–4]. However, the recurrence rate after successful ablation remains high, and is highly dependant on the type of AF and on operator experience [2–5]. Therefore, novel ablation tools such as single-shot devices and robotic navigation systems (RNS) have been designed to facilitate the overall ablation procedure or to enhance catheter tip-to-tissue contact in an attempt to improve clinical outcomes [6–9]. The remote RNS (Sensei™, Hansen Medical, Mountain View, CA, USA) has been developed to improve navigation properties within the left atrium (LA) as well as tip-to-tissue contact to increase ablation success. The system was introduced in 2007 and has been increasingly used, demonstrating acceptable short- and mid-term success rates when compared to manually performed ablation procedures [7–15]. Our study reports on the long-term results of circumferential pulmonary vein isolation (CPVI) using the RNS for the treatment of patients with PAF compared to manually performed CPVI.
Methods
200 patients with paroxysmal, drug-refractory AF were included in this prospective study. CPVI was performed using RNS in 100 patients [RN-group; median age 63.3 (52.5–68) years; male n = 71 (71 %)]. These patients were compared to a control group of 100 manually ablated patients [MN-group; median age 62 (54.8–67.3, male n = 80; (80 %)]. The control group consists of consecutive patients from the same time period with comparable follow-up.
All patients provided written informed consent. The follow-up of patients in the MN-group was censored after 2 years.
Transesophageal echocardiography (TEE) was performed in all patients prior to the ablation procedure to rule out intracardiac thrombus. Oral anticoagulation with phenprocoumon was discontinued 5 days prior to the ablation procedure until an INR <2 was reached and bridging anticoagulation with low-molecular-weight heparin was prescribed.
This study conforms to the guiding principles of the Declaration of Helsinki of 2008 and was approved by the local institutional review board. All authors had full access to the data, and have read and agreed to the manuscript as written.
The Sensei™ RN system
The Sensei™ (Hansen Medical, Mountain View, CA, USA) RNS is an electromechanical system facilitating catheter navigation within the cardiac chambers via two steerable sheaths (Artisan™, Hansen Medical, Mountain View, CA, USA) and incorporates the ablation catheter. The Artisan™ sheath consists of an inner (10.5F) and an outer (14F) sheath, both manipulated via a pull-wire mechanism. A robotic arm carrying the Artisan™ sheath is fixed at the patient’s table. The robotic arm is controlled remotely from the physician’s workstation, which can be positioned outside the procedure room. The system continuously monitors contact forces exerted by the ablation catheter tip on the myocardial tissue via the IntelliSense™ software (Hansen Medical, Mountain View, CA, USA) [7, 12].
Ablation procedure
The ablation procedure was performed as described in detail previously [1, 7]. In brief, a standard diagnostic catheter was inserted into the coronary sinus (CS). For the RN-group, a single transseptal puncture using a Brockenbrough needle was performed and an 8.5F SL1 sheath (St. Jude Medical, St. Paul, MN, USA) was advanced into the LA. A guide wire was then advanced into the left superior pulmonary vein (PV) via the SL1 sheath. The sheath was then retracted back into the right atrium (RA) and the Artisan™ sheath (Hansen Medical, Mountain View, CA, USA), incorporating the ablation catheter was then advanced remotely beside the guide wire and across the interatrial septum as described previously [10], Subsequently, the previous 8.5F SL1 transseptal sheath was re-advanced into the LA over the guide wire through the same puncture site. For the MN-group, double transseptal punctures using a Brockenbrough needle were performed and two 8.5F SL1 sheaths were advanced into the LA.
Following transseptal punctures, boluses of intravenous heparin were administered and the activated clotting time (ACT) measured every 30 min aiming for a target of 250–350 s. The 8.5F SL1 transseptal sheaths were flushed with a continuous infusion of heparinized saline (flow rate 10 ml/h) to prevent thrombus formation or air embolism. For the Artisan™ sheath, both the inner and outer sheaths were also flushed continuously with heparinized saline to prevent clot formation or air embolism.
In all patients, selective angiography of each pulmonary vein in the right anterior oblique (RAO) 30° and left anterior oblique (LAO) 40° fluoroscopic views were performed. A 3D map of the LA was then created using either the CARTO™ 3 system (Biosense Webster, Diamond Bar, CA, USA) or the NavX/Ensite™ Velocity system (St. Jude Medical, St. Paul, MN, USA). 3D geometry was acquired using point-by-point mapping with a mapping catheter (CARTO™) or mapping with a spiral catheter (NavX/Ensite™ Velocity). The PV ostia, which were identified by selective angiographies, were marked with 3D tags on the 3D map using the mapping catheter (see below for details).
Pulmonary vein isolation
In all patients, a circumferential ablation line was deployed around the ipsilateral PV ostia, either manually or using the RNS as described previously [11]. In both the RNS and manual groups, ablation was performed using either a 3.5 mm irrigated tip catheter (Biosense Webster, Inc.) or a 4 mm irrigated tip catheter (Cool path duo, SJM Inc.). For the initial procedures, the following power settings were used according to our institutional standard for manual procedures: maximum power limit of 40 W at the anterior wall and 30 W at the posterior wall of the LA, with a catheter irrigation rate of 17–25 ml/minute and a target temperature of 43 °C. After an esophageal perforation occured in one patient following RNS-guided PVI using a power limit of 30 W at the posterior LA wall, the maximum power limit was reduced to 20 W at the posterior wall in the subsequent RNS-guided procedures using the same contact force settings (10–40 g) [16]. The original maximum power limit of 30 W at the posterior LA wall continued to be used in the MN-group. RF current was applied for a maximum of 30 s at each location using a dragging technique until the maximal local electrogram amplitude decreased by 70 % or there was development of double potentials. In the RNS procedures, operators aimed to maintain a catheter-to-tissue contact force between 10 and 40 g during ablation as assessed by the IntelliSense™ software (Hansen Medical, Mountain View, CA, USA) [15]. The procedural endpoint was the absence or dissociation of PV spikes registered with a spiral mapping catheter placed within the PVs after a 20 min waiting period.
In the RN-group-b an esophageal temperature probe (SensiTherm™; St. Jude Medical, St. Paul, MN, USA) was inserted in all patients for endoluminal esophageal temperature monitoring. Ablation was stopped whenever an endoluminal esophageal temperature of 41 °C was observed.
Postablation care
All patients were treated with oral anticoagulation and bridged with therapeutic low-molecular-weight heparin until an INR between 2 and 3 was reached. Oral anticoagulation was resumed the day after the procedure. For all patients, transthoracic echocardiography was performed prior to discharge to rule out pericardial effusion, and a chest X-ray was performed to rule out a pneumothorax. In addition, a 24 h Holter-ECG and 12-lead resting ECGs were obtained before discharge.
Oral anticoagulation was maintained for a minimum of 3 months following ablation and thereafter according to the individual CHADS2 score [17] regardless of the underlying rhythm. The ineffective antiarrhythmic drugs used prior to ablation were continued for at least 3 months. All patients were treated with proton-pump inhibitors (PPI) for 6 weeks after discharge.
Follow-up
24 h Holter recordings for follow-up were obtained at our outpatient clinic or by the referring physicians 1, 3, and 6 months after ablation and thereafter at 6 month intervals. In the case of symptoms suggestive of arrhythmia recurrence, patients received additional Holter recordings or an event recorder for closer follow-up. Arrhythmia recurrence was defined as any documented episode of AF or atrial tachycardia lasting more than 30 s after a 3 month blanking period [17].
Learning curve using the RNS
To assess the learning curve during the use of RNS compared to manual ablation, the 100 RN-patients as well as the 100 manually ablated patients were divided into quartiles of 25 patients each. The quartiles were labeled as follows: quartile 1 (Q1, pts 1–25), quartile 2 (Q2, pts 26–50), quartile 3 (Q3, pts 51–75), quartile 4 (Q4, pts 76–100).
The learning curve was assessed by:
-
a)
Evaluation of procedural and fluoroscopy times
-
b)
Success rate compared between Q1 and Q4
Furthermore, the learning curve was also evaluated for the manual ablation group.
Statistical analysis
Continuous data were described as means and standard deviations, if the variables were normally distributed, or as medians, first and third quartiles otherwise. Differences of metric variables between two groups were analyzed with t tests, if the data were approximately normally distributed, and with Wilcoxon–Mann–Whitney tests in case of non-normally distributed data.
Categorical data were described with absolute and relative frequencies. Differences between categorical variables were evaluated with the Chi square test or with Fisher’s exact test in case of small expected cell frequencies.
For the manual and robotic group the recurrence-free survival after a single and after multiple procedures was estimated by the Kaplan–Meier method. Additionally the recurrence-free survival of the ablation groups was examined between four (and two) equally sized groups based on the date of procedure. This was envisaged to test for learning effects. If appropriate the log-rank test was used to examine survival differences between groups. Otherwise the Wilcoxon test was applied.
Univariable Cox proportional hazards models were used to identify risk factors on survival, respectively. Since not a single covariable was significant on the significance level of 5 % a multiple predictive survival model was not considered.
All p values are two-sided. For all statistical tests p < 0.05 was considered significant. All calculations were performed with the statistical analysis software SAS (SAS Institute Inc., version 9.3, Cary, NC, USA).
Results
Patient characteristics
Overall patient characteristics are displayed in Table 1. There were no significant differences in the patient characteristics of the RNS and manual groups except for the parameters hypertension (RN-group: n = 61 (61 %) vs MN-group: n = 75 (75 %), p = 0.03), LA diameter (RN-group: 41 mm (39–45) vs MN-group: 43 mm (40–46.5), p = 0.046) and the number of previously ineffective AADs (RN-group: 2.0 (1.0, 2.0) vs MN-group: 2.0 (0.0, 3.0); p = 0.048, Table 1). RN-group was subdivided into the initial patients treated with a maximum power limit of 30 W at the LA posterior wall (RN-group-a; n = 49), and the subsequent patients treated with a maximum power limit of 20 W at the LA posterior wall (RN-group-b; n = 51). The patient characteristics of the RN-group-a and RN-group-b were comparable except for the total duration of AF (RN-group-a: 72 months (48–132) vs RN-group-b: 48 months (24–84), p = 0.0498, Table 2). Patients of RN-group-b were also compared to the last 51 patients of the manually ablated patients (MN-group-b, n = 51). Patients were comparable with regard to age [60.6 ± 10.8 vs 59.8 ± 10.2 years; p = 0.75), left atrial diameter (42.5 ± 3.5 vs 43.7 ± 4.9; p = 0.16), male gender (36 (71) vs 44 (86 %);p = 0.054]; duration of AF history [48.0 (24.0, 84.0) months vs 72.0 (42.0, 96.0) months; p = 0.14], hypertension [35 (69) vs 39 (76 %); p = 0.37) or the number of previously ineffective AADs (2.0 (1.0, 2.0) vs 2.0 (0.0, 2.0); p = 0.36].
Acute success rate
In the MN-group, PVI was achieved in all patients. In the RN-group, a switch to manual navigation was necessary in 5/100 (5 %) patients. In four patients of RN-group-a, manual navigation was necessary; three of these patients required manual ablation to isolate the lateral PVs and one patient required manual navigation to isolate the septal PVs. In one patient of RN-group-b, manual ablation was necessary to isolate the lateral PVs. The rate of conversion from RNS to manual ablation was not statistically significant between RN-group-a and RN-group-b (4 vs 1, p = 0.20).
Procedural details
Procedural times were shorter in RN-group compared to MN-group [180 (150–225) vs 230 (200–260) minutes, p < 0.01) as were fluoroscopy times (15.4 (11.2–20) vs 25.8 (20.9–34.9) minutes, p < 0.01]. In RN-group-a patients, procedural times [200 (170–230) vs 152 (132–200) minutes, p < 0.01] and fluoroscopy times [16.6 (12.9–21.6) vs 13.7 (9.5–19) minutes, p = 0.043] were significantly longer compared to RN-group-b patients.
For PVI in patients of the RN-group the following 3D-mapping systems were used: Ensite™/NavX (SJM; n = 61 (61 %)) and CARTO™ (Biosense webster; n = 39 (39 %)). In the MN-group all patients were ablated using the CARTO™ System (Biosense webster; n = 100 (100 %); p < 0.001).
In the RN-group the following ablation catheters were used: Navistar/Celsius Thermocool™ [Biosense Webster; n = 79 (79 %)] or the Coolpath Duo™ [SJM; n = 21 (21 %)]. In the MN-group, all patients were ablated with the Navistar Thermocool™ ablation catheter [Biosense Webster; n = 100 (100 %); p < 0.001].
For PVI in patients of the RN-group-b either the Ensite/NavX (SJM; n = 45) or the CARTO system (Biosense Webster; n = 6) were used for 3D-Mapping, whereas in the MN-group-b all patients were ablated using the CARTO System (Biosense Webster; n = 51; p < 0.001).
In the RN-group-b the ablation catheters used were the Navistar/Celsius Thermocool™ (Biosense Webster; n = 32) and the Coolpath Duo™ (SJM; n = 19); in the MN-group-b, all patients were ablated with the Navistar Thermocool™ ablation catheter (Biosense Webster; n = 51; p < 0.001).
Procedure times (166.3 ± 47.8 vs 238.8 ± 52.1 min, p < 0.001) and fluoroscopy times [13.7 (9.5, 19.0) vs 27.2 (19.1, 34.5) minutes; p < 0.001) in RN-group-b patients were shorter as compared to patients of MN-group-b.
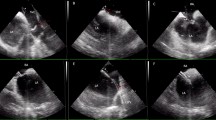
Success rates of RNS vs manual ablation
Recurrence of atrial tachyarrhythmias was observed in 46/200 (23 %) of the overall study population. Both single and multiple procedural success rates were comparable between RN-group and MN-group (Fig. 1a). Recurrence occurred in 23/100 (23 %) patients in RN-group and 23/100 (23 %) patients in MN-group during a follow-up of 2 years after the initial procedure. Multiple procedure success rate was 90 % in RN-group and 93 % in MN-group after 2 years and a median of 1.21 procedures (Fig. 1b). In the RN-group patients, AF recurred in 20/23 (87 %) and AT in 3/23 (13 %) patients. In the MN-group patients, AF recurred in 19/23 (82.6 %) and AT in 4/23 (17.4 %) patients.
Kaplan–Meier plots presenting the recurrence-free survival probability for the manual and robotic group. a (left panel): single procedure success rate for RNS-guided ablation patients (red) and manually ablated patients (blue) after 2-year follow-up. b (right panel): multiple procedure success rates for RNS (red) vs manually ablated patients (blue)
Redo-procedures were performed in 22 (22 %) patients of the RN-group and 19 (19 %) patients of the MN-group. During redo-procedures gaps were observed in 21 (95 %) patients of the RN-group and 17 (89 %) patients of the MN-group (p = 0.46). Gaps were observed in the septal veins in 17/21 (80.9 %) patients in the RN-group and 11/17 (64.7 %) patients in the MN-group (p = 0.18) and in the lateral veins in 18/21 (85.7 %) patients of the RN-group and 13/17 (76.5 %) patients of the MN-group (p = 0.32). Gaps in both, the septal and lateral PVs were observed in 14/21 (66.7 %) and 7/17 (41.2 %) patients (p = 0.087).
Success rates of RNS ablation using 20 vs 30 w at posterior LA wall
Whenever FU times were different in duration, statistical adjustment was performed between both groups (see section “statistics”).
Comparison of RN-group-a and RN-group-b showed a significantly lower single procedure success rate (65.3 vs 88.2 %, p = 0.047) (Fig. 2a) in the RN-group-a patients compared to the RN-group-b patients after 2 years of follow-up. The multiple procedure success rate was 85.7 % in RN-group-a compared to 94.1 % in RN-group-b after a median of 1.21 procedures and were therefore comparable (p = 0.48) (Fig. 2b). In RN-group-a patients AF recurred in 14/17 (82.4 %) patients and AT in 3/17 (17.6 %) patients and in RN-group-b patients AF recurred in 6/6 (100 %) patients and in no patient AT occurred.
Kaplan–Meier plots presenting the recurrence-free survival probability for the RN-group-a and RN-group-b. a (left panel): single procedure success rate for RNS-guided ablation patients with a maximum power limit of 30 W at the posterior LA wall (red) compared to patients ablated with a maximum power limit of 20 W at the posterior LA wall (blue). b (right panel): Multiple procedure success rate for RNS-guided ablation patients with a maximum power limit of 30 W at the posterior LA wall (red) compared to patients ablated with a maximum power limit of 20 W at the posterior LA wall (blue)
Recurrence rate did not differ statistically significant between patients of RN-group-b [n = 6 (11.76 %)] and patients of MN-group-b [n = 12 (23.53 %); p = 0.09].
Learning curve and relation to outcome
Whenever FU times were different in duration, statistical adjustment was performed between groups (see “statistics” section).
For assessment of the learning curve, the robotic and manual ablation groups were divided in four subgroups, respectively (Table 3). Although there were no statistically significant differences between the baseline characteristics of the subgroups, a significant reduction of procedural times and fluoroscopy times were observed between the initially ablated patients and the latter patients in the RN-group (Table 3). No significant differences were observed in the manual group (Table 3).
In regards to the single procedure success rate, clinically relevant differences in the success rate were observed between the 4 RN-subgroups (Q1: 64 %, Q2: 68 %, Q3: 92 %, Q4: 84 %; p = 0.267); however, these did not reach statistical significance (Fig. 3a).
Kaplan–Meier plots presenting the recurrence-free survival probability for the different subgroups (Q1–Q4). a (left panel): single procedure success rate of the different subgroups (Q1–Q4) in the RN-group. b (right panel): single procedure success rate of the different subgroups (Q1–Q4) in the MN-group
No statistically significant differences were observed in the MN-group (Fig. 3b. Q1: 80 %, Q2: 76 %, Q3: 80 %, Q4: 80 %; p = 1.0).
Complications
Major complications occured in two patients in the MN-group: in one patient, LA perforation occurred during the procedure, without leading to pericardial effusion. In another patient, significant pulmonary vein stenosis (>50 %) occurred that required PV stenting. In the RN-group, three major complications occurred: in one patient esophageal perforation occured requiring esophageal stenting (see reference [16] for more details). In another patient, a hematothorax occurred as a consequence of subclavian puncture that required drainage. In the third patient, pericardial tamponade requiring surgical intervention occurred.
The incidence of major complications was not statistically different between RN-group-b and MN-group-b (RN-group-b n = 1 (2 %), vs MN-group-b: n = 0 (0 %); p = 0.31).
Univariable analysis
Univariable analysis did not identify any significant parameters influencing the recurrence rates in this study population. Therefore, multiple analysis was not performed.
Discussion
This study presents the long-term success rate after CPVI using a RNS in patients with paroxysmal AF. The main findings of this study are:
-
1)
The long-term success rate is comparable between RNS-guided and manual ablation procedures.
-
2)
The long-term multiple procedure success rate using a RNS with a lower maximum power limit of 20 W at the posterior LA wall is comparable to a maximum power limit of 30 W.
-
3)
A significant learning curve was observed in the RN-group with regards to procedure and fluoroscopy times, resulting in a significant improvement of the success rate.
-
4)
The incidence of major complications is comparable between RNS-guided and manual ablation.
Acute success rate of PVI using RNS
The acute success rate for PVI using the RNS was 95 % in this study. Five patients required conversion from RNS-guided ablation to manual ablation to complete PVI (four patients in RN-group-a and one patient in RN-group-b). Previous reports have described a need to convert from RNS-guided to manual ablation for completion of PVI in only a limited number of patients and this occurs most often during the learning curve, which is estimated to be approximately 50–75 patients [12, 13]. In our study, conversion to manual ablation mainly occured within the first 49 patients and could therefore be attributed to the learning process. Of importance is that the acute success rate was comparable between patients who were ablated with a maximum power limit of 30 W and the patients ablated with reduced power settings at the LA posterior wall (20 W) (RN-group-a: four patients vs RN-group-b: one patient, n.s.).
Safety profile of CPVI using RNS
Potential complications, particularly related to RNS-guided ablation exist, such as the risk of increased catheter tip-to-tissue contact force compared to manual catheter manipulation. Recent publications have, however, described a complication rate comparable to manual ablation when reduced power settings are used [16, 18–22]. The rate of major complications of 2 % percent in our study is in line with these results. Particularly, the incidence of pericardial tamponade was 1 % in the RN-group in our study. Cardiac tamponade occurring when RNS was used has been described by several investigators previously. Whilst initial reports of tamponade had raised the question of whether RNS may increase the incidence of tamponade [7], subsequent reports have shown that this incidence was comparable with manual ablation procedures [7, 12, 13].
Energy settings and contact force when using RNS
Several previous studies have shown that a maximum power limit reduction to 30 W at the LA posterior wall appears to be associated with an acceptable safety profile in manually performed PVI ablation procedures [2]. In our study, the initial maximum power limit of 30 W at the posterior LA wall for the RNS-guided ablation procedures were chosen according to the recommended power settings for conventional manual ablation. After esophageal perforation was observed in one patient from the RN-group, the maximum power limit was changed to 20 W at the posterior LA wall in the subsequent RNS patients and no further esophageal perforations were observed [16]. Reduced power settings at the posterior LA wall have been proposed for several novel ablation tools and have been supported by results from several trials [6]. In addition, RNS-guided ablation not only appears to be effective, but also safe, with the proposed reduced power settings at the posterior LA wall [16, 18, 23], particularly when the IntelliSense™ software is used. As contact force is an important parameter during PVI [24] in all patients where the RNS was used ablation was performed with a contact force between 10 and 40 g as suggested by other investigators [23].
Long-term success rate after RNS-guided PVI
Reported success rates for catheter ablation of patients with paroxysmal AF using conventional manual ablation are reported to be up to 80 % even after 5 years of follow-up [2, 5]. Long-term data after RNS-guided CPVI are lacking and most studies to date have reported only early to mid-term outcomes with a median follow-up time of around 1 year [11, 12]. We present the first long-term follow-up data from RNS-guided PVI with a median follow-up time of 24 months, which showed a single procedure success rate of 77 % and multiple procedure success rate of 90 %. Furthermore, these results were comparable with the success rate of the manual comparison group (see Fig. 1a, b). Recurrence in patients with PAF is mostly due to the development of gaps with PV reconduction. Importantly, neither the overall number of patients with gaps nor the number of septal or lateral gaps was significantly different between patients of the RN-group or the MN-group.
When the two RNS-guided ablation subgroups with different power settings at the posterior LA wall were compared, significant differences were seen in the success rate after a single procedure, with a lower success rate seen in the patients who were initially ablated with a maximum power limit of 30 W at the posterior LA wall (RN-group-a) (Fig. 2a). Although the maximum power limit used was higher in these patients, the success rate was lower when compared to the subsequent patients who were ablated with a lower maximum power limit of 20 W at the posterior LA wall. This is explained by the learning curve identified in this study, which clearly also affects long-term outcome of these patients. This also explains why the single procedure success rate differed significantly, whereas the multiple procedure success rate was comparable between the RN-group-a and RN-group-b. Interestingly, RN-group-b was comparable to the last 51 patients in the MN-group (MN-group-b) with regard to outcome and complication rate.
Procedure and fluoroscopy times
Variable total procedural times using RNS have been described previously and have been comparable [12, 25] or even longer [18] compared to manual ablation. In our study, procedural times were shorter in the RN-group when compared to manual ablation. Longer procedural times in RN-group-a were observed when compared to RN-group-b. This can be explained by a learning curve, which was clearly depicted in this study when comparing the different quartiles of the RN-group (see Table 3). This is in line with previous reports [12, 13].
Learning curve
According to findings of previous reports [13], 4 groups (Q1–Q4, see Table 3) were created in the robotic and manual ablation arms in our study. As expected, in the RN-group a significant learning curve was seen in the procedure and fluoroscopy times. Furthermore, a clinically significant increase in the single procedure success rate was found when comparing Q1 and Q4 after the 2-year follow-up (Q1: 64 %, Q4: 84 %, see “Results” section for details). This is underlined by the statistically significant increase in the single procedure success rate between the RN-group-a as compared to the RN-group-b. These findings are even more relevant, considering that a higher power was used for ablation at the LA posterior wall in the initial patients (Q1–Q2). This underlines that experience matters when AF ablation is performed. In the manual ablation arm no significant learning curve was observed, which is explained by the fact that manual RF ablation has been our institutional standard for many years.
Limitations
This data represents a non-randomized single-center experience of RNS-ablated patients with a manual ablation control group. Larger randomized studies such as the Man and Machine trial are necessary to finally answer the question of potential benefits of RNS-guided ablation compared to manually performed RF ablation [26]. Secondly, follow-up assessment of AF recurrence consisted of 24-h Holter-monitoring and no implantable loop recorders were used. Therefore, the clinical success rate might be over-estimated. However, since only Holter ECGs were performed in the MN-group and RN-groups, this should not affect the comparability of the two ablation arms.
Differences regarding hypertension, the number of ineffective AADs prior to ablation and the LA diameter were observed between the RN-group and the MN-group, slightly favoring a less sick patient population in the RN-group. Though recently it has been shown that LA diameter did not significantly influence the outcome after AF ablation [27] this has to be kept in mind when interpreting the results of our study. Different ablation catheters and 3D mapping systems were used in the RN-group and the MN-group. Although it cannot be excluded, that different ablation or mapping techniques might influence the outcome of PVI [28], previously published data in a large series of consecutive patients, no significant differences were seen between patients where PVI was performed using either the CARTO™ or the NavX/Ensite™ system [29].
Conclusion
Both single and multiple procedure success rates after CPVI using RNS were comparable to manually performed RF ablation, as was the complication rate. An initial learning curve might influence the long-term results of AF ablation using RNS.
References
Schnabel RB, Wilde S, Wild PS, Munzel T, Blankenberg S (2012) Atrial fibrillation: its prevalence and risk factor profile in the German general population. Dtsch Arztebl Int 109(16):293–299
Ouyang F, Tilz R, Chun J, Schmidt B, Wissner E, Zerm T, Neven K, Köktürk B, Konstantinidou M, Metzner A, Fuernkranz A, Kuck KH (2010) Long-term results of catheter ablation in paroxysmal atrial fibrillation: lessons from a 5 year follow-up. Circulation 122:2368–2377
Medi C, Sparks PB, Morton JB, Kistler PM, Halloran K, Rosso R, Vohra JK, Kumar S, Kalman JM (2011) Pulmonary vein antral isolation for paroxysmal atrial fibrillation: results from long-term follow-up. J Cardiovasc Electrophysiol 22:137–141
Chun KR, Schmidt B, Kuck KH, Andresen D, Willems S, Spitzer SG, Hoffmann E, Schumacher B, Eckardt L, Seidl K, Jünger C, Horack M, Brachmann J, Senges J (2013) Catheter ablation of atrial fibrillation in the young: insights from the German Ablation Registry. Clin Res Cardiol 102(6):459–468
Tilz RR, Rillig A, Thum AM, Arya A, Wohlmuth P, Metzner A, Mathew S, Yoshiga Y, Wissner E, Kuck KH, Ouyang F (2012) Catheter ablation of long-standing persistent atrial fibrillation: 5-year outcomes of the Hamburg Sequential Ablation Strategy. J Am Coll Cardiol 60(19):1921–1929
Rillig A, Lin T, Burchard A, Kamioka M, Heeger C, Makimoto H, Metzner A, Wissner E, Wohlmuth P, Ouyang F, Kuck KH, Tilz RR (2014) Modified energy settings are mandatory to minimize esophageal injury using the novel multipolar irrigated radiofrequency ablation catheter for pulmonary vein isolation. Europace. pii: euu269. (Epub ahead of print)
Saliba W, Reddy VY, Wazni O, Cummings JE, Burkhardt JD, Haissaguerre M, Kautzner J, Peichl P, Neuzil P, Schibgilla V, Noelker G, Brachmann J, Di Biase L, Barrett C, Jais P, Natale A (2008) Atrial fibrillation ablation using a robotic catheter remote control system: initial human experience and long-term follow-up results. J Am Coll Cardiol 51:2407–2411
Schmidt M, Dorwarth U, Straube F, Wankerl M, Krieg J, Leber AW, Ebersberger HU, Daccarett M, Huber A, Rummeny E, Hoffmann E (2012) A novel double cryoballoon strategy in persistent atrial fibrillation: a pilot study. Clin Res Cardiol 101(10):777–785
Buiatti A, Hessling G, Semmler V, Ammar S (2014) Remote magnetic navigation for persistent atrial fibrillation ablation via a retrograde aortic access: an approach for patients after atrial septal defect device closure. Clin Res Cardiol 103(12):1028–1030
Schmidt B, Tilz RR, Neven K, Julian Chun KR, Fürnkranz A, Ouyang F (2009) Remote robotic navigation and electroanatomical mapping for ablation of atrial fibrillation: considerations for navigation and impact on procedural outcome. Circ Arrhythm Electrophysiol 2:120–128
Hlivák P, Mlčochová H, Peichl P, Cihák R, Wichterle D, Kautzner J (2011) Robotic navigation in catheter ablation for paroxysmal atrial fibrillation: midterm efficacy and predictors of postablation arrhythmia recurrences. J Cardiovasc Electrophysiol 22(5):534–540
Di Biase L, Wang Y, Horton R, Gallinghouse GJ, Mohanty P, Sanchez J, Patel D, Dare M, Canby R, Price LD, Zagrodzky JD, Bailey S, Burkhardt JD, Natale A (2009) Ablation of atrial fibrillation utilizing robotic catheter navigation in comparison to manual navigation and ablation: single-center experience. J Cardiovasc Electrophysiol 20:1328–1335
Rillig A, Meyerfeldt U, Birkemeyer R, Treusch F, Kunze M, Miljak T, Zvereva V, Jung W (2010) Remote robotic catheter ablation for atrial fibrillation: how fast is it learned and what benefits can be earned? J Inter Cardiac Electrophysiol 29:109–117
Willems S, Steven D, Servatius H, Hoffmann BA, Drewitz I, Müllerleile K, Aydin MA, Wegscheider K, Salukhe TV, Meinertz T, Rostock T (2010) Persistence of Pulmonary Vein Isolation After Robotic Remote-Navigated Ablation for Atrial Fibrillation and its Relation to Clinical Outcome. J Cardiovasc Electrophysiol 21:1079–1084
Ullah W, McLean A, Hunter RJ, Baker V, Richmond L, Cantor EJ, Dhinoja MB, Sporton S, Earley MJ, Schilling RJ (2014) Randomized trial comparing robotic to manual ablation for atrial fibrillation. Heart Rhythm 11(11):1862–1869
Tilz RR, Chun KR, Metzner A, Burchard A, Wissner E, Koektuerk B, Konstantinidou M, Nuyens D, De Potter T, Neven K, Fürnkranz A, Ouyang F, Schmidt B (2010) Unexpected high incidence of esophageal injury following pulmonary vein isolation using robotic navigation. J Cardiovasc Electrophysiol 21:853–858
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Hindricks G, Kirchhof P (2012) ESC Committee for Practice Guidelines-CPG; Document Reviewers: 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation—developed with the special contribution of the European Heart Rhythm Association. Europace 14(10):1385–1413
Rillig A, Meyerfeldt U, Birkemeyer R, Wiest S, Sauer BM, Staritz M, Jung W (2010) Oesophageal temperature monitoring and incidence of oesophageal lesions after pulmonary vein isolation using a remote robotic navigation system. Europace 12:655–661
Rillig A, Meyerfeldt U, Tilz RR, Talazko J, Arya A, Zvereva V, Birkemeyer R, Miljak T, Hajredini B, Wohlmuth P, Fink U, Jung W (2012) Incidence and long-term follow-up of silent cerebral lesions after pulmonary vein isolation using a remote robotic navigation system as compared with manual ablation. Circ Arrhythm Electrophysiol 5(1):15–21
Rillig A, Meyerfeldt U, Kunze M, Birkemeyer R, Miljak T, Jäckle S, Hajredini B, Treusch F, Jung W (2010) Persistent iatrogenic atrial septal defect after a single-puncture, double-transseptal approach for pulmonary vein isolation using a remote robotic navigation system: results from a prospective study. Europace 12:331–336
Rillig A, Schmidt B, Feige B, Wissner E, Metzner A, Arya A, Mathew S, Makimoto H, Wohlmuth P, Ouyang F, Kuck KH (2013) Tilz RR (2013) Left atrial isthmus line ablation using a remote robotic navigation system: feasibility, efficacy and long-term outcome. Clin Res Cardiol 102(12):885–893
Bai R, Biase DI, Valderrabano M, Lorgat F, Mlcochova H, Tilz R, V U, Hranitzky PM, Wazni O, Kanagaratnam P, Doshi RN, Gibson D, Pisapia A, Mohanty P, Saliba W, Ouyang F, Kautzner J, Gallinghouse GJ, Natale V (2012) Worldwide experience with the robotic navigation system in catheter ablation of atrial fibrillation: methodology, efficacy and safety. J Cardiovasc Electrophysiol 23(8):820–826
Di Biase L, Natale A, Barrett C, Tan C, Elayi CS, Ching CK, Wang P, Al-Ahmad A, Arruda M, Burkhardt JD, Wisnoskey BJ, Chowdhury P, De Marco S, Armaganijan L, Litwak KN, Schweikert RA, Cummings JE (2009) Relationship between catheter forces, lesion characteristics, “popping”, and char formation: experience with robotic navigation system. J Cardiovasc Electrophysiol 20:436–440
Wakili R, Clauss S, Schmidt V, Ulbrich M, Hahnefeld A, Schüssler F, Siebermair J, Kääb S, Estner HL (2014) Impact of real-time contact force and impedance measurement in pulmonary vein isolation procedures for treatment of atrial fibrillation. Clin Res Cardiol 103(2):97–106
Steven D, Servatius H, Rostock T, Hoffmann B, Drewitz I, Müllerleile K, Sultan A, Aydin MA, Meinertz T, Willems S (2010) Reduced fluoroscopy during atrial fibrillation ablation: benefits of robotic guided navigation. J Cardiovasc Electrophysiol 21:6–12
Rillig A, Schmidt B, Steven D, Meyerfeldt U, Biase DI, Wissner E, Becker R, Thomas D, Wohlmuth P, Gallinghouse GJ, Scholz E, Jung W, Willems S, Natale A, Ouyang F, Kuck KH, Tilz R (2013) Study design of the man and machine trial: a prospective international controlled noninferiority trial comparing manual with robotic catheter ablation for treatment of atrial fibrillation. J Cardiovasc Electrophysiol 24(1):40–46
Kiliszek M, Miązek N, Peller M, Gajda S, Koźluk E, Lodziński P, Kapłon-Cieślicka A, Piątkowski R, Budaj-Fidecka A, Balsam P, Opolski G (2014) Influence of left atrial size on the outcome of pulmonary vein isolation in patients with atrial fibrillation. Kardiol Pol 72(11):1135–1140
Özcan EE, Szeplaki G, Tahin T, Osztheimer I, Szilagyi S, Apor A, Horvath PM, Vago H, Merkely B, Geller L (2014) Impact of respiration gating on image integration guided atrial fibrillation ablation. Clin Res Cardiol 103(9):727–731
Hahnefeld A, Reithmann C, Ulbrich M, Haserück N, Siebermair J, Steinbeck G (2009) CARTO versus NavX bei der Ablation von paroxysmalem Vorhofflimmern. (CAVERNA AF Studie): vergleich bei 222 konsekutiven Patienten. Clin Res Cardiol 98(1):V270
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Andreas Rillig received travel grants from Biosense Webster, Hansen Medical and St. Jude Medical and lecture fees from St. Jude Medical and takes part at the Boston scientific EP fellowship; Tina Lin received a fellowship grant from EHRA and travel grants from Biosense Webster, St. Jude Medical and Topera Medical. Roland Tilz received research grants from Hansen, St. Jude Medical, travel grants from St. Jude Medical, Topera, Biosense Webster, Daiichi Sankyo, Sentrheart and speaker‘s bureau honoraria from Biosense Webster, Biotronik, Pfizer, Topera, Bristol-Myers Squibb; Bayer, Sanofi Aventis. Prof. Kuck has received research grants from Biosense Webster, Stereotaxis, Prorhythm, Medtronic, Edwards, and Cryocath; and is a consultant to St. Jude Medical, Biosense Webster, Prorhythm, and Stereotaxis.
Rights and permissions
About this article
Cite this article
Rillig, A., Lin, T., Schmidt, B. et al. Experience matters: long-term results of pulmonary vein isolation using a robotic navigation system for the treatment of paroxysmal atrial fibrillation. Clin Res Cardiol 105, 106–116 (2016). https://doi.org/10.1007/s00392-015-0892-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-015-0892-6