Abstract
Ventricular arrhythmias (VAs) remain the major cause of mortality and sudden cardiac death (SCD) in almost all forms of heart disease. Despite so many therapeutic advances, such as pharmacological therapies, catheter ablation, and arrhythmia surgery, management of VAs remains a great challenge for cardiologists. Evidence from histological studies and from direct nerve activity recordings have suggested that increased sympathetic nerve density and activity contribute to the generation of VAs and SCD. It is well known that renal sympathetic nerve (RSN), either afferent component or efferent component, plays an important role in modulation of central sympathetic activity. We have recently shown that RSN activation by electrical stimulation significantly increases cardiac and systemic sympathetic activity and promotes the incidence of acute ischemia-induced VAs, suggesting RSN has a role in the development of VAs. Initial experience of RSN denervation (RDN) in patients with resistant hypertension showed that this novel and minimally invasive device-based approach significantly reduced not only kidney but also whole-body norepinephrine spillover. In addition, experimental studies find that left stellate ganglion nerve activity is significantly decreased after RDN. Based on these observations, it is reasonable to conclude that RDN may be an effective therapy for the management of VAs. Indeed, RDN has provided a protection against VAs in both animal models and patients. In this article, we review the role of the RSN in the generation of VAs and SCD and the role of RDN as a potential treatment strategy for VAs and SCD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ventricular arrhythmias (VAs) remain the major cause of mortality and sudden cardiac death (SCD) in almost all forms of heart disease [1, 2]. Although pharmacological therapies have an important role in the reduction of symptomatic VAs, side-effects and therapeutic failures happen in some patients [3]. For drug-refractory symptomatic patients, catheter ablation is important for reducing the frequency of VAs, especially in patients with idiopathic arrhythmias and without structural heart disease [3, 4]. However, in some cases, these therapeutic strategies may not suffice to suppress the incidence of VAs. Inhibition of sympathetic activity might be an effective choice in these particular cases, since an increase in sympathetic activity contributes to the genesis of VAs [5]. For example, left cardiac sympathetic blockade has been considered in patients with drug or ablation-refractory VAs [6, 7].
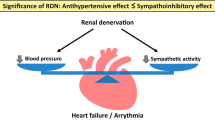
Catheter-based renal sympathetic denervation (RDN), a new approach to decrease sympathetic activity, was firstly reported by Krum et al. [8] in 2009 in patients with refractory hypertension. Over the past 4–5 years, this novel and minimally invasive device-based approach has shown promising therapeutic effects for several clinical conditions associated with chronic sympathetic activation, besides refractory hypertension [9–11]. Other collateral benefits have been reported for heart failure [12, 13], chronic kidney disease [14], obstructive sleep apnea [15], impaired glucose metabolism [15, 16], and atrial fibrillation [17–20]. Recently, several basic studies [21–23] and clinical case reports [24–30] have suggested that RDN is also an effective and safe approach for the treatment of ischemic or non-ischemic VAs. In this article, we review such novel device-based approach as a potential treatment strategy for VAs.
Role of sympathetic nervous system in the genesis of VAs and SCD
It is well accepted that the autonomic nervous system has an important role in the genesis and maintenance of VAs and SCD. Thus, modulating autonomic tone, especially inhibition of sympathetic tone, has been proposed as a method to the treatment of VAs and SCD [5, 31].
In a histological study with explanted hearts, Cao and colleagues [32] found that patients who had a history of VAs/SCD had increased density of sympathetic nerves compared to patients with similar structural heart disease but no arrhythmias, indicating that abnormally increased sympathetic nerve sprouting is in part responsible for the occurrence of VAs and SCD. Subsequently, Chen et al. [33] showed that infusion of nerve growth factor or applying sub-threshold electrical stimulation [34] to the left stellate ganglion (LSG) in dogs with myocardial infarction could increase sympathetic nerve sprouting and facilitate ventricular fibrillation and SCD, further suggesting a causal relationship. In rabbits fed with high cholesterol, there was a significant increase in nerve sprouting, sympathetic innervation, as well as ventricular vulnerability to fibrillation [35]. With directly recording nerve activity from the LSG in a canine model of SCD, Zhou et al. [36] found that increased sympathetic nerve discharges were the major triggers for malignant VAs. In addition, a series of studies in isolated rabbit hearts by Ng et al. [37, 38] showed that sympathetic nerve stimulation could increase maximum slope of restitution but decrease ventricular effective refractory period (ERP), action potential duration (APD), and ventricular fibrillation threshold. These findings suggest that increased sympathetic activity and associated ventricular electrophysiological remodeling have an important role in the generation of VAs and SCD (Fig. 1).
Cardio-renal neuraxial pathways of sympathetic nerve signaling. Renal sympathetic activation can increase nerve activity of left stellate ganglion (LSG) by increasing central sympathetic output, inducing sympathetic nerve sprouting and electrophysiological remodeling in the ventricle, which are important triggers for ventricular arrhythmias (VAs). In contrast, renal sympathetic denervation is able to decrease the whole-body sympathetic activity as well as the nerva activity of LSG, which may offer a protective effect on VAs
Considering the evidence involving autonomic mechanisms, antiadrenergic therapies should provide effective protection against VAs and SCD. Beta-blockers have been shown to reduce the incidence of ventricular tachyarrhythmias, particularly in the setting of cardiac ischemia [39, 40]. Left cardiac sympathetic denervation, e.g., LSG resection, reduced VAs in high-risk patients and dogs following myocardial infarction [41, 42] and in patients with inherited arrhythmia syndromes [43–45]. Spinal cord stimulation, which shows anti-sympathetic effects, improves cardiac function and decreases VAs in a canine model of post-infarction heart failure [46]. High thoracic epidural anesthesia, which reduces sympathetic traffic to the heart, can prevent VAs during acute myocardial ischemia in rats [47]. Our recent study showed that carotid baroreceptor stimulation displayed a beneficial effect on acute ischemia-induced VAs by sympathetic withdrawal [48]. Therefore, inhibition of sympathetic activity is a promising therapy for VAs and SCD.
Role of kidney in modulation of sympathetic activity and in the generation of VAs
The kidney communicates with the central sympathetic nervous system via renal sympathetic nerves (RSNs), which consist of efferent and afferent fibers. These nerves follow the renal artery to the kidney and are found primarily in the adventitia of the renal arteries [49]. Activation of renal efferent nerves results in volume retention, a reduction in renal blood flow, and activation of renin-angiotensin-aldosterone system through renin release [50]. Renal ischemia, hypoxia, oxidative stress, and other triggers can activate renal afferent nerves, directly influencing sympathetic outflow from the brain stem to the kidneys and other highly innervated organs [50]. Chinushi et al. [51] showed that electrical stimulation of RSN could increase the systemic blood pressure, serum catecholamine, and sympathetic nerve indices of heart rate variability, suggesting an increase in systemic sympathetic nervous activity.
In addition to modulation of the systemic sympathetic activity, we have recently shown that activation of RSN by 3-h electrical stimulation is also able to increase LSG nerve activity and promote the incidence of acute ischemia-induced VAs which can be attenuated by LSG ablation [52], indicating that there is a connection between RSN and LSG [53] (Fig. 1). Clinically, compared with patients with normal renal function, patients with chronic kidney disease have a higher risk for SCD [54, 55]. Taken together with the demonstration that the kidney plays an important role in modulation of both systemic and cardiac sympathetic activity, and RSN appears to be involved in the pathogenesis of VAs and SCD [56] (Fig. 1).
RDN as a novel approach to decrease sympathetic activity
A recent clinical study (Symplicity HTN-3) showed the absence of beneficial effects with RDN in comparison to the sham procedure in terms of blood pressure reduction [57]; however, these results might be partially due to increased placebo effect, operator learning curve, procedural discrepancies, and lack of a “biomarker” for ablation endpoint. Recently, considerable publications [58–60] still continuously reported the efficacy of RDN for the improvement of blood pressure in patients with resistant hypertension. Besides, RDN also showed therapeutic effects in other conditions due to an excessive hyper-sympathetic condition, such as heart failure [12], chronic kidney disease [14], obstructive sleep apnea [15], and impaired glucose metabolism [15, 16]. In resistant hypertension patients, RDN has been found to reduce renal norepinephrine spillover by 48 % [8], as well as muscle sympathetic nerve activity by 37 % [61]. Basic and clinical studies have both shown that RDN is able to reduce the heart rate and AV-conduction velocity, suggesting that RDN may be associated with an antiadrenergic effect [62, 63]. In ambulatory dogs, Tsai et al. [64] recorded LSG nerve activity before and after RDN using implanted radiotransmitters. They found that the 24-h average LSG nerve activity decreased from 275 mV-s at baseline to 233 mV-s 4 weeks after RDN. In a hyper-sympathetic atrial fibrillation model, Hou et al. [65] showed that LSG stimulation plus rapid atrial pacing induced an elevation in blood pressure, an increase in the sympathetic indices of heart rate variability, and a rise in plasma norepinephrine level, which could be reversed by the catheter-based RDN. These observations indicate that sympathetic denervation from kidney is able to reduce not only systemic but also cardiac sympathetic activity, therefore, may be a promising therapy for VAs and SCD.
Basic evidence for the treatment of VAs by RDN
In a recent study conducted by Linz and colleagues [21], anesthetized pigs were subjected to 20 min of acute left ventricular ischemia followed by reperfusion. They found that these pigs that underwent RDN treatment were associated with lower occurrence of VAs during ischemia compared to those that underwent sham RDN. However, RDN did not affect reperfusion-induced arrhythmias. A very recent study from our group similarly showed that RDN significantly decreased the episodes of VAs during 1-h of acute myocardial ischemia [22]. In this study, we also investigated the effects of RDN on ventricular electrophysiological properties in normal canine heart. We found that RDN significantly prolonged ventricular effective refractory period (ERP) and action potential duration (APD), reduced the dispersion of ERP and the slope of the restitution curve, and suppressed APD alternans, suggesting that RDN was able to stabilize ventricular electrophysiological properties in normal hearts. In a canine model of pacing-induced heart failure, Guo et al. [23] showed that RDN significantly decreased the corrected QT interval, the dispersions of QT interval and ventricular ERP, the heterogeneity of Cx43 distribution in ventricle, as well as the ventricular fibrillation inducibility. Their results suggested that attenuating the ventricular substrate and electrophysiological remodeling may be the potential mechanisms underlying the favorable effects of RDN on VAs in the pacing-induced heart failure model. These studies provided basic evidence that RDN was an effective therapy for the treatment of VAs associated with acute myocardial ischemia or chronic pacing-induced heart failure.
Initial clinical experience with RDN in the management of ventricular tachycardia (VT) storm
There are six small studies [24–29], so far, enrolling only 11 patients (10 males) and initially assessing the feasibility, potential efficacy, and safety of RDN in patients with resistant VT storm (Table 1).
Ukena et al. [24] reported the first-in-man experience of RDN for the treatment of VT storm in 2 patients with chronic heart failure (NYHA III). The first patient had hypertrophic cardiomyopathy, suffering from recurrent monomorphic VT despite multiple antiarrhythmic attempts, including repeated endocardial and epicardial electrophysiological ablations. The second patient, with dilated non-ischemic cardiomyopathy, had recurrent polymorphic VT and ventricular fibrillation but refused catheter ablation. After obtaining informed patient consent, both the patients underwent a bilateral RDN with six ablations at 8 W for 2 min each, without any apparent procedural complications. Blood pressure remained stable during the procedure and follow-up. In both the patients, ventricular tachyarrhythmias were significantly reduced in the first few days after RDN and finally dissipated during up to 6-month follow-up. Interestingly, the second patient who began to use insulin medication 4 years before RDN was able to continuously reduce and eventually terminate this medication.
Clinically using RDN in the treatment of acute myocardial infarction-related VT storm was first reported by Hoffmann et al. [25]. In this case report, a 63-year-old patient who successfully underwent thrombus extraction and percutaneous coronary intervention continued to show recurrent monomorphic VT and fibrillation episodes despite maximum dose of antiarrhythmic drug therapy. VT ablation still failed to eliminate the episodes of ventricular tachyarrhythmias. Due to an increasing instability, RDN was performed. The frequency of episodes dramatically decreased from 3.2/day pre-ablation (6 days, 19 episodes) to 1.8/day post-ablation (6 days, 11 episodes), and the patient had no further VAs episodes after day 23 and up to 6-month follow-up.
Recently, Remo et al. [27] reported four patients with cardiomyopathy (2 non-ischemic, 2 ischemic) suffering from recurrent monomorphic or polymorphic VT despite maximized antiarrhythmic therapy and prior ablation. RDN was successfully performed without any acute or chronic complications. The number of VT episodes was decreased from 11.0 ± 4.2 during the month pre-ablation to 0.3 ± 0.1 per month post-ablation. Another new finding of this study was that the responses to RDN were similar for ischemic and non-ischemic patients.
Similar conclusions were reached by Staico et al. [26] and Scholz et al. [28], who also showed that RDN was effective and safe for the treatment of resistant VT storm in dilated cardiomyopathy patients. Although single-sided RDN in patients with renal artery stenosis was questioned by Wang [66], several case reports suggest that single-sided RDN may be effective and safe in selected patients [67, 68]. Interestingly, Hilbert et al. [29] recently reported that single-sided RDN was able to prevent the episodes of VTs as well in a patient with ischemic cardiomyopathy. These case reports described above only evaluated the implication of RDN in old people (age range 57–83 years). A recent case report by Kosiuk et al. [30] has demonstrated that young people with therapy-resistant VT storm also can be treated by RDN. A 23-year-old male patient with ischemic cardiomyopathy suffered from VT storm despite both endocardial and epicardial catheter ablations, and maximum tolerable dose of beta-blockers. No evidence of VT which allowed reduction of antiarrhythmic drug dosage was achieved 3 days after the performance of RDN and during 10 months of follow-up.
Present challenges and future directions
Although this novel therapeutic approach appears promising in the treatment of VAs, only 11 patients with therapy-resistant VT storm were enrolled in these cases. Therefore, it warrants further clinical investigation. Accordingly, two ongoing trials (NCT01858194 and NCT02071511, Table 2) will provide a more precise definition of the role of RDN in the treatment of VAs.
For this novel technology, there are several challenges with RDN, not only in patients with resistant hypertension but also in patients with VAs. The first challenge is the selection of patients. Genesis of VAs is multifactorial, including not only sympathetic activation but also genetic factor, electrolyte disorder, and organic heart disease. Therefore, simply stating that a patient with VAs will be assigned to RDN therapy is inexact. Since RDN has shown to reduce efferent renal and central sympathetic activity [10], it is likely that patients with pronounced sympathetic overactivity would benefit the most from RDN [69]. Assessment of sympathetic activity before RDN may be suggested to perform in future studies. The second challenge being equally important is the selection of ablation parameters, including power, temperature, ablation time, impedance, and number of ablations. To date, several RDN systems have been employed in clinical studies, such as Medtronic’s Symplicity system, St. Jude’s Enlig HTN system, Vessix’s V2 system, and so on [70]. It should be noted that these systems displayed different ablation parameters which were chosen on the basis of limited animal and human autopsy data. None of the settings have been confirmed by pre-clinical studies. Therefore, future studies should meticulously investigate the effectiveness of ablation with different procedural parameters. Another possible reason for the incomplete ablation is lack of effective method to identify the ablation target and confirm the endpoint of ablation, and this is the third challenge. Electrical stimulation of renal arteries before and after ablation has been proposed as a method to identify renal nerves and confirm the completeness of RDN both in animals [22, 51, 71] and in patients [17, 72]. However, this method was questioned by Tsiachris et al. [73], who suggested that renal hemodynamic parameters may be used as direct invasive markers of successful of RDN [74]. Anyway, the best method of identification of renal nerves and confirmation of complete ablation also need further study to explore.
Conclusions
VAs remain the major cause of mortality and SCD in almost all forms of heart disease. Despite so many therapeutic advances, such as pharmacological therapies, catheter ablation, and arrhythmia surgery, management of VAs remains a great challenge for cardiologists. Increased sympathetic activity is important in the generation of VAs and SCD. The kidney has been shown to play an important role in modulation of both systemic and cardiac sympathetic activity. Basic and clinical studies recently suggest that RDN is able to reduce not only systemic but also cardiac sympathetic activity, indicating that RDN may be a promising therapy for VAs and SCD. Indeed, RDN has provided a protection against VAs in both animal models and patients. However, all the initial clinical data so far are case reports without satisfactory trial design, and publication bias cannot be excluded. The ongoing trials will provide a more precise definition of the role of RDN in the treatment of VAs. However, since this is a novel therapy strategy, several challenges (e.g., selection of patients and ablation parameters) need to be addressed before being widely used.
Abbreviations
- APD:
-
Action potential duration
- ERP:
-
Effective refractory period
- LSG:
-
Left stellate ganglion
- RDN:
-
Renal sympathetic denervation
- RSN:
-
Renal sympathetic nerve
- SCD:
-
Sudden cardiac death
- VAs:
-
Ventricular arrhythmias
- VT:
-
Ventricular tachycardia
References
John RM, Tedrow UB, Koplan BA, Albert CM, Epstein LM, Sweeney MO, Miller AL, Michaud GF, Stevenson WG (2012) Ventricular arrhythmias and sudden cardiac death. Lancet 380(9852):1520–1529. doi:10.1016/S0140-6736(12)61413-5
Chugh SS, Reinier K, Teodorescu C, Evanado A, Kehr E, Al Samara M, Mariani R, Gunson K, Jui J (2008) Epidemiology of sudden cardiac death: clinical and research implications. Prog Cardiovasc Dis 51(3):213–228. doi:10.1016/j.pcad.2008.06.003
Aliot EM, Stevenson WG, Almendral-Garrote JM, Bogun F, Calkins CH, Delacretaz E, Della Bella P, Hindricks G, Jais P, Josephson ME, Kautzner J, Kay GN, Kuck KH, Lerman BB, Marchlinski F, Reddy V, Schalij MJ, Schilling R, Soejima K, Wilber D, European Heart Rhythm A, Registered Branch of the European Society of C, Heart Rhythm S, American College of C, American Heart A (2009) EHRA/HRS Expert Consensus on Catheter Ablation of Ventricular Arrhythmias: developed in a partnership with the European Heart Rhythm Association (EHRA), a Registered Branch of the European Society of Cardiology (ESC), and the Heart Rhythm Society (HRS); in collaboration with the American College of Cardiology (ACC) and the American Heart Association (AHA). Heart rhythm 6(6):886–933. doi:10.1016/j.hrthm.2009.04.030
Winterfield JR, Mahapatra S, Wilber DJ (2013) Catheter ablation of ventricular arrhythmias: targets, tactics, and tools. Curr Opin Cardiol 28(3):344–353. doi:10.1097/HCO.0b013e328360443f
Shen MJ, Zipes DP (2014) Role of the autonomic nervous system in modulating cardiac arrhythmias. Circ Res 114(6):1004–1021. doi:10.1161/CIRCRESAHA.113.302549
Hayase J, Patel J, Narayan SM, Krummen DE (2013) Percutaneous stellate ganglion block suppressing VT and VF in a patient refractory to VT ablation. J Cardiovasc Electrophysiol 24(8):926–928. doi:10.1111/jce.12138
Patel RA, Priore DL, Szeto WY, Slevin KA (2011) Left stellate ganglion blockade for the management of drug-resistant electrical storm. Pain Med 12(8):1196–1198. doi:10.1111/j.1526-4637.2011.01167.x
Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, Kapelak B, Walton A, Sievert H, Thambar S, Abraham WT, Esler M (2009) Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 373(9671):1275–1281. doi:10.1016/S0140-6736(09)60566-3
Symplicity HTNI (2011) Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension 57(5):911–917. doi:10.1161/HYPERTENSIONAHA.110.163014
Schlaich MP, Sobotka PA, Krum H, Lambert E, Esler MD (2009) Renal sympathetic-nerve ablation for uncontrolled hypertension. N Engl J Med 361(9):932–934. doi:10.1056/NEJMc0904179
Krum H, Schlaich MP, Sobotka PA, Bohm M, Mahfoud F, Rocha-Singh K, Katholi R, Esler MD (2014) Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet 383(9917):622–629. doi:10.1016/S0140-6736(13)62192-3
Davies JE, Manisty CH, Petraco R, Barron AJ, Unsworth B, Mayet J, Hamady M, Hughes AD, Sever PS, Sobotka PA, Francis DP (2013) First-in-man safety evaluation of renal denervation for chronic systolic heart failure: primary outcome from REACH-Pilot study. Int J Cardiol 162(3):189–192. doi:10.1016/j.ijcard.2012.09.019
Bohm M, Ewen S, Kindermann I, Linz D, Ukena C, Mahfoud F (2014) Renal denervation and heart failure. Eur J Heart Fail 16(6):608–613. doi:10.1002/ejhf.83
Kiuchi MG, Maia GL, de Queiroz Carreira MA, Kiuchi T, Chen S, Andrea BR, Graciano ML, Lugon JR (2013) Effects of renal denervation with a standard irrigated cardiac ablation catheter on blood pressure and renal function in patients with chronic kidney disease and resistant hypertension. Eur Heart J 34(28):2114–2121. doi:10.1093/eurheartj/eht200
Witkowski A, Prejbisz A, Florczak E, Kadziela J, Sliwinski P, Bielen P, Michalowska I, Kabat M, Warchol E, Januszewicz M, Narkiewicz K, Somers VK, Sobotka PA, Januszewicz A (2011) Effects of renal sympathetic denervation on blood pressure, sleep apnea course, and glycemic control in patients with resistant hypertension and sleep apnea. Hypertension 58(4):559–565. doi:10.1161/HYPERTENSIONAHA.111.173799
Mahfoud F, Schlaich M, Kindermann I, Ukena C, Cremers B, Brandt MC, Hoppe UC, Vonend O, Rump LC, Sobotka PA, Krum H, Esler M, Bohm M (2011) Effect of renal sympathetic denervation on glucose metabolism in patients with resistant hypertension: a pilot study. Circulation 123(18):1940–1946. doi:10.1161/CIRCULATIONAHA.110.991869
Pokushalov E, Romanov A, Corbucci G, Artyomenko S, Baranova V, Turov A, Shirokova N, Karaskov A, Mittal S, Steinberg JS (2012) A randomized comparison of pulmonary vein isolation with versus without concomitant renal artery denervation in patients with refractory symptomatic atrial fibrillation and resistant hypertension. J Am Coll Cardiol 60(13):1163–1170. doi:10.1016/j.jacc.2012.05.036
Pokushalov E, Romanov A, Katritsis DG, Artyomenko S, Bayramova S, Losik D, Baranova V, Karaskov A, Steinberg JS (2014) Renal denervation for improving outcomes of catheter ablation in patients with atrial fibrillation and hypertension: early experience. Heart rhythm 11(7):1131–1138. doi:10.1016/j.hrthm.2014.03.055
Linz D, van Hunnik A, Ukena C, Ewen S, Mahfoud F, Schirmer SH, Lenski M, Neuberger HR, Schotten U, Bohm M (2014) Renal denervation: effects on atrial electrophysiology and arrhythmias. Clin Res Cardiol 103(10):764–774. doi:10.1007/s00392-014-0695-1
Zhang M, Tao H, Shi KH (2014) Renal denervation as a friend of catheter ablation in patients with atrial fibrillation and hypertension. Clin Res Cardiol. doi:10.1007/s00392-014-0752-9
Linz D, Wirth K, Ukena C, Mahfoud F, Poss J, Linz B, Bohm M, Neuberger HR (2013) Renal denervation suppresses ventricular arrhythmias during acute ventricular ischemia in pigs. Heart rhythm 10(10):1525–1530. doi:10.1016/j.hrthm.2013.07.015
Huang B, Yu L, He B, Lu Z, Wang S, He W, Yang K, Liao K, Zhang L, Jiang H (2014) Renal sympathetic denervation modulates ventricular electrophysiology and has a protective effect on ischaemia-induced ventricular arrhythmia. Exp Physiol 99(11):1467–1477. doi:10.1113/expphysiol.2014.082057
Guo Z, Zhao Q, Deng H, Tang Y, Wang X, Dai Z, Xiao J, Wan P, Wang X, Huang H, Huang C (2014) Renal sympathetic denervation attenuates the ventricular substrate and electrophysiological remodeling in dogs with pacing-induced heart failure. Int J Cardiol 175(1):185–186. doi:10.1016/j.ijcard.2014.04.189
Ukena C, Bauer A, Mahfoud F, Schreieck J, Neuberger HR, Eick C, Sobotka PA, Gawaz M, Bohm M (2012) Renal sympathetic denervation for treatment of electrical storm: first-in-man experience. Clin Res Cardiol 101(1):63–67. doi:10.1007/s00392-011-0365-5
Hoffmann BA, Steven D, Willems S, Sydow K (2013) Renal sympathetic denervation as an adjunct to catheter ablation for the treatment of ventricular electrical storm in the setting of acute myocardial infarction. J Cardiovasc Electrophysiol 24(12):E21. doi:10.1111/jce.12282
Staico R, Armaganijan L, Moreira D, Medeiros P, Melo J, Lopes R, Ribamar Costa J, Abizaid A (2013) Renal sympathetic denervation and ventricular arrhythmias: a case of electrical storm with multiple renal arteries. EuroIntervention 10(1):166. doi:10.4244/EIJV10I1A25
Remo BF, Preminger M, Bradfield J, Mittal S, Boyle N, Gupta A, Shivkumar K, Steinberg JS, Dickfeld T (2014) Safety and efficacy of renal denervation as a novel treatment of ventricular tachycardia storm in patients with cardiomyopathy. Heart rhythm 11(4):541–546. doi:10.1016/j.hrthm.2013.12.038
Scholz EP, Raake P, Thomas D, Vogel B, Katus HA, Blessing E (2014) Rescue renal sympathetic denervation in a patient with ventricular electrical storm refractory to endo- and epicardial catheter ablation. Clin Res Cardiol. doi:10.1007/s00392-014-0749-4
Hilbert S, Rogge C, Papageorgiou P, Hindricks G, Bollmann A (2014) Successful single-sided renal denervation in drug-resistant hypertension and ventricular tachycardia. Clin Res Cardiol. doi:10.1007/s00392-014-0790-3
Kosiuk J, Hilbert S, Pokushalov E, Hindricks G, Steinberg JS, Bollmann A (2014) Renal denervation for treatment of cardiac arrhythmias: state of the art and future directions. J Cardiovasc Electrophysiol. doi:10.1111/jce.12553
Zipes DP (2008) Heart-brain interactions in cardiac arrhythmias: role of the autonomic nervous system. Cleve Clin J Med 75(Suppl 2):S94–S96
Cao JM, Fishbein MC, Han JB, Lai WW, Lai AC, Wu TJ, Czer L, Wolf PL, Denton TA, Shintaku IP, Chen PS, Chen LS (2000) Relationship between regional cardiac hyperinnervation and ventricular arrhythmia. Circulation 101(16):1960–1969
Cao JM, Chen LS, KenKnight BH, Ohara T, Lee MH, Tsai J, Lai WW, Karagueuzian HS, Wolf PL, Fishbein MC, Chen PS (2000) Nerve sprouting and sudden cardiac death. Circ Res 86(7):816–821
Swissa M, Zhou S, Gonzalez-Gomez I, Chang CM, Lai AC, Cates AW, Fishbein MC, Karagueuzian HS, Chen PS, Chen LS (2004) Long-term subthreshold electrical stimulation of the left stellate ganglion and a canine model of sudden cardiac death. J Am Coll Cardiol 43(5):858–864. doi:10.1016/j.jacc.2003.07.053
Liu YB, Wu CC, Lu LS, Su MJ, Lin CW, Lin SF, Chen LS, Fishbein MC, Chen PS, Lee YT (2003) Sympathetic nerve sprouting, electrical remodeling, and increased vulnerability to ventricular fibrillation in hypercholesterolemic rabbits. Circ Res 92(10):1145–1152. doi:10.1161/01.RES.0000072999.51484.92
Zhou S, Jung BC, Tan AY, Trang VQ, Gholmieh G, Han SW, Lin SF, Fishbein MC, Chen PS, Chen LS (2008) Spontaneous stellate ganglion nerve activity and ventricular arrhythmia in a canine model of sudden death. Heart rhythm 5(1):131–139. doi:10.1016/j.hrthm.2007.09.007
Ng GA, Brack KE, Patel VH, Coote JH (2007) Autonomic modulation of electrical restitution, alternans and ventricular fibrillation initiation in the isolated heart. Cardiovasc Res 73(4):750–760. doi:10.1016/j.cardiores.2006.12.001
Ng GA, Mantravadi R, Walker WH, Ortin WG, Choi BR, de Groat W, Salama G (2009) Sympathetic nerve stimulation produces spatial heterogeneities of action potential restitution. Heart rhythm 6(5):696–706. doi:10.1016/j.hrthm.2009.01.035
Steinbeck G, Andresen D, Bach P, Haberl R, Oeff M, Hoffmann E, von Leitner ER (1992) A comparison of electrophysiologically guided antiarrhythmic drug therapy with beta-blocker therapy in patients with symptomatic, sustained ventricular tachyarrhythmias. N Engl J Med 327(14):987–992. doi:10.1056/NEJM199210013271404
Antz M, Cappato R, Kuck KH (1995) Metoprolol versus sotalol in the treatment of sustained ventricular tachycardia. J Cardiovasc Pharmacol 26(4):627–635
Schwartz PJ, Snebold NG, Brown AM (1976) Effects of unilateral cardiac sympathetic denervation on the ventricular fibrillation threshold. Am J Cardiol 37(7):1034–1040
Schwartz PJ, Motolese M, Pollavini G, Lotto A, Ruberti U, Trazzi R, Bartorelli C, Zanchetti A, TISDPG (1992) Prevention of sudden cardiac death after a first myocardial infarction by pharmacologic or surgical antiadrenergic interventions. J Cardiovasc Electrophysiol 3:2–16
Wilde AA, Bhuiyan ZA, Crotti L, Facchini M, De Ferrari GM, Paul T, Ferrandi C, Koolbergen DR, Odero A, Schwartz PJ (2008) Left cardiac sympathetic denervation for catecholaminergic polymorphic ventricular tachycardia. N Engl J Med 358(19):2024–2029. doi:10.1056/NEJMoa0708006
Schwartz PJ, Locati EH, Moss AJ, Crampton RS, Trazzi R, Ruberti U (1991) Left cardiac sympathetic denervation in the therapy of congenital long QT syndrome. A worldwide report. Circulation 84(2):503–511
Schneider HE, Steinmetz M, Krause U, Kriebel T, Ruschewski W, Paul T (2013) Left cardiac sympathetic denervation for the management of life-threatening ventricular tachyarrhythmias in young patients with catecholaminergic polymorphic ventricular tachycardia and long QT syndrome. Clin Res Cardiol 102(1):33–42. doi:10.1007/s00392-012-0492-7
Lopshire JC, Zhou X, Dusa C, Ueyama T, Rosenberger J, Courtney N, Ujhelyi M, Mullen T, Das M, Zipes DP (2009) Spinal cord stimulation improves ventricular function and reduces ventricular arrhythmias in a canine postinfarction heart failure model. Circulation 120(4):286–294. doi:10.1161/CIRCULATIONAHA.108.812412
Blomberg S, Ricksten SE (1988) Thoracic epidural anaesthesia decreases the incidence of ventricular arrhythmias during acute myocardial ischaemia in the anaesthetized rat. Acta Anaesthesiol Scand 32(3):173–178
Liao K, Yu L, He B, Huang B, Yang K, Saren G, Wang S, Zhou X, Jiang H (2014) Carotid baroreceptor stimulation prevents arrhythmias induced by acute myocardial infarction through autonomic modulation. J Cardiovasc Pharmacol 64(5):431–437. doi:10.1097/FJC.0000000000000135
Schlaich MP, Sobotka PA, Krum H, Whitbourn R, Walton A, Esler MD (2009) Renal denervation as a therapeutic approach for hypertension: novel implications for an old concept. Hypertension 54(6):1195–1201. doi:10.1161/HYPERTENSIONAHA.109.138610
Schlaich MP, Hering D, Sobotka PA, Krum H, Esler MD (2012) Renal denervation in human hypertension: mechanisms, current findings, and future prospects. Curr Hypertens Rep 14(3):247–253. doi:10.1007/s11906-012-0264-9
Chinushi M, Izumi D, Iijima K, Suzuki K, Furushima H, Saitoh O, Furuta Y, Aizawa Y, Iwafuchi M (2013) Blood pressure and autonomic responses to electrical stimulation of the renal arterial nerves before and after ablation of the renal artery. Hypertension 61(2):450–456. doi:10.1161/HYPERTENSIONAHA.111.00095
Huang B, Yu L, Scherlag BJ, Wang S, He B, Yang K, Liao K, Lu Z, He W, Zhang L, Po SS, Jiang H (2014) Left renal nerves stimulation facilitates ischemia-induced ventricular arrhythmia by increasing nerve activity of left stellate ganglion. J Cardiovasc Electrophysiol 25(11):1249–1256. doi:10.1111/jce.12498
Tsai WC, Chen PS (2014) Cross talk between renal and cardiac autonomic nerves: is this how renal denervation works? J Cardiovasc Electrophysiol. doi:10.1111/jce.12532
Dalal D, de Jong JS, Tjong FV, Wang Y, Bruinsma N, Dekker LR, Wilde AA (2012) Mild-to-moderate kidney dysfunction and the risk of sudden cardiac death in the setting of acute myocardial infarction. Heart rhythm 9(4):540–545. doi:10.1016/j.hrthm.2011.11.014
McCloskey LW, Psaty BM, Koepsell TD, Aagaard GN (1992) Level of blood pressure and risk of myocardial infarction among treated hypertensive patients. Arch Intern Med 152(3):513–520
Huang B, Lu Z, Jiang H (2014) Does the kidney play an important role in the generation of ventricular arrhythmias and sudden cardiac death? Clin Res Cardiol. doi:10.1007/s00392-014-0768-1
Bhatt DL, Kandzari DE, O’Neill WW, D’Agostino R, Flack JM, Katzen BT, Leon MB, Liu M, Mauri L, Negoita M, Cohen SA, Oparil S, Rocha-Singh K, Townsend RR, Bakris GL, Investigators SH- (2014) A controlled trial of renal denervation for resistant hypertension. N Engl J Med 370(15):1393–1401. doi:10.1056/NEJMoa1402670
Esler MD, Bohm M, Sievert H, Rump CL, Schmieder RE, Krum H, Mahfoud F, Schlaich MP (2014) Catheter-based renal denervation for treatment of patients with treatment-resistant hypertension: 36 month results from the SYMPLICITY HTN-2 randomized clinical trial. Eur Heart J 35(26):1752–1759. doi:10.1093/eurheartj/ehu209
Papademetriou V, Tsioufis CP, Sinhal A, Chew DP, Meredith IT, Malaiapan Y, Worthley MI, Worthley SG (2014) Catheter-based renal denervation for resistant hypertension: 12-month results of the Enlig HTN I first-in-human study using a multielectrode ablation system. Hypertension 64(3):565–572. doi:10.1161/HYPERTENSIONAHA.114.03605
Dorr O, Liebetrau C, Mollmann H, Mahfoud F, Ewen S, Gaede L, Troidl C, Hoffmann J, Busch N, Laux G, Wiebe J, Bauer T, Hamm C, Nef H (2014) Beneficial effects of renal sympathetic denervation on cardiovascular inflammation and remodeling in essential hypertension. Clin Res Cardiol. doi:10.1007/s00392-014-0773-4
Hering D, Lambert EA, Marusic P, Walton AS, Krum H, Lambert GW, Esler MD, Schlaich MP (2013) Substantial reduction in single sympathetic nerve firing after renal denervation in patients with resistant hypertension. Hypertension 61(2):457–464. doi:10.1161/HYPERTENSIONAHA.111.00194
Linz D, Mahfoud F, Schotten U, Ukena C, Hohl M, Neuberger HR, Wirth K, Bohm M (2013) Renal sympathetic denervation provides ventricular rate control but does not prevent atrial electrical remodeling during atrial fibrillation. Hypertension 61(1):225–231. doi:10.1161/HYPERTENSIONAHA.111.00182
Ukena C, Mahfoud F, Spies A, Kindermann I, Linz D, Cremers B, Laufs U, Neuberger HR, Bohm M (2013) Effects of renal sympathetic denervation on heart rate and atrioventricular conduction in patients with resistant hypertension. Int J Cardiol 167(6):2846–2851. doi:10.1016/j.ijcard.2012.07.027
Tsai WC, Chan YH, Chinda K, Lai WT, Lin SF, Chen PS (2014) Renal sympathetic denervation decreases the incidence of atrial tachycardia and improves baroreflex sensitivity in ambulatory dogs. Heart Rhythm 11:S236
Hou Y, Hu J, Po SS, Wang H, Zhang L, Zhang F, Wang K, Zhou Q (2013) Catheter-based renal sympathetic denervation significantly inhibits atrial fibrillation induced by electrical stimulation of the left stellate ganglion and rapid atrial pacing. PLoS One 8(11):e78218. doi:10.1371/journal.pone.0078218
Wang Y (2014) Patients with renal artery stenosis may not be suitable for renal denervation. Clin Res Cardiol 103(7):585–586. doi:10.1007/s00392-014-0700-8
Schroeter MR, Koziolek M (2014) Early reduction of therapy-resistant hypertension in a patient after single-sided renal denervation approach. Clin Res Cardiol 103(1):79–81. doi:10.1007/s00392-013-0634-6
Armaganijan L, Staico R, Abizaid A, Moraes A, Moreira D, Amodeo C, Sousa M, Sousa JE (2013) Unilateral renal artery sympathetic denervation may reduce blood pressure in patients with resistant hypertension. J Clin Hypertens 15(8):606. doi:10.1111/jch.12121
Zuern CS, Eick C, Rizas KD, Bauer S, Langer H, Gawaz M, Bauer A (2013) Impaired cardiac baroreflex sensitivity predicts response to renal sympathetic denervation in patients with resistant hypertension. J Am Coll Cardiol 62(22):2124–2130. doi:10.1016/j.jacc.2013.07.046
Papademetriou V, Rashidi AA, Tsioufis C, Doumas M (2014) Renal nerve ablation for resistant hypertension: how did we get here, present status, and future directions. Circulation 129(13):1440–1451. doi:10.1161/CIRCULATIONAHA.113.005405
Hao Y, Lu Z (2014) Renal denervation: should we still hang in there? Int J Cardiol 176(3):1255–1256. doi:10.1016/j.ijcard.2014.07.196
Gal P, de Jong MR, Smit JJ, Adiyaman A, Staessen JA, Elvan A (2014) Blood pressure response to renal nerve stimulation in patients undergoing renal denervation: a feasibility study. J Hum Hypertens. doi:10.1038/jhh.2014.91
Tsiachris D, Tsioufis C, Dimitriadis K, Kordalis A, Thomopoulos C, Kasiakogias A, Papalois A, Papademetriou V, Tousoulis D, Stefanadis C (2014) Electrical stimulation of the renal arterial nerves does not unmask the blindness of renal denervation procedure in swine. Int J Cardiol 176(3):1061–1063. doi:10.1016/j.ijcard.2014.07.141
Tsioufis C, Papademetriou V, Dimitriadis K, Tsiachris D, Thomopoulos C, Park E, Hata C, Papalois A, Stefanadis C (2013) Catheter-based renal sympathetic denervation exerts acute and chronic effects on renal hemodynamics in swine. Int J Cardiol 168(2):987–992. doi:10.1016/j.ijcard.2012.10.038
Acknowledgments
This work was supported by the grants from National Natural Science Foundation of China (81270339; 81300182; 81370281; 81270250; 81300181), Science and Technology Research Project of Wuhan (201306060201010271), Natural Science Foundation of Hubei Province (2013CFB302), and Fundamental Research Funds for the Central Universities (2012302020206; 2042012kf1099; 2042014kf0110).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, B., Scherlag, B.J., Yu, L. et al. Renal sympathetic denervation for treatment of ventricular arrhythmias: a review on current experimental and clinical findings. Clin Res Cardiol 104, 535–543 (2015). https://doi.org/10.1007/s00392-015-0812-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-015-0812-9