Abstract
Background
Sleep disordered breathing (SDB) has important clinical implications in patients with congestive heart failure (CHF). We performed portable recording in unselected CHF patients on contemporary therapy. Data on the interactions of SDB in patients supervised at heart failure clinics are rare and we illustrate diversities of obstructive sleep apnoea (OSA) and central sleep apnoea (CSA).
Methods
We studied 176 consecutive subjects on contemporary medical therapy with a median left ventricular ejection fraction of 25.0 % (range 7–35 %) and median NT-pro BNP levels of 3,413.0 pg/ml (range 305.1–35,000.0 pg/ml). Participants underwent prospective overnight portable recording.
Results
50 % presented with an at least moderate form of nocturnal breathing disorder [apnoea–hypopnoea index (AHI) ≥15/h]. Only 15 patients (17.1 %) with AHI ≥15/h reported excessive daytime sleepiness. Irrespective of left ventricular ejection fraction, patients with CSA had higher levels of NT-pro BNP compared to patients with OSA (differences in medians = 2,639.0 pg/ml, p = 0.016), and compared to patients with an AHI <15/h (differences in medians = 2,710.0 pg/ml, p < 0.001). OSA affected 26 patients (14.8 %).
Conclusions
Patients with severe stable CHF on contemporary therapy have a prevalence of 50.0 % of moderate to severe SDB. The natural cascade of the failing heart is initially characterised by absent SDB or OSA, whereas end-stage CHF is associated with CSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congestive heart failure (CHF) is one of the leading causes of mortality and hospitalisations in the industrialised world. Despite several evidence-based treatment options, prognosis remains poor. In CHF patients, nocturnal breathing disorders are highly prevalent [1–7]. The repetitive oxygen saturation drops may trigger heart failure progression by exposing the myocardium to additional increased sympathetic nervous system activity, [8–10] enlarge preload and afterload, [11, 12] induce arrhythmias, [4, 12–15] and finally contribute to mortality [16, 17].
Previous investigations on the prevalence of sleep apnoea (SA) in patients with depressed left ventricular ejection fraction (LVEF) are multifaceted and therefore difficult to interpret. Beside the use of attended full in-lab polysomnography, [1–3] different AHI cut-off thresholds for diagnosis of SDB were used [6, 7]. Furthermore, it remains unclear if patients were examined with suspicion of SDB, [2–5] or if patients were on optimal medical heart failure therapy [4, 6, 7]. Beta blockade is sought to reduce the prevalence of SDB [18, 19], but in some studies, the beta-blocker status is either unknown or limited to a minority of participants (10–53 %) [2, 4].
Given that SDB in CHF patients has important clinical implications, we performed polygraphic screening in unselected patients of our heart failure clinic. Compared to attended full in-lab polysomnography, we used less expensive and easily available portable recording (PR) devices. Furthermore, we describe diversities of obstructive sleep apnoea (OSA) and central sleep apnoea (CSA), as well as the association of SDB and heart failure progression.
Methods
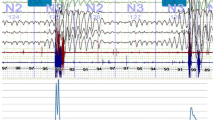
We studied the prevalence of SDB in consecutive patients diagnosed with severe CHF on optimal medical therapy (OMT) under supervision of the heart failure clinic in our hospital. Subjects underwent prospectively unattended level 3 overnight PR using a six channel device (Embletta X10®). Nasal airflow and snoring were detected by nasal pressure. Respiratory plethysmography was used to record thoracic and abdominal effort. Additional measurements included pulse oximetry and body position.
Participants were either recently hospitalised for heart failure or for heart transplantation evaluation. Stable severe heart failure patients for at least three months on contemporary medical therapy according to current guidelines were included prospectively irrespective of symptoms associated with SDB [20]. They suffered from at least moderate to severe impaired LVEF, and levels of amino-terminal fragment of brain natriuretic peptide (NT-pro BNP) exceeded 300 picogram per milliliter (pg/ml).
We excluded patients with clinical signs of instability, chronic obstructive pulmonary disease with long-term oxygen use, as well as primary valvular heart disease and those patients being already treated by non-invasive ventilation therapy. Participants were originally included into an on-going observational study to assess the accuracy of portable monitoring in reference to full in-lab polysomnography in CHF. We performed the study in compliance with the Declaration of Helsinki. Our institutional review board approved the protocol and each patient gave written informed consent.
Sleep disordered breathing and scoring of respiratory events
According to the American Academy of Sleep Medicine, abnormal breathing events were classified as apnoeas and hypopnoeas, as well as obstructive and central events [21]. The AHI reflects the summation of respiratory events per hour and quantifies the severity of SDB. An apnoea had to display a cessation of ventilation (nasal airflow and respiratory drive to <10 % of the mean preceding signal) for at least 10 s. It was scored as a central event if the respiratory drive of the chest and abdomen was absent, and classified as obstructive event if chest and abdominal motions were present. A respiratory event was categorised as a hypopnoea in the case of a clear amplitude reduction of the ventilation to at least <70 % of the mean preceding signal lasting for at least 10 s, but not meeting the criteria of an apnoea, and with an event associated drop of oxygen saturation equal to or greater than 4 % [22]. A hypopnoea was classified as a central event if the chest and abdominal respiratory drive signal was in phase without any evidence of narrowed upper airways, as detected by a reduction of nasal airflow signal [23]. By contrast, obstructive events were defined as event associated flow limitation of the nasal flow signal or persistent or increasing respiratory effort out of phase with or without snoring [23].
Respiratory event scoring
Patients with an AHI ≥15/h were considered to be suffering from relevant SDB. Respiratory events were divided into obstructive or central events. OSA was diagnosed in case of an AHI ≥15/h and if the central events were <50 % of the total AHI. CSA was diagnosed if the OSA-related events were <50 % and an AHI ≥15/h was present. Blinded experienced readers (P.D., L.S.) scored all records manually in consensus with the aid of a computerised scoring system (Somnologica for Embletta Version 5.1.1).
Evaluation of daytime sleepiness
The epworth sleepiness scale (ESS) was used to assess the degree of daytime sleepiness [24]. A patient with a score of >11 was considered as being excessively sleepy.
Statistical analysis
Continuous variables are described as mean ± standard deviation (SD) and range in the case of (group-wise) approximate normal distribution and as median and range otherwise. Comparisons between two groups are performed using independent samples t tests in the former case and using Wilcoxon’s rank sum test in the latter. Categorical variables are described as absolute and relative frequencies and compared between two groups using Chi-square tests. In the case of all pairwise comparisons between three groups, the three p values are corrected using Shaffer’s method by multiplying the smallest p value by the factor three. However, in the case of normally distributed outcomes, Tukey’s correction was employed. No correction for multiple testing with respect to the number of variables has been performed due to the exploratory character of the study, p values and confidence intervals have to be interpreted accordingly. All computations have been performed using SAS software Version 9.2 (SAS Institute Inc., Cary, NC, USA, 2002–2008).
Results
Patient characteristics
A total of 176 patients were investigated with the overnight recording device. Demographic data and concomitant medical therapy are provided in Table 1. The median age was 65.1 years with a range from 33.1 to 88.2 years. Median LVEF was 25.0 % with a range of 7.0–35.0 %. Median levels of NT-pro BNP were 3,413.0 pg/ml with a range from 305.1 to 35,000.0 pg/ml. Optimised CHF therapy consisted of either angiotensin-converting enzyme (ACE) inhibitor or angiotensin-II (AT-2) blocker therapy in 172 patients (97.7 %), beta blockade in 159 patients (90.3 %), and spironolactone in 106 patients (60.2 %).
Prevalence of SDB
88 patients (50.0 %) had an AHI ≥15/h, indicating an at least moderate manifestation of SDB. Of these patients, only a minority of 15 patients (17.1 %) reported excessive daytime sleepiness. By analysing the main type of breathing disorder, 26 patients (14.8 %) suffered from OSA, and 61 patients (34.6 %) exhibited CSA. One patient (0.6 %) was not further classifiable. 88 patients (50.0 %) presented with a mild form or absent sleep apnoea syndrome (AHI <15/h) as displayed in Table 2. Out of 88 patients with relevant SDB, 22 patients are currently being treated with non-invasive ventilation.
Comparison of characteristics at 15 per hour AHI cut-off
Compared to patients with an AHI <15/h, those with an AHI ≥15/h presented with a lower mean oxygen saturation (difference in medians = 1.3 points, p = 0.003), a higher mean oxygen desaturation (difference in medians = 1.7 points, p < 0.001), as well as a lower mean minimal oxygen saturation (difference in medians = 6.0 points, p < 0.001). The period of time with oxygen saturations below 90 % was higher (difference in medians = 54.6 min, p < 0.001).
Patients with AHI ≥15/h had higher levels of NT-pro BNP (difference in medians = 1,683.5 pg/ml, p = 0.003). No significant differences were found when comparing the cause of heart failure, LVEF, gender, electrical device therapy, permanent atrial fibrillation status, body mass index (BMI), level of daytime sleepiness, or contemporary medical therapy. Further comparisons are displayed in Table 3.
Comparison of patients with an AHI <15/h, OSA and CSA
Irrespective of LVEF, group comparisons revealed that patients with CSA had higher levels of NT-pro BNP compared to patients with an AHI <15/h (difference in medians = 2,710.0 pg/ml, p < 0.001), and compared to patients of the OSA group (difference in medians = 2,639.0 pg/ml, p = 0.016). By contrast, we did not observe any differences in levels of NT-pro BNP in patients with OSA and patients with an AHI <15/h (difference in medians = 71.0 pg/ml, p = 0.921).
Patients with OSA had higher scores of BMI compared to patients with an AHI <15/h (mean difference = 2.8 kg/m2, p = 0.041) and compared to patients with CSA (mean difference = 3.2 kg/m2, p = 0.025). We found significant differences of oxygen parameters in patients with an AHI <15/h compared to patients with an AHI >15/h. However, we did not find any significant differences when comparing these parameters within the OSA and CSA groups (AHI >15/h). Only the mean oxygen saturation was higher in the CSA group compared to the OSA group (difference in medians 0.4 % points, p = 0.045). No significant differences between patients with an AHI <15/h, OSA and CSA existed in cause of heart failure, age, sex distribution, frequency of permanent atrial fibrillation, and cardiac medication. Further characterisation of patients with an AHI ≥15/h subdivided into OSA and CSA and comparisons to patients with an AHI <15/h are summarised in Table 4.
Discussion
This hospital specific study describes results of a relatively simple screening test for OSA and CSA. Our investigation describes a high prevalence of these entities and their relationship to CHF severity as judged by NT-pro BNP in patients with severe CHF on OMT under supervision of the heart failure clinic in our hospital. In addition, these data support the observation that OSA is an independent predictor of cardiovascular disease and CHF [25]. OSA affected 14.8 % of our CHF patients, therefore resulting in a higher prevalence than in the middle-aged healthy population (up to 4 %) [26]. Upper airway narrowing provokes repetitive nocturnal oxygen saturation drops [27]. In regards to hypoxia, we did not find any difference in OSA compared to CSA. However, in contrast to CSA, the respiratory effort against the occluded upper airway generates an augmented thoracic pressure in OSA. This leads to an increase in transmural cardiac pressure gradients and further induces an increase of left ventricular afterload [28]. Furthermore, OSA stimulates sympathetic activity in CHF that triggers surges in blood pressure and heart rate [8, 9, 25]. OSA might initiate and further promote CHF progression, explaining the higher OSA rate in our study population. This raises the important question if OSA triggers CHF and if non invasive ventilation (NIV) therapy delays or even reverses CHF in OSA patients. In contrast, it appears that CSA is a symptom of end-stage heart failure [29]. CSA is initiated by hyperventilation leading to a descent of carbon dioxide below the threshold of respiratory drive causing an apnoea with subsequent oxygenation drops [30]. Following the cascade of CHF, our patients with higher levels of NT-pro BNP experience CSA, compared to patients with less severe CHF and lower levels of NT-pro BNP. Irrespective of LVEF, patients with CSA had higher levels of NT-pro BNP compared to patients with an AHI <15/h (difference in medians = 2,710.0 pg/ml, p < 0.001) and compared to patients of the OSA group (difference in medians = 2,639.0 pg/ml, p = 0.016). CSA is therefore a marker of CHF severity. CSA should alert the physician to intensify heart failure therapy. In addition, we observed that patients with CSA had significantly lower scores of BMI compared to the OSA group, probably being another indicator of the advanced CHF stage.
In summary, our data confirm the common manifestation of SDB among CHF patients as reported in previous studies [1–7]. In our patient population, 50 % with severe CHF presented with an at least moderate form of SDB (AHI ≥15/h). 14.8 % suffered from OSA and 34.6 % presented with CSA.
For several reasons, prior studies remain difficult to interpret resulting in a wide range of prevalences in this patient population. First, there exists no generally accepted AHI threshold for CHF patients. In prior investigations different AHI cut-offs were employed. Given that a AHI suppression to <15/h by NIV therapy compared to control subjects is associated with increased transplant-free survival in severe CHF, this cut-off seems reasonable for us [31]. Schulz et al. [6] investigated an unselected population with depressed LVEF (mean LVEF 28 %) and used an AHI threshold of >10/h. SDB was found in 71 % of his study patients (43 % OSA, 28 % CSA). Using an AHI cut-off of 10/h in our patient population, 106 patients (60.2 %) suffered from SA, indicating that compared to our population, Schulz’s patients had a higher prevalence of SDB.
By contrast, Oldenburg et al. [7] applied an AHI cut-off >5/h and reported SDB in 76 % of the patients (36 % OSA, 40 % CSA). In addition, it should be mentioned that it is unclear whether an unselected CHF population was examined or if polygraphic examinations were performed due to suspicion of SA.
Another finding of our analysis is the lack of significance of ESS score. One reason might be the fact, that fatigue and sleepiness are similar symptoms in heart failure and SDB. Therefore, as in an unselected patient population, ESS score appears not to be valid, and ambulant PR is a reasonable primary screening tool in this high risk patient population.
In addition, our study demonstrated the lack of symptoms in most CHF patients with SA. Only a minority of 15 patients (17.1 %) with an AHI ≥15/h reported excessive daytime sleepiness. This finding is in accordance with the previous data reporting that SA cannot be easily ruled out by a simple questionnaire in CHF patients [32]. Our patients were mainly free of any symptoms, apart from manifestations of the advanced heart disease. Therefore, patients with severe CHF might be adapted to the symptoms, not being able to further distinguish between their advanced stage of heart disease and impairment due to unrefreshable sleep.
Limitations
We investigated a selected population of CHF patients on OMT under supervision of the heart failure clinic of our University Hospital. The reported prevalence of SDB (50 % had an AHI ≥15/h) cannot be applied to heart failure patients in general, as our heart failure clinic supervises mainly severe manifestations of CHF. Another important point is the fact that for diagnosis of SDB, we used PRs without measurements of sleep stages. Thus, our results are not comparable to level 1 in-lab attended polysomnographic results [1–3]. Compared to polysomnography-performed investigations, PR is more easily available and time saving, less expensive, and unattended PR can be performed at the patient’s home. Nevertheless, we did not measure sleep stages. Thus, our AHI measurement is based on a total recording time rather than a total sleeping time. This could lead to an underestimation of the AHI, because the sleeping time might be shorter than the recording time. By contrast, CSA might be overestimated, because in severe CHF, many patients experience CSA even while being awake. Nevertheless, for all studies, the suggested most sensitive and non-invasive equipment was applied [21]. Respiratory inductance plethysmography was used to record the respiratory effort, and nasal airflow and snoring were evaluated by nasal pressure.
Screening CHF patients with ambulatory unattended devices has already been proven to be useful [33]. In most OSA patients, AHI can be accurately classified using Embletta devices. Dingli et al. [34]reported a difference between the results obtained by PSG and polygraphic examination of only 2 ± 5/h. Since PSG is not widely available, PR allowed us to gain data pertaining to a larger and more representative group of stable patients with severe CHF. In general, the increasing demand for the detection of SDB in patients with cardiovascular diseases emphasises the need for alternative tools to identify patients at high risk. PR might be used to rule out OSA and to monitor CSA and heart failure progression in this high risk patient population.
Blood pressure and heart rate are important variables in SDB. Based on the fact, that ACE-inhibitors and beta-blockers are strictly indicated in CHF [35–39], treatment native patients were not present in our cohort. Therefore, no differences were found in our population. More important for the general population of SDB patients, these markers appear not to be relevant if heart failure is present. Unfortunately, Berlin Questionnaire was not performed. For statistical reasons, our data should be interpreted with caution given that no correction for multiple testing was applied. It was not our primary intent to establish risk factors for SDB in this patient population. Our results display the prevalence of SDB in CHF patients on OMT under supervision of the heart failure clinic in our hospital.
Clinical implications
The used screening device counteracts the lack of full in-lab PSG units and the long waiting lists for level 1 in-lab attended examinations. Identifying CHF patients with relevant SDB may have important clinical implications. First, patients with SDB have a worse prognosis [31, 40, 41]. Second, up-titration of medical heart failure therapy obviously has a certain beneficial effect on the prevalence of CSA. It has been established that beta blockade suppresses dose-dependently CSA in CHF [18, 19]. Moreover, renin angiotensin aldosterone system blockade lowers intracardiac filling pressures, which additionally influence CSA [42]. Therefore, CSA could be used to monitor CHF worsening and be decisive to optimise heart failure therapy. Third, a generally accepted AHI cut-off for diagnosis of SDB in CHF patients is required. Fourth, NIV therapy is a promising approach in the treatment of SDB [43]. But it must be kept in mind that there exist explicit distinctions of SA in CHF. While OSA is an independent trigger of cardiovascular disease and CHF, CSA displays a symptom of the failing myocardium. NIV therapy has been proven to sufficiently reduce the AHI and repetitive oxygen saturation drops [44]. Nevertheless, results of large randomised trials are still needed to value the impact of NIV in CHF patients with OSA and CSA.
Conclusions
Using a relative simple screening test for OSA and CSA, we demonstrated a high prevalence of 50.0 % of at least moderate to severe SDB in patients with severe stable CHF being under supervision of our heart failure clinic. ESS score was not a suitable screening method. In our heart failure population, OSA is prevalent in earlier stages of heart failure, whereas CSA appears to be a manifestation of end-stage heart failure, as mirrored in the significant difference in NT-pro BNP levels.
References
Vazir A, Hastings PC, Dayer M, McIntyre HF, Henein MY, Poole-Wilson PA, Cowie MR, Morrell MJ, Simonds AK (2007) A high prevalence of sleep disordered breathing in men with mild symptomatic chronic heart failure due to left ventricular systolic dysfunction. Eur J Heart Fail 9(3):243–250. doi:10.1016/j.ejheart.2006.08.001
Javaheri S (2006) Sleep disorders in systolic heart failure: a prospective study of 100 male patients. The final report. Int J Cardiol 106(1):21–28. doi:10.1016/j.ijcard.2004.12.068
Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD (1999) Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med 160(4):1101–1106
Lanfranchi PA, Somers VK, Braghiroli A, Corra U, Eleuteri E, Giannuzzi P (2003) Central sleep apnea in left ventricular dysfunction: prevalence and implications for arrhythmic risk. Circulation 107(5):727–732
Javaheri S (2005) Central sleep apnea in congestive heart failure: prevalence, mechanisms, impact, and therapeutic options. Semin Respir Crit Care Med 26(1):44–55. doi:10.1055/s-2005-864206
Schulz R, Blau A, Borgel J, Duchna HW, Fietze I, Koper I, Prenzel R, Schadlich S, Schmitt J, Tasci S, Andreas S (2007) Sleep apnoea in heart failure. Eur Respir J 29(6):1201–1205. doi:10.1183/09031936.00037106
Oldenburg O, Lamp B, Faber L, Teschler H, Horstkotte D, Topfer V (2007) Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 9(3):251–257. doi:10.1016/j.ejheart.2006.08.003
Bradley TD, Tkacova R, Hall MJ, Ando S, Floras JS (2003) Augmented sympathetic neural response to simulated obstructive apnoea in human heart failure. Clin Sci (Lond) 104(3):231–238. doi:10.1042/CS20020157
Spaak J, Egri ZJ, Kubo T, Yu E, Ando S, Kaneko Y, Usui K, Bradley TD, Floras JS (2005) Muscle sympathetic nerve activity during wakefulness in heart failure patients with and without sleep apnea. Hypertension 46(6):1327–1332. doi:10.1161/01.HYP.0000193497.45200.66
Usui K, Bradley TD, Spaak J, Ryan CM, Kubo T, Kaneko Y, Floras JS (2005) Inhibition of awake sympathetic nerve activity of heart failure patients with obstructive sleep apnea by nocturnal continuous positive airway pressure. J Am Coll Cardiol 45(12):2008–2011. doi:10.1016/j.jacc.2004.12.080
Gami AS, Howard DE, Olson EJ, Somers VK (2005) Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med 352(12):1206–1214. doi:10.1056/NEJMoa041832
Mehra R, Stone KL, Varosy PD, Hoffman AR, Marcus GM, Blackwell T, Ibrahim OA, Salem R, Redline S (2009) Nocturnal arrhythmias across a spectrum of obstructive and central sleep-disordered breathing in older men: outcomes of sleep disorders in older men (MrOS sleep) study. Arch Intern Med 169(12):1147–1155. doi:10.1001/archinternmed.2009.138
Bradley TD, Hall MJ, Ando S, Floras JS (2001) Hemodynamic effects of simulated obstructive apneas in humans with and without heart failure. Chest 119(6):1827–1835
Tkacova R, Rankin F, Fitzgerald FS, Floras JS, Bradley TD (1998) Effects of continuous positive airway pressure on obstructive sleep apnea and left ventricular afterload in patients with heart failure. Circulation 98(21):2269–2275
Javaheri S, Corbett WS (1998) Association of low PaCO2 with central sleep apnea and ventricular arrhythmias in ambulatory patients with stable heart failure. Ann Intern Med 128(3):204–207
Arzt M, Young T, Finn L, Skatrud JB, Ryan CM, Newton GE, Mak S, Parker JD, Floras JS, Bradley TD (2006) Sleepiness and sleep in patients with both systolic heart failure and obstructive sleep apnea. Arch Intern Med 166(16):1716–1722. doi:10.1001/archinte.166.16.1716
Jilek C, Krenn M, Sebah D, Obermeier R, Braune A, Kehl V, Schroll S, Montalvan S, Riegger GA, Pfeifer M, Arzt M (2011) Prognostic impact of sleep disordered breathing and its treatment in heart failure: an observational study. Eur J Heart Fail 13(1):68–75. doi:10.1093/eurjhf/hfq183
Kohnlein T, Welte T (2007) Does beta-blocker treatment influence central sleep apnoea? Respir Med 101(4):850–853. doi:10.1016/j.rmed.2006.11.023
Tamura A, Kawano Y, Naono S, Kotoku M, Kadota J (2007) Relationship between beta-blocker treatment and the severity of central sleep apnea in chronic heart failure. Chest 131(1):130–135. doi:10.1378/chest.06-0919
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Sanchez MA, Jaarsma T, Kober L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Ronnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Bonet LA, Avraamides P, Ben Lamin HA, Brignole M, Coca A, Cowburn P, Dargie H, Elliott P, Flachskampf FA, Guida GF, Hardman S, Iung B, Merkely B, Mueller C, Nanas JN, Nielsen OW, Orn S, Parissis JT, Ponikowski P (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. doi:10.1093/eurheartj/ehs104
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force (1999). Sleep 22(5):667–689
Meoli AL, Casey KR, Clark RW, Coleman JA Jr, Fayle RW, Troell RJ, Iber C (2001) Hypopnea in sleep-disordered breathing in adults. Sleep 24(4):469–470
Ryan CM, Usui K, Floras JS, Bradley TD (2005) Effect of continuous positive airway pressure on ventricular ectopy in heart failure patients with obstructive sleep apnoea. Thorax 60(9):781–785. doi:10.1136/thx.2005.040972
Johns MW (1992) Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15(4):376–381
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342(19):1378–1384. doi:10.1056/NEJM200005113421901
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235. doi:10.1056/NEJM199304293281704
Bradley TD, Floras JS (2003) Sleep apnea and heart failure: part I: obstructive sleep apnea. Circulation 107(12):1671–1678. doi:10.1161/01.CIR.0000061757.12581.15
Buda AJ, Pinsky MR, Ingels NB Jr, Daughters GT 2nd, Stinson EB, Alderman EL (1979) Effect of intrathoracic pressure on left ventricular performance. N Engl J Med 301(9):453–459. doi:10.1056/NEJM197908303010901
Mansfield DR, Solin P, Roebuck T, Bergin P, Kaye DM, Naughton MT (2003) The effect of successful heart transplant treatment of heart failure on central sleep apnea. Chest 124(5):1675–1681
Bradley TD, Floras JS (2003) Sleep apnea and heart failure: part II: central sleep apnea. Circulation 107(13):1822–1826. doi:10.1161/01.CIR.0000061758.05044.64
Arzt M, Floras JS, Logan AG, Kimoff RJ, Series F, Morrison D, Ferguson K, Belenkie I, Pfeifer M, Fleetham J, Hanly P, Smilovitch M, Ryan C, Tomlinson G, Bradley TD (2007) Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure Trial (CANPAP). Circulation 115(25):3173–3180. doi:10.1161/CIRCULATIONAHA.106.683482
Ferrier K, Campbell A, Yee B, Richards M, O‘Meeghan T, Weatherall M, Neill A (2005) Sleep-disordered breathing occurs frequently in stable outpatients with congestive heart failure. Chest 128(4):2116–2122. doi:10.1378/chest.128.4.2116
Quintana-Gallego E, Villa-Gil M, Carmona-Bernal C, Botebol-Benhamou G, Martinez–Martinez A, Sanchez-Armengol A, Polo-Padillo J, Capote F (2004) Home respiratory polygraphy for diagnosis of sleep-disordered breathing in heart failure. Eur Respir J 24(3):443–448. doi:10.1183/09031936.04.00140603
Dingli K, Coleman EL, Vennelle M, Finch SP, Wraith PK, Mackay TW, Douglas NJ (2003) Evaluation of a portable device for diagnosing the sleep apnoea/hypopnoea syndrome. Eur Respir J 21(2):253–259
Bohm M, Borer J, Ford I, Gonzalez-Juanatey JR, Komajda M, Lopez-Sendon J, Reil JC, Swedberg K, Tavazzi L (2013) Heart rate at baseline influences the effect of ivabradine on cardiovascular outcomes in chronic heart failure: analysis from the SHIFT study. Clin Res Cardiol 102(1):11–22. doi:10.1007/s00392-012-0467-8
Fujita B, Franz M, Goebel B, Fritzenwanger M, Figulla HR, Kuethe F, Ferrari M, Jung C (2012) Prognostic relevance of heart rate at rest for survival and the quality of life in patients with dilated cardiomyopathy. Clin Res Cardiol 101(9):701–707. doi:10.1007/s00392-012-0447-z
Zugck C, Franke J, Gelbrich G, Frankenstein L, Scheffold T, Pankuweit S, Duengen HD, Regitz-Zagrosek V, Pieske B, Neumann T, Rauchhaus M, Angermann CE, Katus HA, Ertl GE, Stork S (2012) Implementation of pharmacotherapy guidelines in heart failure: experience from the German Competence Network Heart Failure. Clin Res Cardiol 101(4):263–272. doi:10.1007/s00392-011-0388-y
Hoke RS, Muller-Werdan U, Lautenschlager C, Werdan K, Ebelt H (2012) Heart rate as an independent risk factor in patients with multiple organ dysfunction: a prospective, observational study. Clin Res Cardiol 101(2):139–147. doi:10.1007/s00392-011-0375-3
Reil JC, Custodis F, Swedberg K, Komajda M, Borer JS, Ford I, Tavazzi L, Laufs U, Bohm M (2011) Heart rate reduction in cardiovascular disease and therapy. Clin Res Cardiol 100(1):11–19. doi:10.1007/s00392-010-0207-x
Wang H, Parker JD, Newton GE, Floras JS, Mak S, Chiu KL, Ruttanaumpawan P, Tomlinson G, Bradley TD (2007) Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol 49(15):1625–1631. doi:10.1016/j.jacc.2006.12.046
Javaheri S, Shukla R, Zeigler H, Wexler L (2007) Central sleep apnea, right ventricular dysfunction, and low diastolic blood pressure are predictors of mortality in systolic heart failure. J Am Coll Cardiol 49(20):2028–2034. doi:10.1016/j.jacc.2007.01.084
Walsh JT, Andrews R, Starling R, Cowley AJ, Johnston ID, Kinnear WJ (1995) Effects of captopril and oxygen on sleep apnoea in patients with mild to moderate congestive cardiac failure. Br Heart J 73(3):237–241
Oldenburg O, Bitter T, Lehmann R, Korte S, Dimitriadis Z, Faber L, Schmidt A, Westerheide N, Horstkotte D (2011) Adaptive servoventilation improves cardiac function and respiratory stability. Clin Res Cardiol 100(2):107–115. doi:10.1007/s00392-010-0216-9
Arzt M, Wensel R, Montalvan S, Schichtl T, Schroll S, Budweiser S, Blumberg FC, Riegger GA, Pfeifer M (2008) Effects of dynamic bilevel positive airway pressure support on central sleep apnea in men with heart failure. Chest 134(1):61–66. doi:10.1378/chest.07-1620
Acknowledgments
An Embletta® recording device and technical support was kindly provided by Vivisol Austria. We would like to thank Mrs Monika Knoetig, biomedical scientist, for assistance in polygraphic related patient care.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dolliner, P., Brammen, L., Graf, S. et al. Portable recording for detecting sleep disorder breathing in patients under the care of a heart failure clinic. Clin Res Cardiol 102, 535–542 (2013). https://doi.org/10.1007/s00392-013-0563-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-013-0563-4