Abstract
Purpose
In colon cancer (CC), nodal involvement is the main prognostic factor following potentially curative (R0) resection. The purpose of this study was to examine data from the literature to provide an up-to-date analysis of the management of nodal disease with special reference to laparoscopic treatment.
Methods
MEDLINE and EMBASE databases were searched for potentially eligible studies published in English up to July 15, 2014.
Results
In CC, nodal involvement is a frequent event and represents the main risk of cancer recurrence. Node negative patients recur in 10–30 % of cases most likely due to underdiagnosed or undertreated nodal disease. Extended colonic resections (complete mesocolic excision with central vascular ligation; D3 lymphadenectomy) provides a survival benefit and better local control. Sentinel lymph node mapping in addition to standard surgical resection represents an option for improving staging of clinical node negative patients. Both extended resection and sentinel lymph node mapping are feasible in a laparoscopic setting.
Conclusions
Both extended colonic resection and sentinel lymph node mapping should play a role in the laparoscopic treatment of CC with the purpose of improving control and staging of nodal disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC), with 1.2 million cases and 600,000 deaths reported annually, is one of the most common cancers worldwide. According to recent estimates, CRC is the most common cancer and the second most common cause of cancer-related death in Europe [1].
Surgical resection is the mainstay therapy, with a laparoscopic approach rapidly becoming the treatment methodology of choice for colon cancer (CC) [2, 3]. Laparoscopic colonic resection has comparable oncological outcomes and better perioperative results compared with open surgery, especially in Enhanced Recovery After Surgery (ERAS) program settings [4–6].
After potentially curative surgery for CC, nodal involvement is the major determinant of prognosis and represents the main indicator for adjuvant chemotherapy [7–11]. Nonetheless, disease recurrence or progression develops in about 10–30 % of node-negative patients, most likely because of undetected or undertreated occult nodal disease [12–15].
Accordingly, several strategies have been proposed to improve staging and to control nodal disease. Some authors have proposed extended surgical resection (i.e., complete mesocolic excision [CME] with central vascular ligation [CVL]; D3 lymphadenectomy) [16–18], while others prefer adopting innovative strategies allowing for organ and function sparing surgery (i.e., sentinel lymph node mapping [SLNM]) [19–21].
In this review, data from the literature on lymph node involvement were analyzed focusing both on the clinical impact and technical issues with the intention of proposing patient- and tumor-tailored lymphadenectomy with minimally invasive surgery.
Adopted criteria for lymph node staging
The AJCC/UICC staging system
In non-metastatic CC, lymph node involvement is the main prognostic factor. More specifically, the number of positive nodes has been accepted as the most valuable, reproducible, and easy to use predictor of disease recurrence and prognosis [22, 23].
The actual American Joint Committee on Cancer/Union for International Cancer Control (AJCC/UICC) staging system considers pN category according to the absolute number of involved regional nodes. Regional nodes are determined according to the location of the tumor and includes nodes located adjacent to the colon, along the vascular arcades of the marginal artery, and along the course of the major vessels supplying the colon. Specifically, the regional lymph nodes are the pericolic and those found along the ileocolic, right colic, middle colic, left colic, inferior mesenteric, and superior rectal arteries [24].
Though the seventh Edition of the AJCC/UICC staging system includes substantial changes from previous editions, which are particularly complex for stage II and III disease, controversy still exists with respect to its ability to address all survival discrepancies observed in CC [25–27].
The JSCCR staging system
The Japanese Society for Cancer of the Colon and Rectum (JSCCR) staging system considers the pN categories according to the number and site of nodal involvement. Regional lymph nodes consist of three groups: pericolic, intermediate, and main lymph nodes. The extent of regional lymph nodes varies according to the anatomical location of the primary tumor in relation to its feeding arteries. Pericolic nodes are lymph nodes along the marginal artery; intermediate nodes are lymph nodes along colic arteries (ileocolic, right colic, right middle colic, left middle colic, left colic, and sigmoid arteries). Main nodes are lymph nodes at the origin of each colic artery for those tumors located in the superior mesenteric artery territory or proximal to the origin of the left colic artery for those tumors located in the inferior mesenteric artery territory. When present, lymph node metastases are classified as follows: N1, metastasis into one to three pericolic or intermediate lymph nodes; N2, metastasis in four or more pericolic or intermediate lymph nodes; and N3, metastasis in main lymph nodes.
Accordingly, the extent of lymphadenectomy is defined as D1 when lymph node dissection is limited to pericolic nodes; D2 when lymph node dissection entails complete dissection of pericolic and intermediate nodes, and D3 when lymph node dissection is extended to all regional nodes. Hence, D3 lymphadenectomy entails the removal of lymph nodes along the superior mesenteric artery in right-sided CC and removal of lymph nodes proximal to the inferior mesenteric artery in left-sided CC (Fig. 1) [28].
Lymph node classification according to the Japanese Society for Cancer of the Colon and Rectum (JSCCR). Level 1 lymph node stations are represented in red, level 2 lymph node stations in blue, and level 3 lymph node stations in yellow. (Modified from: Japanese Society for Cancer of the Colon and Rectum (JSCCR). Japanese Classification of Colorectal Carcinoma, 2nd English Edition, Kanehara & Co., Ltd., Tokyo 2010) [28]
Importance of number of analyzed nodes
The evaluation of at least 12 nodes is recommended by the AJCC/UICC staging system, and this suggestion is accepted by the great majority of authors. Nonetheless, population-based as well as many multicenter studies report that less than 50 % of patients with CC receive adequate lymph node evaluation [13–15, 29–31]. In this setting, adjuvant chemotherapy is proposed to pN0 patients with less than 12 analyzed nodes because of high recurrence rates demonstrated in previous studies [32–34].
Besides stage migration (Will Rogers phenomenon), a positive association between the number of analyzed nodes and long-term outcome in stage II and III CC has been reported in several reports [35–37].
Gleisner et al., using Surveillance, Epidemiology, and End Results (SEER) data from 1998 to 2007 with 154,208 patients, demonstrated that the total number of nodes examined was associated with long-term outcome. More specifically, total nodal count was associated with a non-linear decrease in the risk of death. Among node-negative patients, the risk of death decreased considerably for each negative node up to 20–25 lymph nodes examined. Among node-positive patients, the risk of death increased with the number of positive nodes independent of the number of nodes analyzed. However, when the number of analyzed nodes was less than 10–15, the risk of death was higher than predicted by the independent effect of total nodal count or number of positive nodes [38].
Budde et al. recently confirmed the association between higher lymph node counts and better survival using data from the 2004 to 2010 SEER database on 147,076 patients [39].
Pathologic assessment of nodal disease
Lymph node search via manual dissection of fatty tissue and hematoxylin and eosin (HE)-stained histological examination of the largest cut surface remain the standard approach in pathological lymph node evaluation. However, some nodes remain undetected and only a small portion of analyzed nodes is assessed, leaving most parts of the identified nodes unexamined. This undoubtedly leads to understaging of the disease, and it partially explains the 10–30 % recurrence rate observed in stage I and II CCs [40].
Adopting additional sections and immunohistochemistry (IHC) may improve the identification of positive lymph nodes. Of note, many patients who are initially staged as lymph node-negative and experience disease recurrence have isolated tumor cells (ITCs) or micrometastases (MMs) after advanced evaluation [41, 42]. Similarly, molecular analysis of lymph node tissue has been introduced as an additional tool in the work-up of cancer patients. This technique allows identification of minimal disease in lymph nodes by examining the entire node, thereby overcoming the problem of sampling bias. Importantly, the molecular detection of tumor cells in regional lymph nodes has been associated with disease recurrence and poor survival in node-negative patients [43]. Nonetheless, some drawbacks exist in adopting these techniques in actual clinical practice. For instance, analysis of multiple HE- and IHC-stained sections is expensive and time-consuming, and it is difficult to adopt for every retrieved lymph node. Moreover, molecular analysis has not yet been standardized; it is expensive, and some false-positive results have been described [44]. Furthermore, although positive lymph nodes are usually those nearest to the primary tumor, analysis of unselected nodes can lead to false-negative results [45].
Micrometastases and isolated tumor cells
The AJCC/UICC staging system recommends evaluating the presence of MMs or ITCs in CC specimens, although these categories have not yet been included in the actual TNM classification. ITCs are defined as the presence of a single or small number of tumor cells equal of less than 0.2 mm in diameter, while MMs are described as the presence of deposits equal to or less than 2.0 mm, but greater than 0.2 mm in diameter. MMs and ITCs, whether detected by standard histologic techniques or IHC, are coded as pN0 (i+), and a tumor that is detected only by special molecular techniques such as reverse transcriptase polymerase chain reaction (RT-PCR) is coded as pN0 (mol+) [24]. The AJCC/UICC recommendations do not explicitly indicate the method to use to detect occult disease. For this reason, some authors have strictly adopted HE and IHC while molecular analysis is employed by others [43, 44, 46].
The presence of occult malignant cells, either in the form of ITCs or MMs, has been demonstrated in 25–58 % of node-negative CRC patients depending on their characteristics and method of detection used [42, 43, 46–48]. Although the prognostic value of these methods or techniques has not yet been completely clarified, occult disease remains of great interest, since it may represent a possible indication for adjuvant chemotherapy in the near future.
Nodal tumor deposits
The actual AJCC/UICC staging system uses the term “satellite tumor deposits” to designate discrete rounded nodules of tumor cells of any size within the pericolic fat or in adjacent mesentery. They are considered the equivalent of nodal metastases, even if they lack residual nodal architecture, and staged as N1c disease in the absence of other nodal metastases. Each should be counted separately for the involved lymph node count that determines pN status.
The presence of tumor deposits is a strong adverse prognostic feature [25, 49]. The prognostic impact was addressed in a recent study by Ueno et al. in which they analyzed the optimal categorization of nodal tumor deposits and reported presence in 17 % of 3,958 colorectal cancer patients. The recommendation of the AJCC/UICC for considering nodal tumor deposits as nodal metastases irrespective of contours was therefore confirmed [50].
Lymph node involvement
Roughly 60 % of CCs show nodal involvement upon histopathological examination [51]. However, the great majority of studies do not show an increase in nodal positive count in relation to the number of analyzed nodes, unless a very small number of nodes are analyzed [36]. Nonetheless, nodal count is clearly associated with survival advantages [37–39]. Furthermore, when considering the relationship between lymph node count and positivity, many confounding factors may affect the results [36, 52].
In Western countries, since it is not strictly required in a clinical setting, the location of nodal metastases is usually not recorded, and this may represent a major limitation for deep knowledge of the disease. Understanding lymphatic drainage of the colon is challenging because of its variety and complexity; however, it is generally accepted that the lymphatic tracts tend to accompany supplying arteries of the colon. Because of the diversity of blood supply, particularly in the right and transverse colon, it is difficult to detect clear margins of lymphatic drainage for each colon segment. A clear and precise classification of lymph node areas according to the location of the tumor may therefore generate very useful information.
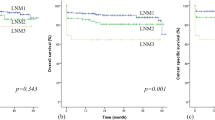
Figure 2 shows data on the level of lymph node involvement according to the JSCCR classification for right, transverse, left, and sigmoid colon.
a Level of lymph node involvement for node positive patients according to the JSCCR classification for right colon, transverse colon, left colon, and sigmoid colon [53–58]. b Level of lymph node involvement for node positive patients according to the JSCCR classification for right colon segments [53, 55]
Complete mesocolic excision with central vascular ligation
After total mesorectal excision (TME) was introduced, local recurrence rate as well as prognosis improved significantly in rectal cancer [59, 60]. In fact, the observation that a better prognosis for rectal cancer compared with CC was observed in some countries after adopting TME leads Hohenberger et al. to hypothesize that CC surgery may be improved by implementing the concept of surgical dissection along embryological planes. With this concept, the integrity of the embryological envelope around the mesocolon is maintained, allowing maximal lymph node retrieval and minimizing the possibility of cancer cell seeding. This represents the idea of CME. The accompanying concept of CME in Hohenberger et al.’s idea was CVL, obtained through the division of supplying arteries at their real origin after completing colonic mobilization and dissection along the main vessels [16].
For cecum and ascending CC, division of ileocolic and right vessels is obtained at the origin with the superior mesenteric artery and vein, while division of middle colic vessels is obtained at the origin of the right branches. For transverse CC, including right and left flexures, division of the middle colic vessels is obtained through central ligation of the middle colic artery and vein considering possible anatomical variations. Additionally, central division of the right gastroepiploic artery and vein may be accomplished using this approach. For cancer of the right flexure, division of the colon is performed in proximity to the left flexure. For cancer of the transverse colon and left flexure, the descending colon is also sacrificed. For cancer of the proximal descending colon, the root of the superior mesenteric artery is usually preserved, and division of the left colic artery is obtained at its origin. For cancer of the middle descending colon down to the sigmoid colon, the root of the inferior mesenteric artery and the inferior mesenteric vein below the pancreas are divided. The proximal colonic division is performed between the distal transverse colon and the distal descending colon depending on the site of the tumor [16].
West et al. demonstrated that CME with CVL specimens are characterized by more tissue compared with standard surgery in terms of distance between the tumor and vascular tie, length of bowel removed (both colon and terminal ileum), and area of mesentery. Importantly, CME with CVL allows more mesocolic plane resections (92 vs. 40 %) and a greater number of nodes analyzed (30 vs. 18). According to West et al.’s hypothesis, these differences may explain the 15 % survival advantage observed at 5 years as reported in a previous study on the completeness of mesocolon resection [61, 62].
Recently, West et al. demonstrated that Japanese D3 resection and CME with CVL are comparable in terms of quality of mesocolic plane resection and distance between main ties and tumor area. In Japanese experience, according to JSCCR guidelines, the extent of longitudinal resection was significantly shorter; hence, total nodal count and mesentery area were less represented [63]. Differences in the extent of colonic and lymph node resection between D3 lymphadenectomy according to JSCCR guidelines and CME with CVL according to Hohenberger et al.’s idea are exemplified in Fig. 3. JSCCR guidelines suggests D3 lymphadenectomy for clinical T3 and T4 tumors or clinical evidence of lymph node metastasis [16], while Hohenberger et al. offer CME with CVL even in early tumors [17].
Several experiences from Eastern countries have demonstrated the feasibility and safety of laparoscopic extended colonic resections (either CME or D3 lymphadenectomy) for CC. Table 1 reports short- and long-term results of the main studies. While in countries from the Far East, such as Japan or Korea, the concept of preservation of the mesocolic plane and lymph node clearing are strictly respected, many surgeons in the United States and Europe argue there are not enough data for this procedure to be performed [68].
In the original study by Hohenberger et al. on 1,438 patients submitted to CME with CVL for CC, the mean number of retrieved nodes was 32. A prognostic cut-off value for the number of analyzed nodes was computed according to the “Le Blanc” method, and a value of 28 was demonstrated both in node-negative (682) and node-positive (383) patients. The survival benefit when more than 28 nodes were analyzed was 5.6 % for node-negative patients (96.3 vs. 90.7 %) and 7.1 % for node-positive patients (71.7 vs. 64.6 %) [16].
In accordance with these results, Kotake et al. recently demonstrated an 18 % advantage in 5-year survival rate in patients with pT3 and pT4 CC after D3 compared with D2 lymphadenectomy. The mean number of nodes analyzed was 15 and 23 after D2 and D3 lymphadenectomy, respectively [69].
Sentinel lymph node mapping
The first lymph node or group of nodes along the route of lymphatic drainage of a primary tumor is known as the sentinel lymph node (SLN). Since the concept of SLN mapping (SLNM) was demonstrated in a clinical study involving patients with malignant melanoma, the clinical impact of SLNM has become a major topic with regard to various solid tumors.
While SLNM is widely adopted in melanoma and breast cancer and prevents unnecessary lymphadenectomies, its application for gastrointestinal malignancies meets resistance because of the multidirectional lymphatic flow and the possibility of skip metastases that characterize the gastrointestinal tract [57, 70].
However, although some authors recommend adopting SLNM to minimize the extent of resection in early-stage CC [71, 72], it is actually proposed with the aim of improving nodal staging in the setting of a standard lymph node dissection by carefully evaluating a restricted number of lymph nodes. Therefore, SLNM has to be considered as a technique for potentially improving CC staging without defined prognostic impact and therapeutic implication [73, 74].
Unfortunately, SLNM has not yet been standardized, and many differences exist regarding indications, methods, and materials, making inter-study comparisons very difficult and delaying its application in normal clinical practice. Additionally, the results seem to be very much influenced by the experience of the operating surgeon with a learning curve that has been described to be as high as 20–30 cases [75–77].
Techniques for sentinel lymph node mapping
In vivo SLNM consists of the detection of SLNs before colonic resection by using peritumoral injection of dye agents or radiotracers (i.e., 99mTc). SLNs are identified by directly visualizing colored nodes or intraoperative lymphoscintigraphy.
Blue-dye SLNM is the most used method; blue-dye agents are injected subserosally at the time of surgery or submucosally via intraoperative or preoperative colonoscopy, with injected volumes varying from 0.5 to 5.0 mL. Several blue-dye agents have been used, without any differences between them (i.e., methylene blue, patent blue, sulfan, and isosulfan blue). Regarding dye agents, some limitations have been described, such as injections should be performed prior to colonic mobilization, observation of coloration has to be done in real-time, and visualization of stained nodes is difficult in obese patients, right-sided CC, and small tumors, particularly during laparoscopic surgery [72, 78].
Radiotracer-guided SLNM has been applied to improve the accuracy of SLN detection. Radiotracer 99mTc-injection is usually performed submucosally using preoperative colonoscopy, and intraoperative localization of hot nodes is then performed using a gamma probe. The radio-colloid method has shown comparable results in terms of detection rate and sensitivity with several practical limitations, such as the requirement of radiation safety regulations and specific equipment not always being available in community hospitals together with the need for an adjunctive colonoscopy. Furthermore, current available rigid-type laparoscopic gamma probes are fixed by the trocar, thus the freedom to search for sentinel nodes and to avoid the “shine through” effect from the injection site is seriously restricted [79–81].
Ex vivo SLNM was first described by Wong et al. [82] and consisted of the detection of SLNs by blue-dye injection in fresh specimens early after resection. Wong et al. described the use of 0.25 mL isosulfan blue injected submucosally using a tuberculin syringe into four quadrants around the tumor after incision of the antimesenterial border of the colon [82]. Moreover, subserosal injection of other dye agents (i.e., methylene blue, patent blue, and sulfan blue) have been used with comparable results [73, 74].
No differences in detection rates or sensitivity have been described between in vivo and ex vivo techniques (Table 2), though some authors report a higher detection rate after adding ex vivo techniques in SLN-negative cases [72, 74].
In vivo techniques have the potential advantage of evaluating aberrant lymphatic drainage, which has been described to occur in 4–29 % of patients [20, 74, 90, 91]. Recently, Saha et al. performed a prospective study focused on detecting aberrant lymphatic drainage and its impact on the extent of surgery. Of 192 patients, 44 (22 %) underwent extended resection caused by aberrant lymphatic drainage, and in 19 of these cases (10 %), one or more positive SLNs were found outside the standard resection field. Moreover, SLNs were the only site of nodal metastasis in two patients [20].
The ex vivo technique has the advantage of being completely safe for the patient eliminating the low but present risk of allergic reactions that have been described in 0.5–2.5 % with patent blue and 0.9–1.9 % with isosulfan blue. No allergic reactions have thus far been described with methylene blue [92–94].
Indocyanine green (ICG) is a near-infrared (NIR) fluorophore that has shown promising results in SLNM in gastrointestinal as well as non-gastrointestinal neoplasias (i.e., lung, bladder, uterus, breast, etc.). ICG may represent an ideal tracer because of the lack of endogenous NIR tissue fluorescence and because it does not alter the normal surgical field as it is invisible to the human eye. However, special imaging systems are required to visualize NIR fluorescent light [95]. However, several NIR imaging systems for open and laparoscopic surgery are presently available. Nagata et al. first described ICG application in laparoscopic SLNM of colorectal cancer in 2006 [87]. The main advantages of ICG compared with the blue-dye and radiotracer methods relate to the real time and better visualization of lymphatic vessels and SLNs embedded deep inside tissues without the risk of radioactivity. The advantage of deep penetration in fatty tissue of NIR fluorescent light is particularly beneficial in obese patients [96].
Histopathological examination of sentinel lymph nodes (HE, IHC, PCR)
Upstaging in CC is the most inviting idea in the SLNM concept. About 10–30 % of node-negative patients develop disease progression or recurrence, most likely due to the presence of occult tumor cells [7–10]. In-depth analysis through serial sectioning, IHC, and RT-PCR has demonstrated 5.7–46.5 % upstaging of pN0 CCs with SLNM may facilitate pathologic examination, making this technique more applicable, since in-depth analysis is focused on one to a few nodes [21, 75, 83, 86, 89]. Many studies have confirmed the validity of SLNM in this setting with meta-analyses showing a mean upstaging of 15 and 19 % [73, 74].
Braat et al. recently reported very high survival rates for node-negative CC patients with negative SLNs with a 5-year disease-free survival rate approaching 95 %. These results seem to confirm the use of SLNM in discriminating patients with very good prognoses [97].
Sentinel lymph node mapping in open surgery
Two systematic reviews and meta-analyses by van der Pas et al. in 2011 [73] and van der Zaag et al. in 2012 [74] evaluated SLNM in colorectal cancer. The two papers included almost exclusive studies from open surgery using blue-dye and radiotracer or the combination of both methods; substantial result homogeneity was demonstrated among different techniques. The pooled detection rate for colorectal cancer was 94 and 91 %, while overall sensitivity was 76 and 86 %, respectively [73, 74]. van der Zaag et al. showed significantly higher sensitivities for T1 and T2 compared with T3 and T4 colorectal cancers (93 vs. 59 %) [74]. Conversely, stratification by stage limited to CC showed no significant difference in sensitivity among T1, T2, T3, and T4 tumors in the meta-analysis by van der Pas et al. [73]. Interestingly, van der Pas et al. selected eight studies with high-quality SLN procedures that had a detection rate and sensitivity for CC of 96 and 90 %, respectively [73].
Both studies concluded that SLNM should be considered as an additional procedure to be performed in addition to standard resection with the purpose of improving staging of clinical node negative patients [73, 74].
Laparoscopic sentinel lymph node mapping
There is great interest in laparoscopic SLNM as it is becoming the preferred approach for CC treatment. In 2002, Tsioulias et al. first reported the adoption of SLNM in laparoscopically assisted colectomy for CC. In 2003, Bilchik et al. reported using the same protocol with increased numbers (30 cases) of laparoscopic SLNM using isosulfan blue injected submucosally through intraoperative colonoscopy (27 cases) or subserosally using a spinal needle (three cases); their detection rate was 100 %, sensitivity 75 %, and upstaging 14 %, and aberrant lymphatic drainage was described in 29 % of the cases [91].
In two distinct Italian experiences, Bianchi et al. reported laparoscopic SLNM using patent blue or radiotracer [72, 98]. In the more recent study, 75 patients affected by stage I and II CC were enrolled. Blue-dye was the used method with injection performed subserosally at the time of surgery. The detection rate was 93 %, while the false-negative rate was in 22 %. Eight more patients underwent SLNM guided by radiotracer 99mTc that was injected submucosally through colonoscopy the day before surgery. With this approach, the detection rate was reported to be 100 %, and no false-negatives were reported [72].
In 2006, Nagata et al. reported on the use of ICG and NIR laparoscopic light for SLNM of CC and cancer of the upper rectum. A detection rate of 98 % was reported together with the absence of false negative cases in T1 and T2 patients. The false-negative rate for T3 tumors was 32 % [87].
Hirche et al. published the results on 26 CC patients who underwent open (15 cases) and laparoscopic assisted (11 cases) colonic resection with in vivo SLNM using NIR navigation and ICG. The detection rate, sensitivity, and upstaging were 96, 82, and 33 %, respectively [88]. In laparoscopic-assisted resections, ICG injection was accomplished intraoperatively after mini-laparotomy.
Most recently, van der Pas et al. reported 14 patients with CC treated by laparoscopy with intraoperative subserosal injection of ICG/albumin solution obtained using a spinal needle or an endoscopic flexible needle (Wang needle). The lymphatic flow and SLNs were identified using a NIR laparoscopic system, and the detection rate was reported to be 100 %. All the SLNs were negative by histopathological examination, but four cases had metastasis in non-sentinel nodes. It is possible that these results were due to the high percentage of T3 tumors (71 %) included in this cohort [96].
Conclusions
In CC, lymph node involvement is a frequent event, and it represents the main predictor of long-term survival and recurrence. As many as one in every four node-negative patients experience recurrence after potentially curative resection because of underdiagnosed and/or undertreated nodal disease. Extended colonic resections (i.e., CME with CVL and D3 lymphadenectomy) seem to offer a survival benefit and better local control. SLNM, in addition to standard surgical resection, may represent an option for improving staging in clinical node-negative patients. Both extended resections and SLNM are feasible in a laparoscopic setting.
References
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C et al (2013) GLOBOCAN 2012 v1.0, Cancer incidence and mortality worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer. Available from: http://globocan.iarc.fr. Accessed 15 July 2014
Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J (2008) Long-term outcome of laparoscopic surgery for colorectal cancer: a Cochrane systematic review of randomised controlled trials. Cancer Treat Rev 34:498–504
Di B, Li Y, Wei K, Xiao X, Shi J, Zhang Y et al (2013) Laparoscopic versus open surgery for colon cancer: a meta-analysis of 5-year follow-up outcomes. Surg Oncol 22:e39–e43
Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J (2011) Enhanced Recovery After Surgery Study Group. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 146:571–577
Kennedy RH, Francis EA, Wharton R, Blazeby JM, Quirke P, West NP et al (2014) Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an Enhanced Recovery Programme: EnROL. J Clin Oncol 32:1804–1811
Pedrazzani C, Moro M, Ghezzi G, Ruzzenente A, Delaini G, Guglielmi A (2014) What should we intend for minimally invasive treatment of colorectal cancer? Surg Oncol 23(3):147-154
IMPACT (1995) Efficacy of adjuvant fluorouracil and folinic acid in colon cancer. International Multicentre Pooled Analysis of Colon Cancer Trials (IMPACT) investigators. Lancet 345:939–944
André T, Boni C, Mounedji-Boudiaf L, Navarro M, Tabernero J, Hickish T et al (2004) Multicenter International Study of Oxaliplatin/5-Fluorouracil/Leucovorin in the Adjuvant Treatment of Colon Cancer (MOSAIC) investigators. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 350:2343–2351
Gill S, Loprinzi CL, Sargent DJ, Thomé SD, Alberts SR, Haller DG et al (2004) Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 22:1797–1806
André T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C et al (2009) Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 27:3109–3116
Haller DG, Tabernero J, Maroun J, de Braud F, Price T, Van Cutsem E et al (2011) Capecitabine with oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 29:1465–1471
Nitsche U, Rosenberg R, Balmert A, Schuster T, Slotta-Huspenina J, Herrmann P et al (2012) Integrative marker analysis allows risk assessment for metastasis in stage II colon cancer. Ann Surg 256:763–771
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr et al (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg 246:655–662
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E et al (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG et al (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 100:75–82
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation–technical notes and outcome. Colorectal Dis 11:354–364
Ishiguro M, Higashi T, Watanabe T, Sugihara K, Japanese Society for Cancer of the Colon and Rectum Guideline Committee (2014) Changes in colorectal cancer care in Japan before and after guideline publication: a nationwide survey about D3 lymph node dissection and adjuvant chemotherapy. J Am Coll Surg 218:969–977
Kawada H, Kurita N, Nakamura F, Kawamura J, Hasegawa S, Kotake K et al (2014) Incorporation of apical lymph node status into the seventh edition of the TNM classification improves prediction of prognosis in stage III colonic cancer. Br J Surg 101(9):1143–1152
Cahill RA, Leroy J, Marescaux J (2008) Could lymphatic mapping and sentinel node biopsy provide oncological providence for local resectional techniques for colon cancer? A review of the literature. BMC Surg 8:17
Saha S, Johnston G, Korant A, Shaik M, Kanaan M, Johnston R et al (2013) Aberrant drainage of sentinel lymph nodes in colon cancer and its impact on staging and extent of operation. Am J Surg 205:302–305
Vogelaar FJ, Reimers MS, van der Linden RL, van der Linden JC, Smit VT, Lips DJ et al (2014) The diagnostic value of One-Step Nucleic acid Amplification (OSNA) for sentinel lymph nodes in colon cancer patients. Ann Surg Oncol 21(12):3924–3930
Goldstein NS (2002) Lymph node recoveries from 2427 pT3 colorectal resection specimens spanning 45 years: recommendations for a minimum number of recovered lymph nodes based on predictive probabilities. Am J Surg Pathol 26:179–189
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ et al (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 21:2912–2919
AJCC (American Joint Committee on Cancer) Cancer staging manual (2010) In: Edge SB, Byrd DR, Compton CC et al (eds) 7th edn. Springer, New York, p 143
Ueno H, Mochizuki H, Akagi Y, Kusumi T, Yamada K, Ikegami M et al (2012) Optimal colorectal cancer staging criteria in TNM classification. J Clin Oncol 30:1519–1526
Hari DM, Leung AM, Lee JH, Sim MS, Vuong B, Chiu CG et al (2013) AJCC Cancer Staging manual 7th edition criteria for colon cancer: do the complex modifications improve prognostic assessment? J Am Coll Surg 217:181–190
Hashiguchi Y, Hase K, Kotake K, Ueno H, Shinto E, Mochizuki H et al (2012) Evaluation of the seventh edition of the tumour, node, metastasis (TNM) classification for colon cancer in two nationwide registries of the United States and Japan. Colorectal Dis 14:1065–1074
Japanese Society for Cancer of the Colon and Rectum (JSCCR) (2010) Japanese classification of colorectal carcinoma, 2nd edn. Kanehara & Co., Ltd., Tokyo
Baxter NN, Virnig DJ, Rothenberger DA, Morris AM, Jessurun J, Virnig BA (2005) Lymph node evaluation in colorectal cancer patients: a population-based study. J Natl Cancer Inst 97:219–225
Parsons HM, Begun JW, Kuntz KM, Tuttle TM, McGovern PM, Virnig BA (2013) Lymph node evaluation for colon cancer in an era of quality guidelines: who improves? J Oncol Pract 9:e164–e171
Hewett PJ, Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Rieger NA et al (2008) Short-term outcomes of the Australasian, randomized, clinical study comparing laparoscopic and conventional open surgical treatments of colon cancer: the ALCCaS trial. Ann Surg 248:728–738
Cunningham D, Atkin W, Lenz HJ, Lynch HT, Minsky B, Nordlinger B et al (2010) Colorectal cancer. Lancet 375:1030–1047
O’Connor ES, Greenblatt DY, LoConte NK, Gangnon RE, Liou JI, Heise CP et al (2011) Adjuvant chemotherapy for stage II colon cancer with poor prognostic features. J Clin Oncol 29:3381–3388
Hanna NN, Onukwugha E, Choti MA, Davidoff AJ, Zuckerman IH, Hsu VD et al (2012) Comparative analysis of various prognostic nodal factors, adjuvant chemotherapy and survival among stage III colon cancer patients over 65 years: an analysis using surveillance, epidemiology and end results (SEER)-Medicare data. Colorectal Dis 14:48–55
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA (2007) Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 99:433–441
Willaert W, Mareel M, Van De Putte D, Van Nieuwenhove Y, Pattyn P, Ceelen W (2014) Lymphatic spread, nodal count and the extent of lymphadenectomy in cancer of the colon. Cancer Treat Rev 40:405–413
Kotake K, Honjo S, Sugihara K, Hashiguchi Y, Kato T, Kodaira S et al (2012) Number of lymph nodes retrieved is an important determinant of survival of patients with stage II and stage III colorectal cancer. Jpn J Clin Oncol 42:29–35
Gleisner AL, Mogal H, Dodson R, Efron J, Gearhart S, Wick E et al (2013) Nodal status, number of lymph nodes examined, and lymph node ratio: what defines prognosis after resection of colon adenocarcinoma? J Am Coll Surg 217:1090–1100
Budde CN, Tsikitis VL, Deveney KE, Diggs BS, Lu KC, Herzig DO (2014) Increasing the number of lymph nodes examined after colectomy does not improve colon cancer staging. J Am Coll Surg 218:1004–1011
Wood TF, Saha S, Morton DL, Tsioulias GJ, Rangel D, Hutchinson W Jr et al (2001) Validation of lymphatic mapping in colorectal cancer: in vivo, ex vivo, and laparoscopic techniques. Ann Surg Oncol 8:150–157
Iddings D, Ahmad A, Elashoff D, Bilchik A (2006) The prognostic effect of micrometastases in previously staged lymph node negative (N0) colorectal carcinoma: a meta-analysis. Ann Surg Oncol 13:1386–1392
Mescoli C, Albertoni L, Pucciarelli S, Giacomelli L, Russo VM, Fassan M et al (2012) Isolated tumor cells in regional lymph nodes as relapse predictors in stage I and II colorectal cancer. J Clin Oncol 30:965–971
Rahbari NN, Bork U, Motschall E, Thorlund K, Büchler MW, Koch M et al (2012) Molecular detection of tumor cells in regional lymph nodes is associated with disease recurrence and poor survival in node-negative colorectal cancer: a systematic review and meta-analysis. J Clin Oncol 30:60–70
Sloothaak DA, Sahami S, van der Zaag-Loonen HJ, van der Zaag ES, Tanis PJ, Bemelman WA et al (2014) The prognostic value of micrometastases and isolated tumour cells in histologically negative lymph nodes of patients with colorectal cancer: a systematic review and meta-analysis. Eur J Surg Oncol 40:263–269
Wiese D, Sirop S, Yestrepsky B, Ghanem M, Bassily N, Ng P et al (2010) Ultrastaging of sentinel lymph nodes (SLNs) vs. non-SLNs in colorectal cancer—do we need both? Am J Surg 199:354–358
Croner RS, Geppert CI, Bader FG, Nitsche U, Späth C, Rosenberg R et al (2014) Molecular staging of lymph node-negative colon carcinomas by one-step nucleic acid amplification (OSNA) results in upstaging of a quarter of patients in a prospective, European, multicentre study. Br J Cancer 110:2544–2550
Faerden AE, Sjo OH, Bukholm IR, Andersen SN, Svindland A, Nesbakken A et al (2011) Lymph node micrometastases and isolated tumor cells influence survival in stage I and II colon cancer. Dis Colon Rectum 54:200–206
Reggiani Bonetti L, Di Gregorio C, De Gaetani C, Pezzi A, Barresi G, Barresi V et al (2011) Lymph node micrometastasis and survival of patients with Stage I (Dukes’ A) colorectal carcinoma. Scand J Gastroenterol 46:881–886
Nagayoshi K, Ueki T, Nishioka Y, Manabe T, Mizuuchi Y, Hirahashi M et al (2014) Tumor deposit is a poor prognostic indicator for patients who have stage II and III colorectal cancer with fewer than 4 lymph node metastases but not for those with 4 or more. Dis Colon Rectum 57:467–474
Ueno H, Mochizuki H, Shirouzu K, Kusumi T, Yamada K, Ikegami M et al (2012) Multicenter study for optimal categorization of extramural tumor deposits for colorectal cancer staging. Ann Surg 255:739–746
Hogan NM, Winter DC (2013) A nodal positivity constant: new perspectives in lymph node evaluation and colorectal cancer. World J Surg 37:878–882
Nash GM, Row D, Weiss A, Shia J, Guillem JG, Paty PB et al (2011) A predictive model for lymph node yield in colon cancer resection specimens. Ann Surg 253:318–322
Park IJ, Choi GS, Kang BM, Lim KH, Jun SH (2009) Lymph node metastasis patterns in right-sided colon cancers: is segmental resection of these tumors oncologically safe? Ann Surg Oncol 16:1501–1506
Kanemitsu Y, Komori K, Kimura K, Kato T (2013) D3 lymph node dissection in right hemicolectomy with a no-touch isolation technique in patients with colon cancer. Dis Colon Rectum 56:815–824
Kobayashi H, Enomoto M, Higuchi T, Uetake H, Iida S, Ishikawa T et al (2011) Clinical significance of lymph node ratio and location of nodal involvement in patients with right colon cancer. Dig Surg 28:190–197
Feng B, Sun J, Ling TL, Lu AG, Wang ML, Chen XY et al (2012) Laparoscopic complete mesocolic excision (CME) with medial access for right-hemi colon cancer: feasibility and technical strategies. Surg Endosc 26:3669–3675
Liang JT, Huang KC, Lai HS, Lee PH, Sun CT (2007) Oncologic results of laparoscopic D3 lymphadenectomy for male sigmoid and upper rectal cancer with clinically positive lymph nodes. Ann Surg Oncol 14:1980–1990
Park IJ, Choi GS, Lim KH, Kang BM, Jun SH (2008) Different patterns of lymphatic spread of sigmoid, rectosigmoid, and rectal cancers. Ann Surg Oncol 15:3478–3483
Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B (2000) Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm Colorectal Cancer Study Group, Basingstoke Bowel Cancer Research Project. Lancet 356:93–96
Kapiteijn E, Putter H, van de Velde CJ, Cooperative investigators of the Dutch ColoRectal Cancer Group (2002) Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg 89:1142–1149
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P (2010) Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 28:272–278
West NP, Morris EJ, Rotimi O, Cairns A, Finan PJ, Quirke P (2008) Pathology grading of colon cancer surgical resection and its association with survival: a retrospective observational study. Lancet Oncol 9:857–865
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W et al (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30:1763–1769
Gouvas N, Pechlivanides G, Zervakis N, Kafousi M, Xynos E (2012) Complete mesocolic excision in colon cancer surgery: a comparison between open and laparoscopic approach. Colorectal Dis 14:1357–1364
Adamina M, Manwaring ML, Park KJ, Delaney CP (2012) Laparoscopic complete mesocolic excision for right colon cancer. Surg Endosc 26:2976–2980
Han DP, Lu AG, Feng H, Wang PX, Cao QF, Zong YP et al (2013) Long-term results of laparoscopy-assisted radical right hemicolectomy with D3 lymphadenectomy: clinical analysis with 177 cases. Int J Colorectal Dis 28:623–629
Shin JW, Amar AH, Kim SH, Kwak JM, Baek SJ, Cho JS et al (2014) Complete mesocolic excision with D3 lymph node dissection in laparoscopic colectomy for stages II and III colon cancer: long-term oncologic outcomes in 168 patients. Tech Coloproctol 18(9):795–803
Killeen S, Mannion M, Devaney A, Winter DC (2014) Complete mesocolic resection and extended lymphadenectomy for colon cancer: a systematic review. Colorectal Dis 16(8):577–594
Kotake K, Mizuguchi T, Moritani K, Wada O, Ozawa H, Oki I et al (2014) Impact of D3 lymph node dissection on survival for patients with T3 and T4 colon cancer. Int J Colorectal Dis 29:847–852
Yagci G, Unlu A, Kurt B, Can MF, Kaymakcioglu N, Cetiner S et al (2007) Detection of micrometastases and skip metastases with ex vivo sentinel node mapping in carcinoma of the colon and rectum. Int J Colorectal Dis 22:167–173
Cahill RA, Leroy J, Marescaux J (2009) Localized resection for colon cancer. Surg Oncol 18:334–342
Bianchi PP, Petz W, Casali L (2011) Laparoscopic lymphatic roadmapping with blue dye and radioisotope in colon cancer. Colorectal Dis 13(Suppl 7):67–69
van der Pas MH, Meijer S, Hoekstra OS, Riphagen II, de Vet HC, Knol DL et al (2011) Sentinel-lymph-node procedure in colon and rectal cancer: a systematic review and meta-analysis. Lancet Oncol 12:540–550
van der Zaag ES, Bouma WH, Tanis PJ, Ubbink DT, Bemelman WA, Buskens CJ (2012) Systematic review of sentinel lymph node mapping procedure in colorectal cancer. Ann Surg Oncol 19:3449–3459
Bembenek AE, Rosenberg R, Wagler E, Gretschel S, Sendler A, Siewert JR et al (2007) Sentinel lymph node biopsy in colon cancer: a prospective multicenter trial. Ann Surg 245:858–863
Iddings D, Bilchik A (2007) The biologic significance of micrometastatic disease and sentinel lymph node technology on colorectal cancer. J Surg Oncol 96:671–677
Nicholl M, Bilchik AJ (2008) Is routine use of sentinel node biopsy justified in colon cancer? Ann Surg Oncol 15:1–3
Schaafsma BE, Verbeek FP, van der Vorst JR, Hutteman M, Kuppen PJ, Frangioni JV et al (2013) Ex vivo sentinel node mapping in colon cancer combining blue dye staining and fluorescence imaging. J Surg Res 183:253–257
Kitagawa Y, Kitajima M (2002) Gastrointestinal cancer and sentinel node navigation surgery. J Surg Oncol 79:188–193
Mutter D, Rubino F, Sowinska M, Henri M, Dutson E, Ceulemans R et al (2004) A new device for sentinel node detection in laparoscopic colon resection. JSLS 8:347–351
Wallace AM, Ellner SJ, Méndez J, Hoh CK, Salem CE, Bosch CM et al (2006) Minimally invasive sentinel lymph node mapping of the pig colon with Lymphoseek. Surgery 139:217–223
Wong JH, Steineman S, Calderia C, Bowles J, Namiki T (2001) Ex vivo sentinel node mapping in carcinoma of the colon and rectum. Ann Surg 233:515–521
Saha S, Seghal R, Patel M, Doan K, Dan A, Bilchik A et al (2006) A multicenter trial of sentinel lymph node mapping in colorectal cancer: prognostic implications for nodal staging and recurrence. J Am Coll Surg 191:305–310
Lim SJ, Feig BW, Wang H, Hunt KK, Rodriguez-Bigas MA, Skibber JM et al (2008) Sentinel lymph node evaluation does not improve staging accuracy in colon cancer. Ann Surg Oncol 15:46–51
Faerden AE, Sjo OH, Andersen SN, Hauglann B, Nazir N, Gravdehaug B et al (2008) Sentinel node mapping does not improve staging of lymph node metastasis in colonic cancer. Dis Colon Rectum 51:891–896
van der Zaag ES, Buskens CJ, Kooij N, Akol H, Peters HM, Bouma WH et al (2009) Improving staging accuracy in colon and rectal cancer by sentinel lymph node mapping: a comparative study. Eur J Surg Oncol 35:1065–1070
Nagata K, Endo S, Hidaka E, Tanaka J, Kudo SE, Shiokawa A (2006) Laparoscopic sentinel node mapping for colorectal cancer using infrared ray laparoscopy. Anticancer Res 26:2307–2311
Hirche C, Mohr Z, Kneif S, Doniga S, Murawa D, Strik M et al (2012) Ultrastaging of colon cancer by sentinel node biopsy using fluorescence navigation with indocyanine green. Int J Colorectal Dis 27:319–324
Sardón Ramos JD, Errasti Alustiza J, Campo Cimarras E, Cermeño Toral B, Romeo Ramírez JA, de Ugarte S, Sobrón J et al (2013) Sentinel lymph node biopsy technique in colon cancer. Experience in 125 cases. Cir Esp 91:366–371
Paramo JC, Summerall J, Wilson C, Cabral A, Willis I, Wodnicki H et al (2001) Intraoperative sentinel lymph node mapping in patients with colon cancer. Am J Surg 182:40–43
Bilchik AJ, Trocha SD (2003) Lymphatic mapping and sentinel node analysis to optimize laparoscopic resection and staging of colorectal cancer: an update. Cancer Control 10:219–223
Montgomery LL, Thorne AC, Van Zee KJ, Fey J, Heerdt AS, Gemignani M et al (2002) Isosulfan blue dye reactions during sentinel lymph node mapping for breast cancer. Anesth Analg 95:385–388
Thevarajah S, Huston TL, Simmons RM (2005) A comparison of the adverse reactions associated with isosulfan blue versus methylene blue dye in sentinel lymph node biopsy for breast cancer. Am J Surg 189:236–239
Bézu C, Coutant C, Salengro A, Daraï E, Rouzier R, Uzan S (2011) Anaphylactic response to blue dye during sentinel lymph node biopsy. Surg Oncol 20:e55–e59
Khullar O, Frangioni JV, Grinstaff M, Colson YL (2009) Image-guided sentinel lymph node mapping and nanotechnology-based nodal treatment in lung cancer using invisible near-infrared fluorescent light. Semin Thorac Cardiovasc Surg 21:309–315
van der Pas MH, Ankersmit M, Stockmann HB, Silvis R, van Grieken NC, Bril H et al (2013) Laparoscopic sentinel lymph node identification in patients with colon carcinoma using a near-infrared dye: description of a new technique and feasibility study. J Laparoendosc Adv Surg Tech 23:367–371
Braat AE, Pol RA, Oosterhuis JW, de Vries JE, Mesker WE, Tollenaar RA (2014) Excellent prognosis of node negative patients after sentinel node procedure in colon carcinoma: a 5-year follow-up study. Eur J Surg Oncol 40:747–755
Bianchi PP, Ceriani C, Rottoli M, Torzilli G, Roncalli M, Spinelli A et al (2007) Laparoscopic lymphatic mapping and sentinel lymph node detection in colon cancer: technical aspects and preliminary results. Surg Endosc 21:1567–1571
Acknowledgments
The authors thank Tiziano Leso for editing figures and tables.
Conflict of interests
None declared
Research funding
None declared
Author information
Authors and Affiliations
Corresponding author
Additional information
Short summary
Extended colonic resection and sentinel lymph node mapping play roles in the management of nodal disease from colon cancer, both of which can improve staging in node negative patients in a minimally invasive setting.
Rights and permissions
About this article
Cite this article
Pedrazzani, C., Lauka, L., Sforza, S. et al. Management of nodal disease from colon cancer in the laparoscopic era. Int J Colorectal Dis 30, 303–314 (2015). https://doi.org/10.1007/s00384-014-2075-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-2075-8