Abstract
Purpose
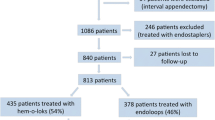
The present study aims to compare strength, healing, and inflammation of appendiceal stumps closed by LigaSure Precise™ (Valleylab, Boulder, CO, USA) device, ligatures using polyglactin 910 (Vicryl, Ethicon, Edinburgh, UK) and endoclips (Ligaclip ERCA, Ethicon, OH, USA), and operation time (OT) in experimental appendectomy.
Methods
Forty-eight Sprague–Dawley rats were divided into two (Group A and B). Each group was further subdivided into three subgroups (AS, AC, AL, BS, BC, BL) containing eight rats. Appendectomy was performed and stump was closed by ligatures in S, by endoclips in C and by LigaSure™ in L subgroups. OT was recorded. In Group A, cecum bursting pressures (BP) were determined instantly after the operation. In Group B, BP, histological evaluations, and measurements of collagen contents estimated by the tissue hydroxyproline (HPL) level were made on the seventh postoperative day. Statistical analyses were performed with Kruskal–Wallis test and Mann–Whitney U test. P value was considered significant at less than 0.05.
Results
BPs of subgroups were comparable on postoperative immediate period and day 7. HPLs and OTs were significantly better in L subgroups. BL had the least inflammation.
Conclusion
Better healing, less inflammation, shorter OT, and equal strength achieved with LigaSure™ device comparing with polyglactin 910 ties and endoclips in experimental appendectomy is encouraging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although laparoscopic appendectomy in children is mostly well adopted, technical difficulties may limit its wider acceptance [1–3]. Ligatures, clip appliance, or stapling of both appendix and meso-appendix were described in laparoscopic appendectomy for controlling the appendiceal stump and vessels [3, 4]. Intracorporal ligature techniques requiring major skill are usually accused of increasing the operation time while stapling techniques are of increasing costs [1, 3, 5]. Besides, use of endoclips for securing the appendiceal stump is under debate because of the possible insufficiency of attained occlusive force [4].
The LigaSure™ vessel sealing system is a bipolar feedback-controlled sealing system that effectively seals vessels up to 7 mm in diameter with the minimal thermal spread. The device applies a precise amount of mechanical pressure and radiofrequency energy to tissue, causing fusion of the opposing layers by creating a seal of denatured collagen, which can then be transected [6]. The superiority of LigaSure™ over bipolar electrocautery is that the tissue fusion is created by the denaturation of proteins, thus forming a true seal rather than creation of a proximal thrombus [http://www.ligasure.com/pages/atlas.htm]. Experimental cystic duct closures, intestinal resection, and anastomosis were performed by LigaSure™ vessel sealing system [6, 7–10]. As collagen is abundantly present in the intestinal wall, we assumed that the device would have been capable of creating intestinal seals, and would have had enabled secure appendectomy.
This study was designed to search for an alternative, easier, and safer technique in laparoscopic appendectomy. Experimental appendectomy was performed in Sprague–Dawley rats, comparing the use of LigaSure Precise™ vessel sealing device, endoclips, and ligatures in division of meso-appendix and securing of the appendiceal stump.
Materials and methods
Experiments were conducted in accordance with the Guide for the Care and Use of Laboratory Animals and the experimental protocol was approved by the Faculty Committee for the Ethics on Animal Care and Experiments.
Forty-eight male Sprague–Dawley rats (weights ranged between 230 and 325 g with a mean of 276.02 ± 28.76 g) were randomly allocated into two groups (Group A and B). These groups were further subdivided into six subgroups as AS, AC, AL, BS, BC, and BL each containing eight rats.
Operations were performed under aseptic conditions. Ether inhalation was combined with intraperitoneal ketamine hydrochloride (50 mg/kg body weight) for anesthesia. After abdominal skin was shaved, a midline vertical laparotomy was performed. Appendix vermiformis (or a blind bowel originated from the cecum, approximately 1 cm in diameter and 1.5–2 cm in length) was found. In S subgroups, meso-appendix, and appendiceal base were ligated with 4/0 polyglactin 910 (Vicryl, Ethicon, Edinburgh, UK) ties and appendectomy was performed subsequently. In C subgroups, following utilization of two endoclips (10 mm, Ligaclip ERCA, Ethicon, OH, USA) on the meso-appendix, transection was performed. Base of appendix was occluded with an endoclip and appendectomy was then performed. In L subgroups after meso-appendix was divided by LigaSure Precise™ (Valleylab, Boulder, CO, USA) instrument, the device was applied to appendiceal base until the formation of two adjacent white lines delineating the coagulation borders (Fig. 1). Subsequently, the appendix was resected from just middle of the coagulation lines thus both appendiceal base and stump remained sealed (Fig. 2). None of the appendiceal stumps were buried to resemble laparoscopic removal of appendices. Diameters of all appendices were measured as millimeters, and the time needed to perform each appendectomy (OT) was measured as minutes and noted. All appendices were preserved for histological evaluation.
In Group A, rats were sacrificed by high dose of intraperitoneal ketamine hydrochloride (100 mg/kg body weight) immediately after the appendectomy. The colon was opened 2 cm distally from the cecum, contents were removed and tied with a 2/0 silk suture. The proximal ileal segment was cut and opened at a 2 cm distance from the cecum, intestinal contents were removed and a 22-gauge catheter was introduced to the lumen. This catheter was secured and fixed to a three-way stopcock connected to an infusion pump (62-HF-0267-00, Abbott, Chicago, IL, USA), which was infusing air at a constant rate of 1 mL/min and a manometer for simultaneous bursting pressure (BP) measurement. BP measurement as mmHg was performed in a saline-filled container. The bursts were defined as air bubbles escaping from the appendiceal stump.
In Group B, abdomen was closed after appendectomy and the rats were allowed to live until the seventh postoperative day when they would be sacrificed and cecum-bursting pressures would be measured. Integrity of the stump, sign of leakage, presence of adhesions, and existence of peritonitis were recorded during postmortem exploration. In order to protect intraperitoneal conditions, adhesions were not separated and the cecum was removed with the surrounding omentum and intestines together [11]. Following aforementioned BP measurement, endoclips, and ligatures on the stump were removed, and a 1 cm2 cecal segment containing the stump in the middle, was resected and divided into two pieces. One of these pieces was preserved for hydroxyproline level (HPL) analysis, which represented the tissue collagen content and the other one for histological evaluation.
The specimens for HPL analyses were wrapped in an aluminum package and conserved in a deep freezer at −80°C. HPL analyses were performed by using hydroxyproline kit (Hypronisiticon, Organon, NL, USA) according to the principles described by Stegemann and Stalder [12]. Results were noted as micrograms per milligram of wet tissue.
Histological sections were stained by hematoxylin and eosin (H&E) and photomicrographs were taken by a histologist who was blinded to the origin of the specimen. Inflammation was evaluated with a semi-quantitative scale modified from Biert et al. and Verhofstad et al. (Table 1) [13, 14].
Statistical analyses were performed with SPSS 13.0 (SPSS Inc, Chicago, IL, USA) software system. Kruskal–Wallis test was utilized for variance analyses. Mann–Whitney U test was used to calculate the differences between two subgroups. Paired subgroups were compared by Wilcoxon-Signed Rank test. The statistical significance was set at P less than 0.05 with a confidence rate of 95%.
Results
All rats in Group A were sacrificed immediately after the operation. All rats in Group B survived, and had started feeding and were defecating within 24 h postoperatively. All subgroups were comparable according to their weights.
When re-laparotomy was performed, clear intraabdominal fluid was present in all rats but no fecal material was detected. All appendiceal stumps were found to be surrounded by omentum. In one rat in BC, omentum and intestinal segments were found to be adhered to the stump. In three rats in BS, local abscess formation, and adhesion of omentum and intestinal segments, forming a compact mass tissue was noted.
In Group A, the difference among BP values of AL (121.87 ± 29.02 mmHg), AC (130.00 ± 17.72 mmHg) and AS (137.50 ± 25.49 mmHg) were not statistically significant (P > 0.05) (Table 2). Similarly, BPs in Group B were comparable with values of BL (160.00 ± 26.18 mmHg), BC (152.50 ± 28.15 mmHg) and BS (165.00 ± 22.03 mmHg) (P > 0.05) (Table 3). BPs in Group A were lower than the BPs in Group B (P < 0.05). Although, BPs of AS versus BS (P = 0.05) and AC versus BC (P = 0.055) were similar, BPs of AL was significantly lower than BL (P = 0.046).
Statistical analyses of HPLs revealed a significant difference between the subgroups (P = 0.01). HPL was significantly increased in BL (3.98 ± 0.16 μg/wet tissue) compared with BC (3.54 ± 0.27 μg/wet tissue) (P < 0.001) and BS (3.00 ± 0.27 μg/wet tissue) (P < 0.001). HPLs in BC were significantly higher than BS (P < 0.05) (Table 3).
Comparison of OTs in Group A revealed a significant difference (P = 0.01). AL (2.68 ± 0.59 min) and AC (3.81 ± 1.25 min) (P = 0.05) were hardly comparable, but AL was significantly shorter than AS (4.75 ± 1.38 min) (P = 0.005). AC and AS were also comparable (P = 0.23) (Table 2). In Group B comparison of OTs also revealed a significant difference (P = 0.012). BL (2.50 ± 0.80 min) was significantly shorter than BC (3.75 ± 0.88) (P = 0.015) and BS (4.25 ± 1.25 min) (P = 0.01), but BC and BS were similar (P = 0.5) (Table 3). Although, Group B had a shorter duration (3.50 ± 1.21 min) than Group A (3.75 ± 1.38 min) they were comparable (P > 0.05).
Appendix diameters in Group A was 9.9 ± 0.9 mm, and in Group B was 9.8 ± 0.7 mm. Comparison of appendix diameters in Group A (P = 0.94) and in Group B (P = 0.99) showed that all subgroups were comparable (Tables 2, 3).
Histological examinations
Macroscopic examination of the appendiceal bases in AS, AC, BS, and BC revealed luminal patency of all specimens, while appendices in AL and BL were found to be totally closed. Similarly, histological evaluation showed that the appendiceal bases were patent with normal cellularity and structure in AS, AC, BS, and BC. Appendiceal bases in AL and BL were all found to be completely sealed. The crypt-villi architecture, surface epithelium and lamina propria was observed to be disappeared, but muscularis mucosa and tunica submucosa were found to be spared. Sealing created by LigaSure™ device was beginning by the surface epithelium and extending to the muscularis mucosa. Cavitation defects, those were scattered between lamina propria and muscularis externa were abundantly increased in the submucosa (Fig. 3a, b). Neighboring area had normal configuration and architecture.
Histological findings of the specimens sealed by LigaSure in subgroup AL. a Cross section of a sealed appendiceal base (H&E, ×20). The lumen is closed and tunica mucosa is disappeared. Gray arrow fused muscularis mucosa of the opposing walls. Black arrows fissuring/cavitation defects along the appendix. b Cross section of a sealed appendiceal stump and cecum (H&E, ×20). Gray arrow disappearance of tunica mucosa and tunica submucosa in the sealing area. Black arrow presence of tunica mucosa and tunica submucosa in cecum
Microscopic evaluation of appendiceal stumps revealed that inflammation in lamina propria and submucosa was more profuse in BS. Micro abscess formation with polymorpho-nuclear leukocytes (PMNL) and macrophages were detected in three specimens in BS and one in BC. Subgroups BL, BC, and BS were comparable with respect to lymphocyte quantity (P = 0.058). Evaluation of necrosis status (P = 0.005), PMNL quantity (P = 0.047), macrophage quantity (P = 0.028), and total scores (P = 0.001) revealed significant differences (Table 3). Comparison of BC versus BS revealed a significantly elevated total score in BS (P = 0.005). Comparison of BL versus BS revealed significant increases in necrosis status (P = 0.005), PMNL quantity (P = 0.038), macrophage quantity (P = 0.021) and total score (P = 0.001) in BS. Comparison of BL vs. BC showed that necrosis status (P = 0.015) and total score (P = 0.038) were significantly elevated in BC.
Discussion
Despite the documented benefits of laparoscopic appendectomy in pediatric patients, there is still ongoing reluctance at least at beginners, which can be partly attributed to the increased technical demand for controlling the meso-appendix and the appendiceal stump [1, 2, 5, 15–21]. Certainly, the optimal method should comprise minimal skill requirements with maximum security avoiding bleeding from appendiceal vessels, intra-operative spillage of appendiceal contents and postoperative stump leakage [19, 21].
Several methods are described to achieve a reduction in the complexity of the procedure [1, 4, 17, 19–21]. Meso-appendix can be controlled successfully with endoclips or electro-coagulation [3, 19, 22]. Intracorporal ligatures, prettied knots or endoloops can be used to ensure closing of the appendiceal stump, but they may be accused of increasing operation time in inexperienced hands [5]. Furthermore, they may have the disadvantages of slipping and spillage of infective content, unless appendix is divided between two ligatures one of which remains on appendix and one on the stump [5, 21]. Although, linear staples are utilized with the advantage of closing appendiceal stump with concurrent securing of the meso-appendix they have the handicap of raising operative costs [2, 5, 17, 21, 23, 24]. Laparoscopic clips may be of another choice but sufficiency of attained occlusive force for the stump is under discussion [4, 25, 26]. Thermal electro-coagulation with bipolar electrocautery was used in two studies and found to yield satisfactory results for controlling the meso-appendix with closing appendiceal base and stump [17, 22]. Similarly, Yang et al. performed the laparoscopic appendectomy by radiofrequency coagulation with LigaSure™ device, and concluded that it was practical in division of meso-appendix and occlusion of the stump [19].
Healing in the appendiceal stump may be regarded as a normal polyphasic wound repair process occurring in three periods as: Lag phase (day 0–4), fibroplasia phase (day 3–14) and maturation phase (beyond 10 days) [27]. Hence, the surgical trauma causes an inflammatory reaction, fibrin clot formation, edema, PMNL and macrophage infiltration, fibroblast accumulation and formation of new collagen [13]. Following full thickness injury of the intestine healing can be achieved by approximation of intestinal layers, particularly collagen containing submucosa of the opposing intestinal walls [6, 13, 14, 28]. This type of primary healing in the appendiceal stump can be valid only if appendiceal walls are approximated and fused layer by layer as done by LigaSure™ [6]. On the contrary, healing in ligated or clipped stumps seems to occur as a secondary process. Since we found increased necrosis status in BC and BS comparing with BL, we believe that mucosal and sub-mucosal necrosis due to compression of clips or ligatures was followed by inflammation and new collagen formation which in turn improved the strength of the stump on the ongoing healing.
The collagen content which is measured by the HPL content is a good indicator of healing [13]. Increased HPL levels in BL compared with BC and BS may be due to the collagen reforming feature of LigaSure™ ensuring a better healing [6, http://www.ligasure.com/pages/atlas.htm]. Thus, collagen synthesis seems to have started immediately and had a faster onset after the tissue damage in BL [29]. On the other hand, lower HPL levels in BC and BS may be because of either disruption of the blood flow at the stump site caused by sutures or clips compression, or foreign body reaction against these materials that may cause severe tissue damage with concomitant profuse inflammation and lessened healing as previously described in intestinal anastomoses [30, 31].
Bursting pressure measurement demonstrates evenly distributed transmural pressure in both longitudinal and circular directions and is considered as a reliable index that closely approximates the clinical situation [11, 32]. In our experimental model, although BPs of L subgroups was lower than C and S subgroups the difference was not statistically significant. As the strength of the stump should mainly depend on the suture materials holding capacity on the first few days of healing it can easily be assumed that seal created by LigaSure™ was as powerful as polyglactin 910 sutures and endoclips on both postoperative immediate period and on day 7 [33]. The significant increase in BPs in BL versus AL may indirectly indicate that the fibroplasia phase was better in L subgroups and the wound integrity was solely relied on the newly formed collagen on day 7 [27].
Wound healing is the outcome of coordinated action of several cell types. PMNLs and macrophages are involved in removal of cell debris [14]. We observed increased PMNL and macrophage quantity in BS and BC with micro-abscess formation in three specimens in BS and in one specimen in BC conceptually similar to stump abscess seen after appendectomy [34]. Stump abscess is usually considered to result from a long stump left behind [35]. As we left only a 1–2 mm long stump, we believe that tight sutures or endoclips leading to ischemic injury might be the cause which may be concluded by the increased necrosis status in BC and BS [23]. On the other hand, the current condition might be due to exposure of the remaining contaminated intestinal mucosa to the abdominal cavity. Microbial contamination of the abdomen was not subject to the present study, but we may speculate that, as no mucosa was present in BL no contamination and abscess formation occurred [23]. But, the fact that many appendectomies are performed without complications with only simple ligation of the stump may be attributed to the use of postoperative antimicrobial therapy in the humans and thus confines our hypothesis to rats.
The diameter of normal appendix in children is usually less than 1 cm, and the maximal outer diameter of the appendix is calculated to be as 0.21–0.64 cm [36]. Je et al. found an increase in the maximal outer diameter of the appendix in children with appendicitis up to 4.2-14.5 mm (Median: 7.6 mm) [37]. On this context, utilization of LigaSure™ device on appendices with a mean diameter of 9.9 ± 0.79 mm seems to be legitimate. All the appendiceal bases in L subgroups were found to be completely sealed, which is certainly an advantage in preventing spillage of infective content in laparoscopic removal of appendices [19]. We used a 5 mm LigaSure™ device instead of a 10 mm one as its jaws would be too wide for the rat appendix. Obviously, the latter would have had the ability of creating a wider seal ensuring securer closing of both appendiceal base and stump, which could have been an advantage in longer appendices and bigger cecums as in humans.
Our study is an animal survey, and it has got some limitations, one of which is the lack of the clinical picture of appendicitis in the transected appendices. Thus, our results do not reflect the actual effect of LigaSure™ on the inflamed intestine. Besides, rat blind bowel although resembles the appendix in the human, is not a true lymphoid organ. Another point is the cost of LigaSure™ usage in appendectomy. The cost of the LigaSure™ generator may be offset as it is standard equipment in the operating theatre but the cost of one LigaSure™ head is about 900 USD. When compared with staples used in appendectomy, a two-folded increase in the operation expenses is established, which may be subdued by the invention of re-usable LigaSure™ heads in the future.
In the present study, appendiceal stumps 1 cm in diameter were closed easily by laparoscopic LigaSure Precise™ device. In addition, shorter duration of operation, decreased rate of inflammation and better healing of the appendiceal stumps achieved by LigaSure™ vessel sealing system is encouraging. Experimental studies using the appendicitis models may be needed. Further researches on the application of LigaSure™ to inflamed human appendix and its effects on the healing are mandatory before recommending its usage in the clinical setting. However, utilization of LigaSure™ vessel sealing system was observed to be a safe and efficient method for transection of meso-appendix as well as complete closure of the appendiceal base and stump in the experimental setting.
References
Dunn JCY (2006) Appendicitis. In: Grosfeld JL, O’ Neill JA, Fonkalsrud EW et al (eds) Pediatric Surgery, 6th edn. Mosby, Philadelphia, pp 1501–1513
Wehrman WE, Tangren CM, Inge TH (2007) Cost analysis of ligature versus stapling techniques of laparoscopic appendectomy in children. J Laparoendosc Adv Surg Tech A 17:371–374
Ponsky TA, Rothenberg SS (2009) Division of the mesoappendix with electrocautery in children is safe, effective, and cost-efficient. J Laparoendosc Adv Surg Tech A 19:11–13. doi:10.1089/lap.2008.0101.supp
Hanssen A, Plotnikov S, Dubois R (2007) Laparoscopic appendectomy using a polymeric clip to close the appendicular stump. JSLS 11:59–62
Sajid MS, Rimple J, Cheek E, Baig MK (2009) Use of endo-GIA versus endo-loop for securing the appendicular stump in laparoscopic appendicectomy: a systematic review. Surg Laparosc Endosc Percutan Tech 19:11–15
Smulders JF, de Hingh IH, Stavast J, Jackimowicz JJ (2007) Exploring new technologies to facilitate laparoscopic surgery: creating intestinal anastomoses without sutures or staples, using a radio-frequency-energy-driven bipolar fusion device. Surg Endosc 21:2105–2109
Shamiyeh A, Vattay P, Tulipan L, Schrenk P, Bogner S, Danis J, Wayand W (2004) Closure of the cystic duct during laparoscopic cholecystectomy with a new feedback-controlled bipolar sealing system in case of biliary obstruction–an experimental study in pigs. Hepatogastroenterology 51:931–933
Matthews BD, Pratt BL, Backus CL, Kercher KW, Mostafa G, Lentzner A, Lipford EH, Sing RF, Heniford BT (2001) Effectiveness of the ultrasonic coagulating shears, LigaSure vessel sealer, and surgical clip application in biliary surgery: a comparative analysis. Am Surg 67:901–906
Schulze S, Krisitiansen VB, Fischer Hansen B, Rosenberg J (2002) Sealing of cystic duct with bipolar electrocoagulation. Surg Endosc 16:342–344
Sorgato N, Bernante P, Pelizzo MR (2008) Application of the LigaSure tissue sealing system to intestinal resection. Experimental and clinical trial. Ann Ital Chir 79:383–388
Cihan A, Armutcu F, Ucan BH, Acun Z, Numanoglu VK, Gürel A, Ulukent SC (2003) Comparison of the measurement methods of bursting pressure of intestinal anastomoses. Hepatogastroenterology 50(Suppl 2):ccxxxii–ccxxxiv
Stegemann H, Stalder K (1967) Determination of hydroxyproline. Clin Chim Acta 18:267–273
Biert J, Seifert WF, Verhofstad AA, Wobbes T, de Man BM, Hoogenhout J, Hendriks T (1998) A semiquantitative histological analysis of repair of anastomoses in the rat colon after combined preoperative irradiation and local hyperthermia. Radiat Res 149:372–377
Verhofstad MH, Lange WP, van der Laak JA, Verhofstad AA, Hendriks T (2001) Microscopic analysis of anastomotic healing in the intestine of normal and diabetic rats. Dis Colon Rectum 44:423–431
Morrow SE, Newman KD (2007) Current management of appendicitis. Semin Pediatr Surg 16:34–40
Esposito C, Borzi P, Valla JS, Mekki M, Nouri A, Becmeur F, Allal H, Settimi A et al (2007) Laparoscopic versus open appendectomy in children: a retrospective comparative study of 2,332 cases. World J Surg 31:750–755
Aslan A, Karaveli C, Elpek O (2008) Laparoscopic appendectomy without clip or ligature. An experimental study. Surg Endosc 22:2084–2087
Little DC, Custer MD, May BH, Blalock SE, Cooney DR (2002) Laparoscopic appendectomy: an unnecessary and expensive procedure in children? J Pediatr Surg 37:310–317
Yang HR, Wang YC, Chung PK, Jeng LB, Chen RJ (2005) Laparoscopic appendectomy using the LigaSure Vessel Sealing System. J Laparoendosc Adv Surg Tech A 15:353–356
Olguner M, Akgür FM, Uçan B, Aktuğ T (1998) Laparoscopic appendectomy in children performed using single endoscopic GIA stapler for both mesoappendix and base of appendix. J Pediatr Surg 33:1347–1349
Kazemier G, in’t Hof KH, Saad S, Bonjer HJ, Sauerland S (2006) Securing the appendiceal stump in laparoscopic appendectomy: evidence for routine stapling? Surg Endosc 20:1473–1476
Khanna S, Khurana S, Vij S (2004) No clip, no ligature laparoscopic appendectomy. Surg Laparosc Endosc Percutan Tech 14:201–203
Beldi G, Vorburger SA, Bruegger LE, Kocher T, Inderbitzin D, Candinas D (2006) Analysis of stapling versus endoloops in appendiceal stump closure. Br J Surg 93:1390–1393
Klima S (1998) Importance of appendix stump management in laparoscopic appendectomy. Zentralbl Chir 123:90–93
Cristalli BG, Izard V, Jacob D, Levardon M (1991) Laparoscopic appendectomy using a clip applier. Surg Endosc 5:176–178
Antal A, Pósa I, Kovács Z, Nagy G (2007) Simplified economical laparoscopic appendectomy. Magy Seb 60:87–89
Ballantyne GH (1983) Intestinal suturing. Review of the experimental foundations for traditional doctrines. Dis Colon Rectum 26:836–843
Shomaf M (2003) Histopathology of human intestinal anastomosis. East Mediterr Health J 9:413–421
Knighton DR, Hunt TK, Thakral KK, Goodson WH 3rd (1982) Role of platelets and fibrin in the healing sequence: an in vivo study of angiogenesis and collagen synthesis. Ann Surg 196:379–388
Thornton FJ, Barbul A (1997) Healing in the gastrointestinal tract. Surg Clin North Am 77:549–573
Elemen L, Sarimurat N, Ayik B, Aydin S, Uzun H (2009) Is the use of cyanoacrylate in intestinal anastomosis a good and reliable alternative. J Pediatr Surg 44:581–586
Del Rio JV, Beck DE, Opelka FG (1996) Chronic perioperative steroids and colonic anastomotic healing in rats. J Surg Res 66:138–142
Wise L, McAlister W, Stein T, Schuck P (1975) Studies on the healing of anastomoses of small and large intestines. Surg Gynecol Obstet 141:190–194
Menteş O, Zeybek N, Oysul A, Onder SC, Tufan T (2008) Stump appendicitis, rare complication after appendectomy: report of a case. Ulus Travma Acil Cerrahi Derg 14:330–332
Al-Dabbagh AK, Thomas NB, Haboubi N (2009) Stump appendicitis. A diagnostic dilemma. Tech Coloproctol 13:73–74
Wiersma F, Srámek A, Holscher HC (2005) US features of the normal appendix and surrounding area in children. Radiology 235:1018–1022
Je BK, Kim SB, Lee SH, Lee KY, Cha SH (2009) Diagnostic value of maximal-outer-diameter and maximal-mural-thickness in use of ultrasound for acute appendicitis in children. World J Gastroenterol 15:2900–2903
Conflict of interest statement
The authors declare that, they do not have a financial relationship with any organization, and that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elemen, L., Yazir, Y., Tugay, M. et al. LigaSure™ compared with ligatures and endoclips in experimental appendectomy: how safe is it?. Pediatr Surg Int 26, 539–545 (2010). https://doi.org/10.1007/s00383-010-2557-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-010-2557-x