Abstract
Background
We aimed to test the efficacy and safety of closure of the appendeceal stump with only laparoscopic bipolar electrocautery in rats.
Methods
In this study, 40 female Wistar-Albino rats were used. In group I (n = 10), appendix vermiformis, approximately 1 cm in width, was completely ligated with 3/0 silk suture close to cecum, and removed. In group II (n = 20) and group III (n = 10), the appendeceal stump was coagulated by bipolar cautery. The coagulation of 70 mA took 10 s, and was repeated one more time. The stump was divided, and checked to ensure complete occlusion. Groups I and II underwent relaparotomy at 15 days, cecum was taken out, and the burst pressure of the stump was measured. Group III did not undergo relaparotomy; the burst pressure was measured during the first laparotomy.
Results
All rats survived. At relaparotomy, no intra-abdominal complications were detected, including intestinal obstruction, abscess, and leakage. Omentum and fatty tissue of uterus was adhered to the appendix stump in group I, but only fatty tissue of uterus was adhered on the stump in group II. Although the intracecal pressure reached 30 cmH2O, at which pressure the cecum was highly stretched, ligated (group I) or coagulated (group II) stumps did not burst or opened. In group III, the burst or opening pressure of the stump (11.2 ± 2.7 cmH2O) was significantly lower than in groups I and II (p < 0.001). Of group II rats, 80% had complete epithelial regeneration at the coagulated stump sites in contrast to ligated rats (p < 0.001) with severe inflammatory changes, abscess, and necrosis.
Conclusions
At late course, coagulated stumps did not allow the leakage or burst, unlike ligated stumps. However, coagulation of the stump seemed to contribute more to epithelial healing. This experimental model suggests that the closure of the stump with only bipolar coagulation was a safe and feasible method.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Appendicitis is one of the leading causes of acute abdomen requiring urgent surgery [1], with a lifetime incidence of 8% in males and 6.3% in females [2]. Compared with conventional laparotomy, laparoscopic appendectomy has the advantages of precise operative diagnosis, lower morbidity, and fewer intraoperative and postoperative complications [3–7]. Although the global cost may be less, particularly for patients whose return to work is hastened by a laparoscopic approach, the cost of hospital care is higher [8]. To diminish the cost of laparoscopic appendectomy, several methods have been incorporated, such as one- or two-trocar techniques, instrument-assisted knotting, skeletonization of appendix by bipolar coagulation, and closure of the stump by endoloop suture or clip applier rather than endostaplers [9–12]. Khanna et al. [13] recommended a novel technique of laparoscopic appendectomy, in which the stump is closed by bipolar coagulation and no clip applicators, needle holders or knot pushers were required; in the English literature, despite the first clinical study [13] related to this topic, the safety and efficacy of this novel technique are not satisfactorily demonstrated. In this study, we designed an experimental model in rats in which the stump of appendix vermiformis was closed only by bipolar coagulation for the evaluation of the burst or leakage pressure of the stump and histopathological changes in the stump site.
Materials and methods
The study was initiated after its approval by the animal investigation committee of Akdeniz University School of Medicine. The animals (female Wistar–albino rats) weighing 210–240 g were kept under standard laboratory conditions before operation, and all rats underwent surgery following overnight fasting. Anesthesia was achieved with intramuscularly xylazine (10 mg/kg) and ketamine (50 mg/kg). No rat took antibiotics.
Surgical procedure
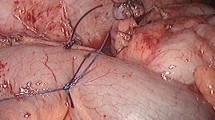
The rats were divided into three groups. In group I (ligature, n = 10), appendix vermiformis (or a blind bowel originated from the cecum, approximately 1 cm in diameter and 1.5–2 cm in length) was ligated with 3/0 silk suture just above the cecum, and taken out. In group II (n = 20) and group III (n = 10), the appendeceal stump was coagulated by laparoscopy-fitted bipolar cautery (Power Blade, Lina Tripol 5, Denmark). Initially, in the pilot studies we detected that the degree of bipolar coagulation should be 70 mA for safety and complete closure of the appendeceal base. Each coagulation took 10 s, and was repeated one more time, with the stump site wetted before each coagulation so that the legs of the cautery could adhere to the tissue. Complete coagulation achieved a constriction ring and no bubbles at the cautery site (Fig. 1a). The stump was then divided with scissors at the constriction site (Fig. 1b), and checked to ensure complete occlusion. If leakage was detected from the stump site, the process of coagulation was repeated until the stump was completely occluded. Groups I and II underwent relaparotomy at 15 days after the first laparotomy, cecum was taken out, and the burst pressure or intracecal pressure (cmH2O) of the stump was measured. Group III did not undergo relaparotomy; the burst pressure of the stump was measured during the first laparotomy, and cecum was then removed and kept in 10% formalin for histopathological evaluation.
Histopathological evaluation
The fixed tissues were embedded in paraffin, and sectioned to 5 μm. Histological preparations were stained with hematoxylin and eosin and reviewed by a pathologist blinded to the groups.
Statistical analysis
All data were expressed as means ± standard deviation. Intracecal pressures were subjected to one-way analysis of variance for repeat measurement and statistical significance was determined by the least significant difference (LSD) post hoc test. Also, the chi-square test was used for the histopathological evaluation (SPSS 9.0 for Windows). Differences were considered significant for p values less than 0.05.
Results
All rats survived. On postoperative day 1, rats from both groups I and II tolerated oral feeding well. At relaparotomy, no complications were detected, including wound infection, volvulus, intestinal obstruction, abscess, and leakage.
Intracecal pressure
Although intracecal pressure increased to 30 cmH2O, at which pressure the cecum wall was highly stretched, ligated or coagulated stumps did not burst or open. In group III, the burst or opening pressure of the stump (11.2 ± 2.7 cmH2O) was significantly lower than in groups I and II (p < 0.001).
Histopathological evaluation
Under macroscopic examination, ligated stumps were detected to be overlaid with fatty tissue of uterus and omentum leaves, and a firm mass approximately 5 mm in diameter, while only fatty tissue of uterus was seen to adhere to the coagulated stumps.
Under microscopic examination (Table 1), while mild mucosal inflammation was seen in cecum in 20% of group I, mild mucosal inflammation combined with granulation tissue of cecum was observed in 70% of group I and 90% in group II.
The incidence of severe mucosal inflammation, necrosis, and granulation tissue was markedly lower in the coagulated stumps (group II) compared with the ligated stumps (Fig. 2) (p < 0.001). Unlike the ligated stumps, 80% of the coagulated stumps were completely covered by intestinal neomucosa (Fig. 3) (p < 0.001).
Discussion
In the past two decades, laparoscopic appendectomy has gained popularity and was the treatment of choice over the open technique because of its advantages such as less postoperative pain, earlier feeding, better cosmesis, shorter hospitalization, earlier return to normal activity and work, less incidence of wound infection, and less negative laparotomy [3–7]. Despite the standard technique of open appendectomy, different methods have been described for laparoscopic appendectomy; to date discussions about the advantages of these methods are ongoing, with each method aiming to eliminate intra- and postoperative morbidity, longer operative, time, and higher cost.
The most common technique known for laparoscopic appendectomy involves three trocars. However, the laparoscope-assisted two- or one-trocar technique is as safe as the open technique [9,14]. In fact, the size and number of trocars depend on the technique for controlling mesoappendix and appendeceal base. Cautery and/or clips can efficiently control the mesoappendix, and endoloops are mostly used for the appendeceal stump. In both adults and children, the endoscopic linear stapler has also been preferred to control the mesoappendix and base of the appendix, but it requires a 12 mm trocar [15]; despite not being cost effective, it has the advantages of speed and ability to control an inflamed appendeceal base more easily. Khanna et al. [13] reported a technique of laparoscopic appendectomy by bipolar coagulation in 60 patients; the technique was very simple and economical, and the duration of surgery was shorter than the standard technique of laparoscopic appendectomy; no clip applicators, needle holders or knot pushers were required, and no ligatures or clips were used. However, the efficacy and safety of this novel technique should be demonstrated experimentally before being commonly used. In the present experimental study, we evaluated the intracecal pressure or burst pressure of the stump and the histopathological characteristics of appendeceal bases closed only by bipolar coagulation. At 15 days after closure of the stumps, in spite of the high intracecal pressure of 30 cmH2O, at which the cecum wall was stretched as if being torn, neither the coagulated nor the ligated stumps opened or burst. On the other hand, we also measured the intracecal pressure just after closure with bipolar coagulation; the stumps burst at an average intracecal pressure of 11.2 ± 2.7 cmH2O. Khanna et al. [13] coagulated appendeceal specimens, which had been removed by the open method, with water pressure applied through the pressure infuser in the appendix; the intra-appendiceal pressure was up to 15 cmH2O. However, as mentioned above, we evaluated the intracecal or burst pressure of the stump in both the early and late period of closure.
At 15 days, no evidence of leakage from the ligated or coagulated stumps was observed. In the gross examination, a firm mass was seen at the ligated stump sites but not at the coagulated stumps. Microscopic examination supported this finding; severe mucosal inflammation, necrosis, and granulation tissue were marked in 90% of the ligated stumps. However, the course of wound healing was seen to be better in the coagulated stumps, which were completely covered by intestinal neomucosa. This result showed that the ligation was an unfavorable factor for epithelial healing of the stump.
The diameter of the normal appendix is commonly less than 1 cm; in a prospective study the mean diameter was reported to be 6.7 ± 1.2 mm [16]. In children, the mean diameter of the appendix is 0.39 cm [17]. On the other hand, appendicitis causes the appendeceal diameter to increase to 9–18 mm [18]. However, the diameter of inflammed appendix distal to the stump is somewhat greater than that of the stump just distal to the cecum. In this study, appendeceal stumps 1 cm in diameter were closed safely and easily by bipolar coagulation. In this context, further studies using experimental models of the noncomplicated and complicated appendicitis may be needed. However, this procedure was observed to be a safe and efficient method for complete closure of the appendeceal base, supporting Khanna’s report [13].
References
Andersen BR, Kallehave FL, Andersen HK (2001) Antibiotics versus placebo for prevention of postoperative infection after appendectomy. Cochrane Database Syst Rev CD001439
Anderson KD, Parry RL (1998) Appendicitis. In: O’Neill JA, Rowe MI, Grosfeld JL, Fonkalsrud EW, Coran AG (eds). Pediatric Surgery, Mosby, St. Louis, Missouri, pp 1369–1379
Bresciani C, Perez RO, Habr-Gama A, Jacob CE, Ozaki A, Batagello C, Proscurshim I, Gama-Rodrigues J (2005) Laparoscopic versus standard appendectomy outcomes and cost comparisons in the private sector. J Gastrointest Surg 9:1174–1180
Cox MR, McCall JL, Toouli J, Padbury RT, Wilson TG, Wattchow DA, Langcake M (1996) Prospective randomized comparison of open versus laparoscopic appendectomy in men. World J Surg 20:263–266
Frazee RC, Roberts JW, Symmonds RE, Snyder SK, Hendricks JC, Smith RW, Custer MD 3rd, Harrison JB (1994) A prospective randomized trial comparing open versus laparoscopic appendectomy. Ann Surg 219:725–728
Kum CK, Ngoi SS, Goh PM, Tekant Y, Isaac JR (1993) Randomized controlled trial comparing laparoscopic and open appendectomy. Br J Surg 80:1599–1600
Tate JJ, Dawson JW, Chung SC, Lau WY, Li AK (1993) Laparoscopic versus open appendectomy: Prospective randomized trial. Lancet 342:633–637
Cothren CC, Moore EE, Johnson JL, Moore JB, Ciesla DJ, Burch JM (2005) Can we afford to do laparoscopic appendectomy in an academic hospital? Am J Surg 190:950–954
Valioulis I, Hameury F, Dahmani L, Levard G (2001) Laparoscope-assisted appendectomy in children: the two-trocar technique. Eur J Pediatr Surg 11:391–394
Ng WT, Lee YK, Hui SK, Sze YS, Chan J, Zeng AG, Wong CH, Wong WH (2004)An optimal, cost-effective laparoscopic appendectomy technique for our surgical residents. Surg Laparosc Endosc Percutan Tech 14:125–129
Cristalli BG, Izard V, Jacob D, Levardon M (1991) Laparoscopic appendectomy using a clip applier. Surg Endosc 5:176–178
Klima S (1998) Importance of appendix stump management in laparoscopic appendectomy. Zentralbl Chir 123:90–93
Khanna S, Khurana S, Vij S (2004) No clip, no ligature laparoscopic appendectomy. Surg Laparosc Endosc Percutan Tech 14:201–203
Koontz CS, Smith LA, Burkholder HC, Higdon K, Aderhold R, Carr M (2006) Video-assisted transumbilical appendectomy in children. J Pediatr Surg 41:710–712
Ortega AE, Hunter JG, Peters JH, Swanstrom LL, Schirmer B (1995) A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy. Laparoscopic Appendectomy Study Group. Am J Surg 169:208–212
Huwart L, El Khoury M, Lesavre A, Phan C, Rangheard AS, Bessoud B, Menu Y (2007) What is the thickness of the normal appendix on MDCT? J Radiol 88:385–389
Wiersma F, Sramek A, Holscher HC (2005) US features of the normal appendix and surrounding area in children. Radiology 235:1018–1022
Yoshida H, Onda M, Tajiri T, Mamada Y, Taniai N, Koizumi M, Yoshimura K, Takasaki H, Furukawa K (2002) Ultrasonography of non-perforated appendicitis in young children. Hepatogastroenterology 49:1293–1295
Acknowledgments
The study was supported by Akdeniz University’s management unit of scientific research projects.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aslan, A., Karaveli, C. & Elpek, O. Laparoscopic appendectomy without clip or ligature. An experimental study. Surg Endosc 22, 2084–2087 (2008). https://doi.org/10.1007/s00464-007-9712-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9712-z