Abstract
Background/purpose
Anaplastic ganglioglioma (AGG) is a rare tumor with both glial and neuronal component accounting for less than 1% of all CNS tumors with limited information about the optimum treatment and outcome of these tumors.
Method and materials
We did a thorough search of the PubMed with the following MesH terms: “Ganglioglioma; Anaplastic ganglioglioma; Ganglioglioma AND treatment; and Anaplastic ganglioglioma AND survival” to find all possible publications related to AGG to perform an individual patient data analysis and derive the survival outcome and optimum treatment of these tumors.
Results
A total of 56 articles were retrieved pertaining to AGG with 88 patients. However, a total of 40 publications found eligible with 69 patients for individual patient data analysis. Median age for the entire cohort was 16 years (range 0.2–77 years). Surgical details were available for 64 patients. A gross total or near total resection was reported in 21 cases (32.8%), subtotal resection or debulking was reported in 25 cases (39.1%). Surgical details were available for 64 patients. A gross total or near total resection was reported in 21 cases (32.8%), and subtotal resection or debulking was reported in 25 cases (39.1%). Median overall survival (OS) was 29 months [95% CI 15.8–42.2 months] with 2- and 5-year OS 61 and 39.4% respectively.
Conclusion
AGG is associated with a dismal. Pediatric age and a gross total resection of tumor confer a better progression-free survival and OS. Hence, surgery should remain the cornerstone of therapy. However, because of modest survival, there is enough opportunity to improve survival with addition of adjuvant radiation and chemotherapy. A whole genome sequencing and molecular characterization would help to derive the best treatment option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ganglioglioma (GG) was first described in 1926 as a rare central nervous system tumor accounting for 0.4–1% of all brain tumors [1]. As the name suggests these tumors are composed of both ganglionic and glial component. GG have been described to arise from all part of the central nervous system but more commonly from the temporal lobe. These highly epileptogenic tumors are often diagnosed in young children and adults presenting with intractable epilepsy. Because of the indolent disease course, WHO has defined GG as grade I. However, these tumors sometimes show an aggressive clinical course and defined as anaplastic ganglioglioma (AGG) which are considered WHO grade III [2]. A surgical excision is considered standard of care for AGG and a maximal safe resection is the aim of surgery [3, 4]. However, even after a surgical complete tumor removal, many patients experience recurrence. Hence, many centers recommend adjuvant radiation or chemotherapy or a combination of both for optimizing tumor control and improve survival [4, 5]. Even after multimodality treatment survival is often poor. However, owing to the rarity of these tumors, most of the data is derived from institutional practice, case reports, or small case series with the limitation of wide range of bias. Hence, we embarked on to do an individual patient data analysis to find the optimum treatment of these tumors. So, the question we asked was “Whether adjuvant therapy has a role in the management of AGG.” We planned to derive basic patient characteristics, treatment details, and survival information from all published studies of AGG and analyzed the impact of treatment.
Search methodology
We did a thorough search of the PubMed with the following MesH terms: “Ganglioglioma; Anaplastic ganglioglioma; Ganglioglioma AND treatment; and Anaplastic ganglioglioma AND survival” to find all possible publications related to AGG. Once we identified the references, we went through all the abstracts to select the articles which have reported clinical information of AGG. After preliminary shortlisting the abstracts, we extracted full text of those articles and archived for data extraction. We also conducted a detail search of the references in the available article to retrieve missing articles and also conducted a hand search in Google to find any possible publication. After a thorough search, duplicates were removed and remaining articles were looked into detail. Individual patient data were tabulated in excel chart with the following headings: age, gender, surgery, type of surgery, radiation and type of radiation (local/craniospinal radiation), chemotherapy, recurrence, duration of disease-free interval, death, and overall survival. Articles which described about the pathological, molecular, and other factors only unrelated to treatment and outcome were excluded from the data extraction. After data extraction, the excel chart was reviewed by the authors independently to rule out any duplication. A total of 56 articles were retrieved pertaining to AGG with 88 patients. However, only 40 articles furnished adequate information related to 69 individual patients of AGG eligible for the present analysis. The PRISMA flow chart (Fig. 1) explains the data synthesis from the eligible studies.
Statistical analysis
The data were analyzed; categorical variables were summarized by frequency and percentage, and quantitative variables by the median and range. Progression-free survival [PFS] and overall survival [OS] was calculated from the date of diagnosis to the date of documented progression or death. Univariate analysis was performed using log-rank test to find the impact of prognostic variables on PFS and OS. The Kaplan-Meier method was used to for survival analysis (Fig. 2). Univariate analysis was done to find an impact of age, gender, type of surgery, use of radiation, and use of chemotherapy on survival outcome. A p value of < 0.05 was taken as significant. SPSS v16. (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, SPSS Inc.) was used for all statistical analysis.
Results
A total of 56 articles were retrieved pertaining to AGG with 88 patients. However, a total of 40 studies found eligible with 69 patients for individual patient data analysis [1, 4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]. Median age for the entire cohort was 16 years (range 0.2–77 years). Out of these 88 patients, 45 (51.1%) were found of the pediatric age group. Out of 88 patients, 43 were male and 33 female with a male:female ratio of 1.3:1, suggestive of a male preponderance; gender of 12 patients were not available. Presenting symptom was available in 56 patients; headache was the commonest symptom (37.5%) followed by seizure (34.6%). Tumor location was available for 65 patients, 53 intracranial, and 12 spinal lesions. The patients’ characteristics have been summarized in Table 1.
Surgical details were available for 64 patients. A gross total [GTR] or near total resection was reported in 21 cases (32.8%), and subtotal resection [STR] or debulking was reported in 25 cases (39.1%). Information regarding adjuvant radiation was available in 65 cases, whereas it was not clearly mentioned in 23 cases. Out of these 65 cases, radiation details were available for 17 cases. Local radiation was used in all 9 patients with available information of radiation volume. Information regarding use of chemotherapy was available for 53 cases only; out of these 53 patients, chemotherapy was used in 28 (52.8%).
A total of 20 patients experienced recurrence. Pattern of recurrence was predominantly local; however, two patients experienced a spinal dissemination, and one of these two patients had cervico-dorsal lesion and the other had right parieto-occipital lesion at the beginning. In addition, one patient with a frontal lesion experienced extracranial dissemination.
Survival outcome
After a median follow-up of 12 months (range 1–132 months), median PFS of the entire cohort was 24 months [95% CI 9.7–38.2 months]. Estimated 2- and 5-year PFS was 47.5 and 30% respectively. In univariate analysis, pediatric patients had median PFS of 34 months [95% CI 7.3–60.6 months] compared to 15 months [95% CI 9.8–20.2 months] for adult patients but failed to reach statistical significance. Patients undergoing a GTR were found to have better PFS [42 months, 95% CI 11.1–72.9 months] compared to those with a STR [9.2 months, 95% CI 0.0–30.1] without statistical significance Fig. 2. However, other factors like gender, use of adjuvant radiation, or chemotherapy were not found to have any impact on PFS.
Median OS was 29 months [95% CI 15.8–42.2 months] with 2- and 5-year OS 60 and 39.4% respectively. In univariate analysis, pediatric patients had median OS of 42 months [95% CI: NR] compared to 24 months [95% CI 20.4–27.6 months] with a trend towards statistical significance (p = 0.091). Patients undergoing a GTR were found to have significantly better OS [132 months, 95%: NR] compared to those with a STR [22 months, 95% CI 10.8–33.2] or those with an unknown surgical extent [34 months, 95% CI 14.4–53.6 months] (p = 0.008). Patients with tumor in cerebral hemisphere or single-lobe involvement had a better OS of 132 months [132 months, 95%: NR] compared to those with a multilobe involvement or disease in infratentorial and spinal location [34 months (95% CI 19.7–48.3 months); p = 0.032] (Fig. 3). However, other factors like gender, use of adjuvant radiation, or chemotherapy were not found to have any impact on OS.
Discussion
Gangliogliomas were described as a distinct entity in 1926 representing 0.4–1.0% of all brain tumors [1]. WHO has recognized ganglioglioma of two distinct grades depending of biology viz., ganglioglioma (grade I) and AGG (grade III) [2]. These tumors are composed of both glial as well as ganglionic component which arises from glioneuronal precursor cells and in few occasions de-differentiates to higher grade tumor. AGG is a rarer tumor of the GG group with more aggressive clinical and biological course than the other subtypes. The rarity of AGG is easily understandable by the fact that this comprehensive literature search could yield only 56 articles of AGG with 88 patients and only 40 studies with 69 patients were eligible for individual patient data analysis [1, 4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]. These tumors found mostly affecting children and young adults with reported median age of 25 years at diagnosis [3, 4]. In the present analysis, median age was 16 years (range 0.2–77 years) which shows a predilection of AGG in younger patients. This finding is further supported by our finding that nearly half of the patients are of pediatric age. Adding a new insight, we found patients of pediatric age group to have a better PFS [34 vs 15 months] and OS [42 vs 24 months, p = 0.091] but could not reach statistical significance because of small sample size. Though AGG is known to arise from any part of the central nervous system, temporal lobe has been reported to be the commonest location [3]. A SEER database analyses by Selvanathan et al. reported 27% patients to have temporal lesion followed by 22% in the frontal lobe. In the present analysis, also 21.5% patients had a temporal lesion followed closely by frontal lesion. Interestingly, the SEER report found only 8.2% patients with a spinal lesion, but in the present analysis, 18.5% patients were found to have a lesion in the spinal cord.
Though, an earlier report correlated better survival for patients with a frontal tumor and worse for temporal tumor, the present analysis could not make such an observation. However, the present analysis revealed better OS for patients with disease in cerebral parenchyma and single-lobe involvement compared to those with multilobe disease or infratentorial and spinal location. This may be because of ease of surgical resection in cerebral parenchymal disease or single-lobe involvement compared to spinal, infratentorial, or multilobe involvement. Location of the tumors correlates well with the presenting symptom as well with nearly one third patient presented with headache and seizure each which emphasizes the importance of keeping ganglioglioma as an important differential in younger patients presenting with seizure or headache.
Surgery plays pivotal role in symptom reduction and allows tissue diagnosis. A reliable diagnosis of ganglioglioma compared to AGG is of paramount importance as AGG is associated with a poorer survival outcome and merits a multidisciplinary adjuvant therapy for improving disease control and survival. In the present analysis, nearly one third patients underwent a gross total resection and another one third patients underwent a STR which can be because of eloquent tumor location. When we looked into the survival outcome, PFS was better for patients with a GTR [42vs 12 months] but failed to reach statistical significance. However, patients with a GTR had a significantly better OS [132 vs 22 months, p—0.008] compared to those with a STR or unknown surgical extent. This clearly emphasizes that surgery should be aimed at achieving a GTR whenever feasible without causing functional compromise and consolidates the observation of Selvanathan et al. and Terrier et al. of a better survival for patients undergoing a GTR compared to those with a STR [3, 4]. The importance of preoperative imaging also is crucial which should be able to derive important information regarding the tumor behavior and help to proceed with a GTR. The newer functional imaging, perfusion and diffusion images may be of great help in this regard. The higher grade and anticipated aggressive behavior of tumor help favorably to decide for adjuvant therapy for AGG across institutes. Because of lack of evidence, many institutes advocate the ongoing adjuvant treatment policy for other high-grade glial tumors for AGG as well. Hence, 75.4% patients received adjuvant radiation with a median dose of 56 Gy (range 40–66 Gy). Because of glial origin and predominantly arising from the cerebral parenchyma, a local radiation has been considered in the available literature. Liauw et al. reported better disease control in ganglioglioma when treated with adjuvant radiation after a STR. Terrier et al. reported a trend towards better survival for patients treated with adjuvant radiation [4]. In addition, the authors observed best survival outcome for patients treated with a GTR followed by adjuvant chemoradiotherapy further emphasizing the role of adjuvant therapy ever after a GTR. In addition to radiation, 52.8% patients in the present analysis received different forms of adjuvant chemotherapy. However, our analysis failed to elicit any advantage of adjuvant radiation and chemotherapy as well. But, note should be made of the fact that we are analyzing a rare disease where 71 patients data have been extracted from 42 studies. Hence, there is every possibility of different biases and errors which should be looked into carefully. The mode of diagnosis, quality of reporting of the histopathology, institutional practice, and patient preference bound to make important impact on the adjuvant treatment plan and outcome. In addition, most of the publications do not furnish much details of the salvage treatment which has an important role in such situation. The present analysis revealed a modest median PFS of 24 months [95% CI 9.7–38.2 months] and OS of 29 months [95% CI 15.8–42.2 months]. The survival outcomes are absolutely not different from the observation made by Selvanathan et al. and Terrier et al. depicting importance of more aggressive course of adjuvant therapy for these patients [3, 4]. Though the analysis failed to find an advantage of adjuvant radiation or chemotherapy, it appears reasonable to advocate at least radiation for those who had a GTR and adjuvant radiation and chemotherapy both for those with a STR or in disease at eloquent location [Fig. 4].
This analysis has many limitations. All the publications included in the analysis are retrospective that brings into question various sources of bias. All relevant data was not available which compelled analysis in limited samples for different parameters. But with such rare diseases like AGGs, it is difficult to get better quality data than this and a randomized controlled trial is not reasonable. The use of individual patient characteristics for analysis may be considered as one of the merits of this work.
Conclusion
AGG is associated with a dismal outcome with a median progression-free survival of 24 months and median overall survival of 29 months. Pediatric patients and patients with a gross total resection of tumor had a better PFS and OS. The role of adjuvant therapy remains unclear because of heterogeneity of practice and small patient number. Hence, a gross total resection should remain the aim of surgery, and adjuvant radiation and chemotherapy should be employed to improve the outcome of these patients. An across institutional pooling of data and detailed molecular analysis will further refine the treatment recommendation and survival.
References
Luyken C, Blümcke I, Fimmers R, Urbach H, Wiestler OD, Schramm J (2004) Supratentorial gangliogliomas: histopathologic grading and tumor recurrence in 184 patients with a median follow-up of 8 years. Cancer 101(1):146–155
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6):803–820
Selvanathan SK, Hammouche S, Salminen HJ, Jenkinson MD (2011) Outcome and prognostic features in anaplastic ganglioglioma: analysis of cases from the SEER database. J Neuro-Oncol 105(3):539–545
Terrier LM, Bauchet L, Rigau V, Amelot A, Zouaoui S, Filipiak I et al. (2017) Natural course and prognosis of anaplastic gangliogliomas: a multicenter retrospective study of 43 cases from the French Brain Tumor Database. Neuro Oncol 19(5):678–688
Liauw SL, Byer JE, Yachnis AT, Amdur RJ, Mendenhall WM (2007) Radiotherapy after subtotally resected or recurrent ganglioglioma. Int J Radiat Oncol Biol Phys 67(1):244–247
Lüdemann W, Banan R, Hartmann C, Bertalanffy H, Di Rocco C (2017) Pediatric intracranial primary anaplastic ganglioglioma. Childs Nerv Syst 33(2):227–231
Boissonneau S, Terrier LM, De La Rosa Morilla S, Troude L, Lavieille JP, Roche PH (2016) Cerebellopontine angle gangliogliomas: report of two cases. Neurochirurgie 62(5):266–270
Rusiecki D, Lach B, Manoranjan B, Fleming A, Ajani O, Singh SK (2017) Progression of atypical extraventricular neurocytoma to anaplastic ganglioglioma. Hum Pathol 59:125–130
Zanello M, Pages M, Tauziède-Espariat A, Saffroy R, Puget S, Lacroix L, Dezamis E, Devaux B, Chrétien F, Andreiuolo F, Sainte-Rose C, Zerah M, Dhermain F, Dumont S, Louvel G, Meder JF, Grill J, Dufour C, Pallud J, Varlet P (2016) Clinical, imaging, histopathological and molecular characterization of anaplastic ganglioglioma. J Neuropathol Exp Neurol 75(10):971–980
Gessi M, Dörner E, Dreschmann V, Antonelli M, Waha A, Giangaspero F, Gnekow A, Pietsch T (2016) Intramedullary gangliogliomas: histopathologic and molecular features of 25 cases. Hum Pathol 49:107–113
Lucas JT Jr, Huang AJ, Mott RT, Lesser GJ, Tatter SB, Chan MD (2015) Anaplastic ganglioglioma: a report of three cases and review of the literature. J Neuro-Oncol 123(1):171–177
Daou B, Zanello M, Varlet P, Brugieres L, Jabbour P, Caron O, Lavoine N, Dhermain F, Willekens C, Beuvon F, Malka D, Lechapt-Zalcmann E, Abi Lahoud G (2015) An unusual case of constitutional mismatch repair deficiency syndrome with anaplastic ganglioglioma, colonic adenocarcinoma, osteosarcoma, acute myeloid leukemia, and signs of neurofibromatosis type 1: case report. Neurosurgery 77(1):E145–E152
Schneider C, Vosbeck J, Grotzer MA, Boltshauser E, Kothbauer KF (2012) Anaplastic ganglioglioma: a very rare intramedullary spinal cord tumor. Pediatr Neurosurg 48(1):42–47
Yust-Katz S, Anderson MD, Liu D, Wu J, Yuan Y, Olar A, Fuller GN, Brown PD, de-Groot JF (2014) Clinical and prognostic features of adult patients with gangliogliomas. Neuro-Oncology 16(3):409–413
Atabey C, Eroglu A, Dinc C, Colak A (2013) Ganglioglioma mimicking the cerebral abscess in advanced age: a case report. Turk Neurosurg 23(4):557–560
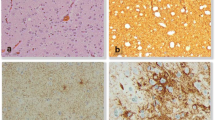
Romero-Rojas AE, Diaz-Perez JA, Chinchilla-Olaya SI, Amaro D, Lozano-Castillo A, Restrepo-Escobar LI (2013) Histopathological and immunohistochemical profile in anaplastic gangliogliomas. Neurocirugia (Astur) 24(6):237–243
Kuten J, Kaidar-Person O, Vlodavsky E, Postovsky S, Billan S, Kuten A, Bortnyak-Abdah R (2012) Anaplastic ganglioglioma in the spinal cord: case report and literature review. Pediatr Neurosurg 48(4):245–248
Reis F, Vieira GH, Schwingel R, Gonçalves VT, Queiroz Lde S (2012) Ganglioglioma with anaplastic transformation. Arq Neuropsiquiatr 70(9):746–747
Scoccianti S, Giordano F, Agresti B, Detti B, Cipressi S, Franceschini D, Greto D, Mussa F, Sardi I, Buccoliero A, Aricò M, Genitori L, Biti G (2012) Pediatric primary anaplastic ganglioglioma: a case report and review of the literature. Pediatr Neurosurg 48(1):35–41
González Toledo E, Nader M, Thomas-Ogunniyi J, Wilson J (2012) Anaplastic ganglioglioma of the brainstem in an adult. Neuroradiol J 25(3):325–329
DeMarchi R, Abu-Abed S, Munoz D, Loch Macdonald R (2011) Malignant ganglioglioma: case report and review of literature. J Neuro-Oncol 101(2):311–318
Shah MJ, Sircar R, Linder-Luch M, Böhm J, Vv V-W, Vv V-W (2012) Anaplastic posterior fossa ganglioglioma in a child: case report and short review of the literature. J Neurol Surg A Cent Eur Neurosurg 73(1):46–49
Kawataki T, Sato E, Sato T, Kinouchi H (2010) Anaplastic ganglioglioma with malignant features in both neuronal and glial components—case report. Neurol Med Chir (Tokyo) 50(3):228–231
Zhi L, Yang L, Quan H, Bo-Ning L, Ying-Jie L (2009) Anaplastic ganglioglioma with gliosarcoma component. Pathology 41(6):590–593
Karremann M, Pietsch T, Janssen G, Kramm CM, Wolff JE (2009) Anaplastic ganglioglioma in children. J Neuro-Oncol 92(2):157–163
Majores M, von Lehe M, Fassunke J, Schramm J, Becker AJ, Simon M (2008) Tumor recurrence and malignant progression of gangliogliomas. Cancer 113(12):3355–3363
Takei H, Dauser R, Su J, Chintagumpala M, Bhattacharjee MB, Jones J et al (2007) Anaplastic ganglioglioma arising from a Lhermitte-Duclos-like lesion. Case report. J Neurosurg 107(2 Suppl):137–142
Schittenhelm J, Reifenberger G, Ritz R, Nägele T, Weller M, Pantazis G, Capper D, Beschorner R, Meyermann R, Mittelbronn M (2008) Primary anaplastic ganglioglioma with a small-cell glioblastoma component. Clin Neuropathol 27(2):91–95
Kang DH, Lee CH, Hwang SH, Park IS, Han JW, Jung JM (2007) Anaplastic ganglioglioma in a middle-aged woman: a case report with a review of the literature. J Korean Med Sci 22(Suppl):S139–S144
Chrétien F, Djindjian M, Caramelle P, Ricolfi F, Christov C (2007) A 42-year-old man with a densely vascular spinal mass. Brain Pathol 17(1):119–121
Karabekir HS, Balci C, Tokyol C (2006) Primary spinal anaplastic ganglioglioma. Pediatr Neurosurg 42(6):374–378
Mekni A, Chelly I, Haouet S, Zitouna M, Kchir N (2006) Malignant cerebellar ganglioglioma. A case report and review of the literature. Neurochirurgie 52(2–3 Pt 1):119–122
Matsuzaki K, Uno M, Kageji T, Hirose T, Nagahiro S (2005) Anaplastic ganglioglioma of the cerebellopontine angle. Case report. Neurol Med Chir (Tokyo) 45(11):591–595
Suzuki H, Otsuki T, Iwasaki Y, Katakura R, Asano H, Tadokoro M, Suzuki Y, Tezuka F, Takei H (2002) Anaplastic ganglioglioma with sarcomatous component: an immunohistochemical study and molecular analysis of p53 tumor suppressor gene. Neuropathology 22(1):40–47
Danjoux M, Sabatier J, Uro-Coste E, Roche H, Delisle MB (2001) Anaplastic temporal ganglioglioma with spinal metastasis. Ann Pathol 21(1):55–58
Takano S (2000) Anaplastic ganglioglioma. Ryoikibetsu Shokogun Shirizu (28 Pt 3):84–6
Kurian NI, Nair S, Radhakrishnan VV (1998) Anaplastic ganglioglioma: case report and review of the literature. Br J Neurosurg 12(3):277–280
Araki M, Fan J, Haraoka S, Moritake T, Yoshii Y, Watanabe T (1999) Extracranial metastasis of anaplastic ganglioglioma through a ventriculoperitoneal shunt: a case report. Pathol Int 49(3):258–263
Dash RC, Provenzale JM, McComb RD, Perry DA, Longee DC, McLendon RE (1999) Malignant supratentorial ganglioglioma (ganglion cell-giant cell glioblastoma): a case report and review of the literature. Arch Pathol Lab Med 123(4):342–345
Nakajima M, Kidooka M, Nakasu S (1998) Anaplastic ganglioglioma with dissemination to the spinal cord: a case report. Surg Neurol 49(4):445–448
Hirose T, Scheithauer BW, Lopes MB, Gerber HA, Altermatt HJ, VandenBerg SR (1997) Ganglioglioma: an ultrastructural and immunohistochemical study. Cancer 79(5):989–1003
Hakim R, Loeffler JS, Anthony DC, Black PM (1997) Gangliogliomas in adults. Cancer 79(1):127–131
Demaerel P, Droessaert M, Lammens M, Menten J, Nuttin B, Verbeeck R, Wilms G, Baert AL (1996) Anaplastic (malignant) ganglioglioma arising from heterotopic grey matter nodules. J Neuro-Oncol 30(3):237–242
Sasaki A, Hirato J, Nakazato Y, Tamura M, Kadowaki H (1996) Recurrent anaplastic ganglioglioma: pathological characterization of tumor cells. Case report. J Neurosurg 84(6):1055–1059
Kroh H (1992) Anaplastic temporal lobe ganglioglioma. Case report. Neuropatol Pol 30(3–4):315–323
Campos MG, Zentner J, Ostertun B, Wolf HK, Schramm J (1994) Anaplastic ganglioglioma: case report and review of the literature. Neurol Res 16(4):317–320
Chintagumpala MM, Armstrong D, Miki S, Nelson T, Cheek W, Laurent J, Woo S, Mahoney DH Jr (1996) Mixed neuronal-glial tumors (gangliogliomas) in children. Pediatr Neurosurg 24(6):306–313
Krouwer HG, Davis RL, McDermott MW, Hoshino T, Prados MD (1993) Gangliogliomas: a clinicopathological study of 25 cases and review of the literature. J Neuro-Oncol 17(2):139–154
Allegranza A, Pileri S, Frank G, Ferracini R (1990) Cerebral ganglioglioma with anaplastic oligodendroglial component. Histopathology 17(5):439–441
Kitano M, Takayama S, Nagao T, Yoshimura O (1987) Malignant ganglioglioma of the spinal cord. Acta Pathol Jpn 37(6):1009–1018
Hall WA, Yunis EJ, Albright AL (1986) Anaplastic ganglioglioma in an infant: case report and review of the literature. Neurosurgery 19(6):1016–1020
Blümcke I, Wiestler OD (2002) Gangliogliomas: an intriguing tumor entity associated with focal epilepsies. J Neuropathol Exp Neurol 61(7):575–584
Tamiya T, Hamazaki S, Ono Y, Tokunaga K, Matsumoto K, Furuta T, Ohmoto T (2000) Ganglioglioma in a patient with Turcot syndrome. Case report. J Neurosurg 92(1):170–175
Zorlu F, Selek U, Onal C, Söylemezoğlu F, Gurkaynak M (2006) Postoperative radiotherapy in cranial ganglioglioma. J Neuro-Oncol 77(3):321–324
Wacker MR, Cogen PH, Etzell JE, Daneshvar L, Davis RL, Prados MD (1992) Diffuse leptomeningeal involvement by a ganglioglioma in a child. Case report. J Neurosurg 77(2):302–306
Rodewald L, Miller DC, Sciorra L, Barabas G, Lee ML (1987) Central nervous system neoplasm in a young man with Martin-Bell syndrome--fra(X)-XLMR. Am J Med Genet 26(1):7–12
Haddad SF, Moore SA, Menezes AH, JC VG (1992) Ganglioglioma: 13 years of experience. Neurosurgery 31(2):171–178
Isimbaldi G, Sironi M, Tonnarelli GP, Roncoroni M, Declich P, Galli C (1996) Ganglioglioma: a clinical and pathological study of 12 cases. Clin Neuropathol 15(4):192–199
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mallick, S., Benson, R., Melgandi, W. et al. Impact of surgery, adjuvant treatment, and other prognostic factors in the management of anaplastic ganglioglioma. Childs Nerv Syst 34, 1207–1213 (2018). https://doi.org/10.1007/s00381-018-3780-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3780-3