Abstract
Purpose
The aim of this study was to report the outcome in children with high-grade astrocytoma outside the brain stem and spinal cord that were treated at a single center.
Materials and methods
The study included 26 patients with anaplastic astrocytoma and 37 patients with glioblastoma; all patients were aged ≤18 years. At initial diagnosis, 18 of the patients with glioblastoma received only temozolomide (TMZ), 14 received other chemotherapies, and 5 did not receive any chemotherapy. Among the patients with anaplastic astrocytoma, 9 received TMZ, 9 received other chemotherapy regimens, and 8 patients did not receive any chemotherapy. The median radiotherapy dose in all patients was 60 Gy.
Results
Median age of the patients was 12.5 years. Median overall survival was 20 months and mean progression-free survival was 4.7–11.3 months (median: 8 months) in all patients. Patients with a Karnofsky performance score (KPS) ≥70 had median overall survival of 32 months, versus 7 months in those with a KPS < 70. Patients aged <15 years had median survival of 38 months, versus 16 months in those aged 15–18 years. Patients with anaplastic astrocytoma that received TMZ, other chemotherapy regimens, and no chemotherapy had median survival of 21 months, 132 months, and 11 months, respectively. Patients with glioblastoma that received TMZ, other chemotherapy regimens, and no chemotherapy had median survival of 32 months, 12 months, and 8 months, respectively.
Conclusion
In the present study, patients with anaplastic astrocytoma treated with chemotherapy protocols other than TMZ had the longest OS; however, in the glioblastoma group, OS was 32 months in those treated with standard TMZ and 12 months in those treated with other protocols (P = 0.493). Although TMZ is less toxic than PCV, it was not shown to be superior.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Astrocytomas account for 40–50 % of central nervous system tumors in children [1]. WHO grade III and IV lesions are considered high grade [2]. In contrast to adults, high-grade astrocytomas are relatively rare in children, and supratentorial high-grade lesions constitute 10 % of brain tumors in children. The outcome in children treated for anaplastic astrocytoma or glioblastoma is poor, with 5-year progression-free survival (PFS) of 23 and 16 %, respectively [3].
High-grade gliomas in adults and children differ in the rate of occurrence and in response to chemotherapy. Sposto et al. [4] reported that chemotherapy consisting of vincristine (VCR), lomustine (CCNU), and prednisone (PCV) prolonged event-free survival (EFS) and overall survival (OS) rates compared to standard surgery and radiotherapy, especially in children with glioblastoma. On the other hand, the only agent that resulted in prolonging survival in adults is temozolomide (TMZ) used in concomitant and adjuvant settings [5]. The role of TMZ in pediatric patients remains to be elucidated.
The behavior of high-grade astrocytomas and the prognostic factors are not fully known in children because of their rarity. The aim of the present study was to report the outcome in children and adolescents diagnosed with high-grade astrocytoma outside the brain stem and spinal cord; prognostic factors and the effect of different chemotherapy protocols on outcome were evaluated.
Materials and methods
A search of the database of Hacettepe University, Department of Radiation Oncology, Ankara, Turkey, was performed to identify patients aged ≤18 years that were diagnosed as anaplastic astrocytoma and glioblastoma between February 1994 and August 2012. The present retrospective study was approved by the institutional ethics committee. In all, 63 patients that were treated for high-grade astrocytomas (anaplastic astrocytoma group: n = 26; glioblastoma group: n = 37) were included in this study.
Clinical and radiological data, including age, Karnofsky performance score (KPS), symptoms at presentation, tumor localization, extent of surgery, pathological findings, and radiotherapy and chemotherapy details, were recorded. Resection of >90 % of a lesion based on the surgery notes was defined as gross total resection (GTR). Subtotal resection was defined as removal of 50–90 % of a lesion, and resection of <50 % of tumor volume was defined as biopsy. Subtotal resection and biopsy were regarded as partial resection and grouped as other surgery in the analysis.
Radiotherapy was administered using 3-D conformal planning in all patients. Gross tumor volume (GTV) was defined based on postoperative MRI. Residual disease noted via T1 post-contrast images and the postoperative cavity were delineated as GTV. Clinical target volume-1 (CTV) was defined as GTV + 2.5 cm. Patients with CTV-1 were scheduled to receive 40 Gy in 20 fractions. After 40 Gy, the treatment field size was reduced. CTV-2 was defined as GTV + 1 cm, and patients with CTV-2 were administered 54–60 Gy.
Patients that received cisplatin + etoposide, or procarbazine, N-(2-chloroethyl)-N’-cyclohexyl-N-nitrosurea, and vincristine (PCV) were grouped together as protocol 1. Patients that received concomitant TMZ and adjuvant cisplatin + etoposide were grouped as protocol 2. Patients that received concomitant and adjuvant TMZ were grouped as protocol 3. Patients were assessed weekly for hematological toxicity during chemoradiotherapy. Following radiotherapy, patients were followed monthly via medical history and physical examination, and MRI was performed every 3 months for evaluation of treatment response.
Statistical analysis
Descriptive data are presented as median (range) or n (%), as appropriate. Time-to-event data analysis was performed using the Kaplan-Meier method. OS was calculated as the time from diagnosis to death due to any cause. PFS was defined as the time from the end of radiotherapy to progression of disease or death due to any cause. The Mantel-Cox test was used to compare survival distribution between independent groups. Cox proportional hazard regression analysis was used to identify independent prognostic factors for survival in the study group, and the hazard ratio of the tested variable was defined as relative risk. Survival data are presented as 1-year, 2-year, and 5-year survival probability and median survival time (standard error, 95 % CI). The type-1 error level was considered as 5 % for all statistical analyses.
Results
This study included 63 patients: 26 (41 %) with anaplastic astrocytoma and 37 (59 %) with glioblastoma. Median age in the anaplastic astrocytoma group (69 % male and 31 % female) was 14 years (range: 5–18 years), versus 12 years (range: 4–18 years) in the glioblastoma group (54 % male and 46 % female). The prominent complaint at admission in both groups was seizures. Median follow-up time was 16 months (range: 2.8–229.6 months). Basic demographic characteristics of the patients are shown in Table 1.
Most tumors were located supratentorially in both groups (anaplastic astrocytoma group: 81 %; glioblastoma group: 89 %) but differed in location according to depth. Twenty-nine patients underwent GTR. GTR of the lesions was performed in 42 % of the anaplastic astrocytoma group and 49 % of the glioblastoma group. In total, 42 % of the anaplastic astrocytoma group received TMZ in their chemotherapy regimen, versus 54 % of the glioblastoma group. The overall mortality rate in the anaplastic astrocytoma and glioblastoma groups was 58 and 76 %, respectively. The progression rate was 88 % in the anaplastic astrocytoma group and 87 % in glioblastoma group. Disease-specific characteristics of the patients are summarized in Table 2.
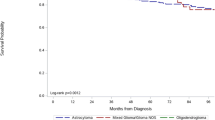
Median OS was 20.2 months in the entire study group, and the 1-year survival rate was 60 %, which decreased to 26 % through the fifth year of follow-up (Fig. 1). When survival rates were compared according to clinical characteristics, it was observed that anaplastic astrocytoma histology, KPS ≥ 70, GTR, and chemotherapy were favorable prognostic factors. Descriptive analysis and comparison of survival data are shown in Table 3.
When survival was analyzed separately for each group, KPS, age, and surgery were observed to be factors that were associated with survival in the anaplastic astrocytoma group. Chemotherapy, in addition to KPS, age, and surgery, were associated with survival in the glioblastoma group. In the glioblastoma group, patients that received standard TMZ had a median OS of 32.4 months, whereas, median OS in those that received protocol-1 and protocol-2 was 12 and 12.5 months, respectively (P = 0.474). Adjusted survival comparison according to tumor histology showed that chemotherapy, KPS, age, and surgery were associated with survival regardless of the diagnosis. Stratified survival data and adjusted comparisons are shown in Table 4.
After determining the clinical parameters that had an effect on survival, multivariate Cox proportional hazard regression analysis was used to identify independent prognostic factors. A model was built for histologic diagnosis, KPS group, age group, surgery type, and chemotherapy regimen. The final model included KPS and surgery type; variables with a P value >0.10 were excluded (histology, age, and chemotherapy) (Figs. 2 and 3). A KPS < 70 was associated with a 5.61-fold higher mortality risk than a KPS ≥ 70, and surgery other than GTR was associated with a 2.30-fold higher mortality risk.
PFS was 8.4 months in the entire study group, versus 14.3 and 5.0 months in the anaplastic astrocytoma and glioblastoma groups, respectively. Although there was not a significant difference in PFS between the 2 groups, the difference was concluded to be clinically significant. The only factor that was associated with PFS was the KPS. Patients with a KPS ≥ 70 had a mean PFS of 9.4 months, whereas those with a KPS < 70 had a mean PFS of 2.8 months (P < 0.001).
In total, 49 patients received a total dose of 60 Gy, 2 patients who were 4 and 5 years old at the time of radiotherapy received 54 Gy, and 12 patients with ages >5 years and ≤9 years old received 56 Gy. Total hearing loss occurred in 2 patients treated with cisplatin + etoposide, of which 1 received 56 Gy and 1 received 60 Gy with cochlea doses ≥54 Gy. In all, 5 patients developed pituitary insufficiency during post-treatment follow-up.
Discussion
The present retrospective study analyzed the outcome in 26 patients with anaplastic astrocytoma and 37 with glioblastoma treated at a single center. Studies on glioblastoma in children report that there is a predilection for the second decade of life (mostly 11–13 years old). In accordance with the literature, median age of the present study’s patients was 12.5 years. Age has been suggested to be a good prognostic factor in adult glioblastoma patients; however, it remains unclear if the prognosis of glioblastoma in children is better than that in adults [6, 7]. Song et al. [8] reported that median OS was 43 months in children, whereas others reported that OS in children was similar to that in the adult population [7]. Median OS in the present study’s glioblastoma group was 12 months, which is similar to that in the adult population [5]; however, OS was significantly longer in patients in the anaplastic astrocytoma group aged <15 years.
Preoperative performance status is a strong prognostic factor in adults. Das et al. [9] reported that KPS is also a prognostic factor in children. Patients in the present study with a KPS ≥ 70 had significantly longer OS. It was observed that a KPS < 70 was associated with a 5.6-fold higher mortality risk than a KPS ≥ 70. In addition to survival, KPS was also associated with PFS; patients with a KPS ≥ 70 had a significantly longer PFS.
The strongest indicator for prognosis is reported to be the extent of resection, with a 5-year OS of 63 % ± 12 % in children that undergo GTR [10]. Sanchez-Herrera et al. [11] studied 16 pediatric cases of glioblastoma and reported that the extent of resection correlated with survival. Perkins et al. [12] reported that the extent of resection was the only prognostic factor associated with prolonged survival in children. Likewise, patients in the present study that underwent GTR had significantly longer OS than patients with partial resection, regardless of group. Additionally, it was observed that undergoing surgery other than GTR was associated with a 2.3-fold higher mortality risk than undergoing GTR.
Addition of chemotherapy (PCV/CCNU/vincristine [pCV]) to radiotherapy resulted in prolonged EFS in children with high-grade astrocytoma, as compared to radiotherapy alone; the difference was greatest in children with glioblastoma [4]. In the CCG-945 [13] study, a more intensive chemotherapy regimen (8-in-1) was compared to the PCV regimen and the results showed that there was not a significant benefit associated with the 8-in-1 regimen. Numerous retrospective and prospective trials with adults failed to show any clinical benefit of chemotherapy in patients with glioblastoma, until the Stupp trial [5]. After that trial, TMZ concomitant with radiotherapy and followed by adjuvant treatment become the standard treatment protocol. In the ACNS0126 [14] study, the Children’s Oncology Group (COG) evaluated the efficacy of TMZ in children and the association between MGMT expression and outcome [14]. In all, 31 patients with anaplastic astrocytoma and 55 patients with glioblastoma were evaluated. The 3-year EFS rate was 7 % ± 4 % in the glioblastoma group and 13 % ± 6 % in the anaplastic astrocytoma group. They compared their results to those of the CCG-945 study and reported that there was not a significant difference. They concluded that TMZ did not result in improved outcome in children with high-grade glioma, as compared to the treatment provided in the CCG-945 study, but that TMZ was less toxic. Cohen et al. [14] thoroughly evaluated the differences between the Stupp trial in adults and their study. They concluded that their study showed that TMZ in pediatric patients with brain tumors was not inferior to other chemotherapeutic agents [14, 15]. Jung et al.’s [16] study included 35 patients (median age: 13 years) with high-grade glioma that were treated with TMZ. Among the patients, 17 had glioblastoma and 18 had anaplastic histology. In all, 22 patients received TMZ for initial treatment and 13 received it following recurrence. They reported that median OS was 15 months in the glioblastoma patients, versus 25 months in the patients with anaplastic histology.
In the present study, patients with anaplastic astrocytoma treated with chemotherapy protocols other than TMZ had the longest OS; however, in the glioblastoma group, OS was 32 months in those treated with standard TMZ and 12 months in those treated with other protocols (P = 0.493). Although TMZ is less toxic than PCV, it was not shown to be superior. As a result, it is not the standard treatment in children with glioblastoma. Besides its retrospective nature, the major pitfall of this study is the lack of information on the methylation status and 1p19q deletions. However, we think that the observed clinically important survival advantage of TMZ should be the basis for further studies of TMZ in children with glioblastoma.
References
Baldwin RT, Preston-Martin S (2004) Epidemiology of brain tumors in childhood—a review. Toxicol Appl Pharmacol 199(2):118–131. doi:10.1016/j.taap.2003.12.029
Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC, Cavenee WK (2002) The WHO classification of tumors of the nervous system. J Neuropathol Exp Neurol 61(3):215–225 discussion 226-219
Finlay JL, Boyett JM, Yates AJ, Wisoff JH, Milstein JM, Geyer JR, Bertolone SJ, McGuire P, Cherlow JM, Tefft M, et al. (1995) Randomized phase III trial in childhood high-grade astrocytoma comparing vincristine, lomustine, and prednisone with the eight-drugs-in-1-day regimen. Childrens Cancer Group. J Clin Oncol Off J Am Soc Clin Oncol 13(1):112–123
Sposto R, Ertel IJ, Jenkin RD, Boesel CP, Venes JL, Ortega JA, Evans AE, Wara W, Hammond D (1989) The effectiveness of chemotherapy for treatment of high grade astrocytoma in children: results of a randomized trial: a report from the Childrens Cancer Study Group. J Neuro-Oncol 7(2):165–177
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996. doi:10.1056/NEJMoa043330
Pollack IF, Hamilton RL, Burnham J, Holmes EJ, Finkelstein SD, Sposto R, Yates AJ, Boyett JM, Finlay JL (2002) Impact of proliferation index on outcome in childhood malignant gliomas: results in a multi-institutional cohort. Neurosurgery 50(6):1238–1244 discussion 1244-1235
Ansari M, Nasrolahi H, Kani AA, Mohammadianpanah M, Ahmadloo N, Omidvari S, Mosalaei A (2012) Pediatric glioblastoma multiforme: a single-institution experience. Indian J Med Paediatr Oncol Off J Indian Soc Med Paediatr Oncol 33(3):155–160. doi:10.4103/0971-5851.103142
Song KS, Phi JH, Cho BK, Wang KC, Lee JY, Kim DG, Kim IH, Ahn HS, Park SH, Kim SK (2010) Long-term outcomes in children with glioblastoma. J Neurosurg Pediatr 6(2):145–149. doi:10.3171/2010.5.PEDS09558
Das KK, Mehrotra A, Nair AP, Kumar S, Srivastava AK, Sahu RN, Kumar R (2012) Pediatric glioblastoma: clinico-radiological profile and factors affecting the outcome. Child’s Nerv Syst ChNS: Off J Int Soc Pediatr Neurosurg 28(12):2055–2062. doi:10.1007/s00381-012-1890-x
Wolff JE, Driever PH, Erdlenbruch B, Kortmann RD, Rutkowski S, Pietsch T, Parker C, Metz MW, Gnekow A, Kramm CM (2010) Intensive chemotherapy improves survival in pediatric high-grade glioma after gross total resection: results of the HIT-GBM-C protocol. Cancer-Am Cancer Soc 116(3):705–712. doi:10.1002/cncr.24730
Sanchez-Herrera F, Castro-Sierra E, Gordillo-Dominguez LF, Vaca-Ruiz MA, Santana-Montero B, Perezpena-Diazconti M, Gonzalez-Carranza V, Torres-Garcia S, Chico-Ponce de Leon F (2009) Glioblastoma multiforme in children: experience at Hospital Infantil de Mexico Federico Gomez. Child’s Nerv Syst ChNS: Off J Int Soc Pediatr Neurosurg 25(5):551–557. doi:10.1007/s00381-008-0780-8
Perkins SM, Rubin JB, Leonard JR, Smyth MD, El Naqa I, Michalski JM, Simpson JR, Limbrick DL, Park TS, Mansur DB (2011) Glioblastoma in children: a single-institution experience. Int J Radiat Oncol Biol Phys 80(4):1117–1121. doi:10.1016/j.ijrobp.2010.03.013
Grovas AC, Boyett JM, Lindsley K, Rosenblum M, Yates AJ, Finlay JL (1999) Regimen-related toxicity of myeloablative chemotherapy with BCNU, thiotepa, and etoposide followed by autologous stem cell rescue for children with newly diagnosed glioblastoma multiforme: report from the Children’s Cancer Group. Med Pediatr Oncol 33(2):83–87
Cohen KJ, Pollack IF, Zhou T, Buxton A, Holmes EJ, Burger PC, Brat DJ, Rosenblum MK, Hamilton RL, Lavey RS, Heideman RL (2011) Temozolomide in the treatment of high-grade gliomas in children: a report from the Children’s Oncology Group. Neuro-Oncology 13(3):317–323. doi:10.1093/neuonc/noq191
Broniscer A, Chintagumpala M, Fouladi M, Krasin MJ, Kocak M, Bowers DC, Iacono LC, Merchant TE, Stewart CF, Houghton PJ, Kun LE, Ledet D, Gajjar A (2006) Temozolomide after radiotherapy for newly diagnosed high-grade glioma and unfavorable low-grade glioma in children. J Neuro-Oncol 76(3):313–319. doi:10.1007/s11060-005-7409-5
Jung TY, Kim CY, Kim DS, Ra YS, Kim SH, Baek HJ, Choi HS, Kim IA (2012) Prognosis of pediatric high-grade gliomas with temozolomide treatment: a retrospective, multicenter study. Child’s Nerv Syst ChNS: Off J Int Soc Pediatr Neurosurg 28(7):1033–1039. doi:10.1007/s00381-012-1786-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
The authors declare there are no actual or potential conflicts of interest—financial or otherwise—relevant to the material presented herein.
Rights and permissions
About this article
Cite this article
Yazici, G., Zorlu, F., Cengiz, M. et al. High-grade glioma in children and adolescents: a single-center experience. Childs Nerv Syst 32, 291–297 (2016). https://doi.org/10.1007/s00381-015-2980-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2980-3