Abstract
Introduction
We performed this study to identify the treatment patterns of patients with low-grade gliomas (LGG) in Korea.
Methods
A total of 555 patients diagnosed as WHO grade II gliomas between 2000 and 2010 at 14 Korean institutions were included. The patients were divided into four adjuvant treatment groups: adjuvant fractionated radiotherapy (RT, N = 204), adjuvant chemotherapy (N = 20), adjuvant fractionated RT and chemotherapy (N = 65), and non-adjuvant treatment (N = 266) groups. We examined differences among the groups and validated patient/tumor characteristics associated with the adjuvant treatments.
Results
Astrocytoma was diagnosed in 210 patients (38%), oligoastrocytoma in 85 patients (15%), and oligodendroglioma in 260 patients (47%). Gross total resection was performed in 200 patients (36%), subtotal resection in 153 (28%), partial resection in 71 patients (13%), and biopsy in 131 patients (24%). RT was most commonly applied as an adjuvant treatment. The use of chemotherapy with or without RT decreased after 2008 (from 38 to 4%). The major chemotherapeutic regimen was procarbazine, lomustine, and vincristine (PCV); however, the proportion of temozolomide increased since 2005 (up to 69%). Patient/tumor characteristics related with RT were male gender, non-seizure, multiple lobes involvement, and non-gross total resection. Chemotherapy was associated with non-gross total resection and non-astrocytoma.
Conclusions
A preference for RT and increased use of temozolomide was evident in the treatment pattern of LGG. The extent of resection was associated with a decision to perform RT and chemotherapy. To establish a robust guideline for LGG, further studies including molecular information are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low-grade glioma (LGG) including astrocytoma, oligodendroglioma, and oligoastrocytoma are classified as World Health Organization (WHO) grade II tumors [1]. LGG is an uncommon disease, which accounts for about 20% of gliomas [2, 3]. It displays slow progression and a wide spectrum of clinical presentations ranging from no symptoms to neurological dysfunction. Because of these disease characteristics, only a limited number of clinical trials of LGG have performed. Consequently, no clear clinical guideline has been formulated. The European Association for Neuro-Oncology (EANO) recently reported a guideline for adult gliomas encompassing histological classification and molecular diagnostics [4]. However, adjuvant treatment options for WHO grade II gliomas are still ambiguous, and comprise watch-and-wait or radiotherapy (RT) followed by chemotherapy. Clinicians should have made treatment decisions based on well-known prognostic factors, such as surgical extent, age, astrocytoma histology, maximal diameter, or neurologic symptoms [5, 6].
The mainstay treatment for LGG is maximal safe resection of tumor. There is some level I evidence concerning adjuvant treatment for LGG. Adjuvant RT can improve progression-free survival compared with salvage RT, but with no impact on overall survival [7]. The combination of RT and chemotherapy has a survival benefit compared with RT alone [6]. It is not clear, however, whether chemotherapy can substitute for RT [8], or which chemotherapy regimen is optimal, i.e. procarbazine, lomustine, and vincristine (PCV) versus temozolomide (TMZ).
As LGG is entering a new era of molecular diagnosis, a study investigating treatment patterns according to histologic diagnosis could provide an opportunity to review our practice and find better treatment options. No study has reported treatment patterns of LGG in Korea. The purpose of this study was to analyze the treatment of patients with the WHO grade II gliomas and to clarify the patient/tumor characteristics associated with the treatment patterns based on a histological four-tiered tumor grading system [1].
Materials and methods
The Korean Neuro-Oncology Group and the Korean Radiation Oncology Group performed a multi-institutional retrospective study to assess the patterns of care of LGG. Fourteen Korean institutes participated in this study. Each institute obtained approval of the Institutional Review Board and collected data. The eligibility criteria were pathologically confirmed WHO grade II LGG (astrocytoma, oligodendroglioma, and oligoastrocytoma) between 2000 and 2010 and age ≥ 20 years at diagnosis. Patients who were diagnosed by imaging study alone or had imaging finding of gliomatosis cerebri were excluded.
The medical records of 600 patients were centrally reviewed. The collected data encompassed patient characteristics, site of tumor, imaging information, initial surgical extent, details of adjuvant treatment and salvage treatment. The surgical extent was defined by postoperative magnetic resonance imaging (MRI) or operation reports: gross total resection (GTR) if > 99% of the tumor was removed, subtotal resection (STR) if ≥ 90% of the tumor removed, partial resection (PR) if ≥ 50% of the tumor removed, and biopsy if < 50% of the tumor removed [9]. Molecular characteristics such as 1p/19q gene deletion status or isocitrate dehydrogenase (IDH) 1/2 mutation status were not demanded in this study because the molecular data were not mandatory for pathologic reports during the study period.
We excluded 34 patients who had insufficient initial or adjuvant treatment data, and 26 patients diagnosed or underwent adjuvant treatment at outside institutions. Finally, a total of 555 patients were analyzed in this study, because 15 patients were doubly counted.
The patients were divided into four groups according to the adjuvant treatment type received: adjuvant fractionated RT alone (RT group), adjuvant chemotherapy alone (CT group), adjuvant fractionated RT and chemotherapy (RTCT group), and non-adjuvant treatment (NAT group). Six patients who underwent Gamma Knife surgery (GKS) after surgical resection were assigned to the NAT group.
Pearson’s Chi square test or linear-by-linear association test was used to find differences among these groups and patient/adjuvant treatment characteristics. To validate that which patient characteristics had influence on the choice of adjuvant RT or chemotherapy, we performed binary logistic regression tests. Age and the longest diameter were categorized using the median values. The Kaplan–Meier method was performed to estimate progression-free survival (PFS). Recurrence or progression of disease on imaging studies was defined by the Response Assessment in Neuro-Oncology (RANO) criteria [10]. When imaging information was not available, neurological status assessed by clinicians was also used. The log-rank test and the Cox proportional hazard regression model were used for univariate and multivariate analyses, respectively. Variables with a p value < 0.05 in the univariate analysis were included in the multivariate analysis. Statistical tests were performed using Predictive Analytics Software, version 18.0 (SAP America, Inc., Newtown Square, PA, USA).
Results
The median age of entire patients was 40 years, and 53% were male. Most of the patients had good performance status (92%) and 56% of patients presented with seizure. The frontal lobe was the most commonly involved site (61%), and 82% of patients had the tumor confined in one lobe. The median diameter was 4.7 cm (range 0.5–10.8 cm) on T2 FLAIR image, except 18 patients whose imaging information was not available. Pathologic diagnoses were astrocytoma in 38%, oligodendroglioma in 47%, and oligoastrocytoma in 15% of the patients. GTR was performed in 36%, STR in 28%, PR in 13%, and biopsy only in 24% of the patients (Supplemental Data).
The patient characteristics were compared according to the adjuvant therapy groups (Table 1). Gender, seizure, the number of involved lobes, the longest diameter, histology, and the extent of resection showed significant difference among adjuvant treatment groups. The proportion of patients with seizure was lower in the RT group than the other groups. More patients had the tumor confined in one lobe in the NAT group. Although there were several missing data, the NAT group had smaller tumor size. GTR was achieved more in the NAT group. Chemotherapy was administered more in patients with oligodendroglioma.
We plotted the proportion of adjuvant treatment groups over time to explore a trend of adjuvant treatment (Fig. 1a). The frequency of chemotherapy decreased during the last 3 years of the study period. This trend could also be found when the plots were divided into GTR and non-GTR patients (Fig. 1b, c). After histological classification, chemotherapy was less commonly administered in astrocytoma patients than oligoastrocytoma or oligodendroglioma patients (Fig. 1d–f).The chemotherapy regimen changed over time. PCV was used frequently in the first half of the study time, while the use of TMZ increased in the latter half of the study time (Fig. 2).
Binary logistic regression tests were performed to evaluate patient or tumor factors with a relationship to decisions concerning adjuvant treatments (Table 2). Patients with male gender, multiple lobe involvement, or non-GTR received RT, while patients with seizure were less likely to undergo RT. Chemotherapy was also preferred for patients with non-GTR, whereas chemotherapy was not preferred for patients with astrocytoma.
Details of adjuvant treatments are as follows. In the RT group, the median time interval between surgery and RT was 4 weeks (range 0.6–130.4 weeks). The median total dose and daily dose were 54 Gy (range 36–63 Gy) and 2 Gy (range 1.8–2.2 Gy), respectively. For the RTCT group, RT (median 3.6 weeks; range 0.1–165.9 weeks) was performed earlier than chemotherapy (median 14.3 weeks; range 1.6–180.6 weeks) after surgery. The median RT dose was 54 Gy (range 39–70 Gy) and median daily fraction size was 2 Gy (1.8–3 Gy). The most common chemotherapy regimen was PCV (60%) followed by TMZ (35%). The CT group patients received adjuvant chemotherapy a median of 5.9 weeks after the surgery. The most common regimen was PCV (55%) followed by TMZ (40%).
Characteristics of salvage treatments are listed in Table 3. The RT group had recurrence or progression in 120 patients (57%). Of these patients, surgical resection was performed in 64 patients (55%). RT was given in 15 patients (13%) with a median dose of 50 Gy. GKS was performed in 8 patients (7%) with the median dose of 20 Gy, and chemotherapy was administered in 66 patients (56%). Malignant transformation was confirmed in 49 patients.
In the RTCT group, progression or recurrence was noted in 24 patients (37%). Surgical resection was administered in 9 patients (38%), RT (median 45 Gy) in 4 patients (17%), GKS (median 25 Gy) in 4 patients (17%), and chemotherapy in 12 patients (50%). Malignant transformation was confirmed in 6 patients.
The CT group had progression in 12 patients (60%). For salvage treatment, surgical resection was performed in 7 patients (58%). RT was done in 9 patients (75%), and the median dose was 54 Gy. Chemotherapy was administered again in 5 patients (42%). Malignant transformation was found in 5 patients.
The NAT group included 6 patients who underwent GKS (median 19.5 Gy) after surgery. Progression or recurrences occurred in 148 patients (56%). Of these patients, 94 (64%) underwent surgery, 101 (68%) was given RT (median 57.6 Gy), 3 (2%) received GKS (median 16 Gy), and 41 (28%) was administered chemotherapy. Malignant transformation was found in 54 patients.
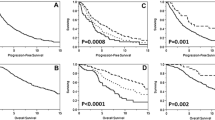
The median follow-up time was 83.4 months (range 6.0–184.7 months). In the entire patients, PFS rates were 52.2% at 5 year and 36.9% at 10 year. The median PFS time was 65.0 months. The results of univariate and multivariate analyses were summarized in Table 4. According to the multivariate analysis, the patient/tumor factors associated with worse PFS were poor performance, multiple lobes involvement, and parietal lobe. Concerning treatment factors, patients with GTR had better PFS than patients with non-GTR (at 5 year, 68.3 vs. 43.1%, p < 0.001; Fig. 3). Among the adjuvant treatments groups, the RTCT group showed statistically improved PFS comparing with the NAT group.
Discussion
We investigated the patterns of care for adult LGG patients between 2000 and 2010 in Korea. This is the first study about the patterns of care for LGG in Asia. At the time of the study, clear guidelines for LGG treatment had not been established. Consequently, we could find varied patterns of treatment used in a large population of LGG. Also, discernible changes of treatment could be observed during the study time.
We examined the association between patient/tumor characteristics and adjuvant treatment. Well-known predictors of adjuvant RT are age ≥ 40 years, tumor crossing midline, and partial surgical resection [11]. The extent of resection significantly affected the decision on adjuvant treatment in our study. Non-GTR patients received RT or chemotherapy more than GTR patients. Another factor significantly associated with adjuvant treatment was the number of involved lobes. Multiple lobes involvement could be an obstacle to tumor removal. GTR was achieved in 41% of patients with single lobe involvement, but in only 13% of patients with multiple lobes involvement (p < 0.001, data not shown). Several studies reported age as an important prognostic factor of LGG, but varied cut-off values have been suggested. We took 40 years, the median age in our study, as a cut-off value. We could not confirm a significant association between age and adjuvant treatment, but could find a trend that older patients had a trend to receive adjuvant treatment (p = 0.093).
An important change in the trend of chemotherapy was the decreased use of PCV regimen over time. In contrast, the proportion of TMZ increased. Although combined RT and PCV regimen was reported to improve overall survival in LGG patients [6], real-world clinicians might prefer to use TMZ in terms of compliance and convenience [12, 13]. Haque et al. [12] analyzed the National Cancer Data Base (NCDB) concerning LGG patients treated with RT and chemotherapy between 2004 and 2012 in the United States. The authors included high risk patients, such as age ≥ 40 years or sub-total resection. Interestingly, 96% of patients received TMZ instead of PCV (4%), and there was no significant difference in overall survival.
PCV can be toxic, particularly in terms of myelosuppression. In the Radiation Therapy Oncology Group (RTOG) 9802 study, considerable toxicities occurred in the RT + PCV arm. Grade ≥ 3 hematologic events were noted in 51% of the RT + PCV arm, but in < 1% of the RT arm [6]. The EORTC 22033–26033 trial compared RT and TMZ in LGG patients with high risk features. Grade ≥ 3 hematologic toxicities were reported in 14% of the TMZ arm and < 1% of the RT arm patients [8].
There are limited numbers of results comparing PCV and TMZ in LGG patients. We found implications in anaplastic glioma studies using different chemotherapy regimens. Wick et al. [14] reported that anaplastic glioma patients had more toxicity when they had PCV after surgery rather than TMZ in the NOA-04 trial. Between PCV and TMZ arms, survival outcomes were similar, but significant differences were found in allergic reaction (19 vs. 1%), hematologic toxicities (21 vs. 4%), and polyneuropathy (15 vs. 0%). The RTOG 9813 trial compared survival and toxicity of anaplastic astrocytoma patients who underwent RT and TMZ or carmustine/lomustine (BCNU/CCNU). Comparable overall survival times (median 3.9 years in the TMZ arm and 3.8 years in the BCNU/CCNU arm) were reported. In terms of toxicity, the BCNU/CCNU arm experienced more grade ≥ 3 toxicities (75.8 vs. 47.9%) and noted lower rate of chemotherapy completion (21.4 vs. 60.4%) than the TMZ arm [15].
In addition to the toxicity, PCV has a potential limitation concerning efficacy. In an animal model, vincristine had a lack of penetration across the blood–brain barrier. The levels of vincristine in the intracranial tumor were up to 11-fold lower than in the liver [16]. TMZ was reported to have better drug exposure in cerebrospinal fluid. In malignant glioma patients, the area under the concentration–time curve ratio in cerebrospinal fluid was 20% of the area under the curve in plasma [17].
Interestingly, the use of combined RT and chemotherapy was not preferred and decreased particularly during the last 3 years of our study period. Even the patients with non-GTR, 50–60% of patients received RT alone and 30–40% of patients underwent surgery alone. Similar with our results, the combined adjuvant treatment was not used frequently in another study. A study conducted at the Mayo Clinic reported their long-term experience about older LGG patients between 1960 and 2011, most of the patients (67%) received RT alone, despite their high-risk features, age ≥ 55 years and lower GTR rate (10%) [18].
Actually, these are paradoxical results because the RTCT group had the most favorable PFS in our study. The RTOG trial 9802 revealed the survival benefit of combining RT and chemotherapy in high-risk LGG patients. Patients with ≥ 40 years-old or non-GTR were enrolled in the RT arm or the RT/PCV arm. The RT/PCV arm had improved OS (median 13.3 vs. 7.8 years, p = 0.003) and PFS (median 10.4 vs. 4.0 years, p < 0.001) than the RT arm [6]. The socioeconomic characteristic of Korea could be a reason for the recession of the combined adjuvant treatment in our study. As mentioned above, the regimen of chemotherapy was changed from PCV to TMZ in Korea. The National Health Insurance in Korea, however, does not cover the use of TMZ in the patients with LGG. Therefore, LGG patients should pay all the cost of TMZ instead of 5% co-pay. A burden of medical costs could be an obstacle to administer TMZ in the adjuvant setting [19].
Concerns about cognitive dysfunction might also influence adjuvant treatments. RT has been examined concerning deteriorated cognitive function of glioma patients or not. Brown et al. [20] performed mini-mental state examinations for patients with LGG before and after RT. After 7 years of median follow up, cognitive function was preserved in most of patients without tumor progression. In contrast, Douw et al. [21] reported that LGG patients who had RT showed a decline in cognitive assessment comparing with who did not have RT. This result must be interpreted cautiously. First, a small number of patients were included (32 patients with RT vs. 33 patients without RT). Second, these patients were not randomly assigned, so patients with more advanced tumor could be suspected to receive RT. Actually, most of patients excluded during the study period because of death were RT group (69%).
When LGG patients with adjuvant RT was compared with “wait-and see” under randomly controlled condition (EORTC 22845 trial), no differences were found for cognitive deficit between two groups [7]. The RTOG 9802 trial reported long-term results of the combined use of RT and PCV chemotherapy comparing with RT alone in high risk LGG patients (≥ 40 years of age or non-GTR). The combined treatment arm improved OS [6] without significant deterioration in cognitive function measured by mini-mental state examination [22].
Recently, high-precision RT technique has been explored to preserve cognitive function. Whole-brain RT holds a significant portion for brain metastases treatment, but the RTOG 0933 trial confirmed memory preservation by sparing neural stem cells in the hippocampus [23]. For LGG patients, several dosimetric studies adopted this technique and reported that contralateral or bilateral hippocampus could be saved [24, 25].
There are several limitations in this study resulting from the retrospective design. The most important limitation is the lack of molecular information. We classified LGG as the traditional criteria using tumor histology, such as astrocytoma, oligoendroglioma, and oligoastrocytoma. This classification depends on morphological presentation, so inter- or intra-observer variability is inevitable. Heterogeneous clinical outcomes could also be resulted from similar pathologic diagnosis [26].
Recently, the Cancer Genome Atlas Research Network analyzed genomic molecular data of tumor samples from 293 adult LGG patients. The authors classified LGG according to the status of IDH mutations and 1p/19q codeletion, and confirmed that genetic status reflects tumor subtypes and clinical outcomes more than microscopic classifications. Wild-type IDH tumors had worst prognosis and related with glioblastoma. Tumors with IDH mutation and 1p/19q codeletion having oligodendroglial characteristics showed better survival than tumors with IDH mutation and no 1p/19q codeletion having astrocytoma or oligoastrocytic characteristics [27]. The WHO 2016 edition of glioma classification adopts the new criteria of IDH mutations and 1p/19q codeletion [28]. A paradigm shift in the treatment for LGG patients is expected, which will depend on molecular diagnosis.
Potential heterogeneity in the decision of adjuvant treatments and insufficiency in the collected patient and treatment data could not be neglected. Nevertheless, this study is meaningful; we could review and discern how we had practiced before the era of molecular biomarker-based diagnosis and treatment.
In conclusion, we reviewed multi-institutional data of LGG patients diagnosed with the WHO grade II gliomas between 2000 and 2010 in Korea. RT alone was most commonly performed after surgical resection for LGG. The combination of RT and chemotherapy shared minor portion, furthermore, it decreased during the last 3 year of the study period. Also, PCV was the main regimen of chemotherapy, however gradually substituted by TMZ. Lastly, the extent of resection or involvement could be associated with the decision on adjuvant treatments. With the emerging of molecular diagnosis, the treatment strategy should be refined according to the biomolecular criteria for LGG patients.
References
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109. https://doi.org/10.1007/s00401-007-0243-4
Ostrom QT, Gittleman H, Xu J, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS (2016) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009–2013. Neuro Oncol 18:v1–v75. https://doi.org/10.1093/neuonc/now207
Dho YS, Jung KW, Ha J, Seo Y, Park CK, Won YJ, Yoo H (2017) An updated nationwide epidemiology of primary brain tumors in Republic of Korea, 2013. Brain Tumor Res Treat 5:16–23. https://doi.org/10.14791/btrt.2017.5.1.16
Weller M, van den Bent M, Tonn JC, Stupp R, Preusser M, Cohen-Jonathan-Moyal E, Henriksson R, Le Rhun E, Balana C, Chinot O, Bendszus M, Reijneveld JC, Dhermain F, French P, Marosi C, Watts C, Oberg I, Pilkington G, Baumert BG, Taphoorn MJB, Hegi M, Westphal M, Reifenberger G, Soffietti R, Wick W, European Association for Neuro-Oncology (EANO) Task Force on Gliomas (2017) European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol 18:e315–e329 https://doi.org/10.1016/S1470-2045(17)30194-8
Pignatti F, van den Bent M, Curran D, Debruyne C, Sylvester R, Therasse P, Afra D, Cornu P, Bolla M, Vecht C, Karim AB, European Organization for Research and Treatment of Cancer Brain Tumor Cooperative Group, European Organization for Research and Treatment of Cancer Radiotherapy Cooperative Group (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20:2076–2084. https://doi.org/10.1200/JCO.2002.08.121
Buckner JC, Shaw EG, Pugh SL, Chakravarti A, Gilbert MR, Barger GR, Coons S, Ricci P, Bullard D, Brown PD, Stelzer K, Brachman D, Suh JH, Schultz CJ, Bahary JP, Fisher BJ, Kim H, Murtha AD, Bell EH, Won M, Mehta MP, Curran WJ Jr (2016) Radiation plus procarbazine, CCNU, and vincristine in low-grade glioma. N Engl J Med 374:1344–1355. https://doi.org/10.1056/NEJMoa1500925
van den Bent MJ, Afra D, de Witte O, Ben Hassel M, Schraub S, Hoang-Xuan K, Malmstrom PO, Collette L, Pierart M, Mirimanoff R, Karim AB, EORTC Radiotherapy and Brain Tumor Groups and the UK Medical Research Council (2005) Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial. Lancet 366:985–990 https://doi.org/10.1016/S0140-6736(05)67070-5
Baumert BG, Hegi ME, van den Bent MJ, von Deimling A, Gorlia T, Hoang-Xuan K, Brandes AA, Kantor G, Taphoorn MJ, Hassel MB, Hartmann C, Ryan G, Capper D, Kros JM, Kurscheid S, Wick W, Enting R, Reni M, Thiessen B, Dhermain F, Bromberg JE, Feuvret L, Reijneveld JC, Chinot O, Gijtenbeek JM, Rossiter JP, Dif N, Balana C, Bravo-Marques J, Clement PM, Marosi C, Tzuk-Shina T, Nordal RA, Rees J, Lacombe D, Mason WP, Stupp R (2016) Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033–26033): a randomised, open-label, phase 3 intergroup study. Lancet Oncol 17:1521–1532. https://doi.org/10.1016/S1470-2045(16)30313-8
McGirt MJ, Chaichana KL, Gathinji M, Attenello FJ, Than K, Olivi A, Weingart JD, Brem H, Quinones-Hinojosa AR (2009) Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J Neurosurg 110:156–162. https://doi.org/10.3171/2008.4.17536
Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, Degroot J, Wick W, Gilbert MR, Lassman AB, Tsien C, Mikkelsen T, Wong ET, Chamberlain MC, Stupp R, Lamborn KR, Vogelbaum MA, van den Bent MJ, Chang SM (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972. https://doi.org/10.1200/JCO.2009.26.3541
Suneja G, Alonso-Basanta M, Lustig R, Lee JY, Bekelman JE (2012) Postoperative radiation therapy for low-grade glioma: patterns of care between 1998 and 2006. Cancer 118:3735–3742. https://doi.org/10.1002/cncr.26693
Haque W, Verma V, Butler EB, Teh BS (2017) Patterns of care and outcomes of multi-agent versus single-agent chemotherapy as part of multimodal management of low grade glioma. J Neurooncol. https://doi.org/10.1007/s11060-017-2443-7
Field KM, Rosenthal MA, Khasraw M, Sawkins K, Nowak AK (2016) Evolving management of low grade glioma: no consensus amongst treating clinicians. J Clin Neurosci 23:81–87. https://doi.org/10.1016/j.jocn.2015.05.038
Wick W, Hartmann C, Engel C, Stoffels M, Felsberg J, Stockhammer F, Sabel MC, Koeppen S, Ketter R, Meyermann R, Rapp M, Meisner C, Kortmann RD, Pietsch T, Wiestler OD, Ernemann U, Bamberg M, Reifenberger G, von Deimling A, Weller M (2009) NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincristine or temozolomide. J Clin Oncol 27:5874–5880. https://doi.org/10.1200/JCO.2009.23.6497
Chang S, Zhang P, Cairncross JG, Gilbert MR, Bahary JP, Dolinskas CA, Chakravarti A, Aldape KD, Bell EH, Schiff D, Jaeckle K, Brown PD, Barger GR, Werner-Wasik M, Shih H, Brachman D, Penas-Prado M, Robins HI, Belanger K, Schultz C, Hunter G, Mehta M (2017) Phase III randomized study of radiation and temozolomide versus radiation and nitrosourea therapy for anaplastic astrocytoma: results of NRG oncology RTOG 9813. Neuro Oncol 19:252–258. https://doi.org/10.1093/neuonc/now236
Boyle FM, Eller SL, Grossman SA (2004) Penetration of intra-arterially administered vincristine in experimental brain tumor. Neuro Oncol 6:300–305. https://doi.org/10.1215/S1152851703000516
Ostermann S, Csajka C, Buclin T, Leyvraz S, Lejeune F, Decosterd LA, Stupp R (2004) Plasma and cerebrospinal fluid population pharmacokinetics of temozolomide in malignant glioma patients. Clin Cancer Res 10:3728–3736. https://doi.org/10.1158/1078-0432.CCR-03-0807
Youland RS, Schomas DA, Brown PD, Parney IF, Laack NNI (2017) Patterns of care and treatment outcomes in older adults with low grade glioma: a 50-year experience. J Neurooncol. https://doi.org/10.1007/s11060-017-2439-3
Yu T, Kang HC, Lim DH, Kim IH, Chung WK, Suh CO, Choi BO, Cho KH, Cho JH, Kim JH, Park CK, Hong YK, Kim IA (2015) Pattern of care of anaplastic oligodendroglioma and oligoastrocytoma in a Korean population: the Korean Radiation Oncology Group study 13–12. J Neurooncol 121:531–539. https://doi.org/10.1007/s11060-014-1660-6
Brown PD, Buckner JC, O’Fallon JR, Iturria NL, Brown CA, O’Neill BP, Scheithauer BW, Dinapoli RP, Arusell RM, Curran WJ, Abrams R, Shaw EG (2003) Effects of radiotherapy on cognitive function in patients with low-grade glioma measured by the folstein mini-mental state examination. J Clin Oncol 21:2519–2524. https://doi.org/10.1200/JCO.2003.04.172
Douw L, Klein M, Fagel SS, van den Heuvel J, Taphoorn MJ, Aaronson NK, Postma TJ, Vandertop WP, Mooij JJ, Boerman RH, Beute GN, Sluimer JD, Slotman BJ, Reijneveld JC, Heimans JJ (2009) Cognitive and radiological effects of radiotherapy in patients with low-grade glioma: long-term follow-up. Lancet Neurol 8:810–818. https://doi.org/10.1016/S1474-4422(09)70204-2
Prabhu RS, Won M, Shaw EG, Hu C, Brachman DG, Buckner JC, Stelzer KJ, Barger GR, Brown PD, Gilbert MR, Mehta MP (2014) Effect of the addition of chemotherapy to radiotherapy on cognitive function in patients with low-grade glioma: secondary analysis of RTOG 98-02. J Clin Oncol 32:535–541. https://doi.org/10.1200/JCO.2013.53.1830
Gondi V, Pugh SL, Tome WA, Caine C, Corn B, Kanner A, Rowley H, Kundapur V, DeNittis A, Greenspoon JN, Konski AA, Bauman GS, Shah S, Shi W, Wendland M, Kachnic L, Mehta MP (2014) Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol 32:3810–3816. https://doi.org/10.1200/JCO.2014.57.2909
Marsh JC, Godbole R, Diaz AZ, Gielda BT, Turian JV (2011) Sparing of the hippocampus, limbic circuit and neural stem cell compartment during partial brain radiotherapy for glioma: a dosimetric feasibility study. J Med Imaging Radiat Oncol 55:442–449. https://doi.org/10.1111/j.1754-9485.2011.02282.x
Kazda T, Pospisil P, Vrzal M, Sevela O, Prochazka T, Jancalek R, Slampa P, Laack NN (2015) Volumetric modulated arc therapy for hippocampal-sparing radiotherapy in transformed low-grade glioma: a treatment planning case report. Cancer Radiother 19:187–191. https://doi.org/10.1016/j.canrad.2014.11.013
van den Bent MJ (2010) Interobserver variation of the histopathological diagnosis in clinical trials on glioma: a clinician’s perspective. Acta Neuropathol 120:297–304. https://doi.org/10.1007/s00401-010-0725-7
Cancer Genome Atlas Research Network, Brat DJ, Verhaak RG, Aldape KD, Yung WK, Salama SR, Cooper LA, Rheinbay E, Miller CR, Vitucci M, Morozova O, Robertson AG, Noushmehr H, Laird PW, Cherniack AD, Akbani R, Huse JT, Ciriello G, Poisson LM, Barnholtz-Sloan JS, Berger MS, Brennan C, Colen RR, Colman H, Flanders AE, Giannini C, Grifford M, Iavarone A, Jain R, Joseph I, Kim J, Kasaian K, Mikkelsen T, Murray BA, O’Neill BP, Pachter L, Parsons DW, Sougnez C, Sulman EP, Vandenberg SR, Van Meir EG, von Deimling A, Zhang H, Crain D, Lau K, Mallery D, Morris S, Paulauskis J, Penny R, Shelton T, Sherman M, Yena P, Black A, Bowen J, Dicostanzo K, Gastier-Foster J, Leraas KM, Lichtenberg TM, Pierson CR, Ramirez NC, Taylor C, Weaver S, Wise L, Zmuda E, Davidsen T, Demchok JA, Eley G, Ferguson ML, Hutter CM, Mills Shaw KR, Ozenberger BA, Sheth M, Sofia Tarnuzzer R, Wang Z, Yang L, Zenklusen JC, Ayala B, Baboud J, Chudamani S, Jensen MA, Liu J, Pihl T, Raman R, Wan Y, Wu Y, Ally A, Auman JT, Balasundaram M, Balu S, Baylin SB, Beroukhim R, Bootwalla MS, Bowlby R, Bristow CA, Brooks D, Butterfield Y, Carlsen R, Carter S, Chin L, Chu A, Chuah E, Cibulskis K, Clarke A, Coetzee SG, Dhalla N, Fennell T, Fisher S, Gabriel S, Getz G, Gibbs R, Guin R, Hadjipanayis A, Hayes DN, Hinoue T, Hoadley K, Holt RA, Hoyle AP, Jefferys SR, Jones S, Jones CD, Kucherlapati R, Lai PH, Lander E, Lee S, Lichtenstein L, Ma Y, Maglinte DT, Mahadeshwar HS, Marra MA, Mayo M, Meng S, Meyerson ML, Mieczkowski PA, Moore RA, Mose LE, Mungall AJ, Pantazi A, Parfenov M, Park PJ, Parker JS, Perou CM, Protopopov A, Ren X, Roach J, Sabedot TS, Schein J, Schumacher SE, Seidman JG, Seth S, Shen H, Simons JV, Sipahimalani P, Soloway MG, Song X, Sun H, Tabak B, Tam A, Tan D, Tang J, Thiessen N, Triche T Jr., Van Den Berg DJ, Veluvolu U, Waring S, Weisenberger DJ, Wilkerson MD, Wong T, Wu J, Xi L, Xu AW, Yang L, Zack TI, Zhang J, Aksoy BA, Arachchi H, Benz C, Bernard B, Carlin D, Cho J, DiCara D, Frazer S, Fuller GN, Gao J, Gehlenborg N, Haussler D, Heiman DI, Iype L, Jacobsen A, Ju Z, Katzman S, Kim H, Knijnenburg T, Kreisberg RB, Lawrence MS, Lee W, Leinonen K, Lin P, Ling S, Liu W, Liu Liu Y, Lu Y, Mills G, Ng S, Noble MS, Paull E, Rao A, Reynolds S, Saksena G, Sanborn Z, Sander C, Schultz N, Senbabaoglu Y, Shen R, Shmulevich I, Sinha R, Stuart J, Sumer SO, Sun Y, Tasman N, Taylor BS, Voet D, Weinhold N, Weinstein JN, Yang D, Yoshihara K, Zheng S, Zhang W, Zou L, Abel T, Sadeghi S, Cohen ML, Eschbacher J, Hattab EM, Raghunathan A, Schniederjan MJ, Aziz D, Barnett G, Barrett W, Bigner DD, Boice L, Brewer C, Calatozzolo C, Campos B, Carlotti CG Jr., Chan TA, Cuppini L, Curley E, Cuzzubbo S, Devine K, DiMeco F, Duell R, Elder JB, Fehrenbach A, Finocchiaro G, Friedman W, Fulop J, Gardner J, Hermes B, Herold-Mende C, Jungk C, Kendler A, Lehman NL, Lipp E, Liu O, Mandt R, McGraw M, McLendon R, McPherson C, Neder L, Nguyen P, Noss A, Nunziata R, Ostrom QT, Palmer C, Perin A, Pollo B, Potapov A, Potapova O, Rathmell WK, Rotin D, Scarpace L, Schilero C, Senecal K, Shimmel K, Shurkhay V, Sifri S, Singh R, Sloan AE, Smolenski K, Staugaitis SM, Steele R, Thorne L, Tirapelli DP, Unterberg A, Vallurupalli M, Wang Y, Warnick R, Williams F, Wolinsky Y, Bell S, Rosenberg M, Stewart C, Huang F, Grimsby JL, Radenbaugh AJ, Zhang J (2015) Comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med 372:2481–2498. https://doi.org/10.1056/NEJMoa1402121
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization Classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Koo, T., Lim, D.H., Seol, H.J. et al. Multi-institutional study of treatment patterns in Korean patients with WHO grade II gliomas: KNOG 15-02 and KROG 16-04 intergroup study. J Neurooncol 138, 667–677 (2018). https://doi.org/10.1007/s11060-018-2839-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2839-z