Abstract
Object
Overdrainage is a chronic complication in shunted pediatric patients with hydrocephalus. The use of adjustability of differential pressure (DP) valves in combination with antisiphoning devices may help to overcome this sequela and may diminish the rate of possible shunt failures. The purpose of this retrospective study is to report our experience on shunt survival and infection rate with an adjustable DP valve with integrated gravitational unit in pediatric hydrocephalus.
Methods
The proGAV consists of an adjustable differential pressure (DP) valve and a gravitational unit. During the time period of July 2004 and December 2009, a total of 237 adjustable gravitational valves were used in 203 children (age, 6.5 ± 6.54; 0–27 years). In the follow-up period, valve and shunt failures as well as rate of infection were recorded.
Results
Within the average follow-up time of 21.9 ± 10.3 months (range, 6–72 months), the valve survival rate was 83.8 %. The overall shunt survival rate including all necessary revisions was 64.3 %. Looking at the group of infants (<1 year of age) within the cohort, the valve survival rate was 77.3 % and the shunt survival rate was 60.9 %. The overall infection rate was 4.6 %.
Conclusion
In a concept of avoiding chronic overdrainage by using the proGAV in hydrocephalic children, we observed a good rate of valve and shunt survival. Compared to previous reported series, we experienced the proGAV as a reliable tool for the treatment of pediatric hydrocephalus.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
For the treatment of pediatric hydrocephalus, the technical quality of new valve designs continues to improve by the introduction of adjustability in differential pressure (DP) valves and overcoming the siphoning effect by, e.g., antisiphon devices or gravitational units. It is an evident fact to keep in mind, that the quality of shunts used at the first implantation may significantly influence the neurocognitive development of children by its biomechanical construction as well as by any risks for possible complications or the need of further revisions.
Overdrainage is a well-known chronic complication after long-term shunting in pediatric hydrocephalus [5–8, 11, 29, 33]. The compensatory capacity of the pediatric skull and central nervous system anatomy leads to long-term changes of the cerebrospinal fluid (CSF) tissue ratios which are able to cause microcephaly, calvarial hyperplasia, slit ventricle syndrome, and shunt-induced Chiari malformations [9, 12, 19, 28, 36]. In older children, frequent complications do not only lead to further surgeries and shunt revisions but also to chronic headaches and additional neurological impairments [1, 10, 14, 36, 40]. Since these changes are only recognized after years of treatment, this problem seems to be rather neglected [15].
Previously developed valve designs devoted either to fixed differential pressure assumed to be adequate at the time of implantation and only being revised if problems do occur in later life. The development of adjustable DP valves adds the possibility of reacting to clinical or developmental changes after implantation which may lead to improvement of treating pediatric hydrocephalus. Furthermore, the siphoning effect was recognized as possible factor for chronic overdrainage [6, 7, 18, 31, 33, 36]. That implies that the acting forces for diverting CSF by a ventricular peritoneal shunt are the intracranial pressure (ICP), the intraperitoneal pressure (IPP), and the hydrostatic pressure (HP). The latter is defined by the height level of the CSF-producing cavity (Foramen of Monro) subtracted by the height level of the cavity where the CSF is drained to (measured at level of the diaphragm). While the IP acts negatively and the ICP and HP are acting positively on CSF drainage, the valves need to balance out all these factors to establish a near-physiological drainage over time. The fact that the HP is posture dependent and irrelevant in the lying position since in ventriculo–peritoneal (VP) shunting, the height level of the ventricles and the peritoneum is fairly similar but in the standing position the difference in height level of the compartments adds a drainage force is well-known as siphoning effect. This siphoning effect may be one relevant factor for chronic overdrainage in hydrocephalic patients. Thus, several devices were brought to the market to overcome the hydrostatic linked overdrainage problem. The effect on overdrainage by using either adjustable DP valves and/or antisiphon devices have been shown in previous studies [5, 8, 10, 12–14, 17, 21, 24, 26, 35, 36, 42]. Since overdrainage problems have still been reported, especially in studies, where adjustable DP valves are used alone, it is reasonable to combine the facility of adjustability offering individual adaptation of the DP valve together with an antisiphon device which constantly addresses the siphoning effect.
In the following retrospective study, we report our single-center pediatric neurosurgical experience on shunt survival and infection rate using an adjustable DP valve with gravitational assistance, called programmable gravitational assisted valve (proGAV), in the treatment of hydrocephalus, which is routinely used in our division.
Methods
In this retrospective, single-center cohort study, the use of an adjustable DP valve with gravitational unit for the treatment of childhood hydrocephalus was reviewed. We looked at all proGAVs which have been used either at primary implantation or for shunt revisions within the time period of July 2004 and December 2009 which have been treated by the pediatric neurosurgical division at our medical center. During the initial years until 2007, the valve was used in cases when the surgeon believed that adjustability could be of any benefit for the so defined complex patients instead of using a fixed DP valves with gravitational assistance (paediGAV). During 2007, the strategy was changed in our division to an almost exclusive use of the proGAV for all patients in our pediatric neurosurgical unit. Data were collected from the online surgical report system as well as from the in-house and outpatient clinic charts in order to define the total number of primary surgical implantations as well as possible later surgical revisions. Patients have only been included if they were in follow up on regular basis in our hospital until end of June 2010.
During the time period, a total of 237 valves were used for the treatment in 203 patients. The patients’ age ranged from 0 to 27 years. The median age was 6.51 ± 6.54 years. Among the cohort were 96 females and 107 males (Table 1). Of the 237 valves, 110 were used as a primary implants and 127 as part of a shunt revision. For all new implantations, the valve has been integrated into a VP shunt system. Among the revisions were five ventriculoartrial shunts (VA shunts).
The etiologies of hydrocephalus included various possibilities. Similar to previously reported cohorts, the common causes of hydrocephalus were intraventricular hemorrhage; previous infection; malformations like spina bifida, Chiari, or Dandy–Walker malformations; aqueductal stenosis; traumatic brain injury; brain tumors related hydrocephalus; or idiopathic.
The proGAV (Miethke, Aesculap, Potsdam, Tuttlingen, Germany) consists of an adjustable DP valve and a gravitational unit connected together by a silicon tubing (Fig. 1). Within the adjustable ball-in-cone-valve regulated by a rotor which changes the tension of a spring acting on the valve mechanism, an opening pressure can be chosen in the range of 0–20 cmH2O. The gravitational unit does add an additional resistance to the chosen opening pressure in a gradual manner when the valve is erected from 0° towards an upright position of 90°. The predetermined setting of the gravitational unit was chosen depending on size and age of the child being either 20 or 25 cmH2O. The adjustable setting of the DP valve as well as the predetermined setting of the gravitational units was chosen according to the individual surgeons’ decision. For surgical implantation, the ventricular catheter was placed in a frontal precoronal position in all patients to enable the valve being placed in strictly vertical position subcutaneously behind the ear [3, 30, 37, 41].
Results
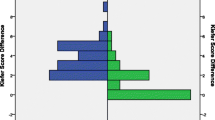
The average follow-up time of 237 implants used in 203 patients was 21.9 ± 10.3 months (6–72 months). As shown in Kaplan–Meier curves, the overall valve survival rate was 83.8 %. The survival rate of valves at 12 and 24 months, respectively, was 87.2 and 85.2 %. The overall shunt survival, including all necessary revisions, was 64.3 % while it was 74.6 % and 65.7 % at 12 and 24 months, respectively (Fig. 2a, b).
Altogether, 111 revisions were performed in 74 patients after using the proGAV. Thirty patients had more than one revision during this time period. Mean revision rate in those were 2.6 per patient (range, two to four per patient). Revisions included the proximal shunt part in 53 cases, the valve in 34 cases, while in 39 cases the distal part of the shunt was involved. The valve alone was exchanged in four patients of the 34 valve revisions. Within these numbers, some overlap of surgeries must be considered, since sometimes more than one part of the shunt was revised within one surgery resulting in a total number of 111 revisions within the follow-up period.
The infection rate was 4.6 % (n = 16), including nine patients aged less than 1 year. Seven patients had an infection after an early revision of the shunt following valve implantation. Occlusion of the valve was seen in 13 cases (5.5 %). Other reasons for revisions were wound healing problems (n = 2), a scheduled explantation after weaning the CSF diversion and proof of shunt independence (n = 1). The exchange of the gravitational unit to another resistance level was performed in two cases (Table 2).
Forty-two of 74 patients were revised within 3 months after surgery, and thus may be classified as surgery-related revisions. The latter include 19 of 34 valve revisions. In the remaining follow-up time in 32 patients, a revision was undertaken including 15 valve revisions.
Looking at the group of infants within the cohort (mean age, 4 ± 3.2 months; follow-up, 20.6 ± 9.2 months), the valve survival rate was 77.3 % (81.8 % at 12 months) and the overall shunt survival rate was 60.9 % (72.4 % at 12 months). Infection rate in infants revealed 8.3 % and occlusion rate 6.8 %, respectively. The wound healing problems of two cases were both infants.
Discussion
The present retrospective study is reporting on the use of an adjustable DP valve with gravitational assistance in hydrocephalus, which shows an overall valve survival of 83.8 % and an overall shunt survival of 64.3 % after 21.9 ± 10.3 months based on a single-center pediatric neurosurgical experience. Thereby, we could show that the use of the proGAV in our CSF diversion protocol was as a reliable and well-tolerated tool for shunt treatment in all age groups of pediatric hydrocephalus.
The use of this valve system has been reported in other studies before [3, 25, 34, 38, 39, 41]. Sprung et al. [39] achieved excellent results in a multicenter study including 144 patients (12 % of them children) over a follow-up time up to 12 months with an overall shunt survival rate without revisions of 83 % and a valve survival rate of 91 %. They also examined the performed 102 adjustments in almost all patients. Eighty-five percent of their patients rated the adjustment as acceptable and there was no skin irritation in 84 %. The most obvious change on the skin was a blue spot in one patient. Underdrainage was found in 67 and overdrainage in 35 patients but except one patient all of them were improved after adjusting the valve settings. In a study of 50 adults whose normal-pressure hydrocephalus (NPH) was treated with a proGAV. Toma et al. [41] reached a revision-free shunt survival rate of 86 % in the follow-up of 12 months. Most revisions were performed because of distal catheter malfunction. Only one revision concerned the valve itself. They performed 24 adjustments in 19 patients (38 %). After an adjustment, four patients (21 % of the adjusted population) needed further surgery. Meier et al. [25] published a study with 34 adult patients receiving a proGAV within 1 year. The patients all had an idiopathic NPH. They achieved a responder rate of 77 % but described problems in six patients within the adjustment in the first 10 postoperative days because of wound swelling and suture problems. Rhode et al. [34] used the proGAV in a population of 53 children with hydrocephalus with a mean follow-up period of 15.2 months. The study reached an overall success rate of 88.7 % without any valve-related complications. The valve pressure was readjusted in 19 patients (35.8 %). In 18 cases, valve settings were changed because of over- or underdrainage. One case was readjusted because of shunt weaning. Ninety-five percent improved after the adjustment. The study reached an end-point with a surgery-free shunt survival in 75.5 %. Our presented study is one of the first studies proving the reliable use of the valve in a bigger cohort of pediatric patients including infants. The results of the previously discussed studies mirror very well our results and offer the perspective that the characteristics of new valves move in a favorable direction.
The proGAV combines two features of modern shunt techniques in order to overcome long-term sequelae of overdrainage. This includes adjustability in a differential pressure valve and the use of a gravitational unit to overcome the siphoning effect [39]. With regards to the utilization of adjustability, we were able to show in a survey of 132 patients and relatives that adjustments of valve settings were performed in ca. 50 % of patients. It was experienced that individual adaptation of valve settings resulted in 96 % satisfaction for this type of valve. Of those patients, only one third needed further surgery after adjusting the valve, leaving two thirds of the patients that have profited by adjusting the valve settings (unpublished data). A possible drawback of adjustability may be that individual patient may focus their expectation on possible adjustments in order to enhance any clinical symptoms which may be unrelated to the valve settings. In some cases, it can also be difficult to identify clinical symptoms of being related to over- or underdrainage. Thus, meticulous and repeated investigation of clinical history and symptomatology is necessary in order to manage valve adjustments correctly in tough cases. Therefore, it becomes important for us that adjustments should only be performed with clear reasoning, liberal handling must be avoided and the adjustment unit itself must offer high reliability. In this context, an advantage of the proGAV, in contrast to other adjustable valves may become obvious. The adjustment unit is not influenced by magnetic resonance imaging (MRI) or other magnetic fields and the setting can be determined without X-ray [2–4, 22, 23, 27]. Allin et al. [3] demonstrated in an in vitro trial that the proGAV setting was unaltered in magnetic fields up to 3 T. Three valves were tested over 28 days in three identical testing rigs. They proved the stability of the adjustment unit under the influence of 3 T in different temperatures (from 34 to 40 °C), in different pressure conditions, in different settings, and in the vertical and horizontal position. The same study also demonstrated a high reliability using the measurement pen to determine the valve setting. Despite similar results regarding the first year shunt survival, the MRI sensitivity of other adjustable valves remains a problem. The adjustable Codman Hakim was examined in a single-center study by Zemack et al. [42] with 583 patients (162 children). The 1 year survival rate was 74.6 % but there were 35 cases documented in whom the opening pressure was altered by MRI causing 27 of 706 re-adjustments of the opening pressure in 247 patients, thereof 84 children. Nevertheless, the surgeons performed 318 revisions, thereof 90 valve removals, mostly because of infection. Four valves had been replaced because of adjustment problems.
According to the gained experience with using the proGAV during the observation period, we suggested a protocol for the initial selection of the DP unit in our children. This protocol is shown in Table 3. The basic idea is that the increasing activity of children during their development might increase the risk of overdrainage. Thus, the resistance level of the valve should be gradually increased over time until adolescence. Thereafter, a gradual decrease of the resistance might be considered. Nevertheless, this protocol is only used as a rough guideline within our pediatric neurosurgical unit and individual adaptation should be applied in certain cases. In terms of the resistance of the gravitational unit, we use 25 cmH2O in older and taller children or adolescents. During follow-up, we usually see our patients as outpatients 4–8 weeks after surgery in order to clinically evaluate the need of further adaptation. Follow-up MRI is performed every 12 months and in complex cases 3 months after surgery. This protocol will need further evaluation to gain scientific evidence.
Looking at the possible benefit of adjustability for surgical revisions, we are able to compare the current data with the paediGAV study [15] in which the non-adjustable DP valve with gravitational assistance. The study included 169 children with an overall valve survival rate after 12 and 24 months of 79.2 and 75.6 %, respectively. In comparison, the survival rate in the current study was 87.2 and 85.2 % for the same observation period, respectively, demonstrating a possible benefit of adjustability in terms of less surgical revisions. This conclusion has to be handled cautiously, since our data represent a retrospective single-center study and Haberl et al. presented a prospective multicenter observational study.
The same holds true for comparing this study with other reports on different valves. Since shunt survival rate is commonly reported as outcome parameter it is worthwhile comparing this value. A prospective multicenter randomized trial [11] using the Delta valve, which includes an antisiphon unit of different mechanic design (Medtronic, USA) and the Orbis Sigma I valve (Cordis, Miami, USA), including a flow control mechanism, showed a 1 year shunt survival of 56 and 61 %, respectively. Furthermore, the adjustable Codman Hakim (Johnson and Johnson, USA) valve was observed by Zemack et al. [43] in a retrospective manner in a single-center study with 158 patients (mean age at implantation, 4.4 years) demonstrating a 1 year shunt survival rate of 60.5 %. Pollack et al. [32] published their experiences using the adjustable Codman Hakim valve in a randomized controlled trial reaching a surgery-free shunt survival rate of 52 %. In a multicenter prospective study by Hanlo et al. [16] using the Orbis Sigma II valve including 52 % of pediatric patients, 557 patients have been included. Hereby, the overall shunt survival at 1 year was similar to our study with 71 %; however, representing a cohort with a significant higher mean age. The subgroup of children with the age under 6 months reached a shunt survival of 55 %. The adjustable strata valve (Medtronic, Neurosurgery, Goleta, CA, USA) including a siphon-controlled mechanism was evaluated by Kestle et al. [20] in a prospective multicenter study. Following a 12-month follow-up period of a shunt, survival rate of 67 % was observed. All the discussed studies seem to indicate a trend which might not consciously be recognized during the daily routine in pediatric neurosurgery. Over the recent years, the developments have led to an increased shunt survival. Whether this is solely based on an improved valve design has never been proven so far. Advances in surgical implantation techniques might also lead to the positive trends especially those measured within the first 12 months after shunt surgery, since this period includes surgery-related complications. These advances include that experienced surgeons are more often involved in the so-called easy surgery itself which is, however, associated with various complications. Moreover, better hygienic protocols during shunt surgery might have reduced the infection rates. A strict protocol was used in the presented study, which included that only pediatric neurosurgeons performed the shunt operations. A doubled and meticulous procedure of skin preparation and meticulous draping were preceding the surgery. Since 2007, antibiotic-impregnated catheters were used in high-risk patients including those with an external ventricular drainage in place before surgery, those under the age of 1 year and those patients when endoscopic equipment was used during shunt implantation. Thus, we might also conclude an elaborated protocol for shunt surgery is an important factor for an excellent outcome. Nevertheless, an overall valve survival rate of 83.8 % in this study implies a good reliability of the used valve especially since more than 50 % of the valve revisions were primary surgery related and were taken place within the first 3 months. Moreover, we would like to stress that the same valve was successfully used in all age groups in this study with a reasonable success rate. This leads to the conclusion that the proGAV can also be implanted in infants. The evaluation of possible wound healing problems due to a bigger valve design taught us that the height of the valve’s dimension but not its wideness matters in this respect. The wound healing problems that have been seen in this study included two infants. Both infants suffered significant macrocephaly and wound healing was compromised due to increased tension within the skin over the expanded skull.
Further studies need to evaluate if long-term complications of overdrainage can be solved by using gravitational assisted valves or other kind of antisiphon devices. Therefore, long-term data of head growth after shunting, imaging data to evaluate possible anatomical changes like ventricular size, bone hyperplasia and intracranial volume measurements as well as neurocognitive data must be collected to answer this question. Since this needs at least observational measurements until 5 years after shunt implantation, a significant challenge for further research is still evident.
In conclusion, the presented concept to use an adjustable differential pressure valve combined with a gravitational unit in hydrocephalus together with the described protocol seems to be a reliable technique for shunting pediatric patients. By using one single-valve design in all age groups of patients, we observed a reasonable rate of valve and shunt survival, which compares favorably with recent studies of other shunt designs. To prove an advantage in avoiding the long-term sequelae of overdrainage data, a longer follow-up will be needed in prospective controlled studies.
References
Abott R (1991) Chronic headache associated with a functioning shunt: usefulness of pressure monitoring. Neurosurgery 28:72–77
Akbar M (2005) Magnetic resonance imaging and cerebrospinal fluid shunt valves. N Engl J Med 353:1413–1414
Allin D (2006) In vitro hydrodynamic properties of the Miethke proGAV hydrocephalus shunt. Cerebrospinal Fluid Res 3:9
Allin D (2008) Investigation of the hydrodynamic properties of a new MRI-resistant programmable hydrocephalus shunt. Cerebrospinal Fluid Res 5:8
Aschoff A (1995) Overdrainage and shunt technology. A critical comparison of programmable, hydrostatic and variable-resistance valves and flow-reducing devices. Childs Nerv Syst 11:193–202
Browd S (2006) Failure of cerebrospinal fluid shunts: part II: overdrainge, loculation, and abdominal complications. Pediatr Neurol 34(3):171–176
Czonsnyka ZH (1998) Posture-related overdrainage: comparison of the performance of 10 hydrocephalus shunts in vitro. Neurosurgery 42:327–333
Czonsnyka ZH (2001) Laboratory evaluation of the phoenix CRx diamond valve. Neurosurgery 48:689–694
Drake J (1995) The shunt book. Blackwell, Camebridge
Drake J (1996) Rationale and methodology of the multicenter pediatric cerebrospinal fluid shunt design trial. Child’s Nerv Syst 12(8):434–447
Drake J (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 43:294–303
Faulhauer K (1978) Overdrainage phenomena in shunt treated hydrocephalus. Acta Neurochir (Wien) 45:89–101
Gruber R (1980) The problem of chronic overdrainage of the ventriculoperitoneal shunt in congenital hydrocephalus. Z Kinderchir 31:362–369
Gruber R (1984) Experiences with the anti-siphon device (ASD) in shunt therapy of pediatric hydrocephalus. J Neurosurg 61:156–162
Haberl E (2009) Experiences with a gravity-assisted valve in hydrocephalic children. J Neurosurg Pediatr 4:288–293
Hanlo PW (2003) Treatment of hydrocephalus determined by the European orbis sigma valve II survey: a multicenter prospective 5-year shunt survival study in children and adults in whom a flow-regulating shunt was used. J Neurosurg 99:52–57
Hatlen TJ (2012) Nonprogrammable and programmable cerebrospinal fluid shunt valves: a 5-year study. J Neurosurg Pediatr 9:462–467
Higashi S (1994) Effects of head elevation on intracranial hemodynamics in patients with ventriculoperitoneal shunts. J Neurosurg 81:829–836
Hirsch JF (1992) Surgery of hydrocephalus: past, present and future. Acta Neurochir (Wien) 116:155–160
Kestle JRW (2005) A multicenter prospective cohort study of the strata valve for the management of hydrocephalus in pediatric patients. J Neurosurg 102(Pediatrics 2):141–145
Khan RA (2010) Role of shunts with antisiphon device in treatment of pediatric hydrocephalus. Clin Neurol Neurosurg 112:687–690
Lavinio A (2008) Magnetic field interactions in adjustable hydrocephalus shunts. J Neurosurg Pediatr 2:222–228
Lindner D (2005) Effect of 3 T MRI on the function of shunt valves—evaluation of paediGAV, dual switch and proGAV. Eur J Radiol 56:56–59
McGirt MJ (2007) Adjustable vs set-pressure valves decrease the risk of proximal shunt obstruction in the treatment of pediatric hydrocephalus. Child’s Nerv Syst 23:289–295
Meier U (2007) Clinical experience in the treatment of idiopathic normal-pressure hydrocephalus using the new programmable gravity-assisted valves (proGAV Aesculap). Akt Neurol 34:147–150
Meling TR (2005) The gravity-assisted paedi-GAV valve in the treatment of pediatric hydrocephalus. Pediatr Neurosurg 41:8–14
Nakashima K (2011) Programmable shunt valves: in vitro assessment of safety of the magnetic field generated by a portable game machine. Neurol Med Chir 51:635–638
Oi S (1987) Infantile hydrocephalus and the slit ventricle syndrome in early infancy. Child’s Nerv Syst 3:145–150
Oi S (1989) Hydrocephalus in premature infants. Characteristics and therapeutic problems. Child’s Nerv Syst 5:76–82
Park J (2007) Valve inclination influences the performance of gravity-assisted valve. Surg Neurol 68:14–18
Petrella G (2009) In vivo assessment of hydrocephalus shunt. Acta Neurol Scand 120:317–323
Pollack I (1999) A randomized controlled study of a programmable shunt valve versus a conventional valve for patients with hydrocephalus. Hakim Medos Investigator Group. Neurosurgery 45:1399–1408
Pudenz R (1991) Hydrocephalus: overdrainage by ventricular shunts. A review and recommendations. Surg Neurol 35:200–212
Rhode V (2009) First experiences with an adjustable gravitational valve in childhood hydrocepalus. J Neurosurg Pediatrics 3:90–93
Sainte-Rose C (1987) A new approach in the treatment of hydrocephalus. J Neurosurg 66:213–226
Sprung C (1996) The dual-switch valve. A new hydrostatic valve for the treatment of hydrocephalus. Child’s Nerv Syst 12:573–581
Sprung C (2005) The enigma of underdrainage in shunting with hydrostatic valves and possible solutions. Acta Neurochir 95:229–235
Sprung C (2005) Shuntingof hydrocephalus with the new adjustable gravitational proGAV—advantages compared to other devices. Cerebros Fluid Research 2(Suppl 1):37
Sprung C (2010) The adjustable proGAV shunt: a prospective safety and reliability multicenter study. Neurosurgery 66:465–474
Stellman-Ward GR (1997) The incidence of chronic headache in children with shunted hydrocephalus. Eur J Pediatr Surg 7:12–14
Toma AK (2011) Use of the proGAV shunt valve in normal-pressure hydrocephalus. Operative Neurosurgery 2:245–249
Zemack G (2000) Seven years of clinical experience with the programmable Codman Hakim valve: a retrospective study of 583 patients. J Neurosurg 92:941–948
Zemack G (2003) Clinical experience with the use of a shunt with an adjustable valve in children with hydrocephalus. J Neurosurg 98:471–476
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomale, UW., Gebert, A.F., Haberl, H. et al. Shunt survival rates by using the adjustable differential pressure valve combined with a gravitational unit (proGAV) in pediatric neurosurgery. Childs Nerv Syst 29, 425–431 (2013). https://doi.org/10.1007/s00381-012-1956-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1956-9