Abstract
Objective
We reviewed our experience in surgical treatment of craniopharyngiomas. Surgical treatment of craniopharyngiomas in children represents a challenge for neurosurgeons because it presents a different set of surgical problems. Results are controversial and debates concerning strategies to ameliorate the rate of success and to decrease the rate of morbidity and mortality are ongoing. Post-surgical quality of life is related to the anatomical relationship between the hypothalamic region, vascular structures and optic pathways.
Discussion
From 1985 to 2004, 60 children (age range, 4 months to 18 years) were treated in our institution. Since 1987, all patients were studied with pre- and postoperative MRI. Two groups of patients were distinguished: a group of 36 patients treated with surgical direct surgery; a second group of 24 patients treated only with intracystic chemotherapy with bleomycin (18 patients) or associated with surgery (six patients). In the first group, the removal of lesion was total in 74% of cases. Two patients died in the early postoperative period and two more died later (early mortality of 5% and late mortality of 11%). All patients presented ante-pituitary insufficiency and diabetes insipidus, which required substitutive treatment. Twenty-two patients presented with visual problems, including amaurosis in two cases. In the group treated with bleomycin, 18 patients presented a primary cystic or a mixed form of craniopharyngioma and six patients showed a cystic recurrence. Eighteen patients were treated with bleomycin only. The dose used varied from 30 mg to a maximal dose of 150 mg, with a middle dose of 60 mg in the large majority of cases. In this group, the cyst disappeared in 12 patients and reduced to 30% of its initial volume, and stabilization of the lesion was achieved in the other six patients. Only 11 patients presented partial endocrine insufficiency. Of the 18 patients, 16 were of school age, 14 of whom were following a normal educational program and two an assisted program. No mortality was reported.
Conclusion
Our experience showed that in the group treated with intracystic chemotherapy alone, results were better with a low rate of morbidity and mortality. Endocrinological, visual and neuropsychological evaluations were also correlated with better outcome. In cases of cystic craniopharyngiomas, we considered bleomycin as the treatment of choice. For solid forms or for cases resistant to intracystic chemotherapy with bleomycin, direct surgery has to be proposed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of craniopharyngiomas in children represents a challenge for neurosurgeons, because surgical problems are different in children compared to those encountered in adults [16, 20, 24, 32].
In spite of the histological benign nature of the tumor, its deep location and its anatomical relationship with the basal structures pushed to define craniopharyngiomas as benign lesions with a malignant location.
Results of their treatment are also controversial and have been nourishing, for a long time, passionate debates about the strategies to follow to ameliorate the rate of successful treatment and to reduce the rate of morbidity and mortality.
Neurosurgeons and paediatric neurosurgeons have several specific imperatives: to avoid damage of hypothalamic structures responsible for behavioral and cognitive troubles, to preserve the hypotalamo-pituitary axis, and to decrease the rate of recurrences and lesions related to cerebral radiotherapy in young brain.
The necessity of realizing a complete surgical removal with satisfactory neurological, neuropsychological, visual and endocrinological results is opposed by other authors who support a more conservative attitude with partial removal followed by radiotherapy.
The anatomical extension of the tumor, its relationship with the hypothalamus and the vascular structures and its relationship with the optic pathways account for the difficulties in surgery associated with the risk of high morbidity and mortality also in the microsurgical era.
Theoretically, if it is more satisfying to realize total removal for benign lesions with craniopharyngiomas, this adage has to be modulated because many factors play an important role in establishing a surgical strategy: the experience of surgeons, the size and extension of lesions, consistency (solid, cystic or mixed form), and the preoperative clinical state. Microsurgical techniques have favored a decrease in the rate of mortality that, for some people, should be 2% [1, 12, 25].
We present our own philosophy in the treatment of craniopharyngiomas that we have developed in recent years.
Patients and methods
Our experience concerns 122 patients who were treated in our institution from 1962 to 2004, of whom 102 were of paediatric age and 20 were adults. Of these patients, 42 (of paediatric age) who were included in a previous report were not considered for this paper. We also did not consider our experience in adults [24].
From 1985 to 2004, 60 children with craniopharyngioma were treated in our institution. These patients, whose age varied from 4 months to 18 years, were predominantly between 3 and 11 years. Both age and sex distribution were in accordance with the data found in the literature.
Clinical symptoms included increased intracranial hypertension (55% of patients), visual troubles (about 48%) and endocrine disturbances (about 45%). Starting in 1987, all patients were studied with pre- and postoperative cerebral MRI.
We classified our patients into two groups:
-
The first group consisted of 36 patients who were submitted to a direct surgical procedure with a fronto-temporal approach, in most of cases, with the same basic principles: to realize a total removal with the preservation, if possible, of the pituitary stalk, to decompress the optic pathways, opening of lamina terminalis, to preserve the hypothalamic region for reducing the incidence of endocrinological sequels, obesity, sexual troubles and to decrease the risk of recurrence.
-
The second group consisted of 24 children who were managed with intracystic chemotherapy with bleomycine only (18 patients) or associated with surgery (six patients).
In the first group, all patients were operated with a frontal–temporal flap using a subfrontal approach to expose the four basal triangles. Three of these patients required a combined subfrontal transcallosal approach simultaneously; one patient was operated on via a subtemporal avenue, and, more recently one patient was managed by a transnasal (TN) approach assisted by endoscopy.
Removal of lesion was total in 27 patients (74%) and partial in nine cases (26%). Study of the operative chart showed that the pituitary stalk was preserved in nine cases, visualized but not preserved in 20 cases, and not visualized in seven patients.
Two patients died during the immediate postoperative period and two more patients at a later period for metabolic troubles (early mortality of 5.5% and late mortality of 11%).
From a visual point of view, 22 patients presented troubles including amaurosis in two cases, a decreased acuity in three cases aggravated by the surgical procedure, and a visual field deficit in the others.
All patients presented ante-pituitary insufficiency and diabetes insipidus requiring treatment with Minirin.
Six patients were obese and two presented left hemiparesis that did not impede their walking.
In the first group, all patients but one were of school age. Twenty patients attended a normal school, four patients were enrolled in a normal school but followed an assisted program, three were in a specialized institute, and only two patients attended university. Three patients went to a professional school. Two patients in this group got married last year.
In the second group, which consisted of 24 patients treated only with intracystic chemotherapy with bleomycine, we individualized six patients presenting a cystic recurrence and 18 patients with a cystic or mixed form of a primary craniopharyngioma. This group consisted of patients whose age ranged between 6 months and 16 years.
Eighteen patients were managed with intracystic bleomycine only.
Clinically, eight patients presented signs of increased cerebral hypertension, three had visual troubles, one presented potomania, four had endocrine troubles with an arrested growth, and one presented a polycinetic nystagmus. In one patient, the diagnosis was made incidentally after cranial trauma.
The dose used varied from a minimal dose of 30 mg to a maximal dose of 150 mg, with a middle dose of 60 mg in the large majority of cases. Following intracystic bleomycine, the cyst disappeared in 12 patients. In six patients, cyst volume reduced to 30% of the initial volume with stabilization of the lesion. Follow-up period varied from 1 to 14 years, with a mean follow-up of 6 years and 8 months.
After treatment, we focused on the amelioration of visual troubles in three patients. Eleven patients presented endocrine insufficiency: six presented growth hormone deficiency, two had hypothyroidism and three had adrenal–cortical deficiency.
Four patients presented with diabetes insipidus that appeared in three cases after the treatment. Out of 18 patients, 16 were of school age, 14 of whom were following a normal program and two an assisted program. During this period, one patient enrolled at a university and another finished her studies to become a dressmaker. No mortality was observed in this group.
At the beginning of our experience, six patients were treated with bleomycine, followed by surgery, resulting in total removal in five cases and partial removal in one case. In all cases, bleomycine was used to reduce the rate of recurrence.
One patient presented blindness following the injection of a toxic dose of the drug and needed an emergency surgical decompression. Recovery was not achieved. The patient who had a partial tumor removal was treated with conformational radiotherapy.
In this group, all patients presented endocrine insufficiency as well as diabetes insipidus, while four presented visual problems and one became blind.
Discussion
Surgical principles for the removal of craniopharyngiomas are well codified in literature. Craniopharyngiomas represent 5–10% of paediatric cerebral tumors and generally 0.5 or 2 new cases are reported each year [10]. Results in the treatment of craniopharyngiomas have been likewise extensively reported: excellent and good results accounted for 55% of cases reported in the series of the International Series of Pediatric Craniopharyngiomas (ISPC), with a 22% rate of mortality [6, 10, 12, 22, 37, 45].
Generally, in paediatric series, about 66% of patients are autonomous, 17% have moderate handicaps, 8% have severe handicaps, and 4% manifest total dependence [10].
An important point of the surgical program is related to the decision of realizing a complete or a partial removal. In our opinion, if craniopharyngiomas have to be treated with a direct approach, the surgical goal has to be a complete removal because in children it is better to cure patients during the first surgical procedure. Also, calcifications have to be removed to reduce the rate of recurrences. In the literature, narrowed relationships of calcifications with basal vessel are reported. This condition was rarely encountered in our experience.
Many neurosurgeons support the idea that partial removal leads to better clinical results with a decreased rate of recurrences, but it always seems difficult to decide when to stop the surgical procedure to prevent surgical complications.
Surgical risks seem more important with huge lesions extending into the basal cisterns or inside the third ventricle, but they are also present in cases of small craniopharyngiomas having narrow relationships with the floor of the third ventricle.
During dissection, it is important to avoid tractions on the tumor capsule and to avoid the frequent use of bipolar coagulation to prevent vascular lesions related with the closure of pial or perforating vessels.
Partial removal has to be followed by radiotherapy. It must be kept in mind that, despite the new methods of irradiation, complications are not rare. Moreover, they are generally more severe and disabling in children. This point seems to strongly support the realization of a complete removal of tumor to cure children, thus avoiding the risks of irradiation [3, 21, 30].
As reported by Hoffman, radiotherapy increases the delay of recurrences but does not avert the progression of lesions, thereby favoring the development of sarcomas of the cranial base, meningioma, deficits of the visual pathways, ischemic lesions of the brain and calcifications of the basal ganglia with behavioral troubles [3, 21, 30, 31].
An alternative to the direct surgical approach can be represented by radiosurgery with the limitation that only a lesion of less than 3 cm and with a distance from the chiasm of at least 5 mm can be treated.
The risk of irradiation when the lesions are located near the chiasm and the floor of the third ventricle is blindness.
MRI shows with precision the limits of the lesions and the anatomical relationship between the nervous and vascular structures and the axis of the growth.
A posterior extension and the growth inside the third ventricle increase the possibility of damaging the floor of the third ventricle and the limbic system [36].
The suprachiasmatic nuclei and the column of the fornix that lie in the anterior wall of the hypothalamus (just dorsal to the optic chiasm and lateral to the lamina terminalis) represent a major surgical problem because it is difficult to individualize these structures during removal of the tumor. In such cases, total removal is related with the opening of a large space at the level of the floor of the third ventricle, sometimes with severe hypothalamic sequels.
In our opinion, the main surgical problem in the treatment of craniopharyngiomas is related to the occlusion of perforating vessels originating from the posterior communicating artery. Occlusion of these vessels (they can be confused with tumor vessels) can induce extended basal ganglia vascular lesions which lead to adverse results, as stressed by Samii and many other neurosurgeons [33, 44].
Dissection of the tumor from the main vessels of the basal space (like the carotid artery, the basilar tip or posterior cerebral artery) does not represent a problem for experienced neurosurgeons.
Generally speaking, perforating vessels of the basilar tip and of the basilar bifurcation present little surgical problems because they are directed posteriorly and not forward through the tumor with little risk of coagulation.
Neuropsychological evaluation reveals intellectual sequels in 30–60% of the cases, as stressed by Cavazzuti et al. [7], Carpentieri et al. [9] and Clopper et al. [11]. Basso and Villani reported a rate of neuropsychological sequels in 77% and 70% of treated patients in their respective series.
If endocrine troubles are observed in 40% of patients before surgery, their incidence is approximately 74% after surgical treatment, and 50% of patients present visual pathway deficits after the surgical procedure. These troubles are related to the dissection of the lesion in narrowed contact with the optic nerves and the chiasm [10, 15].
Craniopharyngioma recurrence rates are slightly lower after total removal as reported in literature: 11% for Matson and Crigler [27], 25% for Sweet [38], 16% for Hoffman et al. [21] and 4% for Symon and Sprich [39].
Our own rate of recurrence after total removal is 16%, as reported previously.
Surgical approach
Many approaches have been proposed for the removal of craniopharyngiomas: subfrontal, temporal, pterional, interhemispheric, transventricular, transcortical, transcallosal, transphenoidal, and combined methods. Each approach presents advantages and problems in relation with the tumor’s extension, its relationship with the vascular and nervous structures and the surgeon’s experience.
We prefer the enlarged subfrontal–pterional approach that exposes the tumor through the four triangles of the basal space permitting the approach with different angles: the interoptic, the optico-carotid, the latero-carotid and the carotid bifurcation triangle [24, 28, 34].
All patients in our series have been operated on via this approach, except for four who were operated on via a transventricular route, four patients through a combined subfrontal transventricular approach, and two by a temporal approach. In children, we have not used the transphenoidal approach, and in the previous year we addressed an intra- and suprasellar cystic craniopharyngioma with a transnasal approach assisted by endoscopy.
The subfrontal–pterional approach with the opening of the sylvian fissure favors a large vision of the anterior, lateral, postero-lateral extension of the tumor.
The opening of the lamina terminalis is important in order to remove the tumors extending into the anterior part of the third ventricle. This is most useful when the basal triangles are closed by the short length of the optic nerves and when the optic pathways cover the tumor while the carotid artery closes the access to the lateral portion of the craniopharyngiomas because the optico-carotid triangle is narrowed.
Stuffing with a cottonoid the third ventricle through the lamina terminalis pushes down the floor and favors the fall of the tumor, thus revealing the superior pole and enabling the total removal of the tumor with fewer injuries to the nervous structures.
As also reported by Von Effenterre and Boch [45], the opening of the lamina terminalis provides a large view on the anterior part of third ventricle, allowing the removal of remnants of tumor or residual nodules.
Localization of the lamina terminalis is generally always possible because it is close to the plane of the anterior cerebral, anterior communicating arteries and the plane of the optic chiasm [25, 26].
For lesions presenting a posterior and lateral extension, Symon and Sprich [39] proposed an approach through the anterior temporal lobe that mobilizes the temporal pole and provides access to the tumor from the side below the optic chiasm.
The large temporal lobe of children’s brain could lead surgeons to perform an anterior temporal lobectomy in order to have enough space to remove the lesion.
We used this avenue only in one case, where a tumor developed laterally and posteriorly, to control the basilar trunk and the posterior cerebral artery; with its risky potential, however, the price that this approach carries is unacceptable these days.
The transcallosal approach can expose a tumor developing inside the third ventricle. This approach, as proposed by Konovalov, is used when the lesion develops in the third intraventricular space or partially out of the third ventricle with an extension posterior to the chiasm and to the dorsum sella [23].
The pure intraventricular form of craniopharyngiomas is, in our experience, very rare. Therefore our experience with the transcallosal approach for the treatment of intraventricular craniopharyngiomas concerns a few cases (eight patients) in which this avenue was used alone or combined with another approach.
The need for a combined approach is, in our opinion, very rare and necessary only for giant tumors developing behind and above the plane of the chiasm and of the anterior communicant artery and developing inside the third ventricle and extending up to the Monro hole responsible for hydrocephalus and without a cystic component.
Generally speaking, when they develop inside the third ventricular cavity, craniopharyngiomas do not show an intimate relationship with the ventricular walls and remnants of the tumor are rarely found at this level [23, 25, 44].
In the posterior part of the third ventricle, at the entrance of the aqueduct, and in the supero-posterior region, there are no adhesions. In the anterior region, specifically in the infundibular area, special attention has to be paid during the surgical procedure.
For this particular extension, Yasargyl recommends the transcallosal–pterional approach realizing two small skin flaps, simultaneously, in the frontal and in the pterional region.
The transphenoidal transellar approach is very useful for handling lesions growing in the sella turcica. In children, however, the pneumatization and the extension of the lesion inside the sella represents a problem [44]. This approach is used more often in adult patients.
Today, the use of endoscopy favors a less aggressive approach and allows better vision inside the sella. The use of differently angled lens scopes offers better control during removal of the tumor but does not avert problems relating to haemorrhages from perforating vessels nourishing the lateral part of the tumor capsule [8].
We recently encountered this problem in a patient who, at the end of a total removal of a cystic craniopharyngioma, presented haemorrhage that was apparently controlled with Surgicel and haemostatic foam. In the recovery room 30 min after the extubation, she presented a somnolence followed by a generalized seizure. A CT scan showed a basal haemorrhage. She underwent operation via the transcranial approach and haemostasis was obtained with the coagulation of the posterior communicating artery. The patient went into a deep coma and died due to pulmonary infection followed by a septicemia 1 month later.
For this reason, we think that the transphenoidal approach for the removal of craniopharyngiomas should be indicated only for craniopharyngiomas developing inside the sella and without an extension into the suprasellar space, for cystic tumors developing in the suprasellar region, or for cystic recurrences that can be treated with drainage or a simple aspiration of the cyst.
In contrast, endoscopy can also be useful during a microsurgical procedure to visualize the dark angle behind the structure that the tumor is close to, and “sometimes” to visualize the nervous and vascular structures that have to be treated carefully.
Keyhole surgery assisted by endoscopy has been reported by some authors for the treatment of craniopharyngiomas but it requires great deal of experience.
Pituitary stalk
Preservation of the pituitary stalk represents another point of controversy among neurosurgeons. From a theoretical point of view, it is better to preserve the stalk, yet in many cases this structure is also difficult to visualize even after the complete removal of the tumor. This fact is further delineated in cases of giant craniopharyngiomas, because displacement of the stalk is related to the volume of the tumor.
Many authors have stressed that, for a total removal, it is necessary to sacrifice the stalk; however, Konovalov recommends its preservation even if a portion of the capsule has to remain in place [23].
Hoffman supports the sacrifice of the stalk to achieve total removal and Choux is of the same opinion, affirming that a radical removal is now more important than the stalk’s preservation. Preservation of the stalk can be associated with a decreased incidence of diabetes insipidus and with a better functioning of the pituitary gland [10, 21].
In our group of 64 children treated with a direct approach, the stalk was preserved only in 11 patients, sacrificed in 28 cases, and was not seen in 25 cases. In this group, two patients became pregnant. The other patients presented endocrine sequels, thus showing that preservation of the stalk does not necessarily prevent endocrine insufficiency.
Based on our experience, preservation of the stalk does not constitute an argument to prevent a total removal [1, 2, 10, 14, 17, 24, 35, 39, 42, 44, 45].
Surgical decision
Treatment of craniopharyngiomas in children is through surgical removal. Clinical results are influenced by many factors that have been described and stressed in literature. Experience of surgeons is an important factor to improve the rate of success, as well as to reduce the rate of complications, mortality, and recurrences following total tumor removal [41, 43].
The results reported in literature show that after the surgical removal, the quality of life in children is affected by severe sequels. An alternative to direct surgical removal should thus be found, whenever possible, to ameliorate the clinical results.
Age represents an important risk factor for the treatment of craniopharyngiomas because surgical difficulties are, in our experience, more significant in patients who are 5 years old and above. These difficulties are related to the fact that, in very young people, there is a low probability of invasion of the glial tissue around the lesion, as described by Sweet, which represents a more important factor in total removal [38]. Our experience is in contrast with that of the ISPC, which reported a higher rate of sequels in patients younger than 5 years old, with a high rate of recurrence [10].
Solid craniopharyngiomas represent, in our opinion, an indication for surgical removal. For this particular form, we do not think that valuable alternatives in paediatric age patients are currently available.
Treatment of cystic craniopharyngiomas, on the contrary, provides other alternatives to the direct surgical approach with an intracystic treatment like interstitial radiotherapy or chemotherapy. We have obtained satisfying results with the combined use of intracystic chemotherapy with bleomycin and surgery. Treatment of craniopharyngiomas should not only be a gratifying exercise for surgeons; it must also be kept in mind that children should be able to lead a normal life afterwards.
Surgery, in our opinion, has to be reserved for the solid form of craniopharyngiomas with the goal of achieving total removal while avoiding severe complications and sequels of optic function, endocrine and neuropsychological structures, or should be used for the cystic form that is not sensitive to an alternative treatment.
For cystic lesions, we actually prefer the use intracystic chemotherapy with bleomycine; however, good results have been reported with intracavitary irradiation recently [4, 13, 19].
Craniopharyngiomas and bleomycine
Craniopharyngiomas present large cystic components in many cases. Pure cystic craniopharyngiomas represent 20% of cases, but if we consider the mixed form a cystic component can be found in 80% of cases.
Cystic craniopharyngiomas can be the object of an alternative treatment using intracystic chemotherapy or intracystic irradiation with beta or gamma emitters. Treatment with local intracystic irradiation has the advantage in that the injection of radioactive products, using beta or gamma particles, needs to be administered only once. In contrast, bleomycine requires injections 1 day after in relation to the effectiveness of the dose employed—which means a higher risk of infection. Interstitial irradiation is not without complications. Ischemic lesions can occur in the hypothalamic region and could induce severe clinical manifestations.
Bleomycine is an antineoplastic drug that is toxic for nervous tissues and needs an Ommaya reservoir and should be waterproofed to avoid toxic effects on the brain (Fig. 1).
Umezawa described the use of bleomycine in cerebral cystic lesions in 1966. The first report on the treatment of craniopharyngiomas with bleomycine was published in 1985 by Takahashi et al. [40], who treated a series of seven patients with good results.
Broggi, Lapras and Mottolese and other groups reported good preliminary results in the treatment of cystic lesions and cystic recurrences [5, 18, 29, 46].
Bleomycine is an antimitotic drug used to treat renal and epithelial cancer. The mechanism of action is at the level of the duplication of the chains of DNA favoring cellular death. At the beginning, we used bleomycine mainly for treatment of cystic recurrences with the aim of reducing the risk of such recurrences after surgery.
The direct surgical approach showed us that after intracystic chemotherapy the removal of lesion was easier because the lesion became hard with clearer limits and a well-limited cleavage plane. We decided to use this method for primary cystic lesions to reduce the rate of surgical sequels related with the direct approach used in our series.
Initial results convinced us that bleomycine could represent the strategy of choice for treating cystic craniopharyngiomas. In our experience, patients treated with bleomycine presented fewer visual, endocrinal and behavioral problems, with better school results in comparison with our results using the direct surgical approach (Figs. 2, 3).
The results obtained seem definitive because, so far, we have not recorded recurrences or evolution in the growth of craniopharyngiomas in patients treated only with intracystic chemotherapy. In our opinion, bleomycine represents an effort to find new strategies to improve results in the treatment of craniopharyngiomas, thus reducing surgical mortality and morbidity and improving the quality of life of patients, especially children.
Conclusion
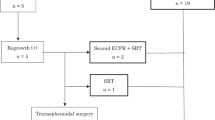
In conclusion, our treatment strategy is programmed to consider the following particular decisional tree:
-
for solid craniopharyngiomas, a direct surgical approach with the goal of obtaining a total removal and definitive cure of the patients;
-
for a cystic or mixed form of tumor, we first propose, when possible, the alternative strategy with intracystic bleomycine.
We rarely propose a simple control. The possibility of a partial removal is submitted to the realization of a complementary radiotherapy that should be proposed only when the patient is at least 7 years old to reduce the occurrence of sequels in the young brain.
In cystic recurrences, for patients who previously underwent operations, we propose intracystic chemotherapy with bleomycine, whereas for nodular solid recurrences, the direct approach should be considered.
In our experience, bleomycine was effective. We do not understand the disparity of the different experiences reported in literature with this drug.
The search for new strategies to improve the quality of life of patients is an important cornerstone of our philosophy but, until now, a definitive solution is still to be found.
We are conscious that in the future (particularly for young neurosurgeons) the increased number of neurosurgical centers and the subsequent dilution of this pathology can lead to a decline in the quality surgical skills, thereby making it even more important to formulate alternative strategies that would ensure a better quality of life for patients.
References
Al-Mefty O, Massounam M, Weaver P, Sakatin S, Jinkins JR, Fox JL (1985) Microsurgery of giant craniopharyngiomas in children. Neurosurgery 17:685–695
Al-Mefty O, Kersh J, Smith R (1990) The long term side effects of radiation therapy for benign brain tumors in adults. J Neurosurg 73:502–512
Amacher AL (1980) Craniopharyngioma: the controversy regarding radiotherapy. Child Brain 6:57–64
Blacklund E, Axelson B, Bergstrand C, Erikson A, Noren B, Ribesso E, Rahn T, Schnel P, Tallstedt L, Saaf M (1989) Treatment of craniopharyngiomas. The stereotactic approach in a ten to twenty-three year’s perspective. Surgical, radiological and ophthalmological aspects. Acta Neurochir 99:11–19
Broggi G, Giorgi C, Franzini A, Servello D, Solero CL (1989) Preliminary results of intracavitary treatment of craniopharyngioma with bleomycin. J Neurosurg Sci 33:145–148
Carmel P, Antunes S, Chang C (1982) Craniopharyngiomas in children. Neurosurgery 11:382–388
Cavazzuti V, Fischer EG, Welch K (1983) Neurological and psychological sequelae following different treatment of craniopharyngioma in children. J Neurosurg 59:409
Chakrabarti I, Amar PA, Couldwell W, Weiss MH (2005) Long-term neurological, visual, and endocrine outcomes following transnasal resection of craniopharyngiomas. J Neurosurg 105:650–657
Carpentieri SC, Waber D, Scott MR, Goumernorova LC, Kieran MW, Cohen LE, Kim F, Billet AL, Tarbell NJ, Pomeroy SL (2001) Memory deficits among children with craniopharyngiomas. Neurosurgery 49(5):1053–1058
Choux M, Lena G, Genitori L (1991) Le craniopharyngiome de l’enfant. Neurochirurgia 37(Suppl 1):1–174
Clopper R, Meyer WJ, Udvarhelyi GB, Honey J, Aarabi B, Hulvihil JJ, Piasio M (1977) Post-surgical IQ and behavioral data on twenty patients with a history of childhood craniopharyngioma. Psychoneuroendocrinology 2:365–372
Duff JM, Meyer BF, Ilstrup D, Laws ED, Schlek CD, Scheithauer BW (2000) Long-term outcomes for surgically resected craniopharyngiomas. Neurosurgery 46(2):291–305
Contine LS, Randall SH, Rubin P, MacDonald J (1989) Craniopharyngiomas: fluctuation in cyst size following surgery and radiation therapy. Neurosurgery 24:53–59
Epstein FJ, Handler MH (1994) Craniopharyngioma: the answer. Proc. Symposium, New York, NY, Dec. 17–19, 1993. Pediatr Neurosurg 21(Suppl 1):1–132
Fischer EG, Welch K, Belli JA, Wallman J, Shillito JJ, Winston KR, Cassady R (1985) Treatment of craniopharyngiomas in children 1972–1981. Neurosurgery 62:496–501
Garcia-Uria J (1978) Surgical experience with craniopharyngioma in adults. Surg Neurol 9:11–14
Graham PH, Gattamanrni HR, Birch JM (1992) Pediatric craniopharyngiomas: a regional review. Br J Neurosurg 6:187–193
Hader WJ, Steinbock P, Hukin J, Fryer C (2000) Intratumoral therapy with bleomycin for cystic craniopharyngiomas in children. Pediatr Neurosurg 33:211–218
Hasegawa T, Kondziolka D, Hadjipanayis CG, Lundsford DL (2004) Management of cystic craniopharyngiomas with phosporus-32 intracavitary irradiation. Neurosurgery 54(4):813–822
Hoff JF, Patterson RH Jr (1972) Craniopharyngiomas in children and adults. J Neurosurg 36:299–302
Hoffman HJ, Hendrick EB, Humphreys RP, Buncic JR, Amstrong DL, Jenkin RD (1977) Management of craniopharyngioma in children. J Neurosurg 47:218–227
Kahn GA, Gosh HH, Seeger JF, Hicks SP (1973) Forty-five years experience with craniopharyngioma. Surg Neurol 1:5–12
Konovalov AN (1998) Technique and strategies of direct surgical management of craniopharyngiomas. In: Apuzzo MLJ (ed) Surgery of the third ventricle, 2 edn. Williams and Wilkins, Baltimore, pp 1133–1142
Lapras C, Patet JD, Mottolese C, Gharbi S, Lapras Jr C (1987) Craniopharyngiomas in childhood: analysis of 42 cases. Prog Exp Tumor Res 30:350–358
Maira G, Anile C, Rossi GF, Colosimo C (1995) Surgical treatment of craniopharyngiomas: an evaluation of the transphenoidal and pterional approaches. Neurosurgery 36:715–724
Maira G, Anile C, Colosimo C, Cabezas D (2000) Craniopharyngiomas of the thirs ventricle: trans-lamina terminalis approach. Neurosurgery 47(4):857–865
Matson DD, Crigler JF (1969) Management of craniopharyngioma in childhood. J Neurosurg 30:377–390
Mac Lone DB, Raimondi AJ, Naidich TP (1982) Craniopharyngiomas. Child Brain 9:188–200
Mottolese C, Stan H, Hermier M, Berlier P, Convert J, Frappaz D, Lapras C (2001) Intracystic chemotharapy with bleomycin in the treatment of craniopharyngiomas. Childs Nerv Syst 17:724–730
Rajan B, Ashley S, Gorman C, Jose CC, Horwich A, Bloom HJ, Marsh H, Brada M (1993) Craniopharyngioma—long term results following limited surgery and radiotherapy. Radiother Oncol 26:1–10
Regine WF, Mohiuddin M, Kramer S (1993) Long term results of pediatric and adult craniopharyngiomas treated with combined surgery and radiation. Report of 92 cases. Radiother Oncol 27:13–21
Rougerie J (1979) What can be expected from the surgical treatment of craniopharyngiomas in children. Report of 92 cases. Child Brain 5:433–449
Samii M, Samii A (1995) Surgical management of craniopharyngiomas. In: Schmidek HH, Sweet WH (eds) Operative neurosurgical techniques: indications, methods and results, 3rd edn., vol 1. Saunders, Philadelphia, pp 357–370
Shillito J (1980) Craniopharyngiomas: the subfrontal approach, or none at all? Clin Neurosurg 27:188–205
Shillito J (1986) Treatment of craniopharyngioma. Clin Neurosurg 33:533–546
Steno J (1985) Microsurgical topography of craniopharyngiomas. Acta Neurochir 35(Suppl):94–100
Sung DI, Chang CH, Harisiadis L, Carmel PW (1981) Treatment results of craniopharyngiomas. Cancer 47:847–852
Sweet WH (1976) Radical surgical treatment of craniopharyngioma. Recurrent craniopharyngiomas: therapeutic alternatives. Clin Neurosurg 23(52–79)206–229
Symon L, Sprich W (1985) Radical excision of craniopharyngiomas. Results in 20 patients. J Neurosurg 62:174–181
Takahashi H, Nakazawa S, Shimura T (1966) Evaluation of postoperative intratumoral injection of bleomycin for craniopharyngioma in children. J Neurosurg 84:124–126
Till K (1982) Craniopharyngioma. Child Brain 9:179–187
Tomita T, Mac Lone DB (1993) Radical resections of childhood craniopharyngiomas. Pediatr Neurosurg 19:6–14
Weiner M, Wisoff J, Rosenberg M, Kupersmith M, Cohen H, Zagzag D, Shiminski-Mahler T, Flam E, Epstein F, Miller D (1994) Craniopharyngiomas: a clinical analysis of factors predictives of recurrence and functional outcome. Neurosurgery 35:1001–1011
Yasargil MG, Curcic M, Kis M, Siegenthaller G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas approaches and long-term results in 144 patients. J Neurosurg 73:3–11
Van Effenterre R, Boch A (1997) Craniopharyngiomes de l’adulte et de l’enfant. Etude d’une série chirurgicale de 106 cas consécutifs. Neurochirurgia 43:187–211
Zanon N (1999) Bleomycin treatment of cystic craniopharyngioma. In: Choux M, Di Rocco C, Hockley A, Walker M (eds) Pediatric neurosurgery. Churchill Livingstone, Edinburgh
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mottolese, C., Szathmari, A., Berlier, P. et al. Craniopharyngiomas: our experience in Lyon. Childs Nerv Syst 21, 790–798 (2005). https://doi.org/10.1007/s00381-005-1242-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-005-1242-1